Abstract
Survivors to COVID-19 have described long-term symptoms after acute disease. These signs constitute a heterogeneous group named long COVID or persistent COVID. The aim of this study is to describe persisting symptoms 6 months after COVID-19 diagnosis in a prospective cohort in the Northwest Spain. This is a prospective cohort study performed in the COHVID-GS. This cohort includes patients in clinical follow-up in a health area of 569,534 inhabitants after SARS-CoV-2/COVID-19 diagnosis. Clinical and epidemiological characteristics were collected during the follow up. A total of 248 patients completed 6 months follow-up, 176 (69.4%) required hospitalization and 29 (10.2%) of them needed critical care. At 6 months, 119 (48.0%) patients described one or more persisting symptoms. The most prevalent were: extra-thoracic symptoms (39.1%), chest symptoms (27%), dyspnoea (20.6%), and fatigue (16.1%). These symptoms were more common in hospitalized patients (52.3% vs. 38.2%) and in women (59.0% vs. 40.5%). The multivariate analysis identified COPD, women gender and tobacco consumption as risk factors for long COVID. Persisting symptoms are common after COVID-19 especially in hospitalized patients compared to outpatients (52.3% vs. 38.2%). Based on these findings, special attention and clinical follow-up after acute SARS-CoV-2 infection should be provided for hospitalized patients with previous lung diseases, tobacco consumption, and women.
Similar content being viewed by others
Introduction
COVID-19 pandemic has been a major health challenge around the world, with an unprecedented impact on health systems, society and modern medicine. Acute phase of COVID-19 varies widely, from asymptomatic disease to pneumonia, acute respiratory distress syndrome (ARDS) and multisystem organ failure. Most commonly reported symptoms are fever, cough, dyspnoea, myalgia and anosmia. Several comorbidities have been identified as risk factors for severe disease, such as arterial hypertension, chronic heart disease or diabetes mellitus1.
In the past few months, many patients reported persisting symptoms after the acute phase of coronavirus disease. These signs are a heterogeneous group, affecting multiple organ systems, including respiratory tract (dyspnoea, chest pain, cough), muscle and joints (arthralgia, myalgia), nervous system (taste or smell alterations, headache, concentration difficulty). There are also many general or unspecified symptoms such as fatigue or hair loss. This group of signs has been named “long COVID” or “persisting COVID”. However, the definition of this syndrome remains unclear and there is not consensus regarding the name and the diagnostic criteria2. It is not clear which symptoms could be related to coronavirus and how to define this persistent period after the acute phase3,4. The origin of these symptoms remains unknown. However, it is likely to be a combination of a direct damage caused by SARS-CoV-2, previous comorbidities, immunological activation, psychological and emotional factors5,6,7. The aim of this study is to describe persisting symptoms 6 months after COVID-19 diagnosis in a prospective cohort in the Northwest Spain. The study population includes mild, moderate, serious or critical cases classified as hospitalized or non-hospitalized patients.
Methods
Study design
This is a prospective cohort study performed in the COVID-19 Cohort of Galicia Sur Health Institute (COHVID-GS). This is an open cohort associated to a Biobank for sample collection including patients in clinical follow-up at Álvaro Cunqueiro Hospital (Vigo, Spain), a reference hospital for 564,534 inhabitants after SARS-CoV-2/COVID-19 diagnosis (all had a positive PCR for SARS-CoV-2 on nasal swab) (https://www.iisgaliciasur.es/apoyo-a-la-investigacion/cohorte-covid19/). Clinical and epidemiological characteristics were collected at the diagnosis time and during the follow up after 6 months of the diagnosis. The aim of this study is to describe the frequency of long COVID symptoms in hospitalized and non-hospitalized subjects.
Procedures
All patients included at the COHVID-GS were scheduled for clinical follow-up visits using phone calls and on site visits after 1, 3 and 6 months of the diagnosis. Subjects were classified as hospitalized when they required hospitalization for at least 24 h. Main hospitalization criteria were pneumonia on chest X-ray and/or respiratory insufficiency. At each visit, patients completed a custom symptom questionnaire (supplementary data). COHVID-GS also includes data about comorbidities, smoke status, weight and height. Pre-existing symptoms that did not change after the diagnosis of COVID-19 were excluded. Symptoms of another suspected origin were also excluded (e.g., iron deficit, thyroid dysfunction). Dyspnoea was classified according to the British Medical Research Council mMRC scale. Brain fog was defined as poor concentration, recent memory disorder or inability to focus. COPD was defined according to the Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (GOLD) as a FEV1/FVC < 70% with or without symptoms (cough, sputum production).
In addition, the COHVID-GS records data about several biomarkers during the follow-up. C-reactive protein (CRP; normal range 0.0–8.0 mg/L), ferritin (normal range 22.0–300.0 ng/mL) and lactate dehydrogenase (LDH; normal range 85.0–240.0 IU/L) after 6 months.
In this study, we only included patients who survived at least 6 months after the COVID-19 diagnosis and completed all follow-up visits. We excluded patients who died during the study period, those who refused to complete all follow-up visits and those who were unable to assist to the site (e.g., cognitive impairment, physical disability).
The recruitment period started in March 2020 and ended by May 2021 and included consecutive cases. For the purpose of this study, data was censored in January 2021 when the first wave cases reached 6 months since COVID-19 diagnosis.
Ethics
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This project was approved by the Ethical Committee of Pontevedra-Vigo-Ourense (reference 2021/184). All the patients included in the study belong to the COHVID-GS, which signed an informed consent form at the time of inclusion in the cohort.
Statistical analysis
For quantitative variables, median and interquartile were calculated. Categorical variables were reported as frequencies and percentages. Subjects were classified in two groups, based on their need for hospitalization due to Covid-19. Symptoms, clinical and epidemiological data were compared in both groups using chi-square test, Fisher’s exact test or U Man–Whitney test as appropriate. p-value less than 0.05 was considered significant. Multivariable logistic regression analysis with backward stepwise elimination was used to identify risk factors for long COVID. Those variables with a p value lesser than 0.1 were considered as independent variables. Statistical analyses were performed with IBM Statistical Product and Service Solutions (SPSS) program, version 22.
Results
Baseline characteristics of the study population
A total of 630 patients were included in the COHVID-GS. However, 81 of them died during the hospitalization period and only 248 subjects who survived completed the 6 months period of follow-up. Of them, 172 required hospitalization and 76 were never hospitalized. The baseline characteristics of the study population are shown in Table 1.
Overall, the median age was 57 years, however, non-hospitalized patients were significantly younger than those who were hospitalized (62 vs. 47 years, respectively). Moreover, men were more frequent in both groups (148 men, 59.7%).
Most common comorbidities were obesity (n = 75, 30.2%), followed by arterial hypertension (n = 65, 26.2%) and diabetes mellitus (n = 26, 10.1%). Moreover, all comorbidities were more usual in the hospitalized group, except for asthma (4.1% vs. 18.4% respectively). In the hospitalized group, 29 patients (16.8%) required critical care management, including 23 who required invasive mechanical ventilation.
6 months after the COVID-19 diagnosis, 119 patients (48.9%) reported at least one symptom (Table 2). Chest symptoms were more frequent (n = 67, 27%), of which dyspnoea (n = 51, 20.6%), chest pain (n = 15, 6.0%) and cough (n = 11, 4.4%) were the most commonly reported.
Extra-thoracic symptoms were described in 97 patients (39.1%) and the most frequently reported were fatigue (n = 40, 16.1%), musculo-skeletal symptoms (n = 18, 7.3%) and hair loss (n = 18, 7.3%).
Overall, smell disorders were more frequent than taste disorders (6.9% vs. 4.0%, respectively). Neurological symptoms 6 months after the COVID-19 diagnosis, excluding smell and taste disruptions, were uncommon (less than 5.0%). Headache, mood disorder and sleep disturbance were the most common neurological symptoms. Nine patients (3.2%) reported symptoms that met brain fog criteria. Digestive symptoms were also uncommon (n = 10, 4.0%).
Persisting symptoms in hospitalized and non-hospitalized patients
Persisting symptoms were more prevalent in the hospitalized group (52.3% vs. 38.2%, p = 0.040). Chest symptoms in this group were more frequently reported compared with the non-hospitalized group (32.0% vs. 15.8%, p = 0.008). However, extra-thoracic symptoms did not differ between both groups (43.0% vs. 30.3%, p = 0.058). The most common chest symptom was dyspnoea, which was more frequently reported in hospitalized patients (25.0% vs. 10.5%, p = 0.010). Most of the subjects reported a mMRC (modified Medical Research Council) grade 1 dyspnoea (n = 43, 17.3%). On the other hand, chest pain (6.4% vs. 5.3%) and persisting cough (5.8% vs. 1.3%) did not vary between both groups.
Fatigue (20.9% vs. 5.3%, p = 0.001) and myalgia (5.8% vs. 0%, p = 0.034) were more frequently reported in the hospitalized group than in the non-hospitalized group. Also, hair loss (9.3% vs. 2.6%) and sleep disorders (5.2% vs. 0%) were more common in hospitalized patients, although this difference was not statistically significant. Arthralgia (5.8% vs. 2.6%), ageusia (2.9% vs. 6.6%) and digestive symptoms (4.1% vs. 3.9%) did not differ between both groups. Anosmia was more prevalent in non-hospitalized subjects (5.2% vs. 10.5%, p = 0.054), but did not meet statistical significance.
Persisting symptoms in ICU-admitted patients
Persisting symptoms were compared between patients admitted to ICU and patients admitted to the hospital ward. We did not find any association between patients admitted to ICU or to the hospital ward and the persistence of any symptoms at 6 months.
Persisting symptoms in men and woman
Overall, persisting symptoms were more common in women than men (59.0% vs. 40.5%, p = 0.004) (Table 3). Dyspnoea (29.0 vs. 14.9%, p = 0.007), headache (10.0% vs. 4.8%, p = 0.004), fatigue (22.0% vs. 12.2%, p = 0.039) and hair loss (15.0% vs. 7.3%, p < 0.001) were all more prevalent in women while anosmia (6.0% vs. 7.4%), taste disturbance (4.0% in both genders) and musculoskeletal symptoms (6.8% vs. 8.0%) did not differ between women and men.
Predictors of COVID-19 persisting symptoms
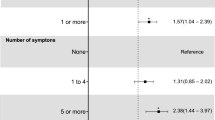
We performed a multivariate analysis in order to determine the risk factors for persisting COVID-19 symptoms. We identified Chronic Pulmonary Obstructive Disease (COPD) (OR 5.009; CI 95%, 1.321–18.997, p = 0.018), woman gender (OR 2.700, 95% CI 1.543–4.724, p < 0.001) and tobacco consumption as independent risk factors for remaining symptoms (OR 1.736; CI 95%, 1.002–3.007, p = 0.049) (Table 4).
COPD was the only comorbidity associated with a higher prevalence of persisting symptoms. Fourteen patients (5.1%) were affected by COPD before COVID-19 diagnosis and 12 of them (80.0%) had at least one persisting symptom. Nine subjects (75.0%) reported new or worsened dyspnoea compared with their perception prior COVID-19 diagnosis. Dyspnoea (60.0% vs. 18.0%, p = 0.001) and chest pain (26.7% vs. 4.7%, p = 0.008) were most commonly reported in COPD group. On the other hand, cough (6.7% vs. 4.3%), fatigue (20.0% vs. 15.9%), myalgia (13.3% vs. 3.4%), arthralgia (6.7% vs. 4.7%) did not differ between COPD and non-COPD subjects.
Biomarkers in symptomatic and asymptomatic patients
The following serum inflammatory biomarkers CRP, ferritin and LDH were assessed 6 months since COVID-19 diagnosis in symptomatic and asymptomatic patients.
Although CRP and LDH levels were higher in the hospitalized group, most of samples met the normal range criteria. Therefore, the levels of inflammatory biomarkers were not associated with the persistence of symptoms.
Discussion
We characterized long COVID in a prospective cohort of patients with mild and severe COVID-19 with a systematic clinical follow-up. The prevalence of any symptom at 6 months was elevated (48%), with a different distribution between hospitalized and non-hospitalized patients. Persisting symptoms did not differ between those patients who needed critical care and those who did not.
Long COVID has been recognized as a public-health problem and a matter of concern for COVID-19 surveys. Several studies have reported information in series of patients in clinical follow-up after the acute infection, but many questions remain unsolved. One of them is if long COVID might be gender-dependent. In our study, women showed a higher prevalence of persisting symptoms in hospitalized and in non-hospitalized groups. Dyspnoea, headache, fatigue and hair loss were all more common in women than men.
A prior study performed by Huang et al. described a high prevalence of long COVID symptoms in a large cohort of hospitalized patients8, around 76%, slightly above our study. The most commonly reported symptoms were fatigue, chronic pain, and anxiety or depression. The prevalence of persisting symptoms was closely related to COVID-19 severity. Our study reported similar symptoms, with a slightly different distribution since we have included an inpatients population, while Huang et al., only included hospitalized patients. This could explain the higher prevalence observed in our series for some symptoms (i.e. dyspnea). Interestingly, they also observed a higher prevalence of long COVID among women compared with men8. A recent study by Blomberg et al. also reported a higher frequency of persisting symptoms in hospitalized patients. Similarly to our results, COPD and asthma were also related to a worse fatigue score and a higher number of persisting symptoms9. Our findings, reinforces the relationship between persisting symptoms, hospitalization, woman gender, and COPD.
In the recent months, more than 200 persistent symptoms have been described after the acute phase of COVID-19. Most of them are related to the respiratory tract (dyspnoea, cough, chest pain), the main target of SARS-CoV-2. However, many patients report other type of symptoms such as fatigue, cognitive impairment or smell disorders10.
Chest symptoms were the most common reported affection, with greater prevalence in the hospitalized group. This difference may be related to pneumonia, respiratory distress and lung damage, which were more frequent in hospitalized subjects. The prevalence of chest symptoms in this group raised to 52%, slightly higher than observed in previous reports11. However, even in the absence of pneumonia, 15% of non-hospitalized patients reported persisting chest symptoms. Recently, Blomberg et al., described long COVID symptoms in Norwegian non-hospitalized and hospitalized population with a slightly higher prevalence than in our study (52.0% vs. 38.2% respectively)9.
Fatigue was also frequent, reaching up to 20.9% in the hospitalized group. Although this percentage is relevant, it was lower than others reported before12,13, around 65–70%. However, these studies had a shorter follow-up period (90–100 days after hospitalization). The reason of fatigue remains unknown. Several causes have been proposed such as direct nervous and muscle damage due to SARS-CoV-2 replication5,6, persisting inflammation, or emotional factors7.
On the other hand, myalgia and arthralgia were less frequent than in previous studies. Sykes et al.14 described a prevalence of 50% of these symptoms in hospitalized patients at 100 days after discharge.
Overall, persisting anosmia was reported in 6.8% of subjects and was more common in the non-hospitalized group (10.5% vs. 5.2%, respectively). This prevalence is lower than published in previous studies15,16. In addition, prior reports have suggested that anosmia may be associated with a mild to moderate COVID-19 and it could be more common in women than men15. However, the low prevalence of anosmia observed in our study cannot confirm this hypothesis.
At 6 months, 9 subjects reported unspecified neurological symptoms such as poor concentration, loss of recent memory or inability to focus. These unspecified symptoms are named brain fog by some authors, but its origin or relationship with coronavirus disease remains unknown5,17. Brain fog syndrome after COVID-19 has been reported previously18,19, although there is not a validated diagnostic criteria established. The studies focused on neurological sequelae of COVID-19 did not use a unanimous criterion and therefore, the conclusions are very heterogeneous. The lack of knowledge about this type of symptoms makes more difficult to study the real prevalence or to establish a relationship with coronavirus disease. Another neurological symptoms like sleep or mood disorders have been reported with a similar prevalence than in our study20. However, psychological conditions, stress and isolation may be associated with these symptoms, alongside with coronavirus infection. The higher prevalence on the hospitalized group may be due to the severity of illness, admission to critical care or treatments (e.g., corticosteroids, immunosuppressants).
Regarding the impact of ICU admission in the development of persisting symptoms, contradictory results have been reported up to now21,22. In our study, we did not find any relationship between ICU admission and the persistence of symptoms. However, the small sample size of ICU-admitted patients could be underestimating this association.
We identified COPD, women gender, tobacco consumption and the need for hospitalization as predictors for long COVID. Women gender has been reported before as a risk factor for hospitalized subjects but there is a lack of information about other predictors of long COVID.
On the other hand, only few studies have evaluated classical inflammatory biomarkers (i.e., CRP, ferritin) in patients with persistent COVID. Pasini et al.23 have observed higher levels of CRP, interleukin-6 and soluble CD25 in hospitalized patients 75 days after the COVID-19 diagnosis. However, we did not find any association of CRP, ferritin and LDH with the persistence of symptoms.
Our findings suggest that some of the persisting symptoms could be related to a previous lung comorbidity and hospitalization. In addition, pneumonia and ARDS may also contribute to develop persisting symptoms.
This study has few limitations. Firstly, some of the symptoms reported are subjective and based on the patient’s testimony (e.g. fatigue, headache, dyspnoea). Additionally, the lack of validated scales to measure most of the symptoms makes difficult to compare data between subjects or studies. Secondly, most of the symptoms may be affected by personal, psychological or environmental factors. We needed to use a non-validated custom questionnaire, as there is not a specific post-COVID-19 document established. Many symptoms could be higher reported in one group than another for unrelated reasons with coronavirus disease. This is the case for hair loss that may be more noticed in women and therefore more reported, leading to a possible increase of the prevalence in women. In addition, previous comorbidities and age could increase the persisting symptoms in the hospitalized group. For COPD patients, we did not record symptoms that started before COVID-19 diagnosis. Therefore, it is possible that COPD patients reported more frequently chest or respiratory symptoms.
Conclusions
In summary, a high prevalence of long COVID (48%) was observed in patients after 6 months of acute SARS-CoV-2 infection. Overall, persistent symptoms were more common in hospitalized patients compared to outpatients (52.3% vs 38.2%). These symptoms were more common in women than men (59.0% vs. 40.5%). COPD, woman gender, and tobacco consumption were identified as long COVID predictors. These findings suggest that in those patients that required hospitalization after SARS-CoV-2 infection a close clinical follow-up might be recommended. Special attention should be provided for patients with previous lung diseases, tobacco consumption and women.
Data availability
The datasets during and/or analyzed during the current study available from the COHVID-GS on reasonable request (https://www.iisgaliciasur.es/apoyo-a-la-investigacion/cohorte-covid19/).
Change history
16 August 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41598-022-18023-z
References
Berenguer, J. et al. Characteristics and predictors of death among 4035 consecutively hospitalized patients with COVID-19 in Spain. Clin. Microbiol. Infect. 26(11), 1525–1536. https://doi.org/10.1016/j.cmi.2020.07.024 (2020).
Al-Jahdhami, I., Al-Naamani, K. & Al-Mawali, A. The post-acute COVID-19 syndrome (long COVID). Oman Med. J. 36(1), e220–e220. https://doi.org/10.5001/omj.2021.91 (2021).
Fernández-de-las-Peñas, C., Palacios-Ceña, D., Gómez-Mayordomo, V., Cuadrado, M. L. & Florencio, L. L. Defining post-COVID symptoms (post-acute COVID, long COVID, persistent post-COVID): An integrative classification. Int. J. Environ. Res. Pub. Health. 18(5), 2621. https://doi.org/10.3390/ijerph18052621 (2021).
Halpin, S., O’Connor, R. & Sivan, M. Long COVID and chronic COVID syndromes. J. Med. Virol. 93(3), 1242–1243. https://doi.org/10.1002/jmv.26587 (2021).
Pezzini, A. & Padovani, A. Lifting the mask on neurological manifestations of COVID-19. Nat. Rev. Neurol. 16(11), 636–644. https://doi.org/10.1038/s41582-020-0398-3 (2020).
Ferrandi, P. J., Alway, S. E. & Mohamed, J. S. The interaction between SARS-CoV-2 and ACE2 may have consequences for skeletal muscle viral susceptibility and myopathies. J. Appl. Physiol. 129(4), 864–867. https://doi.org/10.1152/japplphysiol.00321.2020 (2020).
Morgul, E. et al. COVID-19 pandemic and psychological fatigue in Turkey. Int. J. Soc. Psychiatr. 67(2), 128–135. https://doi.org/10.1177/0020764020941889 (2021).
Huang, C. et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet 397(10270), 220–232. https://doi.org/10.1016/S0140-6736(20)32656-8 (2021).
Blomberg, B. et al. Long COVID in a prospective cohort of home-isolated patients. Nat. Med. https://doi.org/10.1038/s41591-021-01433-3 (2021).
Davis, H. E. et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. medRxiv https://doi.org/10.1101/2020.12.24.20248802 (2021).
Xiong, Q. et al. Clinical sequelae of COVID-19 survivors in Wuhan, China: A single-centre longitudinal study. Clin. Microbiol. Infect. 27(1), 89–95. https://doi.org/10.1016/j.cmi.2020.09.023 (2021).
Mandal, S. et al. ‘Long-COVID’: A cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax 76(4), 396–398. https://doi.org/10.1136/thoraxjnl-2020-215818 (2021).
Carfì, A., Bernabei, R. & Landi, F. Persistent symptoms in patients after acute COVID-19. JAMA 324(6), 603. https://doi.org/10.1001/jama.2020.12603 (2020).
Sykes, D. L. et al. Post-COVID-19 symptom burden: What is long-COVID and how should we manage it?. Lung 199(2), 113–119. https://doi.org/10.1007/s00408-021-00423-z (2021).
Hopkins, C., Surda, P., Whitehead, E. & Kumar, B. N. Early recovery following new onset anosmia during the COVID-19 pandemic: An observational cohort study. J. Otolaryngol.: Head Neck Surg. 49(1), 26. https://doi.org/10.1186/s40463-020-00423-8 (2020).
D’Ascanio, L. et al. A. Olfactory dysfunction in COVID-19 patients prevalence and prognosis for recovering sense of smell. Otolaryngol. Head Neck Surg. 164(1), 82–86. https://doi.org/10.1177/0194599820943530 (2021).
Stefano, G. B. et al. Editorial: The pathogenesis of long-term neuropsychiatric COVID-19 and the role of microglia, mitochondria, and persistent neuroinflammation: A hypothesis. Med. Sci. Monit. 10(27), e933015. https://doi.org/10.12659/MSM.933015 (2021).
Pinna, P. et al. Neurological manifestations and COVID-19: Experiences from a tertiary care center at the Frontline. J Neurol Sci. 415, 116969. https://doi.org/10.1016/j.jns.2020.116969 (2020).
Karadaş, Ö., Öztürk, B. & Sonkaya, A. R. A prospective clinical study of detailed neurological manifestations in patients with COVID-19. Neurol Sci. 41(8), 1991–1995. https://doi.org/10.1007/s10072-020-04547-7 (2020).
Romero-Sánchez, C. M. et al. Neurologic manifestations in hospitalized patients with COVID-19: The ALBACOVID registry. Neurology 95(8), e1060–e1070. https://doi.org/10.1212/WNL.0000000000009937 (2020).
Malik, P. et al. Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL): A systematic review and meta-analysis. J. Med. Virol. https://doi.org/10.1002/jmv.27309 (2021).
Townsend, L. et al. Persistent poor health after covid-19 is not associated with respiratory complications or initial disease severity. Ann. Am. Thorac. Soc. 18(6), 997–1003. https://doi.org/10.1513/AnnalsATS.202009-1175OC (2021).
Pasini, E. et al. Serum metabolic profile in patients with long-covid (PASC) syndrome: Clinical implications. Front. Med. 8(July), 1–8. https://doi.org/10.3389/fmed.2021.714426 (2021).
Acknowledgements
We would like to thank all the members of COHVID-GS and IISGS Biobank, patients and nursing staff and the Methodology and Statistic Unit.
Funding
COVID-19 Cohort Galicia Sur Health Research Institute (COHVID-GS) is funded by the Instituto de Salud Carlos III through the FONDO COVID19 (COV20/00698). Alexandre Pérez is hired under a Rio Hortega contract (CM20/00243).
Author information
Authors and Affiliations
Consortia
Contributions
A.P. wrote the main manuscript. A.A. prepared supplementary material, tables and figures. E.P., A.V. and M.C. reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained an error in Table 1, where the values given for the Tobacco use were incorrect for “Total”, “Hospitalized” and “Non Hospitalized”. Full information regarding the corrections made can be found in the correction for this Article.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pérez-González, A., Araújo-Ameijeiras, A., Fernández-Villar, A. et al. Long COVID in hospitalized and non-hospitalized patients in a large cohort in Northwest Spain, a prospective cohort study. Sci Rep 12, 3369 (2022). https://doi.org/10.1038/s41598-022-07414-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-07414-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.