Abstract
Chronic kidney disease (CKD) has been recognized as a highly prevalent risk factor for both the severity of coronavirus disease 2019 (COVID-19) and COVID-19 associated adverse outcomes. In this multicenter observational cohort study, we aim to determine mortality and readmission rates of patients hospitalized for COVID-19 across varying CKD stages. We performed a multicenter cohort study among COVID-19 patients included in the Dutch COVIDPredict cohort. The cohort consists of hospitalized patients from March 2020 until July 2021 with PCR-confirmed SARS-CoV-2 infection or a highly suspected CT scan-based infection with a CORADS score ≥ 4. A total of 4151 hospitalized COVID-19 patients were included of who 389 had a history of CKD before admission. After adjusting for all confounding covariables, in patients with CKD stage 3a, stage 3b, stage 4 and patients with KTX (kidney transplantation), odds ratios of death and readmission compared to patients without CKD ranged from 1.96 to 8.94. We demonstrate an evident increased 12-week mortality and readmission rate in patients with chronic kidney disease. Besides justified concerns for kidney transplant patients, clinicians should also be aware of more severe COVID-19 outcomes and increased vulnerability in CKD patients.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) has been recognized as a highly prevalent risk factor for both the severity of coronavirus disease 2019 (COVID-19) and COVID-19 associated adverse outcomes1,2. Mortality rates of COVID-19 attributed to CKD may vary between 1.3% and 21.3%3,4. Whether disease severity and mortality rates depend on the CKD stage or are explained either by a higher prevalence of comorbid conditions in COVID-19 or by kidney-specific factors, such as uremic or immunological factors, is incompletely known. In January 2021, the European Renal Association and European Dialysis and Transplantation Association (ERA-EDTA) called for action to include all CKD stages in COVID-19 related clinical research5. So far, most reports about COVID-19 severity and outcomes do not include all CKD stages and direct comparisons with non-CKD patients are limited3,4. Also, a complete characterization of CKD patients hospitalized for COVID-19, including clinical and laboratory data at hospital admission, is infrequently reported. In this multicenter observational cohort study, we aim to determine mortality and readmission rates of patients hospitalized for COVID-19 across varying CKD stages.
Materials and methods
Study population and definitions
We performed a multicenter cohort study among COVID-19 patients included in the Dutch COVIDPredict cohort6,7,8. The COVIDPredict is a consortium of eleven hospitals in the Netherlands that aim to understand better and predict which COVID-19 patients should receive which treatments and which type of care. All methods were carried out in accordance with relevant guidelines and regulations. The study protocol was reviewed by the medical ethics committees of the Amsterdam University Medical Centers (Amsterdam UMC; 20.131). The need for informed consent was waived by the Institutional Review Board of Amsterdam University Medical Centres. An opt-out procedure was communicated by press release according to national guidelines and the European privacy law.
The cohort consists of hospitalized patients from March 2020 until July 2021 with PCR-confirmed SARS-CoV-2 infection or a highly suspected CT scan-based infection with a CORADS score ≥ 49. Patients that were transferred from another hospital with an initial admission date > 48 h, readmission records and CKD patients with an undefined CKD stage pre-admission were excluded. Seven groups of CKD were defined based on the previously reported medical history of CKD. The pre-admission kidney condition was calculated with CKD-EPI formula10 and the eGFR was used to categorized CKD-stages according to the Kidney Disease Improving Outcomes stages of CKD stages11. Patients without CKD were used as controls (“no-CKD”).
Outcomes and statistical analyses
We compared comorbid risk factors, baseline vitals and laboratory values, and disease severity across groups. Parametric variables were presented as mean and standard deviation (SD); for non-parametric data, the median and interquartile range (IQR) was used. Dichotomous data were presented with frequencies (n) and percentages (%). To compare differences for continuous data, we used a one-way ANOVA or Kruskal–Wallis (KW) test, depending on the type of distribution. If the overall group was deemed significant, posthoc pairwise t-tests (after one-way ANOVA) or Wilcoxon rank tests (after KW) were performed (Benjamini-Hochberg (BH), adjusted) to compare no CKD to the CKD group. For categorical data, we used the Fisher exact test to compare group differences, with pairwise posthoc tests (BH adjusted) with the no CKD group if overall significant. The primary outcome was a composite endpoint of all-cause mortality, readmission or palliative hospital discharge in a 12-week follow-up period. Logistic regression was used to adjust the association between CKD groups and primary outcome in a stepwise procedure for the following confounders: age, sex, ethnicity, number of comorbidities, and designated COVID-19 treatment wave, reflective of the introduction of dexamethasone as a standard treatment regimen12. Overall, < 2% observations were missing, which were entirely considered at random and listwise omitted from the adjusted analyses. A P ≤ 0.05 was considered significant. Data analyses were performed with R (v3.6.1)13.
Results
Risk factors and COVID-19 severity
Of the 5153 hospitalized COVID-19 patients enrolled, 755 were excluded because the admission was a readmission of COVID-19, it concerned a transfer from another hospital or were lossed to follow-up. A total of 247 patients with CKD were excluded due to missing pre-admission creatinine values and incomplete CKD stage information (Supplementary Fig. 1). In the remaining 4151 patients, 389 (9.4%) patients were labeled as CKD patients and 3762 (90.6%) patients as no-CKD patients. At admission, baseline characteristics between groups were significantly different for age, ethnicity, designated treatment wave and prevalence of registered comorbidities (Table 1). There were no significant differences in disease severity on admission as measured with MEWS, qSOFA and CRP levels (Tables 1, 2).
There were multiple significant different vital signs and laboratory values at admission (Table 2). Admission diastolic blood pressure was lower in CKD stage 4 compared to no-CKD, while other vital parameters were not significantly different when comparing CKD groups to No CKD in post-hoc analyses. Hemoglobin levels were significantly lower in all CKD patients compared to no-CKD. Albumin was significantly lower in patients with CKD stage 3b and stage 4. The lymphocyte count and platelet count showed no significant difference between groups in post-hoc analyses. There were several other laboratory differences; a significant decrease of plasma sodium, increase of plasma potassium, lower plasma ALAT and lower pH in some of the CKD groups (Table 2). Most of these mean values were, however, within the normal range.
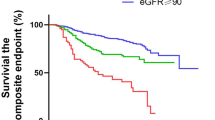
Mortality and readmission rates
A total of 996 patients (24.0%) died or were readmitted after 12 weeks of follow-up. In the unadjusted model, all CKD stages, except CKD stage 5, were associated with significantly higher mortality and readmission rate compared to no-CKD patients (Fig. 1a–c). After adjusting for all confounding covariables, in patients with CKD stage 3a, stage 3b, stage 4 and patients with KTX, odds ratios of death and readmission were significantly different compared to patients without CKD and ranged from 1.96 to 8.94. All CKD patients combined showed a significantly increased unadjusted and adjusted mortality and readmission rate (Supplementary Fig. 2a–c). A subgroup analyses comparing only CKD groups indicated an increased mortality and readmission rate in patients with KTX in the adjusted model. (Supplementary Fig. 3a–c).
(a–c) Unadjusted; age, sex and ethnicity adjusted; and fully adjusted 12-week mortality and readmission odds ratios in patients hospitalized for COVID-19 among CKD groups compared to “no-CKD” with corresponding P values. CKD stage 2 = eGFR 60–79 ml/min/1.73 m2, CKD stage 3a = eGFR 45–59 ml/min/1.73 m2, CKD stage 3b = eGFR 30–44 ml/min/1.73 m2, CKD stage 4 = eGFR 15–29 ml/min/1.73 m2, CKD stage 5 = eGFR < 15 ml/min/1.73 m2, CKD = chronic kidney disease. P is considered significant at P ≤ 0.05.
Complications
We observed differences in the rate of congestive heart failure, anemia requiring transfusion and stroke in various stages of CKD compared to patients without CKD. Also, the self–reported incidence of cognitive decline was higher in patients with CKD stages 2 and 3b (Table 3). All observed differences in complications were not significant in the post-hoc analyses; complications unlikely explained the higher mortality and readmission rate among CKD stages (Table 3).
Discussion
Our multicenter cohort of admitted COVID-19 patients demonstrates overall increased mortality and readmission rates in patients with CKD. We show a strong unadjusted increased clinical mortality and readmission rate in patients with any form of CKD compared to patients without CKD, except for CKD stage 5. After full adjustments, in patients with CKD stages 3a, 3b, 4 and in KTX patients, the odds ratios remain significantly increased compared to patients without CKD. Notably, the odd ratios within CKD groups did not indicate any association with CKD stage severity. We could not identify the main complication responsible for the higher mortality and readmission rate. We also could not identify clear patterns in vital signs or laboratory values at admission that explain increased mortality and readmission rate across CKD groups in our cohort, aside from lower diastolic blood pressure (CKD stage 4) and significant differences in hemoglobin and albumin—the latter being presumably directly related to CKD stage rather than COVID-19. The lack of an apparent factor that explains worse 12-week outcomes underscores that CKD as such is a COVID-19 risk factor.
However, some distinctions can be made, as we also analyzed mortality and readmission rates among CKD patients with dialysis and KTX. Our findings are in concordance with the ERACODA collaborative study, where a higher mortality rate was found among KTX and dialysis patients than data from the general population4. However, in contrast to KTX patients from our cohort, dialysis patients (predominantly hemodialysis) do not appear to have significantly higher mortality and readmission rates after adjusting for known covariates. The significantly higher mortality after correction demonstrates that mortality and readmission rates in the KTX group are not dependent on known COVID-19 risk factors such as older age, male sex and ethnicity14,15. This is in contrast with our findings in dialysis patients in whom the worse 12-week outcomes to some extent seem to be explained by higher age and more prevalent comorbidities associated with worse COVID-19 outcomes in non-renal patients.
It has been suggested that COVID-19 associated mortality in patients with KTX is due to the immunosuppressive condition of patients, which leads to an inability to clear the SARS-CoV-2 infection16. Various studies have also shown a limited yield of SARS-CoV-2 vaccines in patients with a solid transplantation16,17,18. This study again emphasizes the present-day increased risk of mortality in patients with KTX. Besides KTX patients, usage of immune suppressive medication in other CKD groups was not significantly different from the no-CKD group in our cohort.
There are some potential drawbacks associated with our study. First, although we can draw conclusions on the influence of CKD on COVID-19 outcomes, the influence of CKD severity was studied based on eGFR staging only. We were not able to include albuminuria stage, which could affect CKD severity and its association with outcomes. Furthermore, due to requiring pre-admission creatinine values, we have excluded 247 CKD patients. However, we believe this selection provides a more accurate representation of mortality within CKD groups. We also did not study the impact of the primary diagnosis causing CKD on the course of COVID-19 because these data were not completely available. At last, there are differences in baseline characteristics and in designated COVID-19 treatment wave, which might have resulted in different treatment regimens among groups. Although we adjusted for potential confounders, there remains a possibility of an overestimation or underestimation of results. However, we do believe this only makes our results more applicable to general clinical conditions in hospitals.
Conclusion
Our study demonstrates a clinically significant increased mortality and readmission rate in patients with a history of CKD. While previous studies mainly highlighted increased mortality among dialysis and KTX patients, we also demonstrate a clear increased 12-week mortality and readmission rate of SARS-CoV-2 infected patients in nearly all CKD groups. Besides justified concerns for KTX patients, clinicians should also be aware of more severe COVID-19 outcomes and increased vulnerability in CKD patients.
Data availability
The original study protocol and data dictionary will be made available to researchers upon request. Researchers willing to access the de-identified participant dataset should send a request to l.vogt@amsterdamumc.nl. Requests for data will be evaluated, and access will depend on the informed consent and permission of legal research support of Amsterdam UMC.
References
Wiersinga, W. J., Rhodes, A., Cheng, A. C., Peacock, S. J. & Prescott, H. C. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): A review. JAMA J. Am. Med. Assoc. 324, 782–793 (2020).
Eastin, C. & Eastin, T. Clinical characteristics of coronavirus disease 2019 in China. J. Emerg. Med. 58(4), 711–712 (2020).
Gansevoort, R. T. & Hilbrands, L. B. CKD is a key risk factor for COVID-19 mortality. Nat. Rev. Nephrol. 16, 705–706 (2020).
Hilbrands, L. B. et al. COVID-19-related mortality in kidney transplant and dialysis patients: Results of the ERACODA collaboration. Nephrol. Dial. Transplant. 35(11), 1973–1983 (2020).
Ortiz, A. et al. Chronic kidney disease is a key risk factor for severe COVID-19: A call to action by the ERA-edta. Nephrol. Dial. Transplant. 36(1), 87–94 (2021).
Ottenhoff, M. C. et al. Predicting mortality of individual patients with COVID-19: A multicentre Dutch cohort. BMJ Open 11(7), e047347 (2021).
Peters, E. J. et al. Outcomes of persons with coronavirus disease 2019 in hospitals with and without standard treatment with (hydroxy)chloroquine. Clin. Microbiol. Infect. 27(2), 264–268 (2021).
COVIDPredict. COVIDPredict. https://covidpredict.org/en.
Prokop, M. et al. CO-RADS—A categorical CT assessment scheme for patients with suspected COVID-19: Definition and evaluation. Radiology 296(2), E97–E104 (2020).
Pattaro, C. et al. Estimating the glomerular filtration rate in the general population using different equations: effects on classification and association. Nephron Clin Pr. 123(1–2), 102–111 (2013).
CKD Evaluation and Management—KDIGO. Cited 2021 Jul 6. https://kdigo.org/guidelines/ckd-evaluation-and-management/.
The RECOVERY Collaborative. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 384(8), 693–704 (2021).
R Core Team. A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna (2020). https://www.r-project.org/.
Williamson, E. J. et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 584(7821), 430–436. https://doi.org/10.1038/s41586-020-2521-4 (2020).
Velavan, T. P. et al. Host genetic factors determining COVID-19 susceptibility and severity. EBioMedicine 72, 103629 (2021).
Khairallah, P. et al. The impact of COVID-19 on kidney transplantation and the kidney transplant recipient—One year into the pandemic. Transplant. Int. 34, 612–621 (2021).
Benotmane, I. et al. Low immunization rates among kidney transplant recipients who received 2 doses of the mRNA-1273 SARS-CoV-2 vaccine. Kidney Int. 99, 1498–1500 (2021).
Caillard, S. et al. Occurrence of severe Covid-19 in vaccinated transplant patients. Kidney Int. 99, 1498–1500 (2021).
Acknowledgements
We would like to thank the COVIDPredict consortium (www.covidpredict.org) for their efforts in providing patient data.
Funding
This work was supported by Amsterdam UMC and Amsterdam UMC Corona Fund. The following people report grants in the previous 36 months: H. Peters-Sengers report grants of the Dutch Kidney Foundation (KOLFF Grant 19OK009) and W.J. Wiersinga reports a grant from Netherlands Organisation for Health Research and Development (TURN-COVID).
Author information
Authors and Affiliations
Consortia
Contributions
B.A., J.J.O., W.J.W., H.P.-S., L.V.: Conception, design, analysis and interpretation of data. Drafting the article and revising it. Providing intellectual content of critical importance to the work described. Final approval of the version to be published. L.B.: Conception and design. Drafting the article. Providing intellectual content of critical importance to the work described. Final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Appelman, B., Oppelaar, J.J., Broeders, L. et al. Mortality and readmission rates among hospitalized COVID-19 patients with varying stages of chronic kidney disease: a multicenter retrospective cohort. Sci Rep 12, 2258 (2022). https://doi.org/10.1038/s41598-022-06276-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-06276-7
This article is cited by
-
The prognostic value of estimated glomerular filtration rate on admission for death within 30 days among COVID-19 inpatients using fractional polynomial and spline smoothing
International Urology and Nephrology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.