Abstract
HLH syndrome may mimic sepsis but requires entirely different treatment. The aim of the study was to assess the occurrence of HLH features in patients with sepsis and the influence these exert on the patients’ prognosis. The prospective study included 108 patients with suspected sepsis who were routinely evaluated according to HLH criteria. They were divided into group I (SOFA = 2, n = 57) and group II (SOFA ≥ 3, n = 51). Four patients were excluded from analysis: 1 with real HLH, 2 with Still’s disease and 1 with lymphoma. The median (IQR) concentration of ferritin was 613.4 (850.3) ng/mL, however 6 patients revealed a remarkedly high ferritin concentration > 3000 ng/mL, including 2 with ferritin > 10,000 ng/mL. In total, 21 patients met ≥ 4/8 HLH criteria and were found to have sepsis with HLH-like syndrome (SHLS). Out of these, 19 responded to antimicrobials, 2 died due to infection. The sepsis patients presented with the following HLH criteria: fever (95.2%), hyperferritinemia (57.3%), splenomegaly (43.4%), reduced NK cell activity (35.2%), high sCD25 activity (27.4%) and rarely: hypertriglyceridemia (14.4%), duopenia (5.8%), hypofibrinogenemia (1.9%). Although group II patients had higher odds for SHLS presentation (OR 3.26, p = 0.026) and for death (OR 14.3, p = 0.013), SHLS occurrence had no impact on the risk of death (OR 0.77, p = 0.75). Sepsis patients can present with SHLS exclusively due to severe infection. Duopenia, hypertriglyceridemia, hypofibrinogenemia and high level of sCD25 are unusual in sepsis and might indicate real HLH syndrome. Hyperferritinemia, even as high as in real HLH syndrome, can occur in sepsis patients.
Similar content being viewed by others

Introduction
In the course of sepsis, the immune system is activated and its overexpression leads to organ dysfunction. In 2016, a new definition of sepsis based on the SOFA (Sepsis-related Organ Failure Assessment) score was introduced1. Since that time, sepsis has been defined as a life-threatening organ dysfunction caused by a dysregulated host response to infection. Hemophagocytic lymphohistiocytosis (HLH) is a life-threatening condition of a generalized inflammatory response that results from the pathological activation of the immune system2. HLH syndrome can be almost identical to sepsis; therefore, it may contribute to the deaths of patients with an incorrect diagnosis of sepsis3,4. According to its reported incidence, the rate varies from 1 to 10 in 1,000,000 people, but this figure is probably underestimated5,6,7,8. HLH diagnostic criteria have been developed in children and extrapolated to adults, hence their accuracy in the latter seems to be somewhat limited. In adult patients, HLH is mostly secondary, and is caused by three main factors: infections, autoimmune diseases and neoplasms9. Secondary HLH, especially infection-related, almost entirely meets the definition of sepsis, as an abnormal inflammatory syndrome due to infection and leading to organ dysfunction resulting from a “cytokine storm”. Distinguishing the two syndromes is challenging but extremely important, because patients with HLH syndrome require aggressive immunosuppression.
The aim of the study was to assess the occurrence of HLH features in patients with sepsis and the influence these exert on the patients’ prognosis as well as on the assessment of parameters—allowing to differentiate sepsis with HLH features from real HLH syndrome. Moreover, the study concerned the evaluation of ferritin as a marker distinguishing sepsis and real HLH syndrome.
Methods
Our prospective, non-interventional study enrolled patients with suspected sepsis or septic shock over 18 years of age. The patients were hospitalized in the Hospital for Infectious Diseases in Warsaw, in the Department of Adults’ Infectious Diseases specializing in treating severe infections, sepsis and infections of the nervous system, as well as in the Intensive Care Unit intended for unstable, critically ill patients with a similar profile to the one mentioned.
Patients were admitted to our centre from other hospitals in the Mazowieckie voivodship (province), mainly form Internal, Neurological, Neurosurgical Wards and from Emergency Departments.
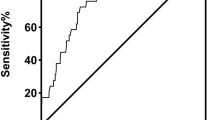
The study was conducted from October 2016 to July 2018. Sepsis was recognized on the basis of organ dysfunction arising from dysregulated host response to infection1. The organ dysfunction was assessed according to the SOFA score amounting to ≥ 2. Infection was defined as potential or microbiologically confirmed. The patients were divided into two groups according to the SOFA score to assess the influence of sepsis severity on HLH feature presentation and the death of the patients: group I with SOFA = 2 and group II with SOFA ≥ 3. The criteria for HLH syndrome were evaluated in all sepsis patients in accordance with the HLH-2004 Diagnostic Protocol established by the Histiocyte Society10. HLH diagnosis is based on the fulfilment of at least 5 out of the 8 criteria listed in Table 1. Given the fact that in the early stage of HLH, patients can present with only 4 out of the 8 criteria, this threshold was found to be appropriate for including patients with HLH features2. Patients with sepsis who presented with HLH features (≥ 4/8) were considered to have sepsis with HLH-like syndrome (SHLS). The patients with SHLS who responded to antimicrobials and showed regression of met HLH criteria had hyperinflammatory reaction and a cytokine storm exclusively due to infection, while those who neither responded to the treatment, nor showed regression of the met HLH criteria—had real HLH syndrome—Fig. 1. The latter patients were enrolled for bone marrow aspiration. The presentation of HLH features due to sepsis (SHLS) or the death of the patients were clinical endpoints.
Material blood was drawn for basic laboratory tests directly after admission—Table 2. Activity of sCD25 was tested by enzyme-linked immunosorbent assay (ALPCO, Human Soluble Interleukin-2 Receptor, sIL-2R ELISA). To determine NK cell activity, lymphocytes were isolated from the patients and incubated with human erythrocytic leukaemia cells and then the NK cells were introduced into a flow cytofluorimeter (FACSCalibur, Beckton-Dickinson). Normal NK cell level: 6–18%. Normal NK cells activity: 4–15%. Additionally, an abdomen ultrasound was performed on the first working day to assess the spleen and liver size.
Statistical analysis
Group comparison was analysed with a non-parametric test (Mann–Whitney U test) and a parametric test (T-St udent test), depending on the data normality distribution (Shapiro–Wilk test). To assess the statistical significance between the qualitative variables, the Chi2 test was used. Logistic regression analysis was performed to determine factors influencing the occurrence of the clinical endpoints (presentation of the HLH features exclusively due to sepsis or the death of the patients). The level of statistical significance was determined with the value of p < 0.05. All the analyses were performed using Statistica version 13.3, StatSoft, with a medical add-on.
Bioethical issues
We confirm that all the experimental protocols were approved by the Bioethical Committee of the Medical University of Warsaw, No. KB/180/2016 of 06.09.2016. We confirm that informed consent was obtained from all participants, as well as that all research was performed in accordance with relevant guidelines and regulations.
Results
The study group consisted of 108 patients, in group I (SOFA = 2) there were 57 patients (52.8%), while in group II (SOFA ≥ 3) 51 patients (47.2%). Despite initially suspected sepsis, 4 patients (3.7%) from group I were eventually diagnosed with another disease and excluded from the analysis. These were: a 56-year-old male with real HLH syndrome (6 HLH criteria, ferritin 1,927 ng/mL, SOFA = 2) who was referred to the Haematological Department, a 59-year-old female and a 22-year-old male with adult-onset Still’s disease—AOSD (4 HLH criteria, ferritin 97,221 ng/mL, SOFA = 2 and 3 HLH criteria, ferritin 3983 ng/mL, SOFA = 2) who were eventually referred to the Rheumatological Department. The fourth patient presented with an advanced neoplasm (lymphoma) and was disqualified from chemotherapy. He died due to infection (male, 58 years old, 4 HLH criteria, ferritin 11,385 ng/mL, SOFA = 2).
In the studied group, sepsis was a result of the following infections (one or more): pneumonia (n = 29), bacterial meningitis and brain abscesses (n = 27), skin and subcutaneous tissue infections (n = 17), gastrointestinal infections (n = 16), urinary tract infections (n = 10), spondylodiscitis (n = 4), infective endocarditis (n = 3), malaria/dengue fever (n = 3), HIV-related infections (n = 3).
Occurrence of HLH features in sepsis
In the sepsis patients, the median Md (interquartile range, IQR) ferritin concentration was 613.4 (850.3) ng/mL, however, 6 sepsis patients presented with a remarkably high ferritin concentration, including 4 with results in the range of 3000–10,000 ng/mL, and 2 with hyperferritinemia 17,725 and 17,284 ng/mL. The most common HLH criteria presented by the patients with sepsis were: fever (95.2%), hyperferritinemia (57.3%) and splenomegaly (43.4%). Every third patient had reduced NK lymphocyte activity (35.2%) and high sCD25 activity (27.4%). Hypertriglyceridemia, duopenia and hypofibrinogenemia were rarely observed, with a frequency of 14.4%, 5.8% and 1.9%, respectively—Table 3.
As many as every fifth patient with sepsis (n = 21, 20.2%) presented with SHLS. Most of these patients (n = 19/21) responded to antimicrobials (n = 6/19 received also steroids), nevertheless, the remaining 2 patients died—Fig. 1. Those who died showed a typical course of severe infection with evident regression of HLH criteria and/or their parameters and initially met only a borderline number of HLH criteria, namely 4. They did not receive steroids.
The severity of sepsis, i.e. belonging to group I or II, had an impact on the presentation of the HLH features (SHLS). The patients in group II showed SHLS 2.5-times more often (n = 15 vs. n = 6, p = 0.02) and had 3.3-fold higher odds (p = 0.026) of revealing SHLS than group I patients—Tables 3, 4. Furthermore, it was found that among the qualitative variables, all HLH criteria but hypofibrinogenemia were strongly related to SHLS presentation. Out of the quantitative variables, triglycerides and sCD25 were found to be independent predictors of SHLS occurrence (OR 2.93, p = 0.002 and OR 1.001, p = 0.008, respectively)—Table 4.
Factors influencing death
A difference was also found between group I and group II patients with respect to the number of deaths. In group I, only 1 patient died, while in group II as many as 11 (p = 0.002) passed away—Table 3. The odds of death in group II were 14 times higher than in group I, p = 0.01. Moreover, belonging to group II was found to be an independent predictor of death (OR 11.2, p = 0.02)—Table 5. In the entire study group, variables related to the risk of death were: SOFA score as well as lactic acid, fibrinogen, TIBC and lactate dehydrogenase (LDH). Lactic acid was the only parameter from the current definition of sepsis which increased the probability of death in a statistically significant way. In multivariate regression, the SOFA score and LDH had a significant impact on the occurrence of death. Mortality was not affected by the SHLS presentation—Table 5.
In total, 30 patients were given steroids in addition to antibiotics. Those patients had bacterial meningitis (dexamethasone 32–40 mg/d, n = 24), septic shock or allergic reaction (hydrocortisone 100–200 mg/d, n = 6). The use of steroids had no influence either on the occurrence of death (p = 0.72), or on the presentation of HLH features (≥ 4 and ≥ 5; p = 0.98 and p = 0.85). Moreover, no relationship between steroid use and patient death was found in sepsis and SHLS subgroups (p = 0.41 and p = 0.37).
Discussion
In the study conducted, routine assessment of HLH criteria in all the patients with sepsis made it possible to identify 1 patient with real HLH syndrome (n = 1/108). The aim of the study was not to assess the occurrence of real HLH syndrome—the study group was too small and included patients with sepsis—so a single case of HLH does not affect epidemiology. However, results significantly different from the global epidemiological data were also obtained in the 3rd degree reference centre of Mayo Clinic, where routine diagnostics of HLH syndrome was introduced in all the patients with a systemic inflammatory syndrome, finding that its incidence could reach the level of 1 in 2000 of the patients admitted11. The results, therefore, showed that HLH syndrome is not as rare as it seemed, so it is rational to make HLH assessment on a routine basis in all patients with inflammatory syndromes, particularly with sepsis.
Evaluation of HLH parameters was based on the classic diagnostic criteria. Novel parameters characteristic for HLH syndrome, such as cytokine IL-18 and interferon gamma were not included. We attempted to find diagnostic hints in widely available, basic HLH criteria, allowing to distinguish SHLS and real HLH. One of the main parameters in the differential diagnosis of sepsis and HLH syndrome is ferritin. The sepsis patients commonly presented with ferritin concentration exceeding the cut-off point for HLH syndrome, namely 500 ng/ml. In our study median, ferritin was 613.4 (850.3) ng/mL and two patients revealed as high a concentration as 17,725 and 17,284 ng/mL, i.e. values typical for patients with HLH syndrome. In an ICU study involving patients with HLH syndrome, it was found that median ferritin was 17,728 (7689–37,981) µg/L12. Furthermore, in an another study, a maximum ferritin value of 9083 µg/L was at 92.5% sensitivity and 91.9% specificity for hemophagocytic lymphohistiocytosis in adult critically ill patients13. Our results indicate that even extreme hyperferritinemia can occur in sepsis and the value of this parameter in HLH recognition seems to be limited.
Complex assessment of HLH criteria revealed that even every fifth patient with sepsis presented with HLH features (SHLS) in the course of severe infection—Table 3. This may indicate the coexistence of real HLH in sepsis or the independent similarity of the pathomechanisms of both syndromes. Studies describing the relationship of sepsis and HLH syndrome are not numerous and usually concern selective aspects of the similarities of both syndromes. It was found that an occurrence of some HLH features in sepsis patients is associated with a higher percentage of multiorgan failure and death3,14,15,16. Furthermore, hemophagocytosis in bone marrow, a typical feature of HLH syndrome, might occur in patients with sepsis and multiorgan failure17. In our group of patients, a strong correlation was found between the severity of organ dysfunction (SOFA score) and the number of HLH criteria met, while the relationship between the number of HLH criteria and patient death was not proven—Tables 4, 5. Our patients improved on antimicrobial treatment, which supports the thesis that SHLS results from severe infection, or on the other hand that sepsis-related HLH is self-limiting. Certainly, patients with SHLS—despite the response to antimicrobials frequently observed in the group we examined—require thorough monitoring and regular check-ups for the occurrence of real HLH syndrome.
Therefore, the key question seems to be whether it is possible to distinguish SHLS and real HLH syndrome in their early stage on the basis of characteristic laboratory deviations.
The results obtained in our group of sepsis patients were compared with the results of patients with real HLH syndrome from other studies18,19,20,21,22—Table 6.
When comparing the frequency of particular criteria in our sepsis patients and in patients with real HLH syndrome, it can be seen that the most common deviations in both groups are hyperferritinemia and organomegaly. The decreased NK lymphocyte activity seems to be somewhat similar in both syndromes. The high activity of sCD25, characteristic for patients with HLH syndrome (77–100%), was found only in 27% of the patients with sepsis. Our results are in line with those obtained by Hayden et al.22. They observed sCD25 > 2400 U/ml only in 37.5% of the patients with non-HLH conditions, including sepsis, while in 100% of the patients with real HLH. Moreover, the authors concluded that 2515 U/ml is the optimal cut-off for sCD25 for HLH patients (100% sensitivity and 72.5% specificity) and that sCD25 > 10,000 U/mL has 93% specificity for ruling in HLH. In our study, no one with SHLS reached the level of sCD25 ≥ 10,000 U/ml, nevertheless 13 patients exceeded 3000 U/ml; 3 patients reached the level of 5000 U/ml and the maximal sCD25 in SHLS was 9307.3 U/ml. The diagnostic utility of sCD25 is particularly visible in malignancy-associated hemophagocytic syndrome, where the superiority of this parameter over ferritin is significantly manifested22.
The main differences in the presentation of both conditions relate to the following parameters: bi-/pancytopenia, hypertriglyceridemia and hypofibrinogenemia. They are common in HLH syndrome and occur in 85–92%, 65–87% and 38–75% of the cases, respectively, while they are rare in sepsis, i.e. they are observed only in 5.8%, 14.4% and 1.9% of the patients, respectively. A clear difference also applies to sCD25, which is a typical HLH parameter less common in sepsis patients—Table 6.
Debaugnies et al. noticed that the main parameters influencing the occurrence of real HLH syndrome are: cytopenia of 3-cell lines (OR 14.8), hypofibrinogenemia (OR 13.5), hypertriglyceridemia > 4 mmol/L (OR 9.6), ferritinemia > 6000 ng/mL (OR 5.8), organomegaly (OR 5.8)23. Pham et al. concluded that the following factors have the most significant impact on the occurrence of HLH syndrome: increased ferritin (OR 36), thrombocytopenia (OR 15), duopenia (OR 8)24. In our sepsis patients, similar qualitative variables influenced SHLS presentation in univariate logistic analysis, while in multivariate analysis only triglycerides and sCD25 were found to be independent predictors of SHLS occurrence—Table 4.
Given these considerations, uncommon in sepsis disorders, namely duopenia, hypertriglyceridemia and/or hypofibrinogenemia might be early indicators of developing real HLH syndrome in patients with sepsis and SHLS. A similar observation regarding duo/pancytopenia was made by Kapoor et al., who found this deviation a potential feature of HLH in patients with septic shock and multi organ failure syndrome, not responding to the standard treatment protocols12.
Castillo et al. put forward the thesis that infection-associated HLH does not represent a separate entity, but falls within the final spectrum of inflammatory response to sepsis25. Both conditions share a similar pathophysiology, which creates difficulties in setting a clear border between them. HLH and sepsis are probably a continuum of the same inflammatory reaction25. The key question remains at what moment the patient with SHLS can benefit from immunosuppressive therapy. In the light of the results obtained, it seems that the main argument for the initiation of aggressive immunosuppressive treatment in patients with SHLS is the lack of response to antibiotic therapy supported by the occurrence of the characteristic laboratory differences that were revealed.
The study has limitations. The study group was not numerous, the use of steroids could have interfered both HLH occurrence and the influence of SHLS on the patients’ prognosis, however, on the other hand the study was prospective, patients were enrolled and evaluated according to strictly defined criteria and none of the statistically significant correlations was found between steroid use and the above-mentioned variables. Moreover, the study features advantages in the form of clearly selected sepsis patients with HLH features assessed at an acute phase of the infection, which allowed us to find specific differences in laboratory parameters between sepsis and HLH syndrome.
Conclusions
Every fifth patient with sepsis presents with HLH features, which mainly result from severe infection, as evidenced by a response to antibiotic therapy and regression of HLH criteria.
Duopenia, hypertriglyceridemia, hypofibrinogenemia and high level of sCD25 are uncommon in sepsis and may indicate the HLH syndrome.
Hyperferritinemia occurs in patients with sepsis and is thereby of limited value in differentiating the two syndromes.
HLH and sepsis are a continuum and development of better diagnostic tools is needed in their diagnosis.
References
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315, 801–810. https://doi.org/10.1001/jama.2016.0287 (2016).
Janka, G. E. & Lehmberg, K. Hemophagocytic syndromes—an update. Blood Rev. 28, 135–142. https://doi.org/10.1016/j.blre.2014.03.002 (2014).
Raschke, R. A. & Garcia-Orr, R. Hemophagocytic lymphohistiocytosis: a potentially underrecognized association with systemic inflammatory response syndrome, severe sepsis, and septic shock in adults. Chest 140, 933–938. https://doi.org/10.1378/chest.11-0619 (2011).
Demirkol, D. et al. Hyperferritinemia in the critically ill child with secondary hemophagocytic lymphohistiocytosis/sepsis/multiple organ dysfunction syndrome/macrophage activation syndrome: what is the treatment?. Crit. Care (London, England) 16, R52. https://doi.org/10.1186/cc11256 (2012).
Arico, M., Danesino, C., Pende, D. & Moretta, L. Pathogenesis of haemophagocytic lymphohistiocytosis. Br. J. Haematol. 114, 761–769 (2001).
Henter, J. I., Elinder, G., Soder, O. & Ost, A. Incidence in Sweden and clinical features of familial hemophagocytic lymphohistiocytosis. Acta Paediatr. Scand. 80, 428–435 (1991).
Niece, J. A., Rogers, Z. R., Ahmad, N., Langevin, A. M. & McClain, K. L. Hemophagocytic lymphohistiocytosis in Texas: observations on ethnicity and race. Pediatr. Blood Cancer 54, 424–428. https://doi.org/10.1002/pbc.22359 (2010).
Machaczka, M., Vaktnas, J., Klimkowska, M. & Hagglund, H. Malignancy-associated hemophagocytic lymphohistiocytosis in adults: a retrospective population-based analysis from a single center. Leuk. Lymphoma 52, 613–619. https://doi.org/10.3109/10428194.2010.551153 (2011).
Ramos-Casals, M., Brito-Zeron, P., Lopez-Guillermo, A., Khamashta, M. A. & Bosch, X. Adult haemophagocytic syndrome. Lancet (London, England) 383, 1503–1516. https://doi.org/10.1016/s0140-6736(13)61048-x (2014).
Henter, J. I. et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr. Blood Cancer 48, 124–131. https://doi.org/10.1002/pbc.21039 (2007).
Parikh, S. A., Kapoor, P., Letendre, L., Kumar, S. & Wolanskyj, A. P. Prognostic factors and outcomes of adults with hemophagocytic lymphohistiocytosis. Mayo Clin. Proc. 89, 484–492. https://doi.org/10.1016/j.mayocp.2013.12.012 (2014).
Kapoor, S., Morgan, C. K., Siddique, M. A. & Guntupalli, K. K. Intensive care unit complications and outcomes of adult patients with hemophagocytic lymphohistiocytosis: a retrospective study of 16 cases. World J. Crit. Care Med. 7, 73–83. https://doi.org/10.5492/wjccm.v7.i6.73 (2018).
Lachmann, G. et al. Hyperferritinemia in critically Ill patients. Crit. Care Med. 48, 459–465. https://doi.org/10.1097/ccm.0000000000004131 (2020).
To, K. K. et al. Delayed clearance of viral load and marked cytokine activation in severe cases of pandemic H1N1 2009 influenza virus infection. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 50, 850–859. https://doi.org/10.1086/650581 (2010).
Henter, J. I., Chow, C. B., Leung, C. W. & Lau, Y. L. Cytotoxic therapy for severe avian influenza A (H5N1) infection. Lancet (London, England) 367, 870–873. https://doi.org/10.1016/s0140-6736(06)68232-9 (2006).
Moller, H. J. et al. Macrophage serum markers in pneumococcal bacteremia: prediction of survival by soluble CD163. Crit. Care Med. 34, 2561–2566. https://doi.org/10.1097/01.ccm.0000239120.32490.ab (2006).
Strauss, R. et al. Multifactorial risk analysis of bone marrow histiocytic hyperplasia with hemophagocytosis in critically ill medical patients–a postmortem clinicopathologic analysis. Crit. Care Med. 32, 1316–1321 (2004).
Li, J. et al. Hemophagocytic lymphohistiocytosis: clinical analysis of 103 adult patients. Medicine 93, 100–105. https://doi.org/10.1097/MD.0000000000000022 (2014).
Otrock, Z. K. & Eby, C. S. Clinical characteristics, prognostic factors, and outcomes of adult patients with hemophagocytic lymphohistiocytosis. Am. J. Hematol. 90, 220–224. https://doi.org/10.1002/ajh.23911 (2015).
Hejblum, G. et al. A web-based delphi study for eliciting helpful criteria in the positive diagnosis of hemophagocytic syndrome in adult patients. PLoS ONE 9, e94024. https://doi.org/10.1371/journal.pone.0094024 (2014).
Bergsten, E. et al. Confirmed efficacy of etoposide and dexamethasone in HLH treatment: long-term results of the cooperative HLH-2004 study. Blood 130, 2728–2738. https://doi.org/10.1182/blood-2017-06-788349 (2017).
Hayden, A. et al. Soluble interleukin-2 receptor is a sensitive diagnostic test in adult HLH. Blood Adv. 1, 2529–2534. https://doi.org/10.1182/bloodadvances.2017012310 (2017).
Debaugnies, F. et al. Performances of the H-score for diagnosis of hemophagocytic lymphohistiocytosis in adult and pediatric patients. Am. J. Clin. Pathol. 145, 862–870. https://doi.org/10.1093/ajcp/aqw076 (2016).
Pham, A. Q. et al. Analysis of serum ferritin levels as a diagnostic criteria for hemophagocytic lymphohistiocytosis (HLH) in hospitalized adult patients. Blood 126, 1014–1014 (2015).
Castillo, L. & Carcillo, J. Secondary hemophagocytic lymphohistiocytosis and severe sepsis/ systemic inflammatory response syndrome/multiorgan dysfunction syndrome/macrophage activation syndrome share common intermediate phenotypes on a spectrum of inflammation. Pediatr. Crit. Care Med. J. Soc. Crit. Care Med. World Fed. Pediatr. Intensive Crit. Care Soc. 10, 387–392. https://doi.org/10.1097/PCC.0b013e3181a1ae08 (2009).
Acknowledgements
The study was supported by Fundacja Rozwoju Nauki w Wojewódzkim Szpitalu Zakaźnym (Foundation for the Development of Infectious Diseases at the Hospital for Infectious Diseases in Warsaw).
Author information
Authors and Affiliations
Contributions
D.B. designed the research, performed statistical analysis and wrote the main manuscript text. A.B. revised and proofread the manuscript. A.P, M.P discussed the data and provided constructive suggestions. A.H. supervised the study and provided constructive suggestions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bursa, D., Bednarska, A., Pihowicz, A. et al. Analysis of the occurrence of hemophagocytic lymphohistiocytosis (HLH) features in patients with sepsis: a prospective study. Sci Rep 11, 10529 (2021). https://doi.org/10.1038/s41598-021-90046-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-90046-4
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.