Abstract
This study designed to evaluate the effect of nutraceutical supplementation on pain intensity and physical function in patients with knee/hip OA. The MEDLINE, Web of Science, Cochrane Library, Scopus, EMBASE, Google Scholar, Science direct, and ProQuest in addition to SID, Magiran, and Iranmedex were searched up to March 2020. Records (n = 465) were screened via the PICOS criteria: participants were patients with hip or knee OA; intervention was different nutritional supplements; comparator was any comparator; the outcome was pain intensity (Visual analogue scale [VAS]) and physical function (Western Ontario and McMaster Universities Arthritis [WOMAC] index); study type was randomized controlled trials. The random effects model was used to pool the calculated effect sizes. The standardized mean difference (SMD) of the outcome changes was considered as the effect size. The random effects model was used to combine the effect sizes. Heterogeneity between studies was assessed by Cochran's (Q) and I2 statistics. A total of 42 RCTs were involved in the meta-analysis. Nutritional supplementation were found to improve total WOMAC index (SMD = − 0.23, 95% CI − 0.37 to − 0.08), WOMAC pain (SMD = − 0.36, 95% CI − 0.62 to − 0.10) and WOMAC stiffness (SMD = − 0.47, 95% CI − 0.71 to − 0.23) subscales and VAS (SMD = − 0.79, 95% CI − 1.05 to − 0.05). Results of subgroup analysis according to the supplementation duration showed that the pooled effect size in studies with < 10 months, 10–20 months and > 20 months supplementation duration were 0.05, 0.27, and 0.36, respectively for WOMAC total score, 0.14, 0.55 and 0.05, respectively for WOAMC pain subscale, 0.59, 0.47 and 0.41, respectively for WOMAC stiffness subscale, 0.05, 0.57 and 0.53, respectively for WOMAC physical function subscale and 0.65, 0.99 and 0.12, respectively for VAS pain. The result suggested that nutraceutical supplementation of patients with knee/hip OA may lead to an improvement in pain intensity and physical function.
Similar content being viewed by others
Introduction
Osteoarthritis (OA) as a degenerative chronic joint cartilage disorder is the most prevalent and principal reason for joint pain and functional impairment in the world1. OA is more prevalent in older adults and it will inflict incredible economic and societal charges and disturb life quality in different aspects subsequently in the future2. On the other hand, discomfort, pain and decreases in functional ability because of OA can consequence a greater risk of overweight/obesity, diabetes mellitus and falls and fractures3. Issues that chip into the development of OA consist of general factors (age, sex, overweight/obesity and nutrition) and local biomechanical factors (joint injury, physical activities and joint space)4.
Existing recommendations for the management of OA consist of three major classes: pharmacologic (i.e. opioids, non-steroidal anti-inflammatory drugs (NSAID), and COX-2 specific drugs), non-pharmacologic (i.e. rehabilitation to facilitate healthy body composition, lifestyle, and physical activity) and surgical treatment4,5,6,7. Present pharmacological treatments simply have a palliative effect on the relief of symptoms whereas not considering the essential problem of the cartilage disorder. Additionally, long-term consumption of these treatments has possible adverse events that might result drastic outcomes such as gastrointestinal problems, unwanted cardiovascular effects and adverse events on the cartilage8. Meanwhile, nutritional intervention demonstrates a continuing approach for management and inhibiting OA as an accompaniment to the traditional treatment of OA9,10,11,12. Nutraceutical supplements, such as chondroitin sulfate (CS), glucosamine sulfate (GS) and Methylsulfonylmethane (MSM), have been applied to manage OA and relieve symptoms in recent years13. Nutraceuticals are described as dietary supplements that comprise a condensed form of a considered bioactive ingredient, initially isolated from food, however existing in a nonfood matrix, and consumed to preserve or increase health situation in the amounts beyond those accessible from common foods13. Nevertheless, there is no agreement in regard to applying the term “nutraceutical” or “dietary supplement”. The “active aging” is a principle objective of dietary supplements, as indicated by the developing sales of vitamins and minerals14. Dietary bioactive combinations have been revealed to be impressive in the improvement of clinical symptoms and in decreasing inflammatory indices in subjects with OA15. Presently 69% of subjects with OA receive various forms of dietary supplements for their problem16.
Even though there are several publications in the medical literature in regard to the use of nutraceuticals as a complementary treatment of OA, there have been variable findings concerning whether or not these nutrients have any beneficial consequence. The purpose of this study is to perform a systematic review and meta-analysis of relevant randomized controlled trials (RCTs) to assess the efficiency of different dietary supplements in the management of the symptoms of hip/knee OA.
Methods
The primary purpose of this systematic review and meta-analysis was to evaluate the efficacy and safety of dietary supplements in subjects with knee or hip OA. The current study has been planned based on the instructions in the Cochrane Collaboration handbook and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. The study question was framed according to the PICOS (participants, interventions, comparators, outcomes, study design) criteria (Table 1), is as follows: Do nutraceutical supplements influence pain and functional status in patients with hip/knee osteoarthritis?
Literature search
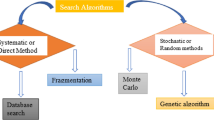
Several search strategies were employed to recognize eligible studies. A medical librarian (FB) in an argument with the team (DA, ND and FB) performed a precise and comprehensive academic literature search of the titles, abstracts and keywords of all studies for competency independently through electronic databases (MEDLINE, Web of Science, Cochrane Library, Scopus, EMBASE, Google Scholar, Clininaltrial.gov, Science direct, and ProQuest in addition to SID, Magiran, Irandoc, and Iranmedex for Persian language literature) up to January 2020. Duplicate studies were excluded. At the same time, a hand search of the related references and cited articles of the included studies was conducted to recognize other appropriate studies that were lost by electronic search.
Search terms included a mix of Medical Subject Headings (MeSH) and a literature search was performed using the following MeSH terms for key concepts (with assistance from a librarian) targeting dietary supplements and hip or knee OA such as : (“supplement ”(All Fields) OR “nutraceuticals”(All Fields) OR “vitamin”(All Fields) OR “mineral”(All Fields) OR “plant”(All Fields)) AND (“OA” OR “osteoarthritis”(All Fields) OR “knee osteoarthritis”(All Fields) OR “hip osteoarthritis”(All Fields) OR “knee OA”(All Fields) OR “hip OA”(All Fields)). After the primary search, titles and abstracts were sent out from EndNote X7 into Microsoft Excel to be screened. Three reviewers separately reviewed all titles and abstracts and full texts (DA, ND, and MH). A fourth reviewer was conferred if discrepancies happened.
Inclusion and exclusion criteria
Inclusion criteria to choose studies for this systematic review and meta-analysis were: (1) RCT (either parallel or crossover designs); (2) a nutraceutical as an intervention either as an adjunctive to standard medicine or as a monotherapy and (3) adults who have been diagnosed with hip or knee OA; (4) sufficient data reported about mean changes for Western Ontario and McMaster Universities Arthritis (WOMAC) index (total score and subscales) and/or Visual analogue scale (VAS) at baseline and at the end of the trial in both intervention and placebo/control groups. Then selected possible clinical trials were excluded based on the exclusion criteria as follows: (1) duplications; (2) subjects have other critical diseases such cardiovascular disease, cancer, diabetes, etc.; (3) Studies with a short period of follow‐up (< 2 weeks); (4) review articles, semi-experimental studies without a control arm, animal studies, study protocols, letter to editors, case reports, case series, observational studies (cross-sectional, case–control and cohort) and unpublished trials.
No language limitations were applied to the search, but only studies published in English or Persian were incorporated because of translation constraints. Trials without full text and those that couldn’t attain the minimum quality appraisement score were not included in this systematic review.
Quality and risk-of-bias assessment
To estimate the risk of systematic errors in the all involved clinical trials, two authors (ND and FB) individually evaluated the risk of bias according to the Cochrane Collaboration consists of the subsequent domains: “randomization sequence generation, allocation concealment, blinding of subjects, personal, and outcome assessment, incomplete outcome data, and selective outcome reporting, as well as other sources of bias”. Incompatibilities between reviewers, were resolved by the fourth author (MH). All studies were judged for each series of bias separately, and the studies were decided to take a score of bias as “low risk”, “high risk”, or “unclear risk” if data was inadequate.
Data extraction
One reviewer extracted the data and abstracted it into an electronic form designed for this review, and a second reviewer confirmed it. Information extracted included: the first author’s name, publication details, location of the study, inclusion and exclusion criteria; the number of subjects for intervention and placebo groups, type of intervention, study design and duration, the mean and standard deviation (SD) for VAS and WOMAC index at baseline and at the end of the intervention in both intervention and control groups and safety.
The outcome measures
The studies that met inclusion criteria were reviewed and the outcomes of these RCTs that could be retained for meta-analysis were considered as the primary outcome in this review. Thereupon, the primary outcome measures included for this review were mean changes in WOMAC total, WOMAC pain, WOMAC stiffness, WOMAC physical function and pain (VAS).
Data synthesis and analysis
The number of subjects in each intervention group with mean and SD of study outcomes before and after the intervention was extracted from the articles included in the study. Then, the mean difference of study outcome was calculated and the mean difference of study outcomes was compared between the two groups. Because of the different scales used in the articles included in the study for the WOMAC index and VAS, the standardized mean difference (SMD) of the outcome changes between the two groups was considered as the effect size in this study. The random effects model was used to combine the effect sizes calculated in the articles. Heterogeneity between studies was assessed by Cochran's (Q) and I2 statistics, which expressed the percentage of variations between studies. In case of high heterogeneity between included studies, we performed subgroup analysis according to the treatment duration (< 10 months, 10–20 months and > 20 months) to evaluate the impression of these factors on the results. The Meta package in R software was used for data analysis. A p-value less than 0.05 was considered as significant level.
Publication bias
Egger's Regression Test and Funnel Plot were used to evaluate the presence or absence of publication bias. Publication bias was assessed for each study outcome. The Trim and Fill method was used to investigate the effect of publication bias on the results of the study.
Results
Study selection process
The systematic searching of the databases identified 1323 articles, of which 858 were excluded as duplicates, 372 were excluded by title and abstract and 52 were excluded after reviewing full texts (Fig. 1).
Study characteristics
This comprehensive systematic review and meta-analysis including 42 RCTs (4160 participants) and 33 supplements assessed the clinical effectiveness of different nutraceutical supplementation in the management of knee/hip OA symptoms, principally concentrating on pain and functional outcomes. The included articles in this systematic review were full articles published from January 2000 to March 2020. Papers were written in English or Persian. The details of the studies are summarized in Table 2.
Risk of bias in included studies
The methodological quality according to the researchers’ decisions on each risk of bias point for each included study is shown in Figs. 2 and 3.
Efficacy of the intervention
WOMAC (total)
The total score of the WOMAC was evaluated in the 28 articles reviewed. There were 1404 cases in the intervention group and 1360 in the control group. The mean follow-up duration of patients (lowest to maximum) was 17.4 (6–144) weeks. There was a significant heterogeneity between studies (Q-value = 110.58, df = 37, p-value < 0.001, I2 = 66.5%). Based on the meta-analysis results, it was observed that the Pooled Standardized Mean Difference between the intervention and control groups was 0.23 units (SMD = − 0.23, 95% CI − 0.37 to − 0.08, z-value = − 3.09, p-value = 0.002). Figure 4 shows the forest plot of the combination of results. Results of subgroup analysis according to the supplementation duration showed that the pooled effect size in studies with < 10 months as short term, 10–20 months as medium term and > 20 months as long term supplementation duration were 0.05, 0.27 and 0.36, respectively. Figure 5 shows the forest plot of the subgroups by the supplementation duration.
WOMAC (pain)
In the included articles, 30 articles evaluated the WOMAC pain subscale. There were 1715 subjects in the intervention group and 1665 subjects in the control group. The mean follow-up duration of patients (lowest to maximum) was 16.82 (3–144) weeks. There was a significant heterogeneity between studies (Q-value = 485.41, df = 40, p-value < 0.001, I2 = 92.2%). The Pooled Standardized Mean Difference between the intervention and control groups was 0.36 units (SMD = − 0.37, 95% CI − 0.63 to − 0.11, z-value = − 2.75, p-value = 0.006). The forest plot of the combination of results is presented in Fig. 6. The pooled effect size in studies with < 10 months as short term, 10–20 months as medium term and > 20 months as long term supplementation duration were 0.14, 0.55 and 0.05, respectively. The forest plot of the subgroups by the supplementation duration is presented in Fig. 7.
WOMAC (stiffness)
In the included articles, 29 articles assessed the WOMAC Stiffness subscale. There were 1539 subjects in the intervention group and 1513 subjects in the control group. The mean follow-up duration of patients (lowest to maximum) was 17.76 (3–144) weeks. There was a significant heterogeneity between studies (Q-value = 353.55, df = 38, p-value < 0.001, I2 = 88.8%). The Pooled Standardized Mean Difference between the intervention and control groups was 0.48 units (SMD = − 0.48, 95% CI − 0.72 to − 0.24, z-value = − 2.88, p-value < 0.001). The forest plot of the combination of results is presented in Fig. 8. The pooled effect size in studies with < 10 months as short term, 10–20 months as medium term and > 20 months as long term supplementation duration were 0.59, 0.47 and 0.41, respectively. The forest plot of the subgroups by the supplementation duration is presented in Fig. 9.
WOMAC (physical function)
In the included articles, 29 articles assessed the WOMAC Physical Function subscale. There were 1496 subjects in the intervention group and 1494 subjects in the control group. The mean follow-up duration of patients (lowest to maximum) was 7.21 (3–144) weeks. There was a significant heterogeneity between studies (Q-value = 583.74, df = 37, p-value < 0.001, I2 = 94.0%) The Pooled Standardized Mean Difference between the intervention and control groups was 0.25 units (SMD = − 0.25, 95% CI − 0.57 to − 0.07, z-value = − 1.55, p-value = 0.12). The forest plot of the combination of results is presented in Fig. 10. The pooled effect size in studies with < 10 months as short term, 10–20 months as medium term and > 20 months as long term supplementation duration were 0.05, 0.57 and 0.53, respectively. The forest plot of the subgroups by the supplementation duration is presented in Fig. 11.
Pain (VAS)
In the included articles, 23 articles assessed the VAS. There were 1081 subjects in the intervention group and 1072 subjects in the control group. The mean follow-up duration of patients (lowest to maximum) was 15.35 (2–96) weeks. There was a significant heterogeneity between studies (Q-value = 246.05, df = 30, p-value < 0.001, I2 = 86.5%). The Pooled Standardized Mean Difference between the intervention and control groups was 0.79 units (SMD = − 0.79, 95% CI − 1.06 to − 0.52, z-value = − 5.77, p-value < 0.001). The forest plot of the combination of results is presented in Fig. 12. The pooled effect size in studies with < 10 months as short term, 10–20 months as medium term and > 20 months as long term supplementation duration were 0.65, 0.99 and 0.12, respectively. The forest plot of the subgroups by the supplementation duration is presented in Fig. 13.
Publication bias for WOMAC index total score
Figure 14 illustrates a Funnel Plot to investigate the publication bias for the WOMAC index total score. According to Eggers Regression Test, the publication bias was not significant (t-value = 1.51, df = 36, p-value = 0.13).
Publication bias for WOMAC index pain subscale
Figure 15 illustrates a Funnel Plot to investigate the publication bias for the WOMAC index pain subscale. According to Eggers Regression Test, the publication bias was not significant (t-value = − 0.42, df = 39, p-value = 0.67).
Publication bias for WOMAC index stiffness subscale
Figure 16 illustrates a Funnel Plot to investigate the publication bias for the WOMAC index stiffness subscale. According to Eggers Regression Test, the publication bias was significant (t-value = − 2.13, df = 37, p-value = 0.03). Trim and Fill test was performed to modify the publication bias and 11 studies added to adjust for the missed study through this method. The results of the Trim and Fill test demonstrate that the pooled effect size was 0.08 (Adjusted SMD = 0.08, 95% CI − 0.33 to − 0.16).
Publication bias for WOMAC index physical function subscale
Figure 17 illustrates a Funnel Plot to investigate the publication bias for the WOMAC index physical function subscale. According to Eggers Regression Test, the publication bias was not significant (t-value = − 0.41, df = 39, p-value = 0.68).
Publication bias for VAS
Figure 18 illustrates a Funnel Plot to investigate the publication bias for the VAS. According to Eggers Regression Test, the publication bias was significant (t-value = − 3.03, df = 29, p-value = 0.004). Trim and Fill test was performed to modify the publication bias and 9 studies added to adjust for the missed study through this method. The results of the Trim and Fill test demonstrate that the pooled effect size was 0.35 (Adjusted SMD = − 0.35, 95% CI − 0.64 to − 0.07).
Adverse events
The adverse events and dropout rates are summarized in Table 3. The dropout rate ranged from 0 to 41%.
Discussion
This meta-analysis demonstrated that nutraceutical supplementation may lead to an improvement in total and also pain and stiffness subscales of WOMAC and VAS but did not affect WOMAC physical function subscale. The existing modalities for managing OA are basically symptomatic and have not been confirmed to slow, arrest or inverse the joint subversion and cartilage degradation progression8. For this reason, over the past few years, attention has been focused on the impact of nutritional supplements in managing and preventing OA, considering its risk–benefit ratio and low cost and great acceptance by patients. Nutraceuticals provide a great variety of products with a broad range of properties such as anti-inflammatory and antioxidant13,58,59. Nevertheless, their efficacy in OA is uncertain, yet.
Short term nutraceutical supplementation in OA patients
In studies with short term duration of supplementation, significant effects of nutraceutical supplement only were seen on VAS and WOMAC stiffness scores. Among these, three supplements [Low dose Sierrasil (2 g/day) in addition to cat's claw extract in patients with mild to moderate knee OA according to Kellgren and Lawrence scoring system for classification of knee OA60 and fortified milk-based bioactive micronutrient beverage and SKI 306X in knee OA patients with unspecified disease severity] had significant effects on VAS pain intensity. Low dose Sierrasil in addition to cat's claw extract and l-carnitine had a considerable effect also on WOMAC all subscales in patients with mild to moderate knee OA. Additionally, milk protein concentrate (MPC) showed significant effects on WOMAC stiffness score in knee OA patients with unspecified disease severity and Chicken comb extract with a high content of hyaluronic acid had a considerable effect on WOMAC total score, in patients with mild to severe knee OA according to Kellgren and Lawrence scoring system for classification of knee OA60.
Sierrasil is an indigenous mineral product isolated from the Sierra Mountains in the USA with a cultural history of usage in the treatment of joint pain and established cartilage degradation reducing properties61. SKI306X is a herbal mixture (Clematis mandshurica, Trichosanthes kirilowii and Prunella vulgaris) applied for the management of inflammatory diseases and is clinically accepted for the treatment of OA in Far East Asia62. In the systematic review of RCTs by Ameye and Chee2 moderate evidence was established for SKI306X in improving the symptoms in OA patients. Hyaluronic acid or hyaluronan (sodium hyaluronate) is accountable for the viscoelasticity and lubricating impacts of synovial fluid of the joint and has been shown to have the biophysical and biochemical roles in synovial tissues63. However, in a recent systematic review and meta-analysis by Liu et al.64, collagen hydrolysate, extract of the skin of the passion fruit (PFP), Curcuma longa extract, Boswellia serrata extract, pycnogenol and L-carnitine exhibited clinically important effects for pain alleviation in short term and only two supplements (green-lipped mussel extract and undenatured type II collagen (UC-II) showed clinically important effects on pain reduction at medium term. However, we founded that long term UC- II supplementation had considerable effects on WOMAC total and also WOMAC pain and physical function scale scores in patients with mild Knee OA. UC-II is a natural component which comprises a glycosylated, undenatured type-II collagen. Studies have revealed that UC-II restrain joint health in both OA and rheumatoid arthritis (RA) diseases48.
Medium term nutraceutical supplementation in OA patients
In the subgroup analysis, the greatest efficacy of nutraceutical supplements on WOMAC index total score and its subscales and also VAS was related to medium term supplementation (10 to 20 months). Most of these studies involved patients with mild to moderate knee OA according to Kellgren and Lawrence scoring system for classification of knee OA60 or American College of Rheumatology Classification Criteria for Knee Osteoarthritis65 which supplements were administered as an adjunctive to symptomatic treatments (NSAIDs and/or analgesics) except nine of them (three33,47,54 involved patients with knee and/or hip OA, four24,32,44,52 involved patients with severe knee OA and two53,55 involved patients for which supplements were administered as a monotherapy and no concomitant treatment were allowed).
Among studies with medium term of supplementation, WOMAC total score was considerably improved through supplementation with CS in patients with mild to moderate knee OA, Deer bone extract (DBE) in patients with moderate to severe knee OA and PFP and collagen peptides isolated from pork skin (PCP) in patients with mild to severe knee OA.
OA is described by damage of type II collagen and GAGs, which are present in the joint. The lessening of GAGs is an essential factor leading to enhanced cartilage deprivation in the OA. CS, a central structural part of cartilage, is a sulfated GAG. Investigations in animal models have suggested that dietary supplements of CS prevent articular cartilage depreciation66. This protecting consequence is related to the anti-inflammatory activities of CS by increasing the synthesis of hyaluronic acid and proteoglycans, and decreasing the production of proteolytic enzymes and nitric oxide57. Deer horn extract has been considered as a noteworthy health restorative in traditional medicine amongst several Asian countries67. Oily DBE and CPC were recently revealed to have anti-inflammatory properties and reduce the morphological deviations related with osteoarthritic cartilage damage in animal models of OA68,69.
The WOMAC all subscale scores were improved through medium term supplementation with A. paniculata purified extract (ParActin) (in patients with mild knee OA), DBE (in patients with moderate to severe knee OA) and MSM (in knee OA patients with unknown severity). PFP improved only WOMAC pain and physical function subscales in patients with mild to severe knee OA, Boswellia serrata extract improved only WOMAC pain and stiffness subscales score and VAS in patients with mild to moderate knee OA and Artemisia annua extract (ART) improved considerably only WOMAC stiffness subscale in knee OA with unknown severity.
Long term nutraceutical supplementation in OA patients
Regarding long term supplementation, skimmed milk containing probiotic Lactobacillus casei Shirota (LcS) had considerably effects on WOMAC total and also WOMAC stiffness scale score and UC- II had considerably effects on WOMAC total and also WOMAC pain and physical function scale scores in patients with mild Knee OA according to Kellgren and Lawrence scoring system for classification of knee OA60. Boswellia serrata extract improved WOMAC stiffness scale score in knee OA patients with unspecified disease severity. No supplements were recognized with significant effects on VAS reduction in the long term. However Liu et al.64, identified that no supplement had important effects on pain alleviation and physical function improvement in long term in patients with hand, hip or knee OA. These different conclusions are somehow because of different eligibility criteria for included studies and also different scales used for measuring pain and physical function.
There is a growing field of interest and research indicating the protective benefits of dietary polyphenols in decreasing risk for chronic diseases59 through accepting electrons from free radicals, distracting chain oxidation reactions, and improving cellular antioxidative capability16. The results of several studies suggested that supplementation with polyphenols and botanical extracts (e.g., Boswellia serrata extract, PFP, ParActin, ART and cat's claw extract) decrease the serum levels of TNF-α and MMP-3 in synovial fluid in patients with knee OA compared with the control groups53,70,71. Cellular and animal models have suggested also the benefits of such compounds and food ingredients (e.g., probiotics) in inhibiting inflammatory paths and reducing the production of iNOS, COX-2 and MMP enzymes to decrease the catabolic destruction of the cartilage16,72,73,74,75,76.
A very important point in our findings which must be considered is that GS and vitamin D with the greatest interest in administration and consumption among OA patients, do not exhibit a clinically significant effect on knee or hip OA. GS is a water-soluble amino monosaccharide, considered as a desired substrate for the biosynthesis of GG chains and is in great amounts in cartilage matrix and synovial fluid. Glucosamine was thought to afford building substrates for the cartilage extracellular matrix biosynthesis. Later studies have established additional clarifications for its anti-inflammatory and anti-catabolic properties. A Cochrane review of RCTs of all GS formulations in OA patients, restricted to studies with satisfactory concealment, failed to display any advantage of GS for pain77. Hereafter, GS was firstly suggested by European League Against Rheumatism (EULAR) and Osteoarthritis Research Society International (OARSI) for pain management and structure enhancement in OA patients, but not in the most recent National Institute for Health and Care Excellence (NICE) guidelines.
It has been theorized that vitamin D supplementation in patients with knee OA might be a practicable and cost-effective approach for managing clinical symptoms and making a structural advance. However most clinical trials showed that vitamin D supplementation does not improve cartilage volume or knee pain41,46,78. In line with our findings, the results of a systematic review of RCTs covering 1189 patients by Hussein79 did not recommend vitamin D supplementation in patients with knee OA.
Our study opens new horizons for the managing of degenerative joint diseases. We collected clinical trials of nutraceuticals and dietary supplements and the findings were really hopeful and encouraging. However, there is a need for more well-designed randomized clinical trials which can confirm the safety and efficacy of such products. This could help clinicians in endorsing them for OA patients.
The present study has some limitations that need to be considered in explicating the results of this systematic review and meta-analysis. Firstly, in spite of an increasing body of nutraceutical researches in subjects with OA, the number of studies included in this specific review after a systematic review of the existing scientific literature was lower than what would have been predicted. We believe that our inclusion criteria had a significant role, because we considered variables (i.e. VAS and WOMAC) that are not measured in many studies. Secondly, there is probable publication bias. Some unpublished abstracts and articles were not included because of unavailability. Thirdly, the language may lead to bias as we selected only the English and Persian language due to limited resources. These may considerably reduce our sample size and accordingly our ability to delineate statistically significant findings. Fourthly, the heterogeneity between the results is an issue need to be considered. Although we did a subgroup analysis, we were not successful to completely minimize these heterogeneities. Finally, there may be some possible aspects not considered in the present systematic review and meta-analysis, such as the severity of OA, region, and race.
In spite of the stated limitations, this systematic review and meta-analysis provides the first systematic work to consider clinical trials on nutraceutical supplementation in relation to pain and physical disability in patients with knee/hip OA. In addition, subgroup analysis was implemented according to the nutraceutical type and we applied more suitable consequence indicators to direct this meta-analysis.
In conclusion, nutraceutical supplementation mostly along with symptomatic treatments (NSAIDs/ COX-2 inhibitors and analgesics) may effectively improve pain and physical function in patients with knee/hip OA. In the subgroup analysis, the greatest efficacy of nutraceutical supplements was related to 10–20 month (medium term) supplementation especially in patients with mild to severe knee OA. Despite recognized supplements with no established significant efficacy in our study (such as glucosamine and vitamin D), some not well-known supplements (Boswellia serrata extract, DBE, PFP, PCP, ParActin, ART and Pycnogenol) seem to have largest benefits in decreasing pain and improving physical function with negligible adverse events. It is recommended to trying these supplements in a safe doses along with conventional symptomatic treatments and physical therapy for at least 10 weeks especially for those with mild to moderate knee OA except low dose Sierrasil in addition to cat's claw extract, fortified bioactive micronutrient beverage, SKI 306X, L-carnitine, MPC and hyaluronic acid which are expected to have beneficial effects in decreasing pain and/or disability in less than 10 weeks of supplementation and also probiotic LcS and UC-II which are not anticipated to have favorable effects in less than 20 weeks of supplementation even in patients with mild knee OA. Other more precise outcome measurement tools, such as inflammatory biomarkers or image study, should probably be introduced into future studies to make them more convincing evidence.
References
Szychlinska, M. A. et al. Co-expression and co-localization of cartilage glycoproteins CHI3L1 and lubricin in osteoarthritic cartilage: morphological, immunohistochemical and gene expression profiles. Int. J. Mol. Sci. 17, 359 (2016).
Ameye, L. G. & Chee, W. S. Osteoarthritis and nutrition. From nutraceuticals to functional foods: a systematic review of the scientific evidence. Arthritis Res. Ther. 8, 127 (2006).
Concetta Aiello, F. et al. Molecular links between diabetes and osteoarthritis: The role of physical activity. Curr. Diabetes Rev. 13, 50–58 (2017).
Fajardo, M. & Di Cesare, P. E. Disease-modifying therapies for osteoarthritis. Drugs Aging 22, 141–161 (2005).
Ravalli, S., Castrogiovanni, P. & Musumeci, G. Exercise as medicine to be prescribed in osteoarthritis. World journal of orthopedics 10, 262 (2019).
Castrogiovanni, P. et al. Moderate physical activity as a prevention method for knee osteoarthritis and the role of synoviocytes as biological key. Int. J. Mol. Sci. 20, 511 (2019).
Di Rosa, M., Castrogiovanni, P. & Musumeci, G. The synovium theory: can exercise prevent knee osteoarthritis? The role of “mechanokines”, a possible biological key. J. Funct. Morphol. Kinesiol. 4, 11 (2019).
Sengupta, K. et al. A double blind, randomized, placebo controlled study of the efficacy and safety of 5-Loxin for treatment of osteoarthritis of the knee. Arthritis Res. Ther. 10, R85 (2008).
Szychlinska, M. A. et al. Physical activity and Mediterranean diet based on olive tree phenolic compounds from two different geographical areas have protective effects on early osteoarthritis, muscle atrophy and hepatic steatosis. Eur. J. Nutr. 58, 565–581 (2019).
Ravalli, S., Szychlinska, M. A., Leonardi, R. M. & Musumeci, G. Recently highlighted nutraceuticals for preventive management of osteoarthritis. World J. Orthop. 9, 255 (2018).
Toopchizadeh, V., Dolatkhah, N., Aghamohammadi, D., Rasouli, M. & Hashemian, M. Dietary inflammatory index is associated with pain intensity and some components of quality of life in patients with knee osteoarthritis. BMC Res. Not. 13, 1–7 (2020).
Toopchizadeh, V. et al. Diet quality is associated with pain intensity and quality of life in a sample of patients with knee osteoarthritis: a cross-sectional study. J. Res. Clin. Med. 8, 6–6 (2020).
Castrogiovanni, P. et al. Nutraceutical Supplements in the Management and Prevention of Osteoarthritis. Int. J. Mol. Sci. https://doi.org/10.3390/ijms17122042 (2016).
Szychlinska, M. A. et al. Assessment of vitamin D supplementation on articular cartilage morphology in a young healthy sedentary rat model. Nutrients 11, 1260 (2019).
Eftekharsadat, B., Aghamohammadi, D. & Dolatkhah, N. Lower serum levels of alpha tocopherol and lycopene is associated with higher pain and physical disability in subjects with primary knee osteoarthritis: s case-control study. Int. J. Vitamin Nutr. Res. https://doi.org/10.1024/0300-9831/a000635 (2020).
Shen, C. L. et al. Dietary polyphenols and mechanisms of osteoarthritis. J. Nutr. Biochem. 23, 1367–1377. https://doi.org/10.1016/j.jnutbio.2012.04.001 (2012).
Reginster, J. Y. et al. Long-term effects of glucosamine sulphate on osteoarthritis progression: a randomised, placebo-controlled clinical trial. Lancet 357, 251–256 (2001).
Appelboom, T., Schuermans, J., Verbruggen, G., Henrotin, Y. & Reginster, J.-Y. Symptoms modifying effect of avocado/soybean unsaponifiables (ASU) in knee osteoarthritis. Scand. J. Rheumatol. 30, 242–247 (2001).
Jung, Y. B. et al. Effect of SKI 306X, a new herbal anti-arthritic agent, in patients with osteoarthritis of the knee: a double-blind placebo controlled study. Am. J. Chin. Med. 29, 485–491. https://doi.org/10.1142/s0192415x01000502 (2001).
Schmid, B. et al. Efficacy and tolerability of a standardized willow bark extract in patients with osteoarthritis: randomized placebo-controlled, double blind clinical trial. Phytother. Res. 15, 344–350 (2001).
Colker, C. M., Swain, M., Lynch, L. & Gingerich, D. A. Effects of a milk-based bioactive micronutrient beverage on pain symptoms and activity of adults with osteoarthritis: a double-blind, placebo-controlled clinical evaluation. Nutrition 18, 388–392 (2002).
Zenk, J. L., Helmer, T. R. & Kuskowski, M. A. The effects of milk protein concentrate on the symptoms of osteoarthritis in adults: an exploratory, randomized, double-blind, placebo-controlled trial. Curr. Ther. Res. 63, 430–442 (2002).
Lequesne, M., Maheu, E., Cadet, C. & Dreiser, R. L. Structural effect of avocado/soybean unsaponifiables on joint space loss in osteoarthritis of the hip. Arthritis Care Res. 47, 50–58 (2002).
McAlindon, T., Formica, M., LaValley, M., Lehmer, M. & Kabbara, K. Effectiveness of glucosamine for symptoms of knee osteoarthritis: results from an internet-based randomized double-blind controlled trial. Am. J. Med. 117, 643–649 (2004).
Miller, M. J. et al. Early relief of osteoarthritis symptoms with a natural mineral supplement and a herbomineral combination: a randomized controlled trial [ISRCTN38432711]. J. Inflamm. 2, 11 (2005).
Kim, L. S., Axelrod, L., Howard, P., Buratovich, N. & Waters, R. Efficacy of methylsulfonylmethane (MSM) in osteoarthritis pain of the knee: a pilot clinical trial. Osteoarthritis Cartil. 14, 286–294 (2006).
Pavelka, K. et al. The efficacy and safety of diacerein in the treatment of painful osteoarthritis of the knee: a randomized, multicenter, double-blind, placebo-controlled study with primary end points at two months after the end of a three-month treatment period. Arthritis Rheum. 56, 4055–4064 (2007).
Farid, R. et al. Pycnogenol supplementation reduces pain and stiffness and improves physical function in adults with knee osteoarthritis. Nutr. Res. 27, 692–697 (2007).
Mehta, K. et al. Comparison of glucosamine sulfate and a polyherbal supplement for the relief of osteoarthritis of the knee: a randomized controlled trial [ISRCTN25438351]. BMC Complement. Altern. Med. 7, 34 (2007).
Ali Shiri, G. H. et al. Efficacy of Elaeagnus angustifolia extract in treatment of osteoarthritis of knee: q randomized double-blind placebo-controlled trial. Kowsar Med. J. 12, 49–57 (2007).
Kalman, D. S., Heimer, M., Valdeon, A., Schwartz, H. & Sheldon, E. Effect of a natural extract of chicken combs with a high content of hyaluronic acid (Hyal-Joint) on pain relief and quality of life in subjects with knee osteoarthritis: a pilot randomized double-blind placebo-controlled trial. Nutr. J. 7, 3 (2008).
Frestedt, J. L., Walsh, M., Kuskowski, M. A. & Zenk, J. L. A natural mineral supplement provides relief from knee osteoarthritis symptoms: a randomized controlled pilot trial. Nutr. J. 7, 9 (2008).
Jacquet, A. et al. Phytalgic, a food supplement, vs placebo in patients with osteoarthritis of the knee or hip: a randomised double-blind placebo-controlled clinical trial. Arthritis Res. Ther. 11, R192 (2009).
Frestedt, J. L., Kuskowski, M. A. & Zenk, J. L. A natural seaweed derived mineral supplement (Aquamin F) for knee osteoarthritis: a randomised, placebo controlled pilot study. Nutr. J. 8, 7 (2009).
Ruff, K. J., Winkler, A., Jackson, R. W., DeVore, D. P. & Ritz, B. W. Eggshell membrane in the treatment of pain and stiffness from osteoarthritis of the knee: a randomized, multicenter, double-blind, placebo-controlled clinical study. Clin. Rheumatol. 28, 907–914. https://doi.org/10.1007/s10067-009-1173-4 (2009).
Farid, R. et al. Oral intake of purple passion fruit peel extract reduces pain and stiffness and improves physical function in adult patients with knee osteoarthritis. Nutr. Res. 30, 601–606 (2010).
Sengupta, K. et al. Comparative efficacy and tolerability of 5-Loxin and Aflapin against osteoarthritis of the knee: a double blind, randomized, placebo controlled clinical study. Int. J. Med. Sci. 7, 366 (2010).
Debbi, E. M. et al. Efficacy of methylsulfonylmethane supplementation on osteoarthritis of the knee: a randomized controlled study. BMC Complement. Altern. Med. 11, 50 (2011).
Notarnicola, A. et al. The “mesaca” study: methylsulfonylmethane and boswellic acids in the treatment of gonarthrosis. Adv. Ther. 28, 894 (2011).
Schauss, A. G., Stenehjem, J., Park, J., Endres, J. R. & Clewell, A. Effect of the novel low molecular weight hydrolyzed chicken sternal cartilage extract, BioCell Collagen, on improving osteoarthritis-related symptoms: a randomized, double-blind, placebo-controlled trial. J. Agric. Food Chem. 60, 4096–4101 (2012).
McAlindon, T. et al. Effect of vitamin D supplementation on progression of knee pain and cartilage volume loss in patients with symptomatic osteoarthritis: a randomized controlled trial. JAMA 309, 155–162 (2013).
Ebrahimi, A. A., Nikniaz, Z., Ostadrahimi, A., Mahdavi, R. & Nikniaz, L. The effect of Elaeagnus angustifolia L. whole fruit and medulla powder on women with osteoarthritis of the knee: a randomized controlled clinical trial. Eur. J. Integr. Med. 6, 672–679 (2014).
Kolahi, S., Mahdavi, A. M., Mahdavi, R. & Lak, S. Effect of l-carnitine supplementation on clinical symptoms in women with osteoarthritis of the knee: a randomized, double-blind, placebo-controlled trial. Eur. J. Integr. Med. 7, 540–546 (2015).
Kumar, S., Sugihara, F., Suzuki, K., Inoue, N. & Venkateswarathirukumara, S. A double-blind, placebo-controlled, randomised, clinical study on the effectiveness of collagen peptide on osteoarthritis. J. Sci. Food Agric. 95, 702–707 (2015).
Dehghan, M. J. T. J. O. Q. U. O. M. S. Effects of adding vitamin B to Diclofenac on knee osteoarthritis pains. J. Qazvin Univ. Med. Sci. 19 (2015).
Jin, X. et al. Effect of vitamin D supplementation on tibial cartilage volume and knee pain among patients with symptomatic knee osteoarthritis: a randomized clinical trial. JAMA 315, 1005–1013 (2016).
Stebbings, S., Beattie, E., McNamara, D. & Hunt, S. A pilot randomized, placebo-controlled clinical trial to investigate the efficacy and safety of an extract of Artemisia annua administered over 12 weeks, for managing pain, stiffness, and functional limitation associated with osteoarthritis of the hip and knee. Clin. Rheumatol. 35, 1829–1836 (2016).
Lugo, J. P., Saiyed, Z. M. & Lane, N. E. Efficacy and tolerability of an undenatured type II collagen supplement in modulating knee osteoarthritis symptoms: a multicenter randomized, double-blind, placebo-controlled study. Nutr. J. 15, 14. https://doi.org/10.1186/s12937-016-0130-8 (2016).
Lubis, A. M., Siagian, C., Wonggokusuma, E., Marsetyo, A. F. & Setyohadi, B. Comparison of glucosamine-chondroitin sulfate with and without methylsulfonylmethane in grade I-II knee osteoarthritis: a double blind randomized controlled trial. Acta Med. Indonesiana 49, 105–111 (2017).
Rafraf, M., Hemmati, S., Jafarabadi, M. A., Moghaddam, A. & Haghighian, M. K. Pomegranate (Punica Granatum L.) peel hydroalcoholic extract supplementation reduces pain and improves clinical symptoms of knee osteoarthritis: a randomized double-blind placebo controlled study. Iran. Red Crescent Med. J. 19, 1 (2017).
Lei, M., Guo, C., Wang, D., Zhang, C. & Hua, L. The effect of probiotic Lactobacillus casei Shirota on knee osteoarthritis: a randomised double-blind, placebo-controlled clinical trial. Beneficial Microb. 8, 697–703 (2017).
Shin, D. et al. Deer bone extract supplementation for mild-to-moderate knee osteoarthritis symptoms: a randomized, double-blind, placebo-controlled trial. J. Med. Food 21, 159–166 (2018).
Dehghani, S. et al. The effect of a garlic supplement on the pro-inflammatory adipocytokines, resistin and tumor necrosis factor-alpha, and on pain severity, in overweight or obese women with knee osteoarthritis. Phytomedicine 48, 70–75. https://doi.org/10.1016/j.phymed.2018.04.060 (2018).
Salimzadeh, A. et al. The effect of 12-week garlic supplementation on symptom relief in overweight or obese women with knee osteoarthritis. Int. J. Clin. Pract. 72, e13208. https://doi.org/10.1111/ijcp.13208 (2018).
Hancke, J. L. & Srivastav, S. A double-blind, randomized, placebo-controlled study to assess the efficacy of Andrographis paniculata standardized extract (ParActin(R)) on pain reduction in subjects with knee osteoarthritis. Phytomedicine https://doi.org/10.1002/ptr.6339 (2019).
Majeed, M., Majeed, S., Narayanan, N. K. & Nagabhushanam, K. A pilot, randomized, double-blind, placebo-controlled trial to assess the safety and efficacy of a novel Boswellia serrata extract in the management of osteoarthritis of the knee. Phytother. Res. https://doi.org/10.1002/ptr.6338 (2019).
Rondanelli, M., Braschi, V. & Gasparri, C. Effectiveness of non-animal chondroitin sulfate supplementation in the treatment of moderate knee osteoarthritis in a group of overweight subjects: a randomized, double-blind, placebo controlled pilot study. Nutrients 11, 20–27. https://doi.org/10.3390/nu11092027 (2019).
McAlindon, T. E. et al. Do antioxidant micronutrients protect against the development and progression of knee osteoarthritis?. Arthritis Rheum. 39, 648–656 (1996).
Pandey, K. B. & Rizvi, S. I. J. O. M. Plant polyphenols as dietary antioxidants in human health and disease. Longevity 2, 270–278 (2009).
Kohn, M. D., Sassoon, A. A. & Fernando, N. D. Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clin. Orthop. Relat. Res. 474, 1886–1893 (2016).
Miller, M. J., Ahmed, S., Bobrowski, P. & Haqqi, T. M. Suppression of human cartilage degradation and chondrocyte activation by a unique mineral supplement (sierrasil) and a cat’s claw extract, vincaria. J. Am. Nutr. Assoc. 7, 32 (2004).
Kim, J.-H. et al. SKI306X, an oriental herbal mixture, suppresses gastric leukotriene B4 synthesis without causing mucosal injury and the diclofenac-induced gastric lesions. Life Sci. 77, 1181–1193 (2005).
Moreland, L. Intra-articular hyaluronan (hyaluronic acid) and hylans for the treatment of osteoarthritis: mechanism of action. Arthritis Res. Ther. 5, 54–67 (2003).
Liu, X., Machado, G. C., Eyles, J. P., Ravi, V. & Hunter, D. J. Dietary supplements for treating osteoarthritis: a systematic review and meta-analysis. Br. J. Sports Med. 52, 167–175 (2018).
Kawasaki, T., Inoue, K., Ushiyama, T. & Fukuda, S. Assessment of the American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the knee. Ryumachi 38, 2–5 (1998).
Hui, J. H. et al. Intra-articular delivery of chondroitin sulfate for the treatment of joint defects in rabbit model. J. Mol. Histol. 38, 483–489 (2007).
Kawtikwar, P. S., Bhagwat, D. A. & Sakarkar, D. M. Deer antlers-traditional use and future perspectives. Indian J. Trad. Knowl. 9, 245–251 (2010).
Choi, H.-S., Im, S., Park, J. W. & Suh, H. J. Protective effect of deer bone oil on cartilage destruction in rats with monosodium iodoacetate (MIA)-induced osteoarthritis. Biol. Pharm. Bull. 39, 2042–2051 (2016).
Ohara, H., Iida, H., Ito, K., Takeuchi, Y. & Nomura, Y. Effects of Pro-Hyp, a collagen hydrolysate-derived peptide, on hyaluronic acid synthesis using in vitro cultured synovium cells and oral ingestion of collagen hydrolysates in a guinea pig model of osteoarthritis. Biosci. Biotechnol. Biochem. 74, 2096–2099 (2010).
Sengupta, K. et al. A double blind, randomized, placebo controlled study of the efficacy and safety of 5-Loxin for treatment of osteoarthritis of the knee. Biosci. Biotechnol. Biochem. 10, 85 (2008).
Puricelli, L., Dell’Aica, I., Sartor, L., Garbisa, S. & Caniato, R. Preliminary evaluation of inhibition of matrix-metalloprotease MMP-2 and MMP-9 by Passiflora edulis and P. foetida aqueous extracts. Fitoterapia 74, 302–304 (2003).
Li, Y. et al. Andrographolide inhibits inflammatory cytokines secretion in LPS-stimulated RAW264.7 cells through suppression of NF-κB/MAPK signaling pathway. Evid. Based Complement. Altern. Med. 2017, 8248142 (2017).
Hunt, S., Yoshida, M., Davis, C. E., Greenhill, N. S. & Davis, P. F. An extract of the medicinal plant Artemisia annua modulates production of inflammatory markers in activated neutrophils. J. Inflamm. Res. 8, 9 (2015).
So, J.-S. et al. Lactobacillus casei enhances type II collagen/glucosamine-mediated suppression of inflammatory responses in experimental osteoarthritis. Life Sci. 88, 358–366 (2011).
Sandoval, M. et al. Cat’s claw inhibits TNFα production and scavenges free radicals: role in cytoprotection. Free Radical Biol. Med. 29, 71–78 (2000).
Sandoval, M. et al. Anti-inflammatory and antioxidant activities of cat’s claw (Uncaria tomentosa and Uncaria guianensis) are independent of their alkaloid content. Phytomedicine 9, 325–337 (2002).
Towheed, T. et al. Glucosamine therapy for treating osteoarthritis. Cochrane Database Syst. Rev. (2005).
Sanghi, D. et al. Does vitamin D improve osteoarthritis of the knee: a randomized controlled pilot trial. Clin. Orthop. Relat. Res. 471, 3556–3562 (2013).
Hussain, S., Singh, A., Akhtar, M. & Najmi, A. K. Vitamin D supplementation for the management of knee osteoarthritis: a systematic review of randomized controlled trials. Rheumatol. Int. 37, 1489–1498 (2017).
Acknowledgements
The authors would like to acknowledge the staff of the Physical Medicine and Rehabilitation Research Center of Tabriz University of Medical Sciences for their support with this study.
Author information
Authors and Affiliations
Contributions
D.A. and N.D. contributed equally to the literature search and analysis design. D.A., N.D. and F.B. analyzed and interpreted the data. N.D., F.E. and M.H. drafted the first and revised version of manuscript. D.A. had primary responsibility for final content. All authors contributed to the critical revision of the manuscript for important intellectual content and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Aghamohammadi, D., Dolatkhah, N., Bakhtiari, F. et al. Nutraceutical supplements in management of pain and disability in osteoarthritis: a systematic review and meta-analysis of randomized clinical trials. Sci Rep 10, 20892 (2020). https://doi.org/10.1038/s41598-020-78075-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-78075-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.