Abstract
The mechanisms underlying emotional alterations constitute a key research target in neuroscience. Emerging evidence indicates that these disruptions can be related to abnormal interoception (i.e., the sensing of visceral feelings), as observed in patients with cardiodynamic deficits. To directly assess these links, we performed the first multicenter study on emotion recognition and interoception in patients with hypertensive heart disease (HHD). Participants from two countries completed a facial emotion recognition test, and a subsample additionally underwent an interoception protocol based on a validated heartbeat detection task. HHD patients from both countries presented deficits in the recognition of overall and negative emotions. Moreover, interoceptive performance was impaired in the HHD group. In addition, a significant association between interoceptive performance and emotion recognition was observed in the control group, but this relation was abolished in the HHD group. All results survived after covariance with cognitive status measures, suggesting they were not biased by general cognitive deficits in the patients. Taken together, these findings suggest that emotional recognition alterations could represent a sui generis deficit in HHD, and that it may be partially explained by the disruption of mechanisms subserving the integration of neuro-visceral signals.
Similar content being viewed by others
Introduction
The intriguing relation between the heart and emotional processing has been gaining increasing attention in cognitive neuroscience, as best seen in recent theories of affect suggesting that interoceptive processing (i.e., the sensing of visceral feelings1) influences subjective emotional states an behaviors2,3. Alterations of the cardiovascular system can affect interoceptive processing4,5. However, the impact of cardiac abnormalities on emotional processing remains poorly understood. Although emotional alterations have been associated with high blood pressure in normotensive and subjects at risk of hypertension6,7,8, these studies lack precise diagnoses, fail to rule out key cognitive confounds, and offer no evaluation of interoceptive processing. The literature is thus deprived of key empirical evidence for neuro-visceral models of the phenomenon. Here, we present the first multicenter study assessing emotional recognition in essential hypertensive heart disease (HHD), accounting for the patients’ general cognitive status and assessing the links between emotion processing and cardiac interoception. In this way, our research contributes to understanding the relationship between emotional and interoceptive deficits in HHD, in particular, and its implications for theories of embodied emotional processing, in general2,9,10,11,12.
Today, the main challenge for characterizing the impact of hypertension of emotional processing lies in the shortcomings of available studies. Existing reports are undermined by sampling issues, including the recruitment of groups that are not matched for sociodemographic variables (e.g., age, gender and education8) or which prove ethnically biased (e.g., comprised only of Afro-American participants)7 or socio-economically restricted (e.g., including only low-income subjects)7, alongside investigations that directly lacked healthy controls13. Moreover, in most studies, HHD diagnosis has been rarely established on the basis of rigorous clinical examination6,7,8,14,15, which may mask potential links between emotional alterations and disease-specific abnormalities. In addition, most previous works have failed to include assessments of general cognitive functions6,7,8,14,15. This is a major caveat, too, since emotional processes are closely related to executive functions, memory, language, and otherwise general cognitive domains16,17,18,19,20,21,22, which, in turn, are typically affected in subjects with high blood pressure23,24,25,26,27,28. Without such data, the literature is moot on whether emotional disturbances in essential hypertension constitute primary deficits or secondary disruptions following from other general alterations triggered by high blood pressure.
Against this background, we performed the first multi-center study assessing emotional recognition in HHD patients diagnosed by specialized cardiologists in clinics from two countries. First, to control for possible cognitive differences between patients and controls23,24,25,26,27,28, and to account for the well-established role of language skills in emotion processing21,22, we administered an executive function battery and a highly sensitive cognitive screening tool including language measures (see details in “Cognitive assessment”, Table 1). Then, participants performed a validated emotion morphing task29. In addition, in Country-2, we capitalized on the opportunity to assess cardiac interoception, a key mediator of emotional processing in healthy subjects3,30,31 that is affected in hypertension4,32. This was done via a validated heartbeat detection task, known to be sensitive to interoceptive deficits in hypertensive subjects4,32. HHD affords a key model to this end, given its alterations in two interrelated mechanisms (emotional processing and interoception)2,4,33,34 and its high prevalence among heart diseases35, which allows recruiting a considerable sample that fulfills stringent inclusion and exclusion criteria. In light of previous reports, we predicted that HHD patients would exhibit emotion recognition deficits across countries, and that these would not be explained by global cognitive state or executive skills. Moreover, we hypothesized that emotional processing would be significantly associated with interoceptive performance in healthy controls, but that such a link would be abolished in the patients.
Methods
Participants
This multicenter study comprised 116 participants (60 HHD patients and 56 healthy controls) recruited from two specialized centers (see Table 1 for demographic information). Using G*Power 3.136, we performed a power estimation analysis for a one-way ANOVA, considering an alpha of α = 0.05, a power of 0.837, and an effect size of η2 = 0.17 (as a median value between η2 = 0.08 and 0.27, based on previous reports for similar experimental tasks and samples38,39,40,41). Results indicated that a total sample size of 41, considering the two groups, was enough to reach the estimated effects. Our actual sample size (n = 116) reaches a power of 0.99. Participants were recruited from Faculty of Health, Santiago de Cali University (Country-1), and the INECO Foundation (Country-2). In both cases, participants were directly recruited from volunteer lists and through postings on relevant social media. The HHD samples were comprised of chronic outpatients from both institutions, each diagnosed with essential hypertension by expert cardiologists (R. S. and J. L.). In all cases, diagnosis was made following current revised criteria42 and guidelines from the American Heart Association43—for further details about clinical measures in each country, see Supplementary Table 1. The patients’ medical histories, provided by expert cardiologists, confirmed the absence of neurological, metabolic, or psychiatric antecedents (e.g., no history of heart attacks, controlled levels of cholesterol, controlled smoking history, no prior strokes, and absence of affective or personality disorders).
The HHD patients were matched with healthy controls in terms of age, gender, education, mood (as tapped through Beck’s Depression Inventory)44, and handedness (Table 1)—this pairing was achieved for each country separately and also for both together. None of the controls presented a history of drug abuse, psychiatric or neurologic disease, cognitive impairment or hypertension. All participants provided informed consent in accordance with the Declaration of Helsinki. The study was approved by the institutional ethics committees of both institutions, the Ethical Research Committee of the Faculty of Health, Santiago de Cali University (Country-1) and the Ethical Research Committee of INECO (Country-2).
Multi-center analysis
Cognitive assessment
Cognitive abilities were examined with two screening measures. First, executive functions were assessed with the INECO Frontal Screening (IFS) battery45, a sensitive tool for neuropsychiatric assessment which taps eight relevant domains, including motor programming, conflict instructions, motor inhibitory control, working memory (numerical, verbal and spatial), abstraction capacity, and verbal inhibitory control. The maximum global score on the IFS is 30 points. Also, the subjects’ global cognitive status was established via the Addenbrooke’s Cognitive Examination Revised (ACE-R)46. This tool encompasses tests of five cognitive domains (attention/orientation, memory, language, verbal fluency, and visuospatial skills), yielding a maximum global score of 100. For a full description of these instruments, see Supplementary Table 2.
Facial emotion recognition
Participants performed a validated Emotional Morphing task47 based on the Pictures of Affect Series48. The task has proven sensitive for neurological30,49,50,51, psychiatric52,53, and cardiological5 conditions. It taps on six basic emotions: happiness, surprise, sadness, fear, anger, and disgust. Participants were instructed to recognize each emotion as fast as they could (watching a video with faces from 0 to 100% morphing) by pressing the ‘space’ key on a keyboard, and then they were requested to identify the emotion at hand from a word list showing the names of six basic emotions.
During the first stage, 48 faces were presented in videos that showed progressive changes in their shape and texture, with a morphing increment of 5%, from a neutral image (0%) to a full emotion face (100%) (for details, see the series of validation experiments in47 and recent adaptations52,53). These stimuli were randomly presented on a computer screen for a maximum of 6 s and subjects were allowed to interrupt the morphing processes if they were sure of what emotion had been presented (i.e., before 100% morphing). Upon the subject’s response or full elapsing of the six-second period, a list of basic emotion categories appeared, and subjects were required to choose the one that matched the face’s emotion. The task was run and analyzed by E-prime Version 2.0 and its toolbox E-studio and E-run.
For both the multicenter and single-country analyses, accuracy was indexed via three scores, namely: global score (i.e., for all emotions combined), in terms of valence (i.e., considering all negative emotions together [sadness, angry, disgust, and fear] and all positive emotions together [happiness and surprise]), and also considering each emotion type separately. Verbal labels were adapted to Spanish and previously validated with samples from both countries50,52,53.
Multicenter behavioral data analysis
To test whether the predicted impairments proved robust despite socio-cultural heterogeneity, we implemented two strategies: statistical analyses were first performed for the combination of samples from both countries, and then repeated for each country separately. Also, to maximize informativeness, we compared the groups’ emotion recognition performance via task via ANOVAs for (i) global scores, (ii) all negative emotions together, (iii) all positive emotions together, and (iv) each individual emotion separately. Gender was compared between groups with Pearson’s chi-squared (χ2) test. Age, education, and mood state data were assessed through ANOVAs. For the analysis of the facial emotion recognition task, we performed ANOVAs for the global, negative, and positive scores, and also for each individual emotion. Also, subjects deviating from the sample’s mean in at least 2 SDs were considered as outliers (as per Chauvenet’s criteria) to remove data points that may not reflect the psychophysiological processes targeted by the task, while increasing the power of the test to find truly significant results52,53,54, as shown in simulation studies55,56,57 (Supplementary Table 8). Furthermore, considering the cognitive deficits observed in the HHD group (see Table 1) and their potential influence on emotion processing2,21,26,34, we re-ran all emotion-recognition analyses using ANCOVAs, including the scores of the IFS and the ACE-R as covariates—all results are reported after this covariation (see “Results” section and Supplementary Tables 4 and 7. As a complementary strategy, we replicated our analyses upon removing subjects with scores indicative of cognitive deficits and explored correlations with potential confounding factors. Effect sizes were reported with partial eta squared (ηp2).
Complementary interoceptive assessment for Country-2
Given that interoceptive skills are pivotal for emotional processing3,30,31,58 and typically impaired in HHD4,32, we tested for associations between emotion recognition and interoception outcomes in Country-2, hypothesizing a positive correlation in controls and no such association in the patients. Correlations were performed by comparing scores in the heartbeat detection task (i.e., subject’ precision index: min 0.0–max 1.0) and global performance in emotion recognition (min 0.0–max 1.0).
Interoceptive performance: heartbeat detection task
Interoceptive performance was assessed through a modified version of a validated heartbeat detection task29,59,60,61,62,63,64, in which patients are asked to attend to their own heartbeats (see Fig. 2A and Supplementary Material C.). The task encompassed both a control and an interoceptive condition. In the control condition (a baseline measure of external monitoring skills), participants tapped a keyboard to follow binaurally presented heartbeats. This condition included two blocks of 2.5 min, featuring regularly timed and irregularly timed heartbeats, respectively. In the interoceptive condition (aimed to assess inner signal monitoring), participants tapped a key to follow their own heartbeats without any external cues. Each participant completed two 2.5-min blocks. The interoceptive condition provides a measure of interoceptive accuracy, namely, the subjects’ objective performance in following their own heartbeats65. While the interoceptive condition had participants follow a relatively uncertain signal (their own heartbeats), the control condition required following a regular and external recorded heartbeat that was easier to track and presented less uncertainty. Behaviorally, these are rather different tasks that measure different abilities but both are critical for the interpretation of the results from the heartbeat detection task66,67. In this way, the control condition allows checking that participants have preserved basic motor tracking abilities, thus ruling out domain-external factors as a possible source of potential between-group differences in interoceptive condition.
During all blocks, participants were requested to respond with their dominant hand, to keep their eyes on a fixation cross, and to avoid excessive blinking and moving while the latter remained on screen—for further details of the task, see4.
Interoceptive performance was analyzed for each subject through a precision index59,61,62,63,68 based on two scores, namely: correct answers and recorded heartbeats. The correct answers scores were calculated as the total number responses that matched each of the subject’s heartbeats. To estimate this match, every motor response is compared within a time window around every recorded heartbeat; if the tap input is temporally locked within any heartbeat, that response is considered as correct –the procedure to estimate the time window for each subject is detailed in59. On the other hand, recorded heartbeats refer to the total number heartbeats registered in each condition. Both scores were used to calculate behavioral accuracy, following this equation: 1 − (Recorded heartbeats − ∑ Correct answers)/(Recorded heartbeats). This precision index can vary between 0 and 1, with higher scores indicating only small differences between correct answers and recorded heartbeats, and, thus, better performance (see Supplementary Material C.).
Heartbeat detection task and correlations analyses
Interoceptive performance for Country-2 participants was compared between groups via one-way ANOVAs. Correlations between facial emotion recognition and interoceptive outcomes were examined through bi-variated Pearson’s correlations, with a significance threshold of p ≤ 0.05. Theoretically, given that the aim of the study was to analyze the interplay between a basic cardio-cognitive mechanism (interoception) involved in emotions processing in general, interoceptive performance was matched only with a global score of emotions recognition. Relative to single-emotion scores, the global score provides a greater number of trials and allows capturing overall performance regardless of the valence of each emotion. Moreover, given the limited range of trials for each emotion (only four trials per emotion are presented in the task), the global score gives a more fine-grained evaluation of the samples’ inter- and intra-group variability, which allows tackling heterogeneity across the participants’ performance.
Although the heartbeat detection task has been criticized in terms of internal validity66 and robustness69,70, these potential caveats have been challenged and several advantages have been noted71,72,73. Unlike Schandry’s classical heartbeat detection task, which overestimates the real perception of heartbeats considering all behavioral answers as accurate66, our task requires tracking every single heartbeat through motor tapping and our accuracy score considers both failed and accurate responses (see details in62,74). At the same time, performance was controlled by heart rate and heart rate variability, and the window selected to consider accuracy ratings was adjusted to subject’s heart rate (see details in Supplementary Material C.).
Results
Cognitive assessments
IFS outcomes revealed lower scores in patients for both the multicenter analysis (p < 0.01) and also when Country-1 (p < 0.01) was evaluated alone. Country-2 presented no between-group differences (p = 0.13). Similarly, Global ACE-R scores revealed significantly poorer cognitive status in patients than controls, when samples were combined for the multicenter approach (p < 0.01) and also when they were framed separately for Country-1 (p = 0.05) and Country-2 (p = 0.01). Null differences were found in language subscales for both the multicenter analysis and the single-country analyses. Statistical details are shown in Table 1 and Supplementary Table 3.
Facial emotion recognition
Multicenter sample
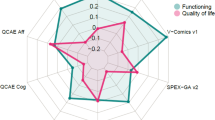
As shown by the accuracy index, patients were outperformed by controls when considering the total average of all emotions [F (1,108) = 12.01, p < 0.01, ηp2 = 0.10] and negative emotions only [F (1,108) = 10.10, p < 0.01, ηp2 = 0.08]—Fig. 1.A. No group differences were found for positive emotions [F (1,108) = 1.57, p = 0.21, ηp2 = 0.01] or individual emotions—see Supplementary Table 6a. After selecting a cognitive unimpaired sample to replicate our main analysis (see criterion in the “Methods” section), we observed that comparison between the multicenter samples (i.e., global score, all negative emotions together, and all positive emotions together) remained intact (Supplementary Table 7). Finally, given that ‘surprise’ may be better classified as a negative emotion75,76, we repeated the analysis reallocating this emotion in the multicenter sample. Results remained the same (Supplementary Table 9).
Facial emotion recognition results. (A) Multicenter results comparing patients and controls. Blue boxes represent controls and red boxes refer to HHD patients. The middle line in each box indicates mean. Whiskers indicate SD. Solid dots indicate each subject’s performance. Asterisks (*) indicate significant differences (p < 0.05) after analyses of covariance. (B) Single-country results. Violet boxes represent controls and pink boxes refer to HHD patients. The middle line in each box indicates mean. Whiskers indicate SD. Asterisks (*) indicate significant differences (p < 0.05) after analyses of covariance.
Country-1
The accuracy index revealed significant poorer performance for patients than controls when considering the average of all emotions [F (1,63) = 4.46, p = 0.03, ηp2 = 0.06], and when fear [F (1,60) = 3.01, p = 0.01, ηp2 = 0.21] and disgust [F (1,61) = 15.71, p < 0.01, ηp2 = 0.41] were analyzed in isolation—Fig. 1.B. No group differences were found for negative and positive scores or for isolated emotions (happiness, surprise, anger, and sadness)—see Supplementary Table 6a.
Country-2
The accuracy index revealed lower performance in patients than in controls when considering the average of all emotions [F (1,43) = 7.62, p < 0.01, ηp2 = 0.15] and when fear [F (1,42) = 5.20, p = 0.02, ηp2 = 0.11] and sadness [F (1,41) = 8.34, p < 0.01, ηp2 = 0.17] were analyzed separately—Fig. 1.B. No group differences were found for negative and positive scores or for isolated emotions (happiness, surprise, anger, and disgust)—see Supplementary Table 6a.
Complementary interoceptive assessment (Country-2 only)
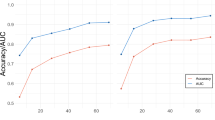
Results from the heartbeat detection task revealed no between-group differences in the control condition [Controls: M = 0.77, SD = 0.14; HHD patients: M = 0.71, SD = 0.18 (F (1,40) = 1.19, p = 0.28, ηp2 = 0.16)], alongside significantly poorer performance for patients than controls in the interoceptive condition [Controls: M = 0.64, SD = 0.20; HHD patients: M = 0.45, SD = 0.13 (F (1,41) = 13.29, p = 0.01, ηp2 = 0.47)]—see Fig. 2, A-bottom.
Associations between facial emotion recognition and interoceptive performance in Country-2. (A) (Top) Schematic representation of the heartbeat detection task. In the interoceptive condition, participants were asked to pay attention to their own heartbeats and tap a key in synchrony with them. (Bottom) Boxplot representation of interoceptive performance. The dots capture each subject’s performance; the horizontal lines inside the box represent the mean; the asterisks indicate statistical differences between groups (p = 0.05). (B) Scatterplots of Pearson’s correlations between interoceptive and emotion recognition outcomes for controls and HHD patients (Country-2). The Y axis represents interoceptive performance in interoceptive condition for each participant. The X axis represents the subjects’ mean score for overall facial emotion recognition.
Also, as a complementary analysis, we compared RTs between groups in each sets of emotions via ANCOVAs, considering the same factors and levels employed in the accuracy analyses. Results showed that patients were consistently slower than controls across emotions, countries, and their combinations (for details, see Supplementary Table 6b). Finally, to explore the relation between accuracy and RT results, we performed Pearson’s correlations between them in each group within the global score indexes. Whereas no significant association emerged in controls (r = 0.07, p = 0.59), a significant positive association was observed in HHD patients (r = 0.33, p = 0.01). This indicates that good outcomes in controls were achieved irrespective of processing time, whereas performance in patients was higher when they devoted more time to categorization decisions. For details, see Supplementary Fig. 6.
Association between interoceptive performance and facial emotion recognition
A significant positive association was observed between interoceptive performance and the global emotion recognition score in controls (r = 0.43, p = 0.03), but not in HHD patients (r = − 0.08, p = 0.74)—Fig. 2B. Still, note that these results should be taken with caution as they were based on relatively small samples (24 controls and 17 HHD). To test the robustness of this result, we performed partial correlations controlling for cognitive outcomes. A significant association was found for controls (r = 0.46, p = 0.029) but not for HHD patients (r = − 0.11, p = 0.688). Additionally, given a different sample size in our independent variables, we generated the Student's t-distribution for testing correlations against each other77,78. Results confirmed that outcomes from the control and HHD samples were different (Z = 1.64, p = 0.05).
Discussion
This is the first multicenter study to reveal systematic emotion recognition impairments in HHD. In both countries, patients exhibited overall emotion recognition impairments, with negative emotion deficits proving robust even in each country separately. Crucially, these disturbances emerged irrespective of the patients’ cognitive dysfunctions and they were unrelated to other potential confounding factors, such language outcomes21,79,80. Accordingly, they would seem to constitute primary (as opposed to epiphenomenal) disruptions. Moreover, complementary evidence from Country-2 revealed that associations between emotion recognition and cardiac interoception (but not other relevant domains) proved significantly positive for controls but were absent in HHD patients, suggesting a partial modulatory effect of viscero-sensing mechanisms in non-pathological emotion processing. Together, these results contribute to recent emotion theories2,3 that emphasize the importance of sensory integration mechanisms in the functioning of cognitive-emotional processes.
Affective dysregulation and deficits in emotion perception and recognition have been previously related to blood pressure alterations in normotensive individuals, subjects at risk for hypertension, and cardiological patients5,6,8,13. However, as noted at the outset, most of these works present several limitations, including imprecise assessments and diagnoses of HHD6,7 as well as scant or null efforts to control for cognitive impairments related to blood pressure alterations8. Here, we overcame these limitations by recruiting a representative multicenter sample with accurate clinical diagnosis while accounting for the potential impact of the patients’ domain-general functions. First, emotion recognition deficits were present across countries after controlling for cognitive status. These deficits were specific for negative emotions at large, and especially robust for disgust, sadness, and fear—the latter two emotions, in fact, were consistently affected in both countries. Interestingly, patients were consistently slower than controls, suggesting that they were not only less effective, but also less efficient at identifying emotions. In addition, accuracy was correlated with RTs in the patients but not in controls. This indicates that good outcomes in the latter were achieved irrespective of processing time, whereas performance in patients was higher when they devoted more time to categorization decisions. Although the overall deficit in emotional recognition mirrors previous results6,7,8,13, our study is the first to show that such an impairment may constitute a primary marker of hypertension, given that it is not explained by overall cognitive disturbances (see Supplementary Material A.). Our study also seems to be the first in reporting specific deficits in negative emotions for HHD patients, given that previous reports on this condition did not present or discuss outcomes in terms of contrastive emotional valances or particular emotions6,7,8,13.
Impaired negative emotion processing in HHD may be influenced by different mechanisms. For example, negative emotions are more dependent on working memory processes than positive ones81,82. However, our results remained the same after covarying for executive-function outcomes (IFS), including working memory tasks. Thus, the alterations observed in negative emotions might not be associated to deficits in this domain. On the other hand, in our multi-centric analysis, the global negative index involves an extensive list of basic emotions (such as fear, anger, sadness, and disgust for our main analysis; and including surprise in a complementary analysis [Supplementary Table 9]), whereas the global positive index is restricted to happiness and surprise (or even to happiness only, as shown in a complementary analysis [Supplementary Table 9]). Therefore, relative to positive emotions, negative stimuli include more individual items that might represent a potential mistake, hence decreasing the associated global score. Yet, when we evaluated each country separately, only individual negative emotions yielded impairments (fear, sadness and disgust), which suggests that the differences in the number of trials are not biasing our global results.
Finally, negative emotions generate greater arousal than positive ones83,84,85,86,87,88. Embodied models of emotional processing (as discussed below) suggest that the perception of bodily changes –mediated by interoceptive processes—is a key aspect that modulates subjective feelings and impacts on emotional processing83,84,85,86,87. Therefore, alterations in this domain, as shown by HHD patients here and in previous studies4,32, might have a larger impact on negative than positive emotions, which generate a less pronounced body arousal. In this way, regarding emotional processing, our results converge with previous evidence showing a prominence of negative emotion as core deficit within the emotional processing repertoire of HHD.
More particularly, results from Country-2 suggest that emotional deficits in HHD could be more related to interoceptive disturbances than to other domains. In fact, whereas emotion recognition and interoceptive outcomes were positively correlated in controls, they were impaired and non-correlated in the patients, even after accounting for the impact of cognitive outcomes and medication status (see “Results” section, Table 1, and Supplementary Material A.). These results align with previous studies showing direct links between interoception and emotion processing, in particular12,30,89,90,91,92,93,94,95,96, and social cognition deficits, in general90,95,97. More specifically, significant associations between interoceptive and emotional outcomes have been reported in a wide range of studies on healthy participants68,91,98,99,100, but no such correlations have emerged in research of psychiatric60,63,101, neurological30,61,102, and cardiovascular5 disorders presenting alterations in one (or both) of these domains. Moreover, interoception and emotion recognition share similar anatomical hubs30,61, including the insular, somatosensory, and anterior cingulate cortices31,103,104,105. Our findings are in line with embodied cognition proposals proposing that emotions are multifactorial constructs based, in part, on the perception of visceral information2,21,33,106. In this context, interoception has been proposed as a neurocognitive mechanism that modulates the subjective feeling and processing of emotions (and also other social cognition domains, such as decision making, empathy and theory of mind)11,34. As discussed above, this interaction between interoception and emotional processing is especially strong for negative emotions (e.g. fear, disgust, sadness, anger), given that they generate a greater physical arousal than positive ones83,84,85,86,87. Moreover, emotions may be modulated by visceral information and shaped by Bayesian inference mechanisms based on bodily inputs3,11,107,108. Those predicted emotional states could be altered when interoceptive pathways become impaired, as shown in HHD4, dampening7 the patients’ perception of their own emotions and the comprehension of emotions in others.
Concerning HHD, existing evidence shows a pattern of emotion emotional6,7,8,13 and interoceptive4,32 deficits. Some theoretical frameworks have been proposed to explain the relation between the alterations of these two domains in cardiovascular diseases14. For example, the baroreflex hypothesis14,109 indicates that the increment of baroreflex activity in the context of high blood pressure could reduce arousal and pain levels and as well as the recognition of negative emotions. On the other hand, the dampening hypothesis6 proposes an inverse relationship between resting blood pressure and emotion responsivity (e.g., pain perception, face emotion recognition)6,7,8. This relationship could be explained by the intimate association between blood pressure regulation in the central nervous system (CNS) and the CNS pathways mediating the expression of emotions, although the specific mechanisms involved are still unclear. In fact, recent evidence suggests that this association should be multifactorial (a basic biobehavioral mechanism, integrating emotional, stress-related, and blood pressure signals)7. Additionally, this hypothesis extends the dampening effect to pain perception, revealing the existence of a general viscero-central integration deficit. In sum, for these two theories, a series of metabolic and emotional conditions could generate more tolerance to negative emotions, leading to their faulty recognition in HHD14. Succinctly, these antecedents coalesce with our results to suggest that emotion recognition deficits in HHD might be associated with disruptions in interoceptive mechanisms.
Our results also align with the view that allostasis is regulated by an internal model of bodily function110 based on previous experiences111. Emotions112 are considered conceptualizations (i.e. high-order domains or metacognition) of those internal states, linked to interoceptive processes113. Indeed, interoceptive theories33,58,114,115,116,117 propose that emotions are constructed by predictions based on (bottom-up) bodily inputs interacting with both internal and external milieu by anticipating (top-down) mental states, feelings, and memories, as well as external (including emotion-laden) stimuli.
Note that interoceptive sensations are usually experienced as lower-order dimensional inputs in affective life110. In HHD literature, essential hypertension is associated with baroceptors impairments in the carotid6,7, that is, the source of cardiac interoception inputsfor a review (see118,119,120). Then, after a series of relays in the brainstem, thalamus and insula, interoceptive information is used as permanent feedback to construct high-order feelings or emotions2,11.
For this model, HHD conditions introduce interferences in the “normal” flow of inner information, as chronic high blood pressure would, altered interoceptive sensations74,99,116,119,121 could disrupt internal predictions. Under normal conditions, when the internal model of the body (top-down) receives new inputs (e.g., an emotional face), chemical adjustments balance the internal and external milieus2,113. Conversely, when high blood pressure alters inner states, this adaptive capacity of the system is dampened7 due to the expansion of tolerance thresholds6, compromising emotional processing.
Beyond its contributions, this work presents limitations that could be tackled in future studies. First, as expected122,123,124,125,126,127, our patients exhibited lower cognitive outcomes tan controls. Although we accounted for this issue through complementary approaches (ANCOVAs, replication analyses with cognitively unimpaired subsamples, correlations with language measures), future studies should assess whether similar outcomes are obtained in HHD samples with and without cognitive deficits. Second, patients were medicated with antihypertensive drugs at the moment of testing in both countries (Supplementary Table 1), as is typical in chronic cases128,129. Although our decision to interrupt medication 48 h before testing has been reported as a strategy to minimize domain-external confounds4, future studies should aim for broader samples including both medicated patients and non-medicated patients. Third, another limitation of our study is that it hinges on the basic emotions model48. It remains uncertain whether similar deficits might be present when considering more complex emotions (such as shame, guilt, among others), although similar alterations in HHD constitute a certain possibility to be explored in future research. Also, given that facial emotion recognition tasks are restricted to visual stimuli representing only basic emotion categories, future studies should consider the role of language and other contextual cues (such as body language and prosody) during the process of recognition and assignment of responses. Indeed, these variables are known to modulate facial emotion recognition21,130. Furthermore, beyond testing for emotion-label words (e.g., sadness, happiness, fear), future works should examine whether HHD patients are also affected in their capacity to process emotion-laden words (e.g., -death, birthday, rape), given that this different type of word categories depend on different cognitive processes79,131,132,133,134. Fourth, also, we did not control the impact of potential language deficits of the HHD sample in emotion perception20,22,135 given that we did not have an specific full battery to measure this domain. Yet, we found no statistical relationship between the “Language” sub-score of the ACE and the ‘global score’ of emotion recognition (Supplementary Table 5). Future studies should include a more comprehensive task to evaluate this ability and corroborate our null findings regarding its association with emotion recognition in HHD patients. Fifth, our correlation results from Country-2 stemmed from a small sample (see “Results” section). Therefore, they should be taken as very preliminary findings until new studies replicate the present analyses. Sixth, future experimental designs could fruitfully extend our present protocol through the addition of tasks tapping other social cognition domains (e.g., empathy or theory of mind), especially in more ecological settings. Finally, the association between interoception and emotional recognition performance was based only on the analysis of the heartbeat detection task. Future research on this field should evaluate the role of other interoceptive dimensions in emotional processing, including awareness104,136,137,138, sensibility65, learning61,139, and metacognition61. Moreover, such extensions of our study could benefit from the inclusion of relevant neurophysiological measures, such as the heart-evoked potential4.
This is the first multicenter study to evaluate emotion recognition processes in HHD. Our findings suggest that alterations in this domain are an intrinsic deficit of this disease (irrespective of other cognitive impairments) and that they may be related to deficits in neurocardiac integration dynamics, as indexed by interoceptive disruptions. Our findings thus nurture the theoretical understanding of embodied mechanisms related to emotional processing in healthy subjects while providing critical insights about their alteration on HHD patients. Further efforts in this direction could contribute to improving the clinical evaluation of this deficit and eventually be tested as a critical marker for diagnosing the disease, tracking its evolution, and assessing the patients’ response to treatment.
References
Paulus, M. P., Tapert, S. F. & Schulteis, G. The role of interoception and alliesthesia in addiction. Pharmacol. Biochem. Behav. 94, 1–7. https://doi.org/10.1016/j.pbb.2009.08.005 (2009).
Barret, L. F. How emotions are made: the secret life of the brain. Booklist 113, 4–4 (2017).
Seth, A. K. Interoceptive inference, emotion, and the embodied self. Trends Cognit. Sci. 17, 565–573. https://doi.org/10.1016/j.tics.2013.09.007 (2013).
Yoris, A. et al. Multilevel convergence of interoceptive impairments in hypertension: New evidence of disrupted body-brain interactions. Hum. Brain Mapp. 39, 1563–1581. https://doi.org/10.1002/hbm.23933 (2018).
Couto, B. et al. The man who feels two hearts: the different pathways of interoception. Soc. Cognit. Affect. Neurosci. 9, 1253–1260. https://doi.org/10.1093/scan/nst108 (2014).
McCubbin, J. A. et al. Cardiovascular-emotional dampening: the relationship between blood pressure and recognition of emotion. Psychosom. Med. 73, 743–750. https://doi.org/10.1097/PSY.0b013e318235ed55 (2011).
McCubbin, J. A. et al. Emotional dampening in persons with elevated blood pressure: affect dysregulation and risk for hypertension. Ann. Behav. Med. 47, 111–119. https://doi.org/10.1007/s12160-013-9526-2 (2014).
Shukla, M., Pandey, R., Jain, D. & Lau, J. Y. F. Poor emotional responsiveness in clinical hypertension: reduced accuracy in the labelling and matching of emotional faces amongst individuals with hypertension and prehypertension. Psychol. Health. 33, 765–782. https://doi.org/10.1080/08870446.2017.1401624 (2018).
Quadt, L. Commentary: first-order embodiment, second-order embodiment, third-order embodiment. Front. Psychol. 9, 445. https://doi.org/10.3389/fpsyg.2018.00445 (2018).
Oosterwijk, S. et al. States of mind: emotions, body feelings, and thoughts share distributed neural networks. NeuroImage 62, 2110–2128. https://doi.org/10.1016/j.neuroimage.2012.05.079 (2012).
Seth, A. K. & Friston, K. J. Active interoceptive inference and the emotional brain. Philos. Trans. R. Soc. Lond. B https://doi.org/10.1098/rstb.2016.0007 (2016).
Seth, A. K. & Critchley, H. D. Extending predictive processing to the body: emotion as interoceptive inference. Behav Brain Sci 36, 227–228. https://doi.org/10.1017/S0140525X12002270 (2013).
Consoli, S. M. et al. Differences in emotion processing in patients with essential and secondary hypertension. Am. J. Hypertens. 23, 515–521. https://doi.org/10.1038/ajh.2010.9 (2010).
Herrmann-Lingen, C. & AlAbsi, M. Exploring the Association of Hypertension with risk for depression: evidence for tamed neurobehavioral arousal versus central emotional dysregulation. Psychosom. Med. 80, 504–507. https://doi.org/10.1097/PSY.0000000000000611 (2018).
Brook, R. D. & Rajagopalan, S. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Soc Hypertens 12, 238. https://doi.org/10.1016/j.jash.2018.01.004 (2018).
Li, X. et al. Disrupted frontoparietal network mediates white matter structure dysfunction associated with cognitive decline in hypertension patients. J. Neurosci. 35, 10015–10024. https://doi.org/10.1523/JNEUROSCI.5113-14.2015 (2015).
Rosenberg, H., Dethier, M., Kessels, R. P., Westbrook, R. F. & McDonald, S. Emotion perception after moderate-severe traumatic brain injury: The valence effect and the role of working memory, processing speed, and nonverbal reasoning. Neuropsychology 29, 509–521. https://doi.org/10.1037/neu0000171 (2015).
White, J., Hopkins, R. O., Glissmeyer, E. W., Kitterman, N. & Elliott, C. G. Cognitive, emotional, and quality of life outcomes in patients with pulmonary arterial hypertension. Respir. Res. 7, 55. https://doi.org/10.1186/1465-9921-7-55 (2006).
Lindquist, K. A. The role of language in emotion: existing evidence and future directions. Curr. Opin. Psychol. 17, 135–139. https://doi.org/10.1016/j.copsyc.2017.07.006 (2017).
Lindquist, K. A., Satpute, A. B. & Gendron, M. Does language do more than communicate emotion?. Curr. Dir. Psychol. Sci. 24, 99–108. https://doi.org/10.1177/0963721414553440 (2015).
Barrett, L. F., Lindquist, K. A. & Gendron, M. Language as context for the perception of emotion. Trends Cognit. Sci. 11, 327–332. https://doi.org/10.1016/j.tics.2007.06.003 (2007).
Lindquist, K. A., Barrett, L. F., Bliss-Moreau, E. & Russell, J. A. Language and the perception of emotion. Emotion 6, 125–138. https://doi.org/10.1037/1528-3542.6.1.125 (2006).
Muela, H. C. S. et al. Impact of hypertension severity on arterial stiffness, cerebral vasoreactivity, and cognitive performance. Dement Neuropsychol 11, 389–397. https://doi.org/10.1590/1980-57642016dn11-040008 (2017).
Muela, H. C. S. et al. Higher arterial stiffness is associated with lower cognitive performance in patients with hypertension. J. Clin. Hypertens. (Greenwich) 20, 22–30. https://doi.org/10.1111/jch.13129 (2018).
Muela, H. C. et al. Hypertension severity is associated with impaired cognitive performance. J. Am. Heart. Assoc. 6, 4579. https://doi.org/10.1161/JAHA.116.004579 (2017).
Iadecola, C. et al. Impact of hypertension on cognitive function: a scientific statement from the American Heart Association. Hypertension 68, e67–e94. https://doi.org/10.1161/HYP.0000000000000053 (2016).
Wu, L. et al. The association between the prevalence, treatment and control of hypertension and the risk of mild cognitive impairment in an elderly urban population in China. Hypertens. Res. 39, 367–375. https://doi.org/10.1038/hr.2015.146 (2016).
Reitz, C., Tang, M. X., Manly, J., Mayeux, R. & Luchsinger, J. A. Hypertension and the risk of mild cognitive impairment. Arch. Neurol. 64, 1734–1740. https://doi.org/10.1001/archneur.64.12.1734 (2007).
Couto, B. et al. The man who feels two hearts: the different pathways of interoception. Social cognitive and affective neuroscience 9(9), 1253–1260. https://doi.org/10.1093/scan/nst108 (2013).
Adolfi, F. et al. Convergence of interoception, emotion, and social cognition: A twofold fMRI meta-analysis and lesion approach. Cortex 88, 124–142. https://doi.org/10.1016/j.cortex.2016.12.019 (2016).
Critchley, H. D., Eccles, J. & Garfinkel, S. N. Interaction between cognition, emotion, and the autonomic nervous system. Handb. Clin. Neurol.. 117, 59–77. https://doi.org/10.1016/B978-0-444-53491-0.00006-7 (2013).
Koroboki, E. et al. Interoceptive awareness in essential hypertension. Int. J. Psychophysiol. 78, 158–162. https://doi.org/10.1016/j.ijpsycho.2010.07.003 (2010).
Barrett, L. F. & Simmons, W. K. Interoceptive predictions in the brain. Nat. Rev. Neurosci. 16, 419–429. https://doi.org/10.1038/nrn3950 (2015).
Barrett, L. F. The theory of constructed emotion: an active inference account of interoception and categorization. Soc. Cognit. Affect. Neurosci. 12, 1–23. https://doi.org/10.1093/scan/nsw154 (2017).
Velasco, M. & Israili, Z. Hypertension: from epidemiology to therapeutics. Int. J. Hypertens. 2012, 908431. https://doi.org/10.1155/2012/908431 (2012).
Faul, F. E., Lang, E. & Buchner, A. G. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 39, 175–191 (2007).
Garcia, A. M. et al. Parkinson’s disease compromises the appraisal of action meanings evoked by naturalistic texts. Cortex 100, 111–126. https://doi.org/10.1016/j.cortex.2017.07.003 (2018).
Kim, Y. R., Eom, J. S., Yang, J. W., Kang, J. & Treasure, J. The impact of oxytocin on food intake and emotion recognition in patients with eating disorders: a double blind single dose within-subject cross-over design. PLoS ONE 10, e0137514. https://doi.org/10.1371/journal.pone.0137514 (2015).
Wang, S. et al. The human amygdala parametrically encodes the intensity of specific facial emotions and their categorical ambiguity. Nat Commun 8, 14821. https://doi.org/10.1038/ncomms14821 (2017).
Scholten, M. R., Aleman, A., Montagne, B. & Kahn, R. S. Schizophrenia and processing of facial emotions: sex matters. Schizophr. Res. 78, 61–67. https://doi.org/10.1016/j.schres.2005.06.019 (2005).
Ho, M. W. et al. Impairments in face discrimination and emotion recognition are related to aging and cognitive dysfunctions in Parkinson’s disease with dementia. Sci Rep 10, 4367. https://doi.org/10.1038/s41598-020-61310-w (2020).
Sanchez, R. A. et al. Parallel renal and extremity blood supply abnormalities in nonmodulation: responses to ACE inhibition. Hypertension 41, 919–924. https://doi.org/10.1161/01.HYP.0000062967.90892.5D (2003).
Whelton, P. K. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 71, e13–e115. https://doi.org/10.1161/HYP.0000000000000065 (2018).
Beck, A. T., Steer, R. A., Ball, R. & Ranieri, W. Comparison of Beck Depression Inventories-IA and -II in psychiatric outpatients. J. Pers. Assess. 67, 588–597. https://doi.org/10.1207/s15327752jpa6703_13 (1996).
Torralva, T., Roca, M., Gleichgerrcht, E., Lopez, P. & Manes, F. INECO Frontal Screening (IFS): a brief, sensitive, and specific tool to assess executive functions in dementia. J. Int. Neuropsychol. Soc. 15, 777–786. https://doi.org/10.1017/S1355617709990415 (2009).
Torralva, T. et al. Validation of the Spanish Version of the Addenbrooke’s Cognitive Examination-Revised (ACE-R). Neurologia 26, 351–356. https://doi.org/10.1016/j.nrl.2010.10.013 (2011).
Young, A. W. et al. Facial expression megamix: tests of dimensional and category accounts of emotion recognition. Cognition 63, 271–313. https://doi.org/10.1016/s0010-0277(97)00003-6 (1997).
Ekman, P. Pictures of Facial Affect (Consulting Psychologists Press, Palo Alto, 1976).
Cardona, J. F. et al. The impact of neuromyelitis optica on the recognition of emotional facial expressions: a preliminary report. Soc. Neurosci. 9, 633–638. https://doi.org/10.1080/17470919.2014.935474 (2014).
Baez, S. et al. Contextual social cognition impairments in schizophrenia and bipolar disorder. PLoS ONE 8, e57664. https://doi.org/10.1371/journal.pone.0057664 (2013).
Baez, S. et al. Integrating intention and context: assessing social cognition in adults with Asperger syndrome. Front. Hum. Neurosci. 6, 302. https://doi.org/10.3389/fnhum.2012.00302 (2012).
Baez, S. et al. Theory of mind and its relationship with executive functions and emotion recognition in borderline personality disorder. J. Neuropsychol. 9, 203–218. https://doi.org/10.1111/jnp.12046 (2015).
Gonzalez-Gadea, M. L. et al. Emotion recognition and cognitive empathy deficits in adolescent offenders revealed by context-sensitive tasks. Front. Hum. Neurosci. 8, 850. https://doi.org/10.3389/fnhum.2014.00850 (2014).
Baez, S. et al. Impairments in negative emotion recognition and empathy for pain in Huntington’s disease families. Neuropsychologia 68, 158–167. https://doi.org/10.1016/j.neuropsychologia.2015.01.012 (2015).
Zimmerman, D. W. Power comparisons of significance tests of location using scores, ranks, and modular ranks. Br. J. Math. Stat. Psychol. 64, 233–243. https://doi.org/10.1348/000711010X501671 (2011).
Zimmerman, D. W. Increasing the power of nonparametric tests by detecting and downweighting outliers. J. Exp. Educ. 1, 71–78 (1995).
Osborne, J. W. & Overbay, A. The power of outliers (and why researchers should ALWAYS check for them). Pract. Assess. Res. Eval. https://doi.org/10.7275/qf69-7k43 (2004).
Garfinkel, S. N. & Critchley, H. D. Interoception, emotion and brain: new insights link internal physiology to social behavior. Commentary on: “Anterior insular cortex mediates bodily sensibility and social anxiety” by Terasawa et al. (2012). Soc. Cognit. Affect. Neurosci. 8, 231–234 (2013).
Melloni, M. et al. Preliminary evidence about the effects of meditation on interoceptive sensitivity and social cognition. Behav. Brain Funct. 9, 47. https://doi.org/10.1186/1744-9081-9-47 (2013).
Sedeno, L. et al. How do you feel when you can’t feel your body? Interoception, functional connectivity and emotional processing in depersonalization-derealization disorder. PLoS ONE 9, e98769. https://doi.org/10.1371/journal.pone.0098769 (2014).
Garcia-Cordero, I. et al. Feeling, learning from and being aware of inner states: interoceptive dimensions in neurodegeneration and stroke. Philos. Trans. R. Soc. Lond. B https://doi.org/10.1098/rstb.2016.0006 (2016).
Yoris, A. et al. The roles of interoceptive sensitivity and metacognitive interoception in panic. Behav.. Brain Funct. 11, 14. https://doi.org/10.1186/s12993-015-0058-8 (2015).
Yoris, A. et al. The inner world of overactive monitoring: neural markers of interoception in obsessive–compulsive disorder. Psychol. Med. 17, 1–14 (2017).
de la Fuente, A. et al. Multimodal neurocognitive markers of interoceptive tuning in smoked cocaine. Neuropsychopharmacology 44, 1425–1434. https://doi.org/10.1038/s41386-019-0370-3 (2019).
Garfinkel, S. N., Seth, A. K., Barrett, A. B., Suzuki, K. & Critchley, H. D. Knowing your own heart: distinguishing interoceptive accuracy from interoceptive awareness. Biol. Psychol. 104, 65–74 (2015).
Ring, C. & Brener, J. Heartbeat counting is unrelated to heartbeat detection: A comparison of methods to quantify interoception. Psychophysiology 55, e13084. https://doi.org/10.1111/psyp.13084 (2018).
Brener, J. & Ring, C. Towards a psychophysics of interoceptive processes: the measurement of heartbeat detection. Philos. Trans. R. Soc. Lond. B https://doi.org/10.1098/rstb.2016.0015 (2016).
Couto, B. et al. Heart evoked potential triggers brain responses to natural affective scenes: a preliminary study. Autonomic Neurosci. https://doi.org/10.1016/j.autneu.2015.06.006 (2015).
Desmedt, O., Luminet, O. & Corneille, O. The heartbeat counting task largely involves non-interoceptive processes: evidence from both the original and an adapted counting task. Biol. Psychol. 138, 185–188. https://doi.org/10.1016/j.biopsycho.2018.09.004 (2018).
Zamariola, G., Maurage, P., Luminet, O. & Corneille, O. Interoceptive accuracy scores from the heartbeat counting task are problematic: evidence from simple bivariate correlations. Biol. Psychol. 137, 12–17. https://doi.org/10.1016/j.biopsycho.2018.06.006 (2018).
Corneille, O., Desmedt, O., Zamariola, G., Luminet, O. & Maurage, P. A heartfelt response to Zimprich et al. (2020), and Ainley et al. (2020)’s : acknowledging issues with the HCT would benefit interoception research. Biol Psychol 152, 107869. https://doi.org/10.1016/j.biopsycho.2020.107869 (2020).
Ainley, V. et al. Comment on Zamariola et al. (2018) Interoceptive accuracy scores are problematic: evidence from simple bivariate correlations: the empirical data base, the conceptual reasoning and the analysis behind this statement are misconceived and do not support the authors’ conclusions. Biol. Psychol. 152, 107870. https://doi.org/10.1016/j.biopsycho.2020.107870 (2020).
Zimprich, D., Nusser, L. & Pollatos, O. Are interoceptive accuracy scores from the heartbeat counting task problematic? A comment on Zamariola et al. (2018). Biol. Psychol. 152, 107868. https://doi.org/10.1016/j.biopsycho.2020.107868 (2020).
Fittipaldi, S. et al. A multidimensional and multi-feature framework for cardiac interoception. NeuroImage 212, 116677. https://doi.org/10.1016/j.neuroimage.2020.116677 (2020).
Noordewier, M. K. & Breugelmans, S. M. On the valence of surprise. Cognit. Emot. 27, 1326–1334. https://doi.org/10.1080/02699931.2013.777660 (2013).
Noordewier, M. K. & van Dijk, E. Surprise: unfolding of facial expressions. Cognit. Emot. 33, 915–930. https://doi.org/10.1080/02699931.2018.1517730 (2019).
Eid, M., Gollwitzer, M. & Schmitt, M. Statistik und Forschungsmethoden Lehrbuch. (2011).
Lenhard, W. & Lenhard, A. Psychometrica (Bibergau, Bayern, 2014).
Zhang, J., Teo, T. & Wu, C. Emotion words modulate early conflict processing in a flanker task: differentiating emotion-label words and emotion-laden words in second language. Lang. Speech 62, 641–651. https://doi.org/10.1177/0023830918807509 (2019).
Lindquist, K. A., MacCormack, J. K. & Shablack, H. The role of language in emotion: predictions from psychological constructionism. Front. Psychol. 6, 444. https://doi.org/10.3389/fpsyg.2015.00444 (2015).
An, S., Ji, L. J., Marks, M. & Zhang, Z. Two sides of emotion: exploring positivity and negativity in six basic emotions across cultures. Front. Psychol. 8, 610. https://doi.org/10.3389/fpsyg.2017.00610 (2017).
An, S. et al. Neural activation in response to the two sides of emotion. Neurosci. Lett. 684, 140–144. https://doi.org/10.1016/j.neulet.2018.07.011 (2018).
Kemp, A. H. et al. Effects of depression, anxiety, comorbidity, and antidepressants on resting-state heart rate and its variability: an ELSA-Brasil cohort baseline study. Am. J. Psychiatry 171, 1328–1334 (2014).
Kemp, A. H., Quintana, D. S., Felmingham, K. L., Matthews, S. & Jelinek, H. F. Depression, comorbid anxiety disorders, and heart rate variability in physically healthy, unmedicated patients: implications for cardiovascular risk. PLoS ONE 7, e30777. https://doi.org/10.1371/journal.pone.0030777 (2012).
Kemp, A. H. et al. Impact of depression and antidepressant treatment on heart rate variability: a review and meta-analysis. Biol. Psychiatry 67, 1067–1074. https://doi.org/10.1016/j.biopsych.2009.12.012 (2010).
Arias, J. M. et al. The Neuroscience of Sadness: A Multidisciplinary Synthesis and Collaborative Review for the Human Affectome Project (Elsevier, Amsterdam, 2020).
Marci, C. D., Glick, D. M., Loh, R. & Dougherty, D. D. Autonomic and prefrontal cortex responses to autobiographical recall of emotions. Cognit. Affect. Behav. Neurosci. 7, 243–250 (2007).
McGaugh, J. L. The amygdala modulates the consolidation of memories of emotionally arousing experiences. Annu. Rev. Neurosci. 27, 1–28. https://doi.org/10.1146/annurev.neuro.27.070203.144157 (2004).
Critchley, H. D. et al. Activity in the human brain predicting differential heart rate responses to emotional facial expressions. NeuroImage 24, 751–762. https://doi.org/10.1016/j.neuroimage.2004.10.013 (2005).
Garfinkel, S. N. & Critchley, H. D. Threat and the body: how the heart supports fear processing. Trends Cognit. Sci. 20, 34–46 (2016).
Gentsch, A., Sel, A., Marshall, A. C. & Schutz-Bosbach, S. Affective interoceptive inference: evidence from heart-beat evoked brain potentials. Hum. Brain Mapp. https://doi.org/10.1002/hbm.24352 (2018).
Herbert, B. M., Herbert, C. & Pollatos, O. On the relationship between interoceptive awareness and alexithymia: is interoceptive awareness related to emotional awareness?. J. Pers. 79, 1149–1175. https://doi.org/10.1111/j.1467-6494.2011.00717.x (2011).
Levy, J., Goldstein, A., Pratt, M. & Feldman, R. Maturation of pain empathy from child to adult shifts from single to multiple neural rhythms to support interoceptive representations. Sci. Rep. 8, 1810. https://doi.org/10.1038/s41598-018-19810-3 (2018).
Schaan, L. et al. Interoceptive accuracy, emotion recognition, and emotion regulation in preschool children. Int. J. Psychophysiol. 138, 47–56. https://doi.org/10.1016/j.ijpsycho.2019.02.001 (2019).
Terasawa, Y., Moriguchi, Y., Tochizawa, S. & Umeda, S. Interoceptive sensitivity predicts sensitivity to the emotions of others. Cognit. Emot. 28, 1435–1448. https://doi.org/10.1080/02699931.2014.888988 (2014).
Zaki, J., Davis, J. I. & Ochsner, K. N. Overlapping activity in anterior insula during interoception and emotional experience. NeuroImage 62, 493–499. https://doi.org/10.1016/j.neuroimage.2012.05.012 (2012).
Garfinkel, S. N. et al. Fear from the heart: sensitivity to fear stimuli depends on individual heartbeats. J. Neurosci. 34, 6573–6582 (2014).
Fukushima, H., Terasawa, Y. & Umeda, S. Association between interoception and empathy: evidence from heartbeat-evoked brain potential. Int. J. Psychophysiol. 79, 259–265 (2011).
Sel, A., Azevedo, R. T. & Tsakiris, M. Heartfelt self: cardio-visual integration affects self-face recognition and interoceptive cortical processing. Cereb. Cortex 27, 5144–5155. https://doi.org/10.1093/cercor/bhw296 (2017).
Shao, S., Shen, K., Wilder-Smith, E. P. & Li, X. Effect of pain perception on the heartbeat evoked potential. Clin. Neurophysiol. 122, 1838–1845. https://doi.org/10.1016/j.clinph.2011.02.014 (2011).
Wiebking, C. et al. Abnormal body perception and neural activity in the insula in depression: an fMRI study of the depressed “material me”. World J. Biol. Psychiatry 11, 538–549. https://doi.org/10.3109/15622970903563794 (2010).
Salamone, P. C. et al. Altered neural signatures of interoception in multiple sclerosis. Hum. Brain Mapp. 39, 4743–4754. https://doi.org/10.1002/hbm.24319 (2018).
Critchley, H. D. & Harrison, N. A. Visceral influences on brain and behavior. Neuron 77, 624–638 (2013).
Critchley, H. D., Wiens, S., Rotshtein, P., Ohman, A. & Dolan, R. J. Neural systems supporting interoceptive awareness. Nat. Neurosci. 7, 189–195 (2004).
Quadt, L., Critchley, H. D. & Garfinkel, S. N. The neurobiology of interoception in health and disease. Ann. N. Y. Acad. Sci. 1428, 112–128. https://doi.org/10.1111/nyas.13915 (2018).
Hoemann, K., Gendron, M. & Barrett, L. F. Mixed emotions in the predictive brain. Curr. Opin. Behav. Sci. 15, 51–57. https://doi.org/10.1016/j.cobeha.2017.05.013 (2017).
Allen, M. & Friston, K. J. From cognitivism to autopoiesis: towards a computational framework for the embodied mind. Synthese 195, 2459–2482. https://doi.org/10.1007/s11229-016-1288-5 (2018).
Allen, M., Levy, A., Parr, T. & Friston, K. J. In the body’s eye: the computational anatomy of interoceptive inference. BioRxiv 2019, 603928 (2019).
Rau, H. & Elbert, T. Psychophysiology of arterial baroreceptors and the etiology of hypertension. Biol. Psychol. 57, 179–201 (2001).
Barrett, L. F. The theory of constructed emotion: an active inference account of interoception and categorization. Soc. Cognit. Affect. Neurosci. 12, 1833. https://doi.org/10.1093/scan/nsx060 (2017).
Damasio, A. The Strange Order of Things: Life, Feeling, and the Making of Cultures (Pantheon Books, New York, 2018).
Steiger, J. H. Testing pattern hypotheses on correlation matrices: alternative statistics and some empirical results. Multivar. Behav. Res 15, 335–352. https://doi.org/10.1207/s15327906mbr1503_7 (1980).
Craig, A. D. How do you feel? Interoception: the sense of the physiological condition of the body. Nat. Rev. Neurosci. 3, 655–666. https://doi.org/10.1038/nrn894 (2002).
Zamariola, G., Frost, N., Van Oost, A., Corneille, O. & Luminet, O. Relationship between interoception and emotion regulation: new evidence from mixed methods. J. Affect. Disord. 246, 480–485. https://doi.org/10.1016/j.jad.2018.12.101 (2019).
Sel, A. Predictive codes of interoception, emotion, and the self. Front. Psychol. 5, 189. https://doi.org/10.3389/fpsyg.2014.00189 (2014).
Critchley, H. D. & Garfinkel, S. N. Interoception and emotion. Curr. Opin. Psychol. 17, 7–14. https://doi.org/10.1016/j.copsyc.2017.04.020 (2017).
Craig, A. D. Interoception: the sense of the physiological condition of the body. Curr. Opin. Neurobiol. 13, 500–505 (2003).
Yoris, A. E. et al. Neurocardiología: Aspectos Fisiopatológicos e Implicancias Clínicas (Elsevier, Amsterdam, 2018).
Yoris, A. et al. In The Interoceptive Basis of the Mind (eds Tsakiris, M. & De Preester, H.) (Oxford University Press, Oxford, 2018).
Craig, A. How Do You Feel? (An Interoceptive Moment with Your Neurobiological Self. Princeton University Press, Princeton, 2015).
Shah, P., Catmur, C. & Bird, G. From heart to mind: Linking interoception, emotion, and theory of mind. Cortex 93, 220–223. https://doi.org/10.1016/j.cortex.2017.02.010 (2017).
Farmer, M. E. et al. Longitudinally measured blood pressure, antihypertensive medication use, and cognitive performance: the Framingham Study. J. Clin. Epidemiol. 43, 475–480 (1990).
Scherr, P. A., Hebert, L. E., Smith, L. A. & Evans, D. A. Relation of blood pressure to cognitive function in the elderly. Am. J. Epidemiol. 134, 1303–1315 (1991).
Van Boxtel, M. P. et al. Can the blood pressure predict cognitive task performance in a healthy population sample?. J. Hypertens. 15, 1069–1076 (1997).
Nitkunan, A. et al. Diffusion tensor imaging and MR spectroscopy in hypertension and presumed cerebral small vessel disease. Magn. Reson. Med. 59, 528–534 (2008).
Hannesdottir, K. et al. Cognitive impairment and white matter damage in hypertension: a pilot study. Acta Neurol. Scand. 119, 261–268 (2009).
Gons, R. A. et al. Hypertension and cerebral diffusion tensor imaging in small vessel disease. Stroke 41, 2801–2806 (2010).
Committee, G. 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J. Hypertens. 21, 1011–1053 (2003).
Hermida, R. C. et al. Circadian rhythms in blood pressure regulation and optimization of hypertension treatment with ACE inhibitor and ARB medications. Am. J. Hypertens. 24, 383–391 (2011).
Aviezer, H., Ensenberg, N. & Hassin, R. R. The inherently contextualized nature of facial emotion perception. Curr. Opin. Psychol. 17, 47–54. https://doi.org/10.1016/j.copsyc.2017.06.006 (2017).
Kazanas, S. A. & Altarriba, J. The automatic activation of emotion and emotion-laden words: evidence from a masked and unmasked priming paradigm. Am. J. Psychol. 128, 323–336. https://doi.org/10.5406/amerjpsyc.128.3.0323 (2015).
Wang, X., Shangguan, C. & Lu, J. Time course of emotion effects during emotion-label and emotion-laden word processing. Neurosci. Lett. 699, 1–7. https://doi.org/10.1016/j.neulet.2019.01.028 (2019).
Zhang, J., Wu, C., Meng, Y. & Yuan, Z. Different neural correlates of emotion-label words and emotion-laden words: an ERP study. Front. Hum. Neurosci. 11, 455. https://doi.org/10.3389/fnhum.2017.00455 (2017).
Zhang, J., Wu, C., Yuan, Z. & Meng, Y. Differentiating emotion-label words and emotion-laden words in emotion conflict: an ERP study. Exp. Brain Res. 237, 2423–2430. https://doi.org/10.1007/s00221-019-05600-4 (2019).
Lindquist, K. A., Gendron, M., Oosterwijk, S. & Barrett, L. F. Do people essentialize emotions? Individual differences in emotion essentialism and emotional experience. Emotion 13, 629–644. https://doi.org/10.1037/a0032283 (2013).
Bekinschtein, T. A. et al. In ACNS-2013 Australasian Cognitive Neuroscience Society Conference. (2013).
Khalsa, S. S., Rudrauf, D., Feinstein, J. S. & Tranel, D. The pathways of interoceptive awareness. Nat. Neurosci. 12, 1494–1496. https://doi.org/10.1038/nn.2411 (2009).
Khalsa, S. S., Rudrauf, D. & Tranel, D. Interoceptive awareness declines with age. Psychophysiology 46, 1130–1136. https://doi.org/10.1111/j.1469-8986.2009.00859.x (2009).
Garcia-Cordero, I. et al. Attention, in and out: scalp-level and intracranial EEG correlates of interoception and exteroception. Front. Neurosci. 11, 411. https://doi.org/10.3389/fnins.2017.00411 (2017).
Acknowledgements
This work was partially supported by CONICET; FONCYT-PICT [grant numbers 2017-1818, 2017-1820]; CONICYT/FONDECYT Regular [grant number 1170010]; FONDAP [grant number 15150012]; the INECO Foundation; the Inter-American Development Bank (IDB); Programa Interdisciplinario de Investigación Experimental en Comunicación y Cognición (PIIECC), Facultad de Humanidades, USACH; GBHI ALZ UK-20-639295; and the Multi-Partner Consortium to Expand Dementia Research in Latin America (ReDLat), funded by the National Institutes of Aging of the National Institutes of Health under award number R01AG057234, an Alzheimer’s Association grant (SG-20-725707-ReDLat), the Rainwater Foundation, and the Global Brain Health Institute. The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health, Alzheimer’s Association, Rainwater Charitable Foundation, or Global Brain Health Institute.
Author information
Authors and Affiliations
Contributions
A.Y. and J.L.P. collected the data, statistically analyzed the data, and wrote the first draft of the manuscript. S.Al. collected the data. S.Ab. and A.L. statistically analyzed the data. A.I. was involved in the study conception and design, writing the protocol, and contributed to the manuscript draft. R.S. contributed in collecting the data and revising the final version of the manuscript. L.S., A.I., A.M.G. and A.Y. contributed to revising the final version of the manuscript. L.S. was involved in the study conception and design and contributed to writing the final version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yoris, A., Legaz, A., Abrevaya, S. et al. Multicentric evidence of emotional impairments in hypertensive heart disease. Sci Rep 10, 14131 (2020). https://doi.org/10.1038/s41598-020-70451-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-70451-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.