Abstract
Next generation sequencing (NGS) together with protein expression analysis is back bone of molecularly targeted therapy in precision medicine. Our retrospective study shows our experience with NGS of 324 genes in combination with protein expression in patients with advanced breast cancer (aBC). The primary purpose was to analyze the prevalence of individual genetic alterations combined with protein expression to define potential targets for an individualized therapy. Between April 2018 and September 2019, 41 patients with aBC were offered a NGS test. The test was used to detect clinically relevant genomic alterations and to support further targeted therapy decisions. Hormone receptors, ERBB2 of tumors and PD-L1 was stained by immunohistochemistry. The data was recorded up to September 2019. After prior consent 41 results were available for further analysis. The most common BC subtypes were triple-negative (n = 16), HR+/ERBB2− (n = 15), and ERBB2+ (n = 9), with one missing data of the primary tumor. 27 patients had more than one genetic alteration. The most common alterations were PIK3CA (n = 14) and ERBB2 alterations (n = 11). Followed by ESR1 (n = 10), FGFR1 (n = 7) and PTEN (n = 7). 68% of the alterations were clinically relevant (tier I and II of ESCAT classification). The most common treatment recommendation was ERBB2-directed therapy (single or double blockade, trastuzumab emtansine and lapatinib) followed by alpelisib in combination with fulvestrant. Comprehensive genomic profiling combined with protein expression analysis in aBC allowed a guided personalized therapy for half of our patients. So far there are no well-defined tools allowing interpretations of genomic alterations detected by NGS in combination with protein expression and other factors.
Similar content being viewed by others
Purpose
The traditional risk and treatment assessment of primary breast cancer was traditionally based on tumor size, lymph node involvement, grading and proliferation index according to the Ki67, and hormone receptor and ERBB2 amplification status1. The recommendation for treatment strategies in the (neo-)adjuvant setting of breast cancer therapy was improved due to the implementation of multi gene expression tests such as Oncotype DX and EndoPredict tests in selective patients’ cohorts.
Spite of these advances in molecular analysis of primary tumor genotypes, in the setting of advanced disease, molecular genetic-based biomarkers are not used routinely. With the publication of Perou et al., BC was classified according to its molecular profile in intrinsic subtypes2. These subtypes differ in their response to systemic treatment and short-/long-term prognosis. Based on these intrinsic subtypes, further understanding of the genetic alterations and pathways has been gained. This increased knowledge has led to the development of therapies targeting special genetic alterations in tumor cells or cells within the microenvironment of a tumor. Alpelisib and Olaparib are two targeted therapies recently approved by the FDA accordingly to the mutational status of tumor. Alpelisib3,4 is indicated in HR+/ERBB2− metastatic breast cancer with PIC3CA mutation and Olaparib5 is approved for treatment of germline BRCA mutated advanced disease.
Germline mutations of BRCA gene can be detected in approximately 5% of all breast cancers5. These patients benefit from PARP inhibitors like Olaparib6. The clinical evidence of somatic BRCA mutation in mBC is unclear and could depend from the detected mutant allele fraction (MAF).
So far there are no well-defined tools that allow interpretations of genomic alterations detected by NGS in combination with protein expression of tumor7. However, there are different frameworks that assign individual gene alterations and corresponding treatments, classified into tiers by the evidence strength from clinical studies; the most established so far is the ESMO Scale for Clinical Actionability of molecular Targets (ESCAT).
In this explorative analysis we present the data of our advanced BC patients and their treatment options based on a solid tumor genomic profiling in conjunction with protein expression. The applied FoundationOne CDx is based on Illumina platform, that has been approved by the FDA on November 30, 20178.
Methods
Starting from April 2018, our cancer center has had access to a hybrid capture based NGS service platform (FoundationOne CDx) for solid tumor samples and subsequently offered this service to patients with advanced disease. The test has been FDA approved for breast cancer since 2017. The test was used to detect clinically relevant genomic alterations (point mutations, indels, rearrangements, and CNAs), and to support the selection of an appropriate targeted therapy by the physicians. The assay interrogates 324 genes, as well as introns of 34 genes involved in rearrangements9 and does also report Tumor Mutational Burden (TMB)10 as well as Microsatellite Instability (MSI)11. Results provide a comprehensive molecular tumor profile, as previously described elsewhere12,13. For each tumor profile, individual therapy options are provided according to the current state of scientific knowledge and approval.
Patients characteristics
From April 2018 up to September 2019, a total of 335 samples were analyzed after receiving informed patient consent of patients for scientific purposes with an advanced solid tumor. We collected 41 samples originating from metastatic sites of patients with advanced breast cancer. Histopathological and immunohistochemical examination of sample confirmed the primary diagnosis of breast cancer. The final database included 41 successfully analyzed BC samples harboring alterations and protein expression (HR, ERBB2 in immune cells, PD-L1) by IHC (Addendum A).
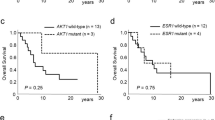
Patient´s characteristics including age, primary tumor subtype, grading, site of metastasis and previous therapies were retrospectively analyzed and correlated with genomic alterations and protein expression and potential treatment options. The results of hormonal assessment for ER, PR, and ERBB2 were dichotomized into negative versus positive. PD-L1 status was determined by using Combined Positive Score (CPS) and Tumor Proportion Score (TPS) with different antibody clones (SP263, SP142 and CAL10). Genomic alterations were clustered into belonging signaling pathways and further analyzed by measures of central tendency. Due to the short follow-up interval of 1.5 years (April 2018–September 2019), a clinical follow up after molecular based treatment decision is not reportable at time and not the primary endpoint of study.
Results
Starting in April 2018 up to September 2019, n = 41, advanced BC patients were offered the solid tumor genomic profiling test FoundationOne CDx. The patient’s characteristics including clinicopathological profile are summarized in Table 1. Our cohort of patients included 100% female with a median age at diagnosis of 50 (range 31–84) and except for one woman, they were all in a postmenopausal status. The most common BC subtypes were triple-negative (n = 16), followed by HR+ (n = 15), and ERBB2+ BC (n = 9). In our cohort, the average number of metastatic sites per patient was more than 2. In four patients, PD-L1 status was positive (> 1% score), with a tumor grading G2 (n = 2) and G3 (n = 2).
Bone-only metastases were present in three patients, making it the most frequent single-site of metastases (out of seven patients in total). Visceral-only metastases were detected in fifteen patients, and others (skin, brain) in three. Almost the half of the patients (n = 20) had a metastatic dissemination of both sites, bone and visceral metastases.
The majority of our patients had received at least one line of therapy before molecular profiling (78%), and almost a third (29.3%) received more than two lines. Previous therapies consisted in sequential chemo- and hormonal therapy; 43% of patients received chemotherapy in the first line and 4.9% a hormonal therapy in 4.9%.
Overall, 41 different genetic alterations were reported (Fig. 1a). MSI was detected by a single case (2.4%).
The prevalence of individual genetic alterations detected in our BC cohort (n = 41) was comparable to results obtained from a significantly larger database (n = 3,871)14, as summarized in Table 2. There was an average of 2.7 genomic alterations per metastatic patient. Most patients had more than one alteration (n = 27; 66%), and therefore more treatment options available. The most common alterations were PIK3CA (n = 14) and ERBB2 (n = 11), followed by ESR1 (n = 10), FGFR1 (n = 7) and PTEN (n = 7), as shown by Fig. 1b.
The most frequently altered oncogenic signaling pathway in our cohort was RTK/RAS (81.4%), comprised of ERBB2 in 33.3%, FGFR1 in 21.2% and NF1 in 15.2%. PI3K/mTOR/AKT mammalian target of rapamycin (mTOR) pathway alteration was detected in 65.8% of cases, most frequently by PIK3CA alteration (52%), followed by PTEN (26%) and AKT1 (11%). Cell-cycle related pathway alterations were observed in 19.5% of cases, including alterations of CCND1 (62.5%), AURKA (25%) and CDK4 (12.5%). 14% of the patients had alterations in the DNA repair pathway with BRCA1 and PALB2 alterations. Alterations in p53 pathway were detected in 12.2% of patients; MDM2 (40%), MDM4 (40%), TP53 (20%). At the same frequency of 12.2%, was an alteration in MYC oncogenic pathway, encompassing only an alteration in the MYC gene. At 4.8% of incidence, there was alteration in the HIPPO pathway (NF2 alteration). The results are shown in Fig. 1c below.
We further classified our patient’s individual recurrent genomic alterations based on the strength of evidence from clinical studies, according to the ESMO Scale for Clinical Actionability of molecular Targets (ESCAT)7,15, as an aid of prioritizing the treatments. Table 3 provides a list of actionable and biologically relevant alterations detected in our cohort. Strictly focusing on the tier subset of clinically actionable genetic targets, 68.3% of patients harbored at least one such an alteration, (e.g. PIK3CA or ERBB2), and therefore belonged to tier I/tier II group, while 17% had a single-only actionable alteration. 12.2% of our patients belonged to tier III and 46.3% belonged to tier IV of ESCAT Classification. As of the genetic targets without evidence of clinical actionability, 25.6% of patients were belonging to the tier X subset, due to the presence of CCND1 and FGFR1 alterations.
In the clinics these NGS results were discussed at the multidisciplinary team meeting with the clinical case. The treatment options, the side effects and the patients quality of life were considered and in 31.7% the final treatment recommendations included the NGS findings.
Relevant gene alterations for treatment
9/11 (82%) patients with ERBB2 alteration showed an amplification by NGS and received an ERBB2 directed antibody therapy. Two patients showed an ERBB2 mutation (L755S, A775_G776insYVMA), with treatment recommendation of osimertinib and afatinib or neratinib respectively.
8/14 (57%) patients with PIK3CA mutation were HR+/ERBB2−. The ERBB2 negativity of the tumor was detected by IHC or FISH and was confirmed by NGS for all eight patients. For this group of patients alectinib + fulvestrant was recommended. Three patients with PIK3CA mutation were TNBC. Ten patients harbored ESR1 gene alteration, for which everolimus + anastrozole is recommended. As for FGFR1 amplification, present in seven patients, aromatase inhibitors are recommended.
MSI was detected in one single case (2.4%). This patient was HR+/ERBB2− and progressive after endocrine and chemotherapy. Recommendation of MTB was pembrolizumab16.
The most common treatment option taken the information of molecular gene alterations and protein expression together was an ERBB2 based therapy followed by alpelisib in a combination with fulvestrant in postmenopausal and trastuzumab emtansine in premenopausal patients.
Discussion
With the broad availability of DNA sequencing techniques, each patient can undergo the detection of the most common genetic alterations, which can be therapeutically targeted to achieve the best tumor response. To find the best treatment decision both the detection of potentially drugable gene alterations and information about protein expression has to be analyzed in the account.
The classical example of this approach is the recent approval of alpelisib3. PIK3CA mutations are identified in 40% of BC patients, mainly hormone receptor-positive and ERBB2−4,17. Recently in the SOLAR-1 trial the efficacy of the combination of alpelisib with fulvestrant in PIK3CA altered ER+ advanced BC was shown, and subsequently, the combination received the approval by FDA18. Therefore, this genomic alteration belongs to tier I of ESCAT classification, meaning that targets are implemented in clinical routine decisions. In our study, FoundationOne CDx could identify 14 patients (34%) who had PIK3CA mutation; but only 8 patients were HR+ and got the recommendation for alpelisib + fulvestrant. Three patients harbouring PIK3CA mutation were TNBC, and therefore, oral AKT inhibitor capivasertib was recommended to them19,20.
In our data an ERBB2 amplification was found in nine patients with NGS compared with only seven ERBB2 positive cases analysed by IHC or FISH. It is necessary to find a threshold on basis of CNV which allows a better interpretation of NGS based amplification analysis. Two ERBB2 mutations were detected in our cohort, namely A775_G776insYVMA insertion and L755S. ERBB2 A775_G776insYVMA results in a gain of function as well due to insertion of four amino acids in the protein kinase domain of the ERBB2 protein between amino acids 775 and 776. This results in an increased phosphorylation of ERBB2 and an activation of downstream signaling. Afatinib and neratinib were shown to be active for this mutation in vitro21. L755P and L755S are the most common ERBB2 mutations in mBC and leads to oncogenic transformation in cell culture assay. L755S mutation lies within the protein kinase domain and results in increased phosphorylation of ERBB2 and an activation of downstream signaling. L755S is associated with resistance to ERBB2 targeted therapy. Osimertinib demonstrated good efficacy against L755P and L755S mutations, the most common mutations in breast cancer21.
MSI is rare event in breast cancer, but patients with MSI mBC seems to benefit from pembrolizumab as recently reported16.
As an example of an alteration belonging to tier II, there is ESR1. Tumor cells with ESR1 gene alteration are considered poor responders to aromatase inhibitors22. All ESR1 mutations were found in the initial hormone receptor-positive tumors; possibly explaining the recurrence and helping clinicians to recommend more efficient anti-hormonal treatment (i.e. everolimus, temsirolimus) instead of changing the anti-hormonal treatment.
The FGFR1 amplification is considered responsible for non-responding to tamoxifen23, and it was found in seven patients; categorized under tier X of ESCAT classification.
14% of the patients had alterations in the DNA repair pathway with BRCA and PALB2 alterations. PARP inhibitors are just approved for germline mutations. Basket trials are necessary to better understand the role of ERBB2 mutations, somatic alterations in DNA repair pathway and MSI in mBC.
Since these alterations are rare events, analysis of real-world data is necessary for an appropriate recruitment of basket trial. In consequence, the OnkoVision alliance was founded to develop an artificial intelligence (AI) based decision support platform to introduce molecular tumor boards in clinical routine. The platform should help to define treatment options for precision medicine based on factors such as druggable gene alterations, coexisting gene alterations, copy number alterations, MAF and protein expression.
Our NGS analysis prevented further antihormonal treatment for three patients and suggested the most promising treatment with tyrosine kinase inhibitors, due to the lack of evidence of targeted treatments.
Mutational evolution is a known phenomenon in cancer genetics. The change in the hormonal profile of breast cancers has been proved by studies in the past24. In the German national oncology guidelines25, a re-testing of every metastasis is recommended for hormone receptors and ERBB2 expression. All patients in our study underwent re-testing of hormonal profile with conventional techniques and those results were compared with the results of NGS. With tumour progress mutations change from the primary tumour to the metastasis. In most early stages the adjuvant therapy cures the patient from the cancer. The extensive phenotypic heterogeneity of breast cancer is currently researched extensively26. Clinically this would warrant a retesting of every metastasis as early as possible in the treatment lines. But clinical trials need to provide the evidence for such recommendations. Here our analysis adds to the clinical implementation data of NGS.
Fourteen of our patients (34.1%) had only one detectable alteration, regardless of whether actionable or non-actionable. This set of single-only detectable mutations harbored nine different mutations, underlining the clinical difficulty to recommend an effective treatment by conventional means. The use of NGS in the metastatic situation is beneficial for treatment decisions from our point of view. Because of the limited sample size and short duration of follow-up, assessment of progression-free survival and overall survival is too premature. However, our data shows how molecular analysis of advanced cancers could identify genomic alterations. This will identify possible drugable known cancer-driving pathways. Although our study comprised only 41 patients, the results are consistent with the prevalence of individual genetic alterations in BC, as compared to a larger database.
Now that we can individualize the treatment according to the tumor genomic alterations, the next step will be to prove its benefits for patients. Treatment options are more and more focused on genomic alterations, but not essentially approved across multiple tumor types, thus increasing the difficulty for clinicians to either treat the pathways or withhold treatment options as they are not approved within a given tumor type.
Conclusion
The NGS of mBC supports the decision for the most promising treatment option in 58.5% of our patients with a Tier I evidence. For an appropriate treatment decision, it is necessary to evaluate gene alterations and protein expression of metastases in account. For an appropriate interpretation of rare gene alterations in mBC, basket trials on basis of real-world data are necessary. We founded the OnkoVision alliance to bring MTB into clinically routine and to identify appropriate patients for basket trials.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Experimental protocols were approved by the institutional ethic committee of the Cancer Center Dachau.
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
Viale, G. The current state of breast cancer classification. Ann. Oncol. 23, x207–x210 (2012).
Perou, C. M. et al. Molecular portraits of human breast tumours. Nature 406, 747–752 (2000).
Markham, A. Alpelisib: First global approval. Drugs 79, 1249–1253 (2019).
André, F. et al. Alpelisib for PIK3CA-mutated, hormone receptor-positive advanced breast cancer. N. Engl. J. Med. 380, 1929–1940 (2019).
Robson, M. et al. Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. N. Engl. J. Med. 377, 523–533 (2017).
Gonzalez-Angulo, A. M. et al. Incidence and outcome of BRCA mutations in unselected patients with triple receptor-negative breast cancer. Clin. Cancer Res. 17, 1082–1089 (2011).
Condorelli, R. et al. Genomic alterations in breast cancer: Level of evidence for actionability according to ESMO Scale for Clinical Actionability of molecular Targets (ESCAT). Ann. Oncol. 30, 365–373 (2019).
Allegretti, M. et al. Tearing down the walls: FDA approves next generation sequencing (NGS) assays for actionable cancer genomic aberrations. J. Exp. Clin. Cancer Res. 37, 47 (2018).
Frampton, G. M. et al. Development and validation of a clinical cancer genomic profiling test based on massively parallel DNA sequencing. Nat. Biotechnol. 31, 1023–1031 (2013).
Chalmers, Z. R. et al. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med. 9, 34 (2017).
Hall, M. J. et al. Evaluation of microsatellite instability (MSI) status in gastrointestinal (GI) tumor samples tested with comprehensive genomic profiling (CGP). J. Clin. Oncol. 34, 528–528 (2016).
Drilon, A. et al. Broad, hybrid capture-based next-generation sequencing identifies actionable genomic alterations in lung adenocarcinomas otherwise negative for such alterations by other genomic testing approaches. Clin. Cancer Res. 21, 3631–3639 (2015).
Rozenblum, A. B. et al. Clinical impact of hybrid capture-based next-generation sequencing on changes in treatment decisions in lung cancer. J. Thorac. Oncol. 12, 258–268 (2017).
Ross, J. S. et al. Immunotherapy predictive biomarkers in metastatic breast cancer (MBC). J. Clin. Oncol. 37, 1023 (2019).
Mateo, J. et al. A framework to rank genomic alterations as targets for cancer precision medicine: The ESMO Scale for Clinical Actionability of molecular Targets (ESCAT). Ann. Oncol. 29, 1895–1902 (2018).
Lemery, S., Keegan, P. & Pazdur, R. First FDA approval agnostic of cancer site: When a biomarker defines the indication. N. Engl. J. Med. 377, 1409–1412 (2017).
Deng, L. et al. Prevalence and prognostic role of PIK3CA/AKT1 mutations in Chinese breast cancer patients. Cancer Res. Treat. 51, 128–140 (2019).
Juric, D. et al. Alpelisib plus fulvestrant in PIK3CA-altered and PIK3CA-wild-type estrogen receptor-positive advanced breast cancer: a phase 1b clinical trial. JAMA Oncol. 5, e184475 (2019).
Jones, R. H. et al. Fulvestrant plus capivasertib versus placebo after relapse or progression on an aromatase inhibitor in metastatic, oestrogen receptor-positive breast cancer (FAKTION): A multicentre, randomised, controlled, phase 2 trial. Lancet Oncol. 21, 345–357 (2020).
Schmid, P. et al. Capivasertib plus paclitaxel versus placebo plus paclitaxel as first-line therapy for metastatic triple-negative breast cancer: The PAKT trial. J. Clin. Oncol. 38, 423–433 (2020).
Nagano, M. et al. High-throughput functional evaluation of variants of unknown significance in ERBB2. Clin. Cancer Res. 15, 5112–5122 (2018).
Gaillard, S. L. et al. Constitutively active ESR1 mutations in gynecologic malignancies and clinical response to estrogen-receptor directed therapies. Gynecol. Oncol. 154, 199–206 (2019).
Turner, N. et al. FGFR1 amplification drives endocrine therapy resistance and is a therapeutic target in breast cancer. Cancer Res. 70, 2085–2094 (2010).
Bernhardt, S. M. et al. Hormonal modulation of breast cancer gene expression: Implications for intrinsic subtyping in premenopausal women. Front. Oncol. 6, 241 (2016).
Woeckel, A. et al. Interdisciplinary screening, diagnosis, therapy and follow-up of breast cancer. Guideline of the DGGG and the DKG. Geburtshilfe Frauenheilkd. 78, 1056–1088 (2018).
Suresh, P. K. Breast cancer heterogeneity: A focus on epigenetics and in vitro 3D model systems. Cell J. 20, 302–311 (2018).
Acknowledgements
This study received no funding.
Author information
Authors and Affiliations
Contributions
D.H., F.E., V.M. and Z.T. wrote the main manuscript text and A.G. (both), A.B., W.S., L.G. prepared figures. W.J., A.D.G. and L.H. initiated the study and provided proof reading at all stages. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hempel, D., Ebner, F., Garg, A. et al. Real world data analysis of next generation sequencing and protein expression in metastatic breast cancer patients. Sci Rep 10, 10459 (2020). https://doi.org/10.1038/s41598-020-67393-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-67393-9
This article is cited by
-
The Association of PTEN Gene Mutations with the Breast Cancer Risk: A Systematic Review and Meta-analysis
Biochemical Genetics (2024)
-
Coexistent ARID1A-PIK3CA mutations are associated with immune-related pathways in luminal breast cancer
Scientific Reports (2023)
-
Implications for surveillance for breast cancer patients based on the internally and externally validated BRENDA-metastatic recurrence score
Breast Cancer Research and Treatment (2023)
-
Applicability of ESMO-MCBS and ESCAT for molecular tumor boards
memo - Magazine of European Medical Oncology (2022)
-
NGS-guided precision oncology in metastatic breast and gynecological cancer: first experiences at the CCC Munich LMU
Archives of Gynecology and Obstetrics (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.