Abstract
Hip fracture (HF) remains a main issue in the elderly patient. About 1.6 million patients a year worldwide are victims of a HF. Their incidence is expected to rise with the aging of the world’s population. Identifying risk factors is mandatory in order to reduce mortality and morbidity. The aim of the study was to identify risk factors of 1-year mortality after HF surgery. We performed an observational, prospective, single-center study at Amiens University Hospital (Amiens, France). After ethical approval, we consecutively included all patients with a HF who underwent surgery between June 2016 and June 2017. Perioperative data were collected from medical charts and by interviews. Mortality rate at 12 months was recorded. Univariate analysis was performed and mortality risk factors were investigated using a Cox model. 309 patients were analyzed during this follow-up. Mortality at 1 year was 23.9%. Time to surgery over 48 hours involved 181 patients (58.6%) while 128 patients (41.4%) had surgery within the 48 hours following the hospital admission. Independent factors associated with 1-year mortality were: age (HR at 1.059 (95%CI [1.005–1.116], p = 0,032), Lee score ≥ 3 (HR at 1,52 (95% CI [1,052–2,198], p = 0.026) and time to surgery over 48 hours (HR of 1.057 (95% CI [1.007–1.108], p = 0.024). Age, delayed surgical (over 48 hours) management and medical history are important risk factors of 1-year mortality in this French cohort
Similar content being viewed by others
Introduction
Hip fracture (HF) remains a main issue in the elderly patient. As bone loss tends to decreases in association with osteoporosis and osteopenia, the risk of hip fracture increases1. HF represents a health care concern as the incidence and the mortality rate remains high2,3. The world estimation of patients with HF is around 1.6 million a year4. In France, 150 000 patients each year suffer HF. The mortality rate varies from 8 to 36% depending on the country5,6,7. Only 50% patients will have independent living preservation following HF management8. Recognized risk factors for HF are old age, reduced activity, female gender and osteoporosis. Though, in every day anesthesia practice, HF represents a surgery all practitioners have to deal with. However, data on perioperative management are lacking or rely on small sample size. Evidence is of low quality or even non-existent.
Besides HF management mainly depends on each country healthcare system. Literature is abundant on national observational cohort9,10. However, data are rarely comparable from one country to another depending on its healthcare system. Moreover, the management requires a multidisciplinary approach including geriatrician, surgeon and anesthetist. It seems that a care organization within a dedicated orthogeriatric ward can reduce long-term mortality11,12,13.
A recent meta-analysis revealed residential status, pulmonary disease, cardiovascular disease, diabetes, and time to surgery increased the risk of mortality after HF surgery14.
It also seems that surgery delay counts for the poor prognosis as reported in another meta-analysis of 190000 patients15. That finding is controversial as reported as non-significant in others studies16.
To date, there is no study in France that evaluated mortality and risk factors after HF during the perioperative time. The aim of the study was to determine the mortality rate at 1-year in a French cohort and to identify mortality risk factors, especially preventable risk factors.
Methods
Ethics
We performed an observational, prospective, single-center study at Amiens University Hospital (Amiens, France). Ethical approval for this study (Ethical Committee N° RNI2016–04 the 26th of may 2016) was provided by the “Comité de Protection des Personnes Nord-Ouest II” of Amiens University Hospital, Amiens, France. The trial was registered on ClinicalTrials.gov (identifier: NCT03117868). The study complied with the Declaration of Helsinki on ethical principles for medical research involving human subjects. Written informed consent was given by all participating patients or their legal representatives and written informed consent was obtained from the next of kin in case of data used from dead patients. The present report was drafted in line with the STROBE statement for observational studies in epidemiology17.
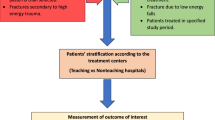
Study population
Patients with HF admitted to the traumatology department between June 2016 and June 2017 were prospectively enrolled in the study. The inclusion criteria were age over 65 years, surgical managing of traumatic HF, and agreement to participate to the study. For patients with cognitive impairment, the closest relative or caregiver was informed. The non-inclusion criteria were non-traumatic HF (pathological fracture), open fracture, traffic accident and periprosthetic fracture.
Measures and follow-up
Patient data were prospectively collected over a 1-year period. The following data were collected from medical records or interviews: age, gender, weight, body mass index (BMI), medical history (dyslipidemia, hypertension, diabetes, active smoking) and drug at baseline, ASA status as defined by the American Society of Anesthesiologists anesthesia and the LEE score18, pre-fracture functional level was assessed with the ADL (activity of daily living) score graded from 1 to 6 (full independence: the ability to do all 6 ADL without assistance; partial dependence as the ability to do 4 or 5 ADL without assistance; and total dependence as the ability to do 3 ADL or fewer without assistance), residential status (1:own home; 2: nursing home). The following biologic test results were collected: preoperative albumin, hemoglobin level at hospital admission, hemoglobin level the day before surgery and hemoglobin level on 1st and 3th postoperative days.
The following surgical data were collected: hip fracture type (total hip arthroplasty, hemiarthroplasty, dynamic hip screw with plate or intra medullar hip screw), time to surgery (≤ 48 h or >48 h, dating from the hospital admission to the beginning of surgery), anesthesia type (general or regional anesthesia (neuraxial technique, peripheral nerve block)) and the hospital length of stay (days). The time to surgery was defined by the delay between hospital admission and start of the surgery. Medical or surgical perioperative complications were recorded. Acute kidney injury (AKI) was defined as serum creatinine >1.5 baseline or increase >26.5 mmol/l.
Mortality data collection
Each patient was followed up with an orthopaedic surgery consultation organised at 1 month, 3 months, 6 months and 1 year from the fracture. When patient did not come for consultation, the status dead or alive at each time (1,3,6 and 12 months) was followed up by calling the attending physician, the patient, the trustworthy person or the city hall to request the death registry.
Statistical analysis
Data were expressed as mean ± standard deviation (SD) if data were normally distributed or as median [interquartile range (IQR)] if not. Categorial data were expressed in numbers (percentage). Normal distribution was verified using Shapiro-Wilk test. Variables were compared in a Student’s t test, a Wilcoxon-Mann-Whitney test, a chi-squared test or a Fischer exact test, as appropriate. Univariate analysis was used to identify risk factors of death at 12 months. Cox proportional hazards were used to display the adjusted cumulative hazard of the mortality at 12 months when p < 0.05 in univariate analysis. Time-to-event analyses were performed with the use of Kaplan-Meier estimates. Statistical analyses were performed with SPSS software for Mac (version 21, IBM, SPSS). The threshold for statistical significance was set to p < 0.05.
Results
Demographic data (Table 1)
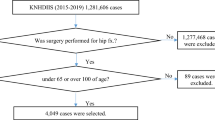
A full description of the study cohort is provided in Table 1. We enrolled patients from June 2016 to June 2017 (Fig. 1). A total of 309 patients were included during the 1-year study period. No patient was excluded. No patient was lost to follow-up.
Overall mortality rate
The mortality rate was 23.9% at one year following HF surgery. The mortality rate was respectively 6.1, 14.2 and 18.8% at respectively 1, 3, 6 months (p < 0.0001).
Univariate analysis between survivor and dead patients (Table 2)
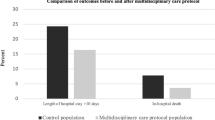
At 1-year follow-up, mortality was significantly higher in patients living in nursing home (46% versus 25% in survivors, p < 0.01), in those with a ASA score at 3 (76% versus 58% in survivors, p < 0.01) and with a Lee score ≥ 3 (13% versus 2% in survivors, p < 0.01). The hemiarthroplasty is associated with higher mortality (49% versus 34% in survivors, p = 0.003). Time to surgery> 48 hours involved 181 patients (58,6%) while 128 patients (41,4%) had surgery within 48 hours of admission. There is a significant association between 1-year mortality and time to surgery, 55 patients (71%) died when surgery occurred after 48 hours whereas 23 (29%) died when operated within 48 hours (p = 0.009). Albumin preoperative level was not associated with 12-month mortality but the risk of mortality was higher in patients having a lower BMI (22.5 [21.1–27.0] versus 23.9 [21.1–27.0] in survivors, p = 0.033]. Furthermore, age was associated with 12-month mortality. We found no association between mortality at 1 year and length of stay, blood cell transfusion or the occurrence of perioperative medical or surgical complication. No association between post-operative AKI and mortality was found. In addition, there was no association between 1-year mortality and type of anesthesia.
Delaying surgery over 48 hours had several causes: 21% for antithrombotic drug management, 38% in high risk patients for additional test (echocardiography for example) and 41% for operating ranges issues. Clinical characteristics according to time of surgery and divided in subgroups according to the cause of delay are presented in the supplementary file. One-year mortality hazard ratio for Lee Score Criteria following surgical hip fracture management are presented in the supplementary file.
Cox model for prediction of one-year mortality and survival analysis by time to surgery and Lee score (Table 3)
Using a Cox model, 1-year mortality rate was increased when Lee score is ≥ 3 (HR at 1,52 (95% CI [1,052–2,198], p = 0.026), time to surgery> to 48 hours from hospital admission (HR of 1.057 (95% CI [1.007–1.108], p = 0.024), age was predictive (HR at 1.059 (95%CI [1.005–1.116]; p = 0,032). The Kaplan-Meier survival chart for time to surgery and Lee score is shown in Fig. 2.
Discussion
In this study performed in a tertiary French hospital, the 1-year mortality rate for patient over 65 admitted for hip fracture is 23.9%. Age, time to surgery >48 h and Lee Score ≥3 were independent 1-year mortality risk factors.
Populations characteristics are similar to prior studies. The average age of patients following HF is 83.2 years, with a majority of ASA 2 or 3 status patients and a large proportion of women4,19. The mortality rate of 29% is 1-year mortality rate found in other studies20.
In our study we found an association between ASA score and Lee Score with mortality after HF surgery. The association between cardiovascular disease and mortality after HF surgery was highlighted by other studies21,22,23. In the literature, as in our study, the ASA score is associated with excess mortality in HF patients24,25. The ASA classification is an extremely common standard measure that identifies high-risks patients before surgery. This score enables a standardized risk assessment score for intra operative and post-operative risk26,27. A meta-analysis of Chang et al. conducted in 2018, including 25,349 patients from16 studies (13 prospective and 3 retrospective), found a significant association between mortality after HF and several risk factors including cardiac disease, diabetes and cancer14. Charleston Comorbidity Index (CCI) was described as able to predict postoperative complications after HF surgery however the odds ratios were not very large28. We did not assessed the CCI in the present study.
In accordance with previous studies, a time to surgery < 48 hours significantly increased the risk of death after HF surgery29,30. In our study, a time to surgery >48 h involved 181 patients (58.6%) while 128 patients (41.4%) had surgery within 48 hours of admission. Several hypotheses have been put forward to explain the existence of physiopathological processes specific to the HF. Among these, inflammation, hypercoagulability state, hypercatabolic state and stress31,32, are able to decompensate some comorbidities. Based on retrospective studies and European studies15 (no one was conducted in France), recent French guidelines (SFAR) recommended that hip surgery should be performed within 48 h after HF in order to increase survival rate33. French guidelines also supports orthogeriatric collaboration to improve mortality after hip repair. In March 2018, Chang et al. described a statistically significant association between increased “time-to-surgery” (>2 days vs <2 days; OR 1.91, 95% CI 1.14–3.18, p = 0.013) and mortality. Although it is clear that at this moment in time, the evidence remains conflicting. Our work is, to our knowledge, the first French prospective study on the field and emphasize the need to decrease the delay between HF and surgery. In our study, delaying surgery over 48 hours had several causes. 21% for antithrombotic drug management, 38% in high risk patients for additional test (echocardiography for example) but also operating range issues (41%). Even if further assessment for high risk patients seems reasonable, the benefit of early surgery for these patients should not be forgotten. Concerning antithrombotic drugs management, a retrospective work by Purushothaman et al. concluded that there is no increased risk of bleeding with clopidogrel for HF surgery34. Moreover, Mas-Atance J et al. have shown in a prospective study, that early surgery for patients receiving antiplatelet therapy reduced hospital length of stay without worsening clinical outcome.35.
In univariate, we identified nursing home residence as a risk factor for mortality following HF surgery. This result is in accordance with previous studies. Harris and al. so found that nursing home residence increased the risk of death after HF surgery in Australia36. In their meta-analysis, Chang and al. reported that patients living in a nursing home have a higher mortality than those at home14.
Using regional or general anesthesia has no influence on 1-year mortality in our follow-up study. Several studies compared the effects of regional anesthesia vs general anesthesia and found no difference on morbidity, mortality and hospitalization costs13,37. Our results are consistent with these recent data.
A recent study found that transfusion is associated with mortality for HF patients25. In our study, 27,8% of the patients were transfused, but we didn’t find any association between transfusion and 1-year mortality. The perioperative transfusion strategy has been the subject of numerous studies and some authors have investigated different strategies to reduce blood loss in order to avoid transfusion without increasing the risk of death38,39.
Giusti et al. showed that a multidisciplinary care model is superior to standard care40. Prestmo and et al.41 conducted a single-center, randomized trial and concluded that treatment of older patients with HF should be organized as orthogeriatric care. The absence of a dedicated orthogeriatric ward could explain the surgical delay in our medical center.
Our study presents some limits. First, as it is a single-center, observational study, some unknown confounding factors may exist. Secondly, we did not report data on anesthesia management. It is well known that ventilation, anesthesia depth and hemodynamic management may have a significant impact on postoperative outcomes and mortality rate.
The methodological strengths of our study include its prospective design and the long-term (1year) follow- up period. To our knowledge, no previous study evaluated risk factors of long term mortality in France. Moreover, as we had a very low rate of missing data, our sample can be considered as representative of the population of the region.
Conclusion
In this first prospective study on long-term mortality in France, we found a 1-year mortality rate of 23.9%. Age, time to surgery >48 h and Lee score ≥3 are independent factor of 1-year mortality following HF surgery. Early surgical management of patients suffering from HF remains an important mean to reduce mortality.
References
Tarazona-Santabalbina, F. J. et al. Early interdisciplinary hospital intervention for elderly patients with hip fractures: functional outcome and mortality. Clinics (Sao Paulo) 67, 547–56 (2012).
Johnell, O. & Kanis, J. A. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17, 1726–33 (2006).
Cram, P. et al. Clinical characteristics and outcomes of Medicare patients undergoing total hip arthroplasty, 1991-2008. JAMA 305, 1560–7 (2011).
Aubrun, F. [Hip fracture surgery in the elderly patient: epidemiological data and risk factors]. Ann Fr Anesth Reanim 30, e37–39 (2011).
Abrahamsen, B., van Staa, T., Ariely, R., Olson, M. & Cooper, C. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int 20, 1633–50 (2009).
Vestergaard, P., Rejnmark, L. & Mosekilde, L. Loss of life years after a hip fracture. Acta Orthop 80, 525–30 (2009).
Haentjens, P. et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152, 380–90 (2010).
Boddaert, J., Raux, M., Khiami, F. & Riou, B. Perioperative management of elderly patients with hip fracture. Anesthesiology 121, 1336–41 (2014).
Henderson, C. Y. & Ryan, J. P. Predicting mortality following hip fracture: an analysis of comorbidities and complications. Ir J Med Sci 184, 667–71 (2015).
Härstedt, M., Rogmark, C., Sutton, R., Melander, O. & Fedorowski, A. Impact of comorbidity on 6-month hospital readmission and mortality after hip fracture surgery. Injury 46, 713–8 (2015).
Moyet J, Deschasse G, Marquant B, Mertl P, Bloch F. Which is the optimal orthogeriatric care model to prevent mortality of elderly subjects post hip fractures? A systematic review and meta-analysis based on current clinical practice. Int Orthop 2018;
Boddaert, J. et al. Postoperative admission to a dedicated geriatric unit decreases mortality in elderly patients with hip fracture. PLoS ONE 9, e83795 (2014).
Neuman, M. D., Rosenbaum, P. R., Ludwig, J. M., Zubizarreta, J. R. & Silber, J. H. Anesthesia technique, mortality, and length of stay after hip fracture surgery. JAMA 311, 2508–17 (2014).
Chang, W. et al. Preventable risk factors of mortality after hip fracture surgery: Systematic review and meta-analysis. Int J Surg 52, 320–8 (2018).
Moja, L. et al. Timing matters in hip fracture surgery: patients operated within 48 hours have better outcomes. A meta-analysis and meta-regression of over 190,000 patients. PLoS ONE 7, e46175 (2012).
Majumdar, S. R. et al. Lack of association between mortality and timing of surgical fixation in elderly patients with hip fracture: results of a retrospective population-based cohort study. Med Care 44, 552–9 (2006).
von Elm, E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 12, 1495–9 (2014).
Lee, T. H. et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 100, 1043–9 (1999).
Grigoryan, K. V., Javedan, H. & Rudolph, J. L. Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis. J Orthop Trauma 28, e49–55 (2014).
Bentler, S. E. et al. The aftermath of hip fracture: discharge placement, functional status change, and mortality. Am J Epidemiol 170, 1290–9 (2009).
Johansen, A., Tsang, C., Boulton, C., Wakeman, R. & Moppett, I. Understanding mortality rates after hip fracture repair using ASA physical status in the National Hip Fracture Database. Anaesthesia 72, 961–6 (2017).
Gerber, Y. et al. Cardiovascular and noncardiovascular disease associations with hip fractures. Am J Med 126(169), e19–26 (2013).
Ribeiro, T. A. et al. Predictors of hip fracture mortality at a general hospital in South Brazil: an unacceptable surgical delay. Clinics (Sao Paulo) 69, 253–8 (2014).
Lin, J. C.-F. et al. Mortality and complications of hip fracture in young adults: a nationwide population-based cohort study. BMC Musculoskelet Disord 15, 362 (2014).
Ercin, E. et al. Risk factors for mortality in geriatric hip fractures: a compressional study of different surgical procedures in 785 consecutive patients. Eur J Orthop Surg Traumatol 27, 101–6 (2017).
Owens, W. D., Felts, J. A. & Spitznagel, E. L. ASA physical status classifications: a study of consistency of ratings. Anesthesiology 49, 239–43 (1978).
Donegan, D. J. et al. Use of medical comorbidities to predict complications after hip fracture surgery in the elderly. J Bone Joint Surg Am 92, 807–13 (2010).
Menzies, I. B., Mendelson, D. A., Kates, S. L. & Friedman, S. M. The impact of comorbidity on perioperative outcomes of hip fractures in a geriatric fracture model. Geriatr Orthop Surg Rehabil 3, 129–34 (2012).
Siegmeth, A. W., Gurusamy, K. & Parker, M. J. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br 87, 1123–6 (2005).
Bottle, A. & Aylin, P. Mortality associated with delay in operation after hip fracture: observational study. BMJ 332, 947–51 (2006).
Beloosesky, Y. et al. Cytokines and C-reactive protein production in hip-fracture-operated elderly patients. J Gerontol A Biol Sci Med Sci 62, 420–6 (2007).
Desborough, J. P. The stress response to trauma and surgery. Br J Anaesth 85, 109–17 (2000).
Colais, P., Di Martino, M., Fusco, D., Perucci, C. A. & Davoli, M. The effect of early surgery after hip fracture on 1-year mortality. BMC Geriatr 15, 141 (2015).
Purushothaman, B. et al. Decision making on timing of surgery for hip fracture patients on clopidogrel. Ann R Coll Surg Engl 98, 91–5 (2016).
Mas-Atance, J. et al. [Randomised comparative study of early versus delayed surgery in hip-fracture patients on concomitant treatment with antiplatelet drugs. Determination of platelet aggregation, perioperative bleeding and a review of annual mortality]. Rev Esp Cir Ortop Traumatol 57, 240–53 (2013).
Harris, I. A., Yong, S., McEvoy, L. & Thorn, L. A prospective study of the effect of nursing home residency on mortality following hip fracture. ANZ J Surg 80, 447–50 (2010).
Le-Wendling, L. et al. Regional anesthesia as compared with general anesthesia for surgery in geriatric patients with hip fracture: does it decrease morbidity, mortality, and health care costs? Results of a single-centered study. Pain Med 13, 948–56 (2012).
Watts, C. D., Houdek, M. T., Sems, S. A., Cross, W. W. & Pagnano, M. W. Tranexamic Acid Safely Reduced Blood Loss in Hemi- and Total Hip Arthroplasty for Acute Femoral Neck Fracture: A Randomized Clinical Trial. J Orthop Trauma 31, 345–51 (2017).
Yoon, B.-H., Ko, Y. S., Jang, S.-H. & Ha, J. K. Feasibility of Hip Fracture Surgery Using a No Transfusion Protocol in Elderly Patients: A Propensity Score-Matched Cohort Study. J Orthop Trauma 31, 414–9 (2017).
Giusti, A., Barone, A., Razzano, M., Pizzonia, M. & Pioli, G. Optimal setting and care organization in the management of older adults with hip fracture. Eur J Phys Rehabil Med 47, 281–96 (2011).
Prestmo, A. et al. Comprehensive geriatric care for patients with hip fractures: a prospective, randomised, controlled trial. Lancet 385, 1623–33 (2015).
Acknowledgements
This study received no financial support. The study was performed at Amiens University Hospital and was approved by the institutional review board of Amiens University Hospital.
Author information
Authors and Affiliations
Contributions
P.H., A.N. and A.D. conceived the study, participated in its design and coordination and final approval. P.H. drafted the manuscript. OAA participated in data analysis and manuscript revision. B.T., C.B., P.-G. G., E.H., H.D., E.L. and Y.M. participated in the coordination of the study, data acquisition and helped to draft the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huette, P., Abou-Arab, O., Djebara, AE. et al. Risk factors and mortality of patients undergoing hip fracture surgery: a one-year follow-up study. Sci Rep 10, 9607 (2020). https://doi.org/10.1038/s41598-020-66614-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-66614-5
This article is cited by
-
Validation of the Charlson Comorbidity Index for the prediction of 30-day and 1-year mortality among patients who underwent hip fracture surgery
Perioperative Medicine (2024)
-
The use of minimum common data set in the development of the Greek Fragility Hip Fracture Registry in the Greek health care setting: the first year of its pilot implementation
Archives of Osteoporosis (2024)
-
Systematic review and meta-analysis of preoperative predictors for early mortality following hip fracture surgery
Osteoporosis International (2024)
-
Comparison of mortality rate and septic and aseptic revisions in total hip arthroplasties for osteoarthritis and femoral neck fracture: an analysis of the German Arthroplasty Registry
Journal of Orthopaedics and Traumatology (2023)
-
Perioperative peri-implant fracture after osteosynthesis for geriatric femoral pertrochanteric fracture with the linear compression integrated screw intramedullary nail system (INTERTAN™): a retrospective study
Journal of Orthopaedic Surgery and Research (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.