Abstract
HA (Hyaluronic acid) filler, the most commonly used dermal filler, causes several side effects. HA-PN (Hyaluronic acid-Polynucleotide), a new composite filler, has excellent biocompatibility and induces tissue regeneration. In this study, we compare the efficacies and safety profiles of these fillers. The characteristics of HA and HA–PN fillers were compared using scanning electron microscopy and rheometry. No morphological difference was noted between the fillers. However, the latter had higher viscosity and elasticity values. The HA-PN filler induced higher cell migration than the HA filler in a wound healing assay. It was also found to stimulate better collagen synthesis in human and mouse fibroblasts. The HA and HA–PN fillers were injected into SKH1 hairless mice to determine changes in their volume for up to 24 weeks. Increased cell migration and collagen synthesis were observed in mice injected with the HA–PN complex filler. Although the safety and durability of the HA and HA–PN fillers were similar, the latter induced a lower transient receptor potential vanilloid 4 expression and caused less stimulation upon injection. In conclusion, HA–PN complex fillers can stimulate fibroblast growth and facilitate volume growth and skin regeneration.
Similar content being viewed by others
Introduction
Dermal fillers can be used in simple and short procedures in surgery and rapid facial rejuvenation. There is growing interest in the use of fillers for tissue enlargement and improvement of skin aesthetic beauty1,2,3.
Synthetic facial fillers are composed of a biosynthetic polymer in combination with different injectable carriers, including hydrogels, beads, and liquids4. The most popular type of filler contains hyaluronic acid (HA). However, the use of HA fillers carries an inherent risk of hypersensitivity reactions because these fillers contain hyaluronan-related proteins and 1,4-butanediol diglycidyl ether (BDDE)5,6. In addition, small fragments of HA can cause inflammation and elicit adverse effects that include erythema, slight oedema, hematoma, itching, and pain7,8,9. A recent study showed that the biocompatibility of HA-based materials decreases with an increase in the number of modifications to this polysaccharide5,6,10.
Various dermal fillers have been developed to overcome the adverse effects accompanying the use of HA fillers6,11,12,13,14. Recently, a new filler product was synthesised using a purified polynucleotide (PN) extracted from salmon and other fish germ cells. This product is currently in use in Europe15. While existing filler products work by simply filling spaces in the skin16, PN-containing products also induce the regeneration of damaged tissues to result in a more natural tissue regeneration15. In addition, it has been reported that nucleotides promote the growth of human corneal fibroblasts and increase their remnants in ultraviolet B-damaged skin fibroblasts17. In vitro studies have demonstrated the therapeutic efficacy of polynucleotides in patients who received treatment for skin ectopia and have shown that polynucleotides promote rapid corneal epithelialisation after photorefractive keratectomy18,19.
The use of a PN filler offers the advantages of skin elasticity, collagen synthesis, and regeneration by stimulation of fibre elasticity. However, the volumising effect and durability of PN dermal fillers are not as good as those of existing dermal fillers15,20,21. In this study, we used an HA–PN (Hyaluronic acid-Polynucleotide) complex filler, which has the advantages of both tissue regeneration and durability. This filler overcomes the disadvantages of its individual components. This study also aimed to demonstrate the commercial feasibility of the HA–PN complex filler by comparing the efficacies and safety profiles of HA and HA–PN complex fillers in vitro and in vivo.
Results
Scanning electron microscopy (SEM) analysis of HA and HA–PN complex fillers
The morphologies of HA and HA-PN complex fillers were compared using SEM. Based on the SEM images, both fillers are made up of irregular and small polygonal particles (Fig. 1).
Comparison of rheological properties of HA and HA–PN fillers
The G′ mean values of elasticity, G″ mean values of viscosity, G* mean values of viscoelasticity, and the mean values of tan δ, indicating the ratio of viscosity to elasticity, were measured (Supplementary Fig. 1, Table 1). All values were higher for the HA–PN complex fillers than for the HA fillers. These results confirmed that the addition of PN to HA increases the filler’s elasticity, viscosity, viscoelasticity, and modulus of elasticity.
Comparison of cell cytotoxicity and proliferation induced by HA, PN, and HA–PN treatments
To assess the cytotoxic effects of HA, PN, and HA–PN treatments on human dermal fibroblast (HDF) and mouse fibroblast (L929) cells, comparative cytotoxicity tests using the MTT (3-(4, 5-dimethylathiazolyl-2)-2, 5-diphenyltetrazolium bromide) assay were performed. The cells were incubated with the fillers for 24 and 72 h before cytotoxicity was assessed (Fig. 2). HA, PN, and HA–PN did not display dose- or time-dependent cytotoxic effects. On the contrary, the proliferation of HDF cells was evident following treatment with only 1% PN, a combination of 0.1% HA and 0.5% PN, and a combination of 0.1% HA and 1% PN. Additionally, the proliferation of L929 cells increased significantly after treatment with a combination of 0.1% HA and 0.5% PN and a combination of 0.1% HA and 1% PN. In particular, co-treatment with 0.1% HA and 1% PN increased the proliferation of HDF and L929 cells by approximately 20%.
Comparison of cell migration following HA, PN, and HA–PN treatment
To further investigate the effects of HA, PN, and HA–PN on the proliferation of HDFs, a wound healing assay was performed after HA, PN, and HA–PN treatments. After incubation for 48 h, cell migration was confirmed (Fig. 3A). In particular, co-treatment with 0.1% HA and 0.5% PN showed the highest cell growth potential (Fig. 3B). These results suggest that PN is effective for cell proliferation.
Effect of PN on the migration of human fibroblast cells. Wound Healing Analysis Images (Zoomth increasing concentrations of Ibidi chambers and cultured to near confluence. A free ‘scratch’ or wound was created on the bound monolayer of cultured cells. The cells were incubated in medium containing 0.1% HA, 0.5% PN, or 1% PN for 0, 24 and 72 h at 37 °C in a humidified incubator with a 5% CO2 atmosphere. Medium Supplemented with 10% FBS was used in the complete medium group. The wound areas were quantified and expressed as a percentage of the initial wound area.
Comparison of collagen synthesis by HA, PN, and HA–PN treatments
To determine the correlation between proliferative capacity and collagen expression, the expression of type I collagen at the protein level was analysed by western blotting using HDF cells treated with HA, PN, or HA–PN. Collagen expression was higher in the 0.5% PN group and the 0.1% HA and 0.5% or 1% PN co-treatment groups when compared to that in untreated HDF cells (Fig. 4A,B). Soluble collagen in cell culture supernatants was quantified using the Sircol collagen assay. A dose-dependent increase in collagen synthesis was observed in the PN group and the HA-PN co-treatment group, but not in the HA group (Fig. 4C). Therefore, PN treatment induced an increase in collagen synthesis in the cells.
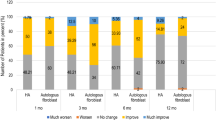
Comparison of durability between HA and HA–PN complex fillers in vivo
To confirm the durabilities of the HA and HA–PN fillers, 100 μL of each filler was injected into the dorsal region of mice, and changes in the volumes of the fillers were observed. Both HA and HA–PN fillers displayed an increase in volume for up to 4 weeks. The largest volume was observed for Juvéderm VOLUMA (250 mm3), followed by those for Juvéderm VOLBELLA (158 mm3), HA–PN 0.1%, 0.5% (134 mm3), and HA–PN 1% (127 mm3). These results suggested that the higher the concentration of HA, the larger is the volume growth rate. In addition, although the HA concentrations (1.5%) for Juvéderm VOLBELLA and the HA–PN complex filler were the same, the volume growth rate decreased in a dose-dependent manner for PN. Both injection fillers decreased in volume over time from 4 weeks after filler injection to 24 weeks of evaluation. The volume changes were as follows: Juvéderm VOLUMA, 120 mm3; Juvéderm VOLBELLA and HA–PN 0.5%, 98 mm3; HA–PN 0.1%, 92 mm3; HA–PN 1%, 97 mm3 (Fig. 5).
Evaluation of durability of HA and HA–PN complex fillers in vivo. (A) Study design scheme(Created with BioRender). (B) Image depicting volume change after the filler injection was taken using PRIMOS. (C) Graph showing volume change after filler injection. (D) A folliscope image depicting volume change after filler injection.
Comparison of histological analysis results between HA and HA–PN complex fillers
To confirm the degree of inflammation and reaction with foreign bodies in vivo, skin tissue at the filler injection site was biopsied at 0 h, 12 weeks, and 24 weeks. Haematoxylin and eosin-stained tissue slides were observed at 100× magnification using an optical microscope, and the main histological features of each slide were determined. Histopathological evaluation showed that there was no reaction to foreign bodies upon the injection of both fillers (Fig. 6). However, with the 1% HA–PN complex filler, the presence of inflammatory cells was detected immediately following filler injection. No inflammatory cells were observed at week 12. Collagen synthesis was confirmed after staining with Masson’s trichrome. Thus, compared to the HA filler, the complex filler containing PN was associated with greater collagen synthesis.
Comparison of transient receptor potential vanilloid 4 (TRPV4) expression between HA and HA–PN complex fillers by immunofluorescence analysis
TRPV4 tissue staining was performed to determine the degree of stimulation in the tissue owing to filler injection. TRPV4 mediates pain-related behaviour caused by mild hyperactivity in the presence of inflammatory mediators. Immunofluorescence staining was confirmed at 4 weeks, and the maximum volume was measured after each filler injection. TRPV4 expression increased in the muscle layer after treatment with the HA fillers Juvéderm VOLUMA (2.0%) and Juvéderm VOLBELLA (1.5%). On the contrary, the TRPV4 expression level after HA–PN 1% complex filler treatment was equivalent to that for treatment with the negative control, PBS (Fig. 7).
Comparison of TRPV4 expression after treatment with HA and HA–PN fillers using immunofluorescence staining of mouse tissue. The extent of stimulation in tissues by TRPV4 at Week 4 was determined using immunofluorescence staining. The increases in volume as a result of filler treatments were also compared.
Discussion
The terms “biological stimulation” and “biological regeneration” have been used to describe the functions of many aesthetic medical devices22. Regeneration is the process of restoration and growth that makes the genome, cell, organism, and ecosystem resilient to events that cause natural fluctuations, disturbances, or damages23,24. Several clinical studies have described the therapeutic use of polynucleotides in skin regeneration and wound healing25,26,27,28. The HA–PN complex filler, composed of HA and PN polymer, is a new formulation for skin regeneration and tissue restoration. We confirmed the improved functions of the HA–PN complex filler through comparisons with the Juvéderm VOLUMA and Juvéderm VOLBELLA high-volume HA fillers. Moreover, we further analysed and compared all these fillers in terms of their morphological and rheological properties, and their effects in cells and animal models.
Polynucleotides are widely distributed in the human body and exist physiologically in the extracellular environment29. They readily bind to water molecules and act as free radical scavengers30,31. The nutritional effects of PN have been shown in multiple in vitro studies using human fibroblasts in primary cultures. The ability of PN to stimulate the secretion of collagen proteins and other proteins in the extracellular matrix has also been demonstrated32,33,34.
The HA–PN complex filler is morphologically similar to the HA filler. However, we confirmed that its rheological properties, in terms of G *, G′, G′′, and tan δ, are different from those of the HA filler. It was confirmed that the hardness, elasticity, viscosity, and viscoelasticity of the cross-linked gel are dependent on the PN content of the HA–PN complex filler. In addition, no toxicity was associated with PN or HA-PN treatments in human and mouse fibroblast cells. Moreover, in human fibroblast cells, the content of type I collagen increased with the increasing PN concentration. However, excess PN inhibited the synthesis of type 1 collagen.
In animal studies, the HA–PN complex filler showed the greatest increase in collagen synthesis and maintained a natural volume, with no significant increases in the initial filler injection volume. In addition, previous studies have identified six TRPV proteins as receptors for stimulation of neurons35,36. Among these TRPV proteins, TRPV4 is a ubiquitously expressed plasma membrane-based calcium-permeable cation channel that is sensitised and activated by chemical and physical stimulation37,38,39,40. When skin is stimulated, the expression of matrix metalloproteinases (MMPs) and inflammatory cytokines can increase41,42. The increased levels of MMPs result in the degradation of collagen and elastic fibres in the skin and promote skin aging43,44. In this study, HA filler containing PN induced a lower expression of the TRPV4 protein, a neuronal stimulatory receptor, compared to HA filler. When PN was included, it induced a reduced stimulation and lower MMP and inflammatory cytokine expression. This finding indicated that HA fillers containing PN are more effective in inhibiting skin aging compared to HA fillers. Numerous fillers have been developed and used to achieve simple volume effects. However, HA–PN complex fillers can stimulate fibroblast growth for skin rejuvenation and have the added benefits of volume enhancement and skin regeneration. In addition, the trend is currently shifting from the provision of components (such as collagen, HA, and glycoproteins) into the skin to the stimulation of cellular components (such as fibroblasts) to enhance regeneration. To the best of our knowledge, this is the first study demonstrating the durability, efficacy, and safety of HA–PN complex fillers. We believe that our results can potentially be the next-generation paradigm in the filler market.
Methods
Materials
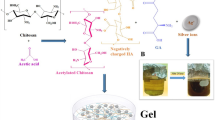
The HA-PN complex filler was supplied by NutraPharmTech (Seoul, Korea). It was prepared by mixing in the PN solution after sterilising the HA-based filler, which is generally cross-linked by BDDE. HA fillers made by Allergan were purchased from Juvéderm VOLUMA and Juvéderm VOLBELLA (Pringy, France). Type I collagen antibody (ab34710) and transient receptor potential vanilloid (TRPV4; ab39260) proteins were obtained from Abcam (Cambridge, Mass.).
Scanning electron microscopy
The morphology of each filler was evaluated using SEM. Each filler was diluted with water for injection (WFI), filtered through a 0.22 μm membrane filter mounted in a stainless-steel filter housing, and then placed in an oven until the filter contents were completely dry. Filler samples were mounted on stainless steel SEM pedestals pre-labelled with double-sided adhesive mounting disks. Samples were prepared by coating with gold-palladium powder and conventionally imaged using a LEO SUPRA 55 microscope (Carl Zeiss, Jena, Germany).
Rheological measurements
The storage modulus (G′) and viscous modulus (G″) were measured using a rheometer (Kinexus Pro, Malvern, UK). G′ characterises the stiffness of the gel – a stiff material has a higher G′ than a soft material. All measurements were carried out using a 20-mm steel plate oscillating at a frequency between 0.1 and 10 Hz. The values presented were compared to the average of the values obtained at frequencies of 1 to 10 Hz. Measurement conditions were as follows: oscillation mode; a shear strain of 1.5%; a frequency of 0.05 to 25 Hz; an interval of 0.5 mm; and a temperature of 25 °C.
Cell maintenance
HDF cells (CCD-25SK; American Type Culture Collection, Manassas, VA, USA) were grown in Dulbecco’s modified Eagle’s medium (DMEM) Supplemented with 10% foetal bovine serum (FBS), 2 mM l-glutamine, 100 U/mL penicillin, and 100 mg/mL streptomycin, at 37 °C in a humidified incubator with a 5% CO2 atmosphere45. In addition, an established mouse fibroblast cell line (L929, catalogue code CCL-1; American Type Culture Collection) was cultured in minimal essential medium Supplemented with 5% foetal calf serum, 100 U/mL penicillin, 100 μL/mL streptomycin, and 2 mmol/L l-glutamine at 37 °C in a humidified incubator with a 5% CO2 atmosphere46.
Cell viability
The MTT assay was performed to measure the cell viability of the HDFs and L929 mouse fibroblasts. HA (0.025% to 0.1%) and PN (0.1% to 1%) were added after 5 h of cell culture. MTT solution (5 mg/mL) was added and incubated at 37 °C for 4 h. After incubation, the supernatant was removed, and the formazan formed by MTT reduction was dissolved in dimethylsulfoxide47. The absorbance of formazan was measured at 570 nm using a SoftMax Pro5 ELISA microplate reader (Molecular Devices, Sunnyvale, CA, USA).
Wound healing assay for cell mobility
The wound healing assay was performed based on previous studies by measuring cell migration. The cell migration is defined as the time taken to close an open wound after a linear ‘scratch’ or wound is created across a monolayer of cultured cells48,49.
Ibidi culture-inserts (μ-Dish 35 mm, high culture-inserts; Thistle Scientific Ltd., Glasgow, UK) were used for the assay. The sample was diluted in DMEM and was used to treat the cells, which were then cultured for 24 to 72 h. DMEM Supplemented with 10% FBS was used as a positive control. After 48 h, the movement of cells was photographed using an Eclipse TS100 inverted microscope (Nikon Instruments Inc., Tokyo, Japan). Images were normalised using the XnConvert software and wound sites were quantified using the Image J software (ImageJ; version 1.51 i; U.S. National Institutes of Health). The final wound area was quantified and expressed as a percentage of the initial wound area. This represented the degree of wound healing at that point in time.
Western blotting
HDF cells were cultured in DMEM Supplemented with FBS for 24 h. The treated cells were exposed to different concentrations of HA and PN in the absence or presence of FBS. Every hour during the culture, the treated and control cells were collected and a defined amount of total protein, as determined using the Bradford protein assay (Bio-Rad Laboratories, Hercules, CA, USA), was resolved using 10% SDS-PAGE. The resolved proteins were transferred to a polyvinylidene fluoride membrane. After the application of primary antibodies and conjugated secondary antibodies, each membrane was washed thrice for 10 min with Tris-buffered saline containing 0.1% Tween 20. The degree of protein expression was determined using ECL detection reagents (Thermo Fisher Scientific, Pierce Biotechnology, Waltham, MA, USA).
Collagen measurement
The total soluble collagen from cell culture supernatants was quantified using the Sircol collagen assay, according to the manufacturer’s instructions (Biocolor, Belfast, UK)50. The absorbance was then measured at 555 nm, as it is directly proportional to the amount of collagen present in the cell culture medium. The soluble collagen was then hydrolysed in HCl, and the hydroxyproline levels were measured by a colourimetric method using an assay kit (QuickZyme Biosciences, Burlington, NC, USA), according to the manufacturer’s instructions51,52. The total collagen content was calculated from the hydroxyproline content of collagen standards50.
Study design
All animal procedures were performed in accordance with the Guidelines for the Care and Use of Laboratory Animals of Chung-Ang University and approved by the Animal Ethics Committee of Chung-Ang University IACUC (Approval No. 201700022). Six-week-old SKH1 hairless mice were bred under temperature cycles of 24 ± 2 °C, 50 ± 10% humidity, and 12 h day/night cycles in the laboratory. The filler (100 µL) was injected into the dorsal skin of the posterior limbs of hairless female mice (n = 5 mice per group).
Volumetric analysis
The volume of filler injected into each dorsal skin was measured in the anesthetised mice. After filler injection, the increase in volume was determined using a PRIMOS device at 0, 1, 4, 8, 12, 18, and 24 weeks. The volume ratios were calculated by comparing the volume and height measurements at each time point to the measurements on Day 0. The change in volume was quantitatively determined through three-dimensional (3D) measurements of the skin region at the different time points before and after treatment and computer-assisted comparison of the measured profile53.
Histological analyses
Paraffin-embedded tissue sections were deparaffinised and stained according to previously published protocols54. Skin samples were fixed in 10% phosphate-buffered formaldehyde, embedded in paraffin, and processed for histological analysis. Sections, 5 μm in thickness, were sliced and mounted on slides. The sections were stained with haematoxylin and eosin (to confirm inflammation and foreign body reaction) and Masson’s trichrome (to confirm collagen biosynthesis), according to standard procedures.
Immunofluorescence analysis
Paraffin-embedded tissue sections were deparaffinised and stained according to previously published protocols55. Anti-Transient Receptor Potential Cation Channel Subfamily V Member 4 (TRPV4) antibody (ab39260, 1:200; Abcam) was used as the primary antibody. After treatment with a blocking buffer containing 2.5% bovine serum albumin (BSA, Sigma-Aldrich, St. Louis, MO, USA) and 2.5% horse serum, the cells were incubated at 25 °C for 4 h. The tissues were washed with phosphate-buffered saline containing 0.1% Triton X-100 (PBST). A fluorescein isothiocyanate-goat anti-rabbit secondary antibody, which exhibits green fluorescence, was added to the blocking buffer containing 2.5% BSA and left in a dark room for 2 h.
Statistical analyses
Statistical significance was computed using SPSS version 21 software (SPSS Inc., Chicago, IL, USA). One-way ANOVA and two-tailed unpaired t-tests were performed. *p ≤ 0.05, **p ≤ 0.005, ***p ≤ 0.0005.
Data availability
All data generated or analysed during this study are included in this published article and its Supplementary Information Files. Extra data are available from the corresponding author upon request.
References
Kruglikov, I. L. & Wollina, U. Soft tissue fillers as non-specific modulators of adipogenesis: change of the paradigm? Exp Dermatol 24, 912–915, https://doi.org/10.1111/exd.12852 (2015).
Wise, J. B. & Greco, T. Injectable treatments for the aging face. Facial Plast Surg 22, 140–146, https://doi.org/10.1055/s-2006-947720 (2006).
Wu, D. C. et al. Evaluation of the in vivo effects of various laser, light, or ultrasound modalities on human skin treated with a collagen and polymethylmethacrylate microsphere dermal filler product. Lasers Surg Med 48, 811–819, https://doi.org/10.1002/lsm.22580 (2016).
Wang, F. et al. In vivo stimulation of de novo collagen production caused by cross-linked hyaluronic acid dermal filler injections in photodamaged human skin. Arch Dermatol 143, 155–163, https://doi.org/10.1001/archderm.143.2.155 (2007).
Fidalgo, J. et al. Detection of a new reaction by-product in BDDE cross-linked autoclaved hyaluronic acid hydrogels by LC-MS analysis. Med Devices (Auckl) 11, 367–376, https://doi.org/10.2147/MDER.S166999 (2018).
Keizers, P. H. J. et al. A high crosslinking grade of hyaluronic acid found in a dermal filler causing adverse effects. J Pharm Biomed Anal 159, 173–178, https://doi.org/10.1016/j.jpba.2018.06.066 (2018).
Fino, P., Toscani, M., Grippaudo, F. R., Giordan, N. & Scuderi, N. Randomized Double-Blind Controlled Study on the Safety and Efficacy of a Novel Injectable Cross-linked Hyaluronic Gel for the Correction of Moderate-to-Severe Nasolabial Wrinkles. Aesthetic Plast Surg 43, 470–479, https://doi.org/10.1007/s00266-018-1284-x (2019).
Shi, X. H. et al. Complications from Nasolabial Fold Injection of Calcium Hydroxylapatite for Facial Soft-Tissue Augmentation: A Systematic Review and Meta-Analysis. Aesthet Surg J 36, 712–717, https://doi.org/10.1093/asj/sjv206 (2016).
Taylor, S. C., Burgess, C. M. & Callender, V. D. Safety of nonanimal stabilized hyaluronic acid dermal fillers in patients with skin of color: a randomized, evaluator-blinded comparative trial. Dermatol Surg 35(Suppl 2), 1653–1660, https://doi.org/10.1111/j.1524-4725.2009.01344.x (2009).
Yeom, J. et al. Effect of cross-linking reagents for hyaluronic acid hydrogel dermal fillers on tissue augmentation and regeneration. Bioconjug Chem 21, 240–247, https://doi.org/10.1021/bc9002647 (2010).
Iverson, S. M. & Patel, R. M. Dermal filler-associated malar oedema: Treatment of a persistent adverse effect. Orbit 36, 473–475, https://doi.org/10.1080/01676830.2017.1337203 (2017).
Tran, C., Carraux, P., Micheels, P., Kaya, G. & Salomon, D. In vivo bio-integration of three hyaluronic acid fillers in human skin: a histological study. Dermatology 228, 47–54, https://doi.org/10.1159/000354384 (2014).
Vidic, M. & Bartenjev, I. An adverse reaction after hyaluronic acid filler application: a case report. Acta Dermatovenerol Alp Pannonica Adriat 27, 165–167 (2018).
Wollina, U. & Goldman, A. Dermal fillers: facts and controversies. Clin Dermatol 31, 731–736, https://doi.org/10.1016/j.clindermatol.2013.05.010 (2013).
Park, K. Y., Seok, J., Rho, N. K., Kim, B. J. & Kim, M. N. Long-chain polynucleotide filler for skin rejuvenation: efficacy and complications in five patients. Dermatol Ther 29, 37–40, https://doi.org/10.1111/dth.12299 (2016).
Spano, S. J., Ghilzon, R., Lam, D. K., Goldberg, M. B. & Tenenbaum, H. C. Subperiosteal Papilla Augmentation With a Non-Animal-Derived Hyaluronic Acid Overlay Technique. Clin Adv Periodontics, https://doi.org/10.1002/cap.10075 (2019).
Muratore, O. et al. A human placental polydeoxyribonucleotide (PDRN) may promote the growth of human corneal fibroblasts and iris pigment epithelial cells in primary culture. New Microbiol 26, 13–26 (2003).
Ichikawa, M. et al. Decreased UV sensitivity, mismatch repair activity and abnormal cell cycle checkpoints in skin cancer cell lines derived from UVB-irradiated XPA-deficient mice. Mutat Res 459, 285–298 (2000).
Wu, C. L. et al. Proteomic analysis of UVB-induced protein expression- and redox-dependent changes in skin fibroblasts using lysine- and cysteine-labeling two-dimensional difference gel electrophoresis. J Proteomics 75, 1991–2014, https://doi.org/10.1016/j.jprot.2011.12.038 (2012).
Hekimi, S., Wang, Y. & Noe, A. Mitochondrial ROS and the Effectors of the Intrinsic Apoptotic Pathway in Aging Cells: The Discerning Killers! Front Genet 7, 161, https://doi.org/10.3389/fgene.2016.00161 (2016).
Pak, C. S. et al. A phase III, randomized, double-blind, matched-pairs, active-controlled clinical trial and preclinical animal study to compare the durability, efficacy and safety between polynucleotide filler and hyaluronic acid filler in the correction of crow’s feet: a new concept of regenerative filler. J Korean Med Sci 29(Suppl 3), S201–209, https://doi.org/10.3346/jkms.2014.29.S3.S201 (2014).
Avantaggiato, A. et al. Radiofrequency treatments: what can we expect? J Biol Regul Homeost Agents 30, 217–222 (2016).
Einhorn, T. A. & Lee, C. A. Bone regeneration: new findings and potential clinical applications. J Am Acad Orthop Surg 9, 157–165 (2001).
Goetsch, S. C., Hawke, T. J., Gallardo, T. D., Richardson, J. A. & Garry, D. J. Transcriptional profiling and regulation of the extracellular matrix during muscle regeneration. Physiol Genomics 14, 261–271, https://doi.org/10.1152/physiolgenomics.00056.2003 (2003).
Kim, J. K. & Chung, J. Y. Effectiveness of polydeoxyribonucleotide injection versus normal saline injection for treatment of chronic plantar fasciitis: a prospective randomised clinical trial. Int Orthop 39, 1329–1334, https://doi.org/10.1007/s00264-015-2772-0 (2015).
Lazzarotto, M., Tomasello, E. M. & Caporossi, A. Clinical evaluation of corneal epithelialization after photorefractive keratectomy in patients treated with polydeoxyribonucleotide (PDRN) eye drops: a randomized, double-blind, placebo-controlled trial. Eur J Ophthalmol 14, 284–289 (2004).
Rubegni, P., De Aloe, G., Mazzatenta, C., Cattarini, L. & Fimiani, M. Clinical evaluation of the trophic effect of polydeoxyribonucleotide (PDRN) in patients undergoing skin explants. A Pilot Study. Curr Med Res Opin 17, 128–131 (2001).
Squadrito, F. et al. Pharmacological Activity and Clinical Use of PDRN. Front Pharmacol 8, 224, https://doi.org/10.3389/fphar.2017.00224 (2017).
Quirin, E. A. et al. Development of sequence characterized amplified region (SCAR) primers for the detection of Phyto.5.2, a major QTL for resistance to Phytophthora capsici Leon. in pepper. Theor Appl Genet 110, 605–612, https://doi.org/10.1007/s00122-004-1874-7 (2005).
Misiaszek, R., Crean, C., Geacintov, N. E. & Shafirovich, V. Combination of nitrogen dioxide radicals with 8-oxo-7,8-dihydroguanine and guanine radicals in DNA: oxidation and nitration end-products. J Am Chem Soc 127, 2191–2200, https://doi.org/10.1021/ja044390r (2005).
Gaidamakova, E. K., Neumann, R. D. & Panyutin, I. G. Site-specific strand breaks in RNA produced by (125)I radiodecay. Nucleic Acids Res 30, 4960–4965, https://doi.org/10.1093/nar/gkf622 (2002).
Furochi, H. et al. Overexpression of osteoactivin protects skeletal muscle from severe degeneration caused by long-term denervation in mice. J Med Invest 54, 248–254 (2007).
Marin, M. P. et al. Vitamin A deficiency alters the structure and collagen IV composition of rat renal basement membranes. J Nutr 135, 695–701, https://doi.org/10.1093/jn/135.4.695 (2005).
Weisse, K., Brandsch, C., Hirche, F., Eder, K. & Stangl, G. I. Lupin protein isolate and cysteine-supplemented casein reduce calcification of atherosclerotic lesions in apoE-deficient mice. Br J Nutr 103, 180–188, https://doi.org/10.1017/S0007114509991565 (2010).
Jain, A. et al. TRP-channel-specific cutaneous eicosanoid release patterns. Pain 152, 2765–2772, https://doi.org/10.1016/j.pain.2011.08.025 (2011).
Ohsaki, A., Tanuma, S. I. & Tsukimoto, M. TRPV4 Channel-Regulated ATP Release Contributes to gamma-Irradiation-Induced Production of IL-6 and IL-8 in Epidermal Keratinocytes. Biol Pharm Bull 41, 1620–1626, https://doi.org/10.1248/bpb.b18-00361 (2018).
Everaerts, W., Nilius, B. & Owsianik, G. The vanilloid transient receptor potential channel TRPV4: from structure to disease. Prog Biophys Mol Biol 103, 2–17, https://doi.org/10.1016/j.pbiomolbio.2009.10.002 (2010).
Gao, X., Wu, L. & O’Neil, R. G. Temperature-modulated diversity of TRPV4 channel gating: activation by physical stresses and phorbol ester derivatives through protein kinase C-dependent and -independent pathways. J Biol Chem 278, 27129–27137, https://doi.org/10.1074/jbc.M302517200 (2003).
Montell, C., Birnbaumer, L. & Flockerzi, V. The TRP channels, a remarkably functional family. Cell 108, 595–598, https://doi.org/10.1016/s0092-8674(02)00670-0 (2002).
Vriens, J. et al. Cell swelling, heat, and chemical agonists use distinct pathways for the activation of the cation channel TRPV4. Proc Natl Acad Sci USA 101, 396–401, https://doi.org/10.1073/pnas.0303329101 (2004).
Bauge, C., Leclercq, S., Conrozier, T. & Boumediene, K. TOL19-001 reduces inflammation and MMP expression in monolayer cultures of tendon cells. BMC Complement Altern Med 15, 217, https://doi.org/10.1186/s12906-015-0748-7 (2015).
Di Girolamo, N., Lloyd, A., McCluskey, P., Filipic, M. & Wakefield, D. Increased expression of matrix metalloproteinases in vivo in scleritis tissue and in vitro in cultured human scleral fibroblasts. Am J Pathol 150, 653–666 (1997).
Huang, C. H. et al. Hinokitiol Exerts Anticancer Activity through Downregulation of MMPs 9/2 and Enhancement of Catalase and SOD Enzymes: In Vivo Augmentation of Lung Histoarchitecture. Molecules 20, 17720–17734, https://doi.org/10.3390/molecules201017720 (2015).
Im, A. R., Nam, K. W., Hyun, J. W. & Chae, S. Phloroglucinol Reduces Photodamage in Hairless Mice via Matrix Metalloproteinase Activity Through MAPK Pathway. Photochem Photobiol 92, 173–179, https://doi.org/10.1111/php.12549 (2016).
Biswas, M., Kwong, E. K., Park, E., Nagra, P. & Chan, J. Y. Glycogen synthase kinase 3 regulates expression of nuclear factor-erythroid-2 related transcription factor-1 (Nrf1) and inhibits pro-survival function of Nrf1. Exp Cell Res 319, 1922–1931, https://doi.org/10.1016/j.yexcr.2013.04.013 (2013).
Kumar, H. et al. Safety and tolerability of intradiscal implantation of combined autologous adipose-derived mesenchymal stem cells and hyaluronic acid in patients with chronic discogenic low back pain: 1-year follow-up of a phase I study. Stem Cell Res Ther 8, 262, https://doi.org/10.1186/s13287-017-0710-3 (2017).
Gasparini, L. S. et al. In vitro Cell Viability by CellProfiler((R)) Software as Equivalent to MTT Assay. Pharmacogn Mag 13, S365–S369, https://doi.org/10.4103/0973-1296.210176 (2017).
Justus, C. R., Leffler, N., Ruiz-Echevarria, M. & Yang, L. V. In vitro cell migration and invasion assays. J Vis Exp, https://doi.org/10.3791/51046 (2014).
Liang, C. C., Park, A. Y. & Guan, J. L. In vitro scratch assay: a convenient and inexpensive method for analysis of cell migration in vitro. Nat Protoc 2, 329–333, https://doi.org/10.1038/nprot.2007.30 (2007).
Lareu, R. R., Zeugolis, D. I., Abu-Rub, M., Pandit, A. & Raghunath, M. Essential modification of the Sircol Collagen Assay for the accurate quantification of collagen content in complex protein solutions. Acta Biomater 6, 3146–3151, https://doi.org/10.1016/j.actbio.2010.02.004 (2010).
Palko, J. R. et al. Biomechanical properties and correlation with collagen solubility profile in the posterior sclera of canine eyes with an ADAMTS10 mutation. Invest Ophthalmol Vis Sci 54, 2685–2695, https://doi.org/10.1167/iovs.12-10621 (2013).
Samuel, C. S. Determination of collagen content, concentration, and sub-types in kidney tissue. Methods Mol Biol 466, 223–235, https://doi.org/10.1007/978-1-59745-352-3_16 (2009).
Kim, J. S., In, C. H., Park, N. J., Kim, B. J. & Yoon, H. S. Comparative study of rheological properties and preclinical data of porous polycaprolactone microsphere dermal fillers. J Cosmet Dermatol, https://doi.org/10.1111/jocd.13076 (2019).
Yamashina, M., Takami, T., Kanemura, T., Orii, T. & Ojima, A. Immunohistochemical demonstration of complement components in formalin-fixed and paraffin-embedded renal tissues. Lab Invest 60, 311–316 (1989).
Skilbeck, N. W. Immunofluorescent staining of leptospires in pepsin treated histologic sections. Stain Technol 61, 273–278, https://doi.org/10.3109/10520298609109953 (1986).
Author information
Authors and Affiliations
Contributions
Beom Joon Kim, Jong Hwan Kim and Tae-Rin Kwon designed research. Sung Eun Lee, Yoo Na Jang and Jong Hwan Kim performed research. Tae-Rin Kwon, Hye Sung Han and Beom Joon Kim analyzed data. Seog Kyun Mun, Tae-Rin Kwon, Jong Hwan Kim and Beom Joon Kim interpreted data. Jong Hwan Kim, Tae-Rin Kwon and Beom Joon Kim wrote the paper. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, J.H., Kwon, TR., Lee, S.E. et al. Comparative Evaluation of the Effectiveness of Novel Hyaluronic Acid-Polynucleotide Complex Dermal Filler. Sci Rep 10, 5127 (2020). https://doi.org/10.1038/s41598-020-61952-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-61952-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.