Abstract
Multiple risk factors are associated with adverse pregnancy outcomes (APO), but how all these different factors combine and accumulate remains unknown. The objective of this observational retrospective study was to describe the accumulation of multiple vulnerability markers in pregnant women living in an urban area. Women living in Besançon (France) who delivered between 2005 and 2009 were included. Individual data were collected from the obstetrical records while environmental exposures were collected using environmental prediction models. The accumulation of 15 vulnerability markers, grouped into six dimensions (maternal age, smoking, body mass index (BMI), socio-economic, medico-obstetrical and environmental vulnerabilities) was described and analyzed in comparison with four APO. Among the 3686 included women, 20.8% were aged under 20 or over 34 and 21.9% had an extreme pre-pregnancy BMI. 18.8% declared smoking during pregnancy. Women exposed to socio-economic, medico-obstetrical or environmental vulnerability were 14.2%, 31.6% and 42.4% respectively. While 20.6% were not exposed to any marker, 18.8% accumulated three or more dimensions. The risk of APO increased significantly with the cumulative number of vulnerabilities. Define and validate a vulnerability score could be useful to identify vulnerable women, adapt their pregnancy monitoring and help policy makers to implement appropriate education or health promotion programs.
Similar content being viewed by others
Introduction
Adverse pregnancy outcomes (APO), such as preterm birth (PTB), low birthweight (LBW) preeclampsia or ante-partum hemorrhage, are important indicators for the health of the newborns and infants. In addition, growth and developmental delays in utero may influence the subsequent health status of individuals, including increased mortality and morbidity in childhood and an elevated risk of coronary heart disease, hypertension and diabetes in adulthood1,2. Multiple and varied etiologies and/or risk factors are associated with these APO; they combine in complex ways and could be related to medico-obstetrical, socio-demographic, behavioral and/or environmental determinants.
Obstetric history is well known to influence pregnancy outcome. Women with history of prior PTB have indeed higher risk for preterm delivery in a subsequent pregnancy compared with those with a prior term birth3. Abnormalities of the female reproductive tract and uterine scar also increase the risk for adverse pregnancy outcome4,5. Various pregnancy characteristics have been associated with PTB, LBW, preeclampsia or ante-partum hemorrhage. Obstetrical disorders such as hypertension, diabetes, genitourinary infections are identified as risk factors of adverse birth outcomes6. Multiple gestations carry a substantial risk of preterm delivery, and results in 15–20% of all PTBs. Nearly 60% of twins are born preterm6. Of course, multiple gestations are also closely linked to birthweight (BW). After 33 weeks of gestation, BW of twins started to deviate from singletons (difference of 900 grams at 42 weeks)7.
Demographic variables such as extremes in maternal age or black maternal ethnicity are also recognized as associated with APO8,9. The extremes of maternal pre-pregnancy body mass index (BMI) seem to be linked with an increase of the overall incidence of APO10. According to a recent meta-analysis, pre-pregnancy underweight increases the risk of LBW11. Some maternal behaviors are identified as preventable risk factors for an unsuccessful pregnancy outcome. Smoking during pregnancy has been associated with fetal growth restriction, placenta praevia (PP) and PTB12,13. Weaker evidence suggests an adverse effect of environmental tobacco smoke, heavy alcohol or cocaine use14. Socio-economic deprivation has been shown to be linked to access to care, behaviors during pregnancy, and pregnancy outcomes15,16,17.
The last decade provide an increasing evidence of the link between environment and pregnancy outcome. A higher risk of fetal growth restriction in relation to air pollution exposure was reported by main of the studies dealing with carbon monoxide (CO), nitrogen dioxide (NO2) or particulate matter (PM10, PM2.5)18,19,20,21. Effects on PTB appears to be more discussed18,19,20,22. According to a recent review of the literature, there is some suggestive evidence of adverse associations with environmental noise, especially for LBW23,24. Otherwise, few studies demonstrate a benefic effect of maternal proximity to green spaces on BW25,26.
However, most studies focus on only one determinant or one class of determinant and/or their influence on pregnancy outcome (when considered, the other determinants are treated as potential confounding variables). So, the distribution of all these determinants and how they potentially accumulate in the population of pregnant women is still largely unknown. Considering simultaneously all of these determinants could help define a concept of global vulnerability. This concept of vulnerability is very broad here: it is not only a socio-economic vulnerability but an interaction between various causes: genetic, socio-economic, psychological and environmental… To our knowledge, such a descriptive approach was never conducted in a large pregnant women population-based study.
The main objective of this article was to describe the distribution of identified vulnerability markers related to medico-obstetrical, demographic, behavioral and environmental dimensions, and to describe their potential accumulation in a population of pregnant women living in a middle-sized urban area (Besançon, France). Indeed, in Europe, cities of 100,000 to 500,000 inhabitants are considered to be “medium-sized”27. They define the largest category of city in demographic terms, hosting more than 44% of the European population28.
The second objective was to analyze the relationship between vulnerability accumulation and some adverse pregnancy complications and outcomes: preeclampsia, vaginal bleeding in the second and third trimesters, PTB and LBW.
Methods
Population
This epidemiological observational retrospective study included all pregnancies resulting in singleton births that occurred in the University Hospital of Besançon between 1 January 2005 and 31 December 2009 and whose mother, at the delivery, aged 18 and over and lived in Besançon City (a medium-sized city in France). Both stillborn and liveborn infants newborns whose birth occurred after 22 completed weeks of gestation and/or with a birthweight of 500 g or above were included. Mothers were considered only once in the study to ensure independence of observations: in case of repeated deliveries during the period, one episode has been randomly selected and the others were excluded. Multiple pregnancies were not included because of special characteristics in terms of duration and fetal growth compared to all pregnancies. Induced abortions, pregnancies with missing or invalid data for delivery date or address of residence at the baby’s birth were excluded.
Study variables
All except environmental markers were obtained from the computerized obstetrical record of Besançon University Hospital (DIAMMTM software), using International Classification diseases ICD-10 codes which were inserted by clinicians at the date of completion of the medical records.
Vulnerability variables
A pragmatic approach was conducted to select variables that could be used to define vulnerability. Selection criteria were as follows. To be retained, factors should be suspected or identified as risk factors of adverse birth outcomes. They should concern the period before pregnancy or the first trimester of pregnancy, which was defined by a window period of 15 weeks from the date of last menstrual period. Among them, medico-obstetrical and demographic markers were retained according to the data availability in the personal medico-obstetrical records, and were collected during current management of delivery. Furthermore, accuracy in the medical database had to be very high, and missing data had to be very low. For example, due to the retrospective nature of the study, known factors of APO such as alcohol consumption during pregnancy had to be excluded from the study because of important downward bias. The women address at the date of delivery was used to geocode the residential building and to define characteristics of the environmental living neighborhood. Fifteen variables were finally retained to describe pregnancy vulnerability (Table 1).
The neighborhood deprivation index was created for the city of Besançon, according to the approach developed by Lalloué et al.29. The statistical unit was the IRIS (Îlots Regroupés pour l’Information Statistique), a geographical unit currently used by the French National Institute of Statistics and Economic Studies for population censuses (approximately 2000 individuals with relatively homogeneous social characteristics). Variables related to family and household, immigration and mobility, employment and income, education and housing were extracted from 2008 INSEE database. Eighteen variables were selected among the 39 variables most often used in the literature29,30,31. (Supporting Information). The first component of a principal component analysis (PCA) was used to calculate the socioeconomic index after a reduction step and standardization. Women living in an IRIS ranked in the tenth decile of the socio economic index were considered to have a very low neighborhood deprivation level.
Noise and NO2 environmental exposures have been assessed by environmental prediction models. The same inputs were used for the two models: meteorological observations, topographic data, shape, size, height and position of both roads and buildings, railway and road traffic data for each segment of the city32. Maps of night noise levels and NO2 levels have been modeled at the city scale, using the MITHRA-SIG (noise), Circul’Air and ADMS-Urban (air) softwares21,22,33,34. Both noise and NO2 maps have been validated by measurement campaigns. To account for the temporal variability of weather conditions and the seasonal variations in concentrations of pollutants in the air, monthly maps have been used to calculate indicators of exposure to NO2. For each woman, monthly NO2 exposure level during pregnancy has been calculated. European NO2 threshold of 40 µg/m3 and the WHO threshold of 55 dB(A) for the night noise level (LAeq,night) were used to define environmental exposure35.
Vulnerability was considered in two steps. The 15 markers were first independently analyzed. Then, 6 vulnerability dimensions were created (and coded as at least one marker observed: yes or no). Three dimensions were single-marker (“extreme” maternal age, maternal smoking during pregnancy, pre-pregnancy body mass index) and three dimensions were multi-markers (medico-obstetrical, socio-economic status, environment and neighborhood). Because it could not be excluded that hypertension, diabetes and/or genitourinary infection markers records could concern events that had occurred during second or third trimester of pregnancy, sensitivity analyses were performed by successively removing these markers.
Adverse pregnancy outcomes
Gestational age at delivery was based on the last menstrual period or on ultrasonography during the first trimester. Preterm delivery was defined by a childbirth before 37 weeks of pregnancy and LBW by a weight at birth under 2500 grams. Vaginal bleeding in the second and third trimesters referred to an episode of bleeding after 28 weeks of gestation, including retro-placental hematoma and bleeding because of placenta praevia (International Classification diseases ICD-10 codes: O45, O46, O441 and P021). Preeclampsia and eclampsia referred to ICD-10 codes O14 and O15.
Statistical analysis
The results of the descriptive phase are expressed as frequencies and percentages (%) and 95% confidence interval (CI). Chi-square test was used to test for the difference of distribution of vulnerability among the pregnant women with or without the medical events. Cochran-Armitage test was used to test for trend of increasing or decreasing of the medical events in each of the vulnerability classes. Significance level was set at P < 0.05. Bivariate logistic regressions were performed to analyze the relationship between each APO and vulnerabilities or dimensions classes. Predicted probabilities of APO were calculated for each combination of the six dimensions.
Databases were managed with SAS version 9.4 software (SAS Institute, Cary, NC) and Microsoft Excel 2010. Statistical analyses were performed with R and SAS 9.4, the R package SesIndexCreatoR29 for the creation of neighborhood deprivation index and R package ggplot2 for plots.
Ethical approval and informed consent
This study was approved by the French National Advisory Committee for the Treatment of Information in Health Research (CCTIRS) and by the French data protection authority (CNIL) [Reference number: 915261]. All methods were carried out in accordance with the ethical standards of CNIL and the Declaration of Helsinki. The requirement for patient consent was waived by the CNIL because of the retrospective nature of the study. A letter of information was sent to each participant. Women who opposed the processing of their data were excluded from the study. All records were anonymized prior to analysis.
Results
Among the 11 630 births identified, 4622 births (39.7%) with mother’s home address located in Besançon. Among them, 936 births were excluded for the following reasons: Families’ objection to processing of their medical data (n = 10), maternal age less than 18 years (n = 37), missing delivery date (n = 3), missing birthweight (n = 2), birthweight under 500 grams (n = 4), unidentifiable address of residence (n = 14), multiple pregnancies (n = 199) and excluded episodes due to repeated pregnancies (n = 667). Finally, 3686 singleton pregnancies were included in the analysis.
Characteristics of mothers, pregnancies and newborns
The observed maternal age was 29.6 years (standard deviation SD = 5.5) on average. Over half the number of mothers were nulliparous and 67% delivered by non-instrumental vaginal delivery. The average birthweight was 3225.0 g (SD = 573.4). The prematurity rate was 7.2% and the rate of low birthweight was 7.3% (Table 2).
Pregnancy vulnerability
The distributions of each vulnerability marker alone and among the 6 dimensions are presented in Table 3.
The proportion of women aged under 20 or over 34 years old at the baby’s birth was 20.8%, while 21.9% of women had a pre-pregnancy BMI < 18.5 or ≥30 kg/m2. Maternal smoking during pregnancy was declared by 18.8% of included women. Fourteen percent of the woman presented one or more markers of socio economic vulnerability; this percent reached 31.6 and 42.4 when considering one or more medico-obstetrical and environmental vulnerabilities, respectively.
Distribution of women according to their vulnerabilities accumulation
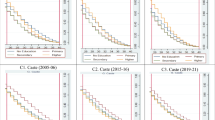
No marker of vulnerability was recorded for 758 women (20.6%), while four markers or more were simultaneously recorded for 376 women (10.2%) (Fig. 1A); 188 (5.1%) women were concerned by four or more of the six vulnerability dimensions (Fig. 1B). One woman was exposed to eight of the fifteen vulnerability markers and two women to the six vulnerability dimensions.
Vulnerabilities accumulation and proportions of APO
An increase of the percent of APO was observed when the number of vulnerability markers increased; the same increasing trends were observed when considering the vulnerability dimensions (all P ≤ 0.03) (Supplementary Tables S1 and S2). Tables 4 and 5 summarize the odds-ratio (OR) of APO according to the observed number of vulnerability markers (Table 4) or the observed number of vulnerability dimensions (Table 5). APO were associated with a higher number of vulnerabilities and dimensions. For example, a higher number of dimensions was significantly associated with preterm birth, with OR = 1.49 (95% CI = 1.01–2.19 among women with two vulnerability dimensions and OR = 2.14 (95% CI = 1.24–3.72) among those with four or more of the six vulnerability dimensions, compared to women without any vulnerability (P = 0.037). Sensitivity analyses were performed by successively removing three markers: hypertension, diabetes and genitourinary infections. The results were very close to those observed with the 15 markers (Supplementary Tables S3 and S4).
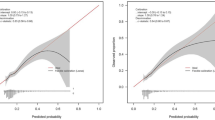
The modulation of the predicted probability of at least one APO among all the different combinations of the vulnerability dimensions is presented in Fig. 2.
Discussion
The vulnerability markers were differently distributed among pregnant women, from less than 2% to more than 20%. However, about 80% of the pregnant women were concerned by at least one vulnerability marker and nearly half (45.5%) accumulated two or more markers. Eleven percent were exposed to at least four of the six vulnerability categories. In addition, the more women combined vulnerabilities, the more their probability of adverse birth outcomes increased.
The study population included patients from public university hospital and did not cover deliveries managed by the private hospital. However, the main characteristics observed in our sample were similar to those observed in the French perinatal survey performed in 2010, especially the mean of maternal age, the percentages of low birthweight and preterm birth36. The main limitation relates to the retrospective recording of vulnerability markers, especially the characterization of medico-obstetrical vulnerabilities and their distinction from APO. The retrospective collect of data from computerized obstetric records could have lead, in some cases, to misclassifications due to a lack of precision. But, when omitting the three less reliable markers, sensitivity analyses produced very close results. Several markers should have also been underestimated, especially smoking during pregnancy. Environmental markers were directly extracted from geocoded mother address using a completely reproducible process and a special attention was paid on collecting the actual address of women at delivery and not the last address recorded in the hospital information system.
The choice of the vulnerability markers was not easy and several factors could miss in the list. The selection was based on the literature and also on the availability of reliable data from medical records. Markers such as addictive behavior were not retained because of the risk of very low rate of identification. Despite being known as a major factor, ethnicity was not available for this approach. Because of legal restrictions, this information is not commonly recorded in official French databases. To select medical markers, we referred to the recommendations of the French National Authority for Health (HAS) about “monitoring and guidance of pregnant women based on risk situations identified”37. The goal was here to separate the diseases identified at the start of the pregnancy (or considered as vulnerabilities implying monitoring to prevent obstetrical complications) and the real APO (i.e. serious complications of late pregnancy, preterm birth or low birthweight). A history of hypertension or pregnancy-induced hypertension was then considered as medico-obstetrical risk factors while preeclampsia and eclampsia were considered as APO.
Environment markers were selected using the same rules. Road traffic is often the main source of air pollution in medium-sized cities like Besançon, and NO2 is a gaseous pollutant known to be a good indicator of road traffic33. Adverse effects are frequently encountered in population expose to noise: annoyance, disturbed sleep, increased risk of cardiovascular disease38. Thus, our team recently showed that these two former pollutants only partially overlap32. The presence or absence of wooded area in the 100 meters around the residence building were used as an indicator of surrounding greenness25,26. If some marker could be discussed, the similar results obtained by considering individually each marker or grouped by dimensions suggest that the results could not be too sensitive to the choice of the study markers.
To our knowledge, this is the first study that describes the exposure to multiple sources of vulnerability (both individual and environmental) during pregnancy in an urban area, without focusing on the effect of one factor or one class of factors on pregnancy outcome. Despite low to moderate proportion of women concerned by each of the selected markers, nearly 80% were exposed to vulnerability markers during pregnancy. Women with no vulnerability markers could be seen as slightly over-represented: considering the observed proportion of women among whom each marker was recorded, the expected proportion would be 16% (based on the hypothesis of independency of markers). Conversely, about 10% of women cumulated more than 3 vulnerability markers. Moreover, when considering the multi-markers dimensions, the gap between the “at least one marker” proportion and the proportion of each of the concerned markers suggest that the markers only partially overlap. Thus, our results suggest: i) a tendency for accumulation of markers in a part of the pregnant women, ii) an accumulation of markers from different vulnerability dimensions rather than from the same dimensions.
The dose/effect relationship between the number of the vulnerabilities the women accumulated and the probability of adverse birth outcomes enhance the interest of our approach. A partition of women in three groups could be proposed. Women with no marker are associated with a lower (but not null) probability of adverse pregnancy outcome. This is in line with the unexplained proportion of APO regularly observed, such as with PTB39. No threshold was identified, but women with two or more markers appeared to be over the national risk of adverse pregnancy outcome36. Finally, in an analytic point of view, markers are missing, such as genetic, behavioral and occupational factors, but our approach was pragmatic and focused on easily and currently recorded data.
One of the limits of the results relies on study site. Besançon city is a European “medium-sized” city (i.e. city of 100,000 to 500,000 inhabitants)27. Environmental pollution (especially air pollution) and social disparity are expected to be higher in larger cities, which could conduct to a higher proportion of accumulation of vulnerabilities markers in a part of the population living in deprived areas.
We worked on markers and dimensions approaches. In a clinical perspective, using only six dimensions would be easily useable and understandable, and a score would potentially be easier to use with only six dimensions, rather than fifteen markers. About the determination of relevant threshold on the number of markers or dimensions, the answer is not obvious as the first results seem to acknowledge a linear or monotonous growth depending on the markers’ accumulation, and needs to be determined. The results of our study are however not directly applicable, and will need to be confirmed with complementary analyses: Building a score, pondering the markers and then providing an external validation of this score. Modelling could also simultaneously take account of the different defined outcomes, using multivariate generalized linear mixed models, rather than using a unique restrictive “at least one” outcome. Concerning the environmental dimension, results are not currently directly applicable in routine practice. Indeed, environmental and neighborhood indicators are not automatically accessible for every patient. A solution could be the use of proxy indicators. For instance, the distance to a major pollution source such as railway or high traffic road, predefined neighborhoods classifications or small area contextual estimations. Maps with an integrated tool of query processing using home address could also be implemented in clinical structures for this purpose. Considering the growing interest for environmental impact of health, and the spreading awareness of environmental risks on maternal health, it is likely that such approaches will be increasingly proposed in routine practice in the foreseeable future.
In conclusion, by combining medical, behavioral, socio-economic and environmental markers, this pragmatic study shows that vulnerabilities are not homogenously distributed and tend to accumulate in a part of the pregnant women. This accumulation could be seen as a particular risk of adverse pregnancy outcome and could be connected to the concept of Exposome40. One perspective could be to define and validate a vulnerability score. This study confirms also the need to identify vulnerable women as early as possible during pregnancy to adapt their pregnancy monitoring. Moreover, targeting vulnerable populations of women across small local urban area level could help policy makers to implement appropriate education or health promotion programs to specific areas of the city.
References
Osmond, C. & Barker, D. J. Fetal, infant, and childhood growth are predictors of coronary heart disease, diabetes, and hypertension in adult men and women. Environ. Health Perspect. 108(Suppl 3), 545–553 (2000).
Dalziel, S. R., Parag, V., Rodgers, A. & Harding, J. E. Cardiovascular risk factors at age 30 following pre-term birth. Int. J. Epidemiol. 36, 907–915 (2007).
Kazemier, B. M. et al. Impact of obstetric history on the risk of spontaneous preterm birth in singleton and multiple pregnancies: a systematic review. BJOG Int. J. Obstet. Gynaecol. 121, 1197–1208, discussion 1209 (2014).
Hiersch, L. et al. The association between Mullerian anomalies and short-term pregnancy outcome. J. Matern.-Fetal Neonatal Med. Off. J. Eur. Assoc. Perinat. Med. Fed. Asia Ocean. Perinat. Soc. Int. Soc. Perinat. Obstet. 29, 2573–2578 (2016).
Deneux-Tharaux, C. Women with previous caesarean or other uterine scar: epidemiological features. J. Gynecol. Obstet. Biol. Reprod. (Paris) 41, 697–707 (2012).
Goldenberg, R. L., Culhane, J. F., Iams, J. D. & Romero, R. Epidemiology and causes of preterm birth. Lancet Lond. Engl. 371, 75–84 (2008).
Gielen, M. et al. Twin-Specific Intrauterine ‘Growth’ Charts Based on Cross-Sectional Birthweight Data. Twin Res. Hum. Genet. 11, 224–235 (2008).
Weng, Y.-H., Yang, C.-Y. & Chiu, Y.-W. Risk Assessment of Adverse Birth Outcomes in Relation to Maternal Age. PloS One 9, e114843 (2014).
Schaaf, J., Liem, S., Mol, B., Abu-Hanna, A. & Ravelli, A. Ethnic and Racial Disparities in the Risk of Preterm Birth: A Systematic Review and Meta-Analysis. Am. J. Perinatol. 30, 433–450 (2012).
Lynch, A. M. et al. Association of extremes of prepregnancy BMI with the clinical presentations of preterm birth. Am. J. Obstet. Gynecol. 210, 428.e1–428.e9 (2014).
Yu, Z. et al. Pre-Pregnancy Body Mass Index in Relation to Infant Birth Weight and Offspring Overweight/Obesity: A Systematic Review and Meta-Analysis. PLoS ONE 8, e61627 (2013).
Cnattingius, S. The epidemiology of smoking during pregnancy: smoking prevalence, maternal characteristics, and pregnancy outcomes. Nicotine Tob. Res. Off. J. Soc. Res. Nicotine Tob. 6(Suppl 2), S125–140 (2004).
Nabet, C., Ancel, P.-Y., Burguet, A. & Kaminski, M. Smoking during pregnancy and preterm birth according to obstetric history: French national perinatal surveys: Smoking and preterm birth. Paediatr. Perinat. Epidemiol. 19, 88–96 (2005).
Savitz, D. A. & Murnane, P. Behavioral Influences on Preterm Birth: A Review. Epidemiology 21, 291–299 (2010).
Metcalfe, A., Lail, P., Ghali, W. A. & Sauve, R. S. The association between neighbourhoods and adverse birth outcomes: a systematic review and meta-analysis of multi-level studies. Paediatr. Perinat. Epidemiol. 25, 236–245 (2011).
Hanke, W. Employment status of pregnant women in Central Poland and the risk of preterm delivery and small-for-gestational-age infants. Eur. J. Public Health 11, 23–28 (2001).
Opatowski, M., Blondel, B., Khoshnood, B. & Saurel-Cubizolles, M.-J. New index of social deprivation during pregnancy: results from a national study in France. BMJ Open 6, e009511 (2016).
Shah, P. S. & Balkhair, T. & Knowledge Synthesis Group on Determinants of Preterm/LBW births. Air pollution and birth outcomes: a systematic review. Environ. Int. 37, 498–516 (2011).
Stieb, D. M., Chen, L., Eshoul, M. & Judek, S. Ambient air pollution, birth weight and preterm birth: a systematic review and meta-analysis. Environ. Res. 117, 100–111 (2012).
Nieuwenhuijsen, M. J., Dadvand, P., Grellier, J., Martinez, D. & Vrijheid, M. Environmental risk factors of pregnancy outcomes: a summary of recent meta-analyses of epidemiological studies. Environ. Health Glob. Access Sci. Source 12, 6 (2013).
Mariet, A.-S. et al. Multiple pregnancies and air pollution in moderately polluted cities: Is there an association between air pollution and fetal growth? Environ. Int. 121, 890–897 (2018).
Barba-Vasseur, M. et al. Does low to moderate environmental exposure to noise and air pollution influence preterm delivery in medium-sized cities? Int. J. Epidemiol. 46, 2017–2027 (2017).
Ristovska, G., Laszlo, H. E. & Hansell, A. L. Reproductive outcomes associated with noise exposure - a systematic review of the literature. Int. J. Environ. Res. Public. Health 11, 7931–7952 (2014).
Nieuwenhuijsen, M. J., Ristovska, G. & Dadvand, P. WHO Environmental Noise Guidelines for the European Region: A Systematic Review on Environmental Noise and Adverse Birth Outcomes. Int. J. Environ. Res. Public. Health 14 (2017).
Agay-Shay, K. et al. Green spaces and adverse pregnancy outcomes. Occup. Environ. Med. 71, 562–569 (2014).
Dadvand, P. et al. Green space, health inequality and pregnancy. Environ. Int. 40, 110–115 (2012).
Boddy, M. Geographical Economics and Urban Competitiveness: A Critique. Urban Stud. 36, 811–842 (1999).
Giffinger, R., Fertner, C., Kramar, H. & Meijers, E.City-ranking of European Medium-Sized Cities. Proceedings of the Future of Cities. 51st IFHP World Congress, 2007, Copenhagen, Denmark, www.smart-cities.eu/download/city_ranking_final.pdf (2007).
Lalloue, B. et al. A statistical procedure to create a neighborhood socioeconomic index for health inequalities analysis. Int. J. Equity Health 12, 21 (2013).
Pornet, C. et al. Construction of an adaptable European transnational ecological deprivation index: the French version. J. Epidemiol. Community Health 66, 982–989 (2012).
Messer, L. C. et al. The development of a standardized neighborhood deprivation index. J. Urban Health Bull. N. Y. Acad. Med. 83, 1041–1062 (2006).
Tenailleau, Q. M. et al. Do outdoor environmental noise and atmospheric NO2 levels spatially overlap in urban areas? Environ. Pollut. 214, 767–775 (2016).
Tenailleau, Q. M., Mauny, F., Joly, D., François, S. & Bernard, N. Air pollution in moderately polluted urban areas: How does the definition of “neighborhood” impact exposure assessment? Environ. Pollut. 206, 437–448 (2015).
Pujol, S. et al. Urban ambient outdoor and indoor noise exposure at home: A population-based study on schoolchildren. Appl. Acoust. 73, 741–750 (2012).
World Health Organization (WHO). Night noise guidelines for Europe, http://www.euro.who.int/en/health-topics/environment-and-health/noise/publications/2009/night-noise-guidelines-for-europe (2009).
Blondel, B. Enquête périnatale 2010. Les naissances en 2010 et leur évolution depuis 2003, http://social-sante.gouv.fr/IMG/pdf/Les_naissances_en_2010_et_leur_evolution_depuis_2003.pdf (2011).
Haute Autorité de Santé (HAS). [Suivi et orientation des femmes enceintes en fonction des situations à risque identifiées], https://www.has-sante.fr/upload/docs/application/pdf/suivi_orientation_femmes_enceintes_synthese.pdf (2007).
World Health Organization (WHO). Burden of disease from environmental noise. Quantification of healthy life years lost in Europe, http://www.euro.who.int/en/what-we-do/health-topics/environment-and-health/noise/publications/2011/burden-of-disease-from-environmental-noise.-quantification-of-healthy-life-years-lost-in-europe (2011).
Muglia, L. J. & Katz, M. The enigma of spontaneous preterm birth. N. Engl. J. Med. 362, 529–535 (2010).
Buck Louis, G. M., Yeung, E., Sundaram, R., Laughon, S. K. & Zhang, C. The exposome–exciting opportunities for discoveries in reproductive and perinatal epidemiology. Paediatr. Perinat. Epidemiol. 27, 229–236 (2013).
Acknowledgements
This study was conducted as part of the initial phase of the “PremaBquA” project: Preterm delivery and Environmental multiple Exposure: Noise and Air in Urban areas. Computations have been performed on the supercomputer facilities of the Mésocentre of the university of Franche-Comté. The authors would like to acknowledge Alain Dussaucy and Odile Allemandet for their crucial help in extraction and management of medico obstetrical data. The authors are also grateful to the regional association for air quality monitoring Atmo Franche-Comté for the collaboration in this project. This work was supported by the French Environment and Energy Management Agency (ADEME) under the National Environmental Research and Occupational Health Program 2012 of the French Agency for Food, Environmental and Occupational Health & Safety (ANSES) [grant number 1217C0065].
Author information
Authors and Affiliations
Contributions
F.M., N.B. and A.S.M. conceived the design of this present study; A.E., G.T. and D.R. provided its implementation and data collection; S.P., Q.T. and H.H. conducted the environmental data collection and analysis; M.B.V., A.B. and A.L.P. conducted statistical analysis; All authors contributed to the interpretation of the results; A.B. and M.B.V. drafted the manuscript; All authors critically revised the manuscript, read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Brembilla, A., Bernard, N., Pujol, S. et al. Pregnancy vulnerability in urban areas: a pragmatic approach combining behavioral, medico-obstetrical, socio-economic and environmental factors. Sci Rep 9, 18878 (2019). https://doi.org/10.1038/s41598-019-55005-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-55005-0
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.