Abstract
Docosahexaenoic acid (DHA) is a long-chain polyunsaturated fatty acid mainly found in fish oil. Although several studies have suggested that it can alleviate allergy symptoms, its mechanism of action remains to be elucidated. In the present study, we found that docosahexaenoyl ethanolamide (DHEA), a metabolite of DHA produced in the human body, exerts the anti-allergic activity in vitro and in vivo. DHEA suppressed degranulation of rat basophilic leukemia RBL-2H3 cells and bone marrow-derived mast cells in a dose-dependent manner without cytotoxicity. This occurred due to a decrease in Ca2+ influx, which is critical for mast cell degranulation. DHEA also suppressed IgE-mediated passive cutaneous anaphylaxis reaction in mice. In addition, DHEA was demonstrated to lessen an allergic symptom in a mouse model of pollinosis and to alter the production of IgE and cytokines secreted by splenocytes collected from the pollinosis mice. Taken together, this study indicates that DHEA is a promising anti-allergic agent as it inhibits mast cell degranulation and modulates other immune cells.
Similar content being viewed by others
Introduction
The prevalence of allergic diseases has been increasing worldwide over the last few decades. For example, the percentage of the population with seasonal allergic rhinitis, one of the most common allergic diseases in the population of Japan, has dramatically increased from 19.6% surveyed in 1998 to 29.8% in 20081. Similarly, in Europe, at least 25% of school-age children have an allergic disease2. Allergic diseases arise as a consequence of IgE-mediated hypersensitivity to a specific allergen3 and are often associated with an impaired quality of life. Therapeutic agents commonly used to treat IgE-mediated allergic diseases include antihistamines, mast cell stabilizers, and other drugs. Although antihistamines are the most commonly prescribed drug for ameliorating allergic symptoms, they sometimes cause adverse effects such as drowsiness and headaches4. Allergen immunotherapy is also a potential treatment for allergies, although there is a risk of serious adverse effects and the exact mechanisms underlying allergen immunotherapy are still not completely elucidated. Recently, food ingredients with anti-allergy activity are attracting attention because they can be safely used long term with no or little adverse effects, although their efficacy as anti-allergy activity is moderate when compared to pharmaceuticals. These food ingredients could be a way to decrease the severity of some allergic symptoms, such as those related to allergic rhinitis.
One such food ingredient is fish oil. A number of epidemiological studies have indicated that fish consumption is associated with decreased prevalence of allergies5,6. Docosahexaenoic acid or DHA ((4Z,7Z,10Z,13Z,16Z,19Z)-docosa-4,7,10,13,16,19-hexaenoic acid, Fig. 1) is a long-chain polyunsaturated fatty acid mainly found in fish oil, and several studies have suggested that it may be important in the reduction of allergies6,7 and have suggested possible mechanisms of action8,9; however, the mechanism underlying the anti-allergy effect of DHA still remains to be completely elucidated. Certain DHA metabolites, such as protectin and resolvin produced in the human body, have been reported to promote the resolution of inflammation10. In addition, α-linolenic acid and eicosapentaenoic acid, which are also long-chain polyunsaturated fatty acids, have been reported to exert an anti-allergic effect by being converted into 17,18-epoxyeicosatetraenoic acid11. We thus explored the anti-allergy activity of DHA metabolites on the stabilization of mast cells, since mast cells, which reside in various tissues, are known to be important key effector cells in IgE-mediated hypersensitivity reactions3. After a preliminary screening of several DHA metabolites, we found that DHA does not have a strong suppressive effect on mast cell degranulation but docosahexaenoyl ethanolamide or DHEA ((4Z,7Z,10Z,13Z,16Z,19Z)-N-(2-hydroxyethyl)docosa-4,7,10,13,16,19-hexaenamide, Fig. 1), a metabolite produced from DHA in the human body, does. In this study, we evaluated whether DHEA suppresses mast cell degranulation by conducting in vitro cell-based assays and in vivo mouse models of IgE-mediated hypersensitivity reactions. Consequently, we found that DHEA is a promising agent for alleviating allergic symptoms.
Results and Discussion
DHEA suppresses degranulation of RBL-2H3 cells and bone marrow-derived mast cells (BMMCs)
In this study, we focused on the effect of DHEA on mast cells. Mast cells are one of the important targets for alleviating allergic symptoms because they play a critical role in IgE-mediated hypersensitivity reactions3. Upon exposure to a multivalent antigen, the IgE-bound high-affinity IgE receptor (FcεRI) on the plasma membrane is crosslinked, which elicits mast cell activation and induces degranulation, leading to the release of various de novo‐synthesized and preformed inflammatory mediators including histamine12. Histamine released from mast cells results in allergic inflammations such as tissue edema and mucus overproduction13. In this study, rat basophilic leukemia RBL-2H3 cells were used for in vitro cell-based assays because the cells express FcεRI on their plasma membrane and hence, have been used for investigations on the mechanism of mast cell degranulation14.
We at first examined the effect of DHEA and DHA on degranulation of RBL-2H3 cells and BMMCs. Anti-dinitrophenyl (DNP) IgE-sensitized RBL-2H3 cells or BMMCs were treated with various concentrations of DHEA or DHA and subsequently stimulated with DNP-human serum albumin (HSA). The amount of β-hexosaminidase released from cells was then determined by measuring the enzymatic activity which was used as a marker to evaluate the effect of DHEA or DHA on mast cell degranulation. β-Hexosaminidase is released along with histamine upon mast cell degranulation15, and the released amount is commonly used as an indicator of degranulation16. As shown in Fig. 2A, DHA did not suppress the degranulation of RBL-2H3 cells, or degranulation of BMMCs (Fig. 2B). DHA sodium salt has been previously reported to suppress degranulation of mouse BMMCs9, which seems to conflict with our observation. In the previous study, they used a higher concentration of DHA sodium salt (100 µM) for the degranulation assay. Thus, the inconsistency may be caused by different experimental conditions and materials.
DHEA suppresses degranulation of RBL-2H3 cells and BMMCs without cytotoxicity. The effect of DHEA and DHA on degranulation of RBL-2H3 cells (A) and of BMMCs (B). Cells sensitized with anti-DNP IgE were treated with various concentrations of DHEA or DHA or with 0.1% ethanol (vehicle). The cells were subsequently stimulated with DNP-HSA, and the enzymatic activity of β-hexosaminidase released from the cells was measured. Relative β-hexosaminidase release was calculated by comparing the enzymatic activity of DHEA-treated cells to that of the cells treated with 0.1% ethanol. The effect of DHEA on the viability of RBL-2H3 cells (C) and of BMMCs (D). Cells were treated with various concentrations of DHEA or with 0.1% ethanol (vehicle) for 24 h. The WST-8 reagent was then added to the culture medium, and the absorbance was measured. Relative cell viability was calculated by comparing the absorbance obtained from the cells treated with DHEA to that treated with 0.1% ethanol. Data are presented as the mean ± SEM (n = 3). Dunnett’s test was used to assess the statistical significance of the difference (*P < 0.05, **P < 0.01, ***P < 0.001) against control. N.S. indicates not statistically significant.
Subsequently, the effect of DHEA on degranulation was also examined. DHEA suppressed degranulation of RBL-2H3 cells in a concentration-dependent manner (Fig. 2A), which was statistically significant at 17 µM or higher concentrations. DHEA also suppressed degranulation of BMMCs in a concentration-dependent manner (Fig. 2B), which was statistically significant at 4.2 µM or higher concentrations, thereby showing that BMMCs are more sensitive to DHEA than RBL-2H3 cells. In higher concentrations of DHEA, degranulation was almost completely suppressed in BMMCs (Fig. 2B), whereas degranulation of RBL-2H3 cells was not strongly inhibited (Fig. 2A). This implies that the target protein of DHEA might be less expressed in RBL-2H3 cells than in BMMCs.
The effect of DHEA on the cell viability was then examined. RBL-2H3 cells were treated with various concentrations of DHEA for 24 h, and viable cell number was then estimated using the WST-8 reagent. As shown in Fig. 2C, there was no statistically significant difference in the viable cell number between DHEA-treated and non-treated cells. In addition, BMMCs were treated in the same way as RBL-2H3 cells, and the effect of DHEA on viability of BMMCs was evaluated. As shown in Fig. 2D, no cytotoxic effect of DHEA was found, suggesting that DHEA does not affect the cell viability at any concentration tested in this study. The result showed that the decreased release of β-hexosaminidase from RBL-2H3 cells and BMMCs is not caused by the cytotoxicity, but by the suppressive activity of DHEA on mast cell degranulation.
DHEA suppresses the increase in the intracellular Ca2+ concentration ([Ca2+]i) in RBL-2H3 cells
FcεRI aggregation initiates signaling cascades leading to the increase in [Ca2+]i. Elevation in [Ca2+]i is a principal signaling for mast cell degranulation17. We then examined the effect of DHEA on [Ca2+]i in RBL-2H3 cells using a fluorescent calcium indicator Fluo 4-AM. Anti-DNP IgE-sensitized and non-sensitized RBL-2H3 cells were loaded with Fluo 4-AM and then treated with 34, 67, or 135 µM DHEA or with 0.1% ethanol (vehicle) alone. The fluorescence was measured immediately upon the stimulation with DNP-HSA. As shown in Fig. 3A, [Ca2+]i increased immediately after stimulation of the vehicle-treated cells with the antigen, while [Ca2+]i did not change with no antigen stimulation. The increase in [Ca2+]i was suppressed in a concentration-dependent manner when the cells were treated with DHEA. Figure 3B shows the relative fluorescence intensity at 20 s after antigen stimulation. The relative fluorescence intensity was significantly reduced by treating the cells with DHEA, suggesting that DHEA reduces degranulation of RBL-2H3 cells by down-regulating the intracellular signaling cascade upstream of the Ca2+ influx.
DHEA suppresses the elevation in intracellular Ca2+ concentration. RBL-2H3 cells sensitized with anti-DNP IgE were incubated in the medium containing Fluo 4-AM. The cells were then treated with various concentrations of DHEA or with 0.1% ethanol (vehicle), and the fluorescent intensity was immediately monitored upon stimulation with DNP-HSA. Relative fluorescent intensity was calculated by comparing the fluorescent intensity after stimulation to that before stimulation. (A) Time course of intracellular Ca2+ concentration in RBL-2H3 cells. Data are presented as the mean of triplicate of wells. (B) Relative fluorescence intensity at 20 s after antigen stimulation. Data are presented as the mean ± SEM (n = 3). Dunnett’s test was used to assess the statistical significance of the difference (*P < 0.05, ***P < 0.001) against control (vehicle).
DHEA tends to down-regulate the intracellular signaling cascades involved in degranulation
Because DHEA suppressed the increase in [Ca2+]i of RBL-2H3 cells, DHEA was expected to modulate the intracellular signaling cascade involved in mast cell degranulation. We thus examined the effect of DHEA on the phosphorylation state of intracellular signaling proteins by immunoblot analysis. Anti-DNP IgE-sensitized RBL-2H3 cells were treated with 0, 17, 34, 67, or 135 µM DHEA for 30 min and subsequently stimulated with DNP-HSA for 5 min. The cells were then lysed and subjected to immunoblotting. The results showed that DHEA indicated a tendency to suppress the phosphorylation of Syk, phospholipase C-γ2 (PLCγ2), and Akt in a dose-dependent manner (Fig. 4). IgE-mediated FcεRI aggregation caused by cross-linking antibodies to antigens provokes intracellular signaling cascades leading to mast cell degranulation. Syk tyrosine kinase plays an essential role in mast cell degranulation and is activated immediately upon FcεRI stimulation, followed by the activation of PLCγ and Akt pathways18,19. PLCγ also plays a crucial role in the production of inositol 1,4,5-trisphosphate and in regulating intracellular Ca2+ mobilization, which leads to mast cell degranulation20. Inhibited phosphorylation of Syk and PLCγ2 has been shown to abolish FcεRI-mediated mast cell degranulation21,22. Akt is located downstream of Syk and is involved in the mast cell degranulation23. Overall, these results indicate that the suppressive effect of DHEA on mast cell degranulation might arise from the inhibition of Syk, which subsequently results in the down-regulation of Syk-PLCγ and Syk-Akt pathways, leading to reduced influx of Ca2+ into the cells and prevention of IgE-mediated degranulation of RBL-2H3 cells; however, statistical significance of the difference between DHEA-treated and non-treated cells was not observed. The reason might be that DHEA does not exert the degranulation-suppressive effect enough at the tested concentrations because the effect of DHEA is less potent in RBL-2H3 cells than in BMMCs in higher concentrations (Fig. 2A,B). In this study the suppressive activity/mechanism of DHEA is not addressing all signaling processes necessary for degranulation and thus under investigation.
DHEA tends to down-regulate intracellular signaling pathways related to degranulation of RBL-2H3 cells in a dose-dependent manner. RBL-2H3 cells sensitized with anti-DNP IgE were treated with 17, 34, 67, or 135 µM DHEA or with 0.1% ethanol (vehicle) and subsequently stimulated with DNP-HSA for 5 min. Each cell lysate was then prepared to use for immunoblot analysis. p-Syk, p-PLCγ2, and p-Akt indicate phosphorylated Syk (Tyr525/526), phosphorylated PLCγ2 (Tyr759), and phosphorylated Akt (Ser473), respectively. A representative blot from three independent experiments is shown. The ratio of phosphorylation is shown as bar graphs. Data are presented as the mean ± SEM of three independent experiments. Dunnett’s test was used to assess the statistical significance of the difference (**P < 0.01) against control (antigen, + ; DHEA, −). The original blots are shown in the supplementary information file.
DHEA attenuates IgE-mediated passive cutaneous anaphylaxis (PCA) reaction in vivo
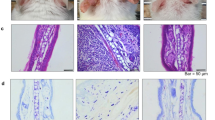
To determine whether DHEA could also suppress degranulation in vivo, we examined the in vivo activity of DHEA using the PCA reaction in mice. PCA is a localized cutaneous allergic response resulting from vascular hyperpermeability and plasma extravasation following the allergen exposure24 and is used as an animal model of IgE-mediated allergic response to evaluate the effect of bioactive molecules25. Because a large amount of DHEA was needed for animal experiments, we synthesized DHEA as described in the “Materials and Methods” section. Mice were administered DHEA at the dose of 50 mg/kg, 200 mg/kg, or 1,000 mg/kg, DHA at 1,000 mg/kg, fexofenadine hydrochloride at 50 mg/kg, or water at 1,000 mg/kg for 5 consecutive days from day 0 to day 4. With the exception of the intact group, mice were intradermally injected with anti-DNP IgE in an ear on day 3, and then all mice were intravenously injected with DNP-HSA and Evans blue dye on day 4 as shown in Fig. 5A. The absorbance of the dye in the tissue after extravasation was then measured. As shown in Fig. 6, the absorbance of the dye extracted from IgE-sensitized mice was much higher than that from non-sensitized mice, indicating that the PCA reaction occurred successfully. Fexofenadine hydrochloride, a selective histamine H1 receptor antagonist, was used as a positive control and significantly abolished PCA reaction. In addition, DHEA appeared to suppress the PCA reaction in a dose-dependent manner; only the highest dose used (1,000 mg/kg) yielded a significant result. DHA showed almost no effect on PCA test, corroborating that DHA itself did not have a suppressive effect on mast cell degranulation (Fig. 2A,B). The result suggested that, in mice, the 5-day intake of DHEA is effective in suppression of mast cell degranulation in vivo.
DHEA suppresses PCA reaction in a mouse model. Mice were orally administered DHEA, DHA, fexofenadine hydrochloride (positive control), or water (intact and control groups) for 5 consecutive days. One day before the final oral administration, an ear of mice was intradermally injected with anti-DNP IgE. One hour after the final oral administration, all mice were intravenously injected with DNP-HSA and Evans blue dye. After 30 min, the ear was excised, and the absorbance of the dye was measured. Data are presented as the mean ± SEM (n = 7–8). Dunnett’s test was used to assess the statistical significance of the difference (*P < 0.05, ***P < 0.001) against control.
DHEA and DHA alter biochemical parameters in a model of pollinosis
Japanese cedar (Cryptomeria japonica) pollen is one of the most common sources of allergens that elicit seasonal allergic rhinitis in Japan. We thus evaluated the effect of DHEA on allergic symptoms caused by Japanese cedar pollinosis using a mouse model. All mice, except intact group, were sensitized with Cry j1 and Cry j2 proteins, which are the major allergen contained in Japanese cedar pollens, as scheduled in Fig. 5B. Mice were orally administered DHEA at the dose of 1,000 mg/kg (DHEA group), DHA at 1,000 mg/kg (DHA group), or water (intact and control groups) at 1,000 mg/kg for seven consecutive days, and then an allergic symptom and serum IgE level were evaluated. The results showed that sneezing frequency of the control mice significantly increased compared with that of the intact mice (Fig. 7A). In addition, serum IgE level of the control mice was significantly higher than that of the intact mice (Fig. 7B). These data indicate that a mouse model of pollinosis was successfully established by sensitizing mice with Cry j1 and Cry j2. Intake of DHEA significantly reduced the sneezing frequency of mice compared with that of control mice (Fig. 7A), suggesting that DHEA blocks the histamine release from mast cells located in the nasal mucosa by suppressing degranulation. Interestingly, oral administration of DHA tended to reduce the sneezing frequency (P = 0.0677 against control) in spite of almost no effect in the PCA test, suggesting that DHA metabolites, not DHA itself, might exert a suppressive effect on mast cell degranulation or that DHA affects certain immune cells other than mast cells to alleviate allergic symptoms. Further investigation is now being conducted to determine the specific causes of this observation. The serum IgE level of the DHEA-administered and DHA-administered mice remained unchanged compared with that of the control mice (Fig. 7B). This result indicates that the mitigation effect of DHEA or DHA on the allergic symptom is not attributed to the decreased IgE production.
DHEA mitigates an allergic symptom of Japanese cedar pollinosis and alters the production of IgE and cytokines secreted by splenocytes collected from pollinosis mice. Mice were intraperitoneally injected on day 0 and intranasally treated on day 7, 14, 21, 28, and 35 to 39 with Cry j1 and Cry j2 (Japanese cedar pollen allergen). Mice in DHEA and DHA groups were dosed with DHEA and DHA, respectively, from day 35 to day 41, while control and intact groups were with water. On day 40, all mice were intranasally treated with Cry j1 and Cry j2, and the sneezing frequency was counted for 10 min. On day 41, the blood and spleen were collected. (A) Sneezing frequency of pollinosis mice after intranasal challenge with the allergen. (B) Serum IgE levels of pollinosis mice. Production of IgE (C), IFN-γ (D), IL-4 (E), IL-5 (F), IL-13 (G), and IL-10 (H) by splenocytes collected from pollinosis mice. Data are presented as the mean ± SEM (n = 8). Dunnett’s test was used to assess the statistical significance of the difference (*P < 0.05, **P < 0.01, ***P < 0.001) against control.
Because DHA appears to ameliorate allergic symptoms by regulating immune cells other than mast cells, we further explored the effect of DHEA and DHA by examining the responses of splenocytes collected from the Cry j1- and Cry j2-sensitized mice after evaluating their effect on the sneezing frequency. The splenocytes were cultured in the presence of allergen (Cry j1 and Cry j2) for 96 h after isolation, and the concentration of cytokines and IgE in the culture medium was measured. The results showed that the production of IgE (Fig. 7C), interferon-γ (IFN-γ; Fig. 7D), interleukin-5 (IL-5; Fig. 7F), IL-10 (Fig. 7G), and IL-13 (Fig. 7H) by splenocytes was significantly suppressed by oral administration of DHEA or DHA. In addition, the secretion of IL-4 tended to reduce, however not significantly, by intake of DHEA (P = 0.1066 against control; Fig. 7E) or of DHA (P = 0.3055). IL-4, IL-5, and IL-13 are classified as Th2 cytokines26. IL-4 and IL-13, in particular, are produced by T cells, mast cells, and basophils and known to induce class switching to IgE and gene expression of FcεRI, IgE, inflammatory cytokines, and chemokines27,28. Thus, DHEA and DHA seemed to affect T cells and mast cells to decrease production of IL-4 and IL-13, which leads to alleviation of allergic reactions. Because DHEA and DHA reduced the production of IL-5 and IL-13 greater than that of IL-4, it may affect the group 2 innate lymphoid cells, which secret IL-5 and IL-13 rather than IL-429. Some bioactives, such as gallic acid30 and skullcapflavone II31, attenuate allergic responses by reducing the expression of Th2 cytokines, such as IL-4, and by increasing Th1 cytokines, such as IFN-γ32,33; however, DHEA or DHA did not increase the production of Th1 cytokine IFN-γ (Fig. 6D). Thus, the mechanism of anti-allergic activity of DHEA and DHA is not to improve the Th1/Th2 balance. DHEA and DHA also significantly reduced the production of IL-10 (Fig. 6H), which is known to be secreted by regulatory T cells to suppress allergic inflammation34; however, some studies have demonstrated that IL-10 might have a facilitative effect on the development of allergy35,36. Takagi et al. (2005) demonstrated that the immunotherapy using allergen-specific T cell epitope peptides for inducing oral tolerance to pollinosis results in reduced production of IL-4, IL-5, IL-13, IL-10, and IFN-γ37. In addition, they showed reduced sneezing frequency, but unaffected serum IgE level in a mouse model of pollinosis. Their results support what we have observed in this study. Hence, the mechanism of anti-allergy activity of DHEA and DHA might be similar to inducing oral tolerance to an allergen. In Fig. 7, DHA was consistently less effective than DHEA in spite of being given at the same dose. The reason might be that DHA has less effect on T cells or other immune cells than DHEA or that the serum level of DHA is more readily reduced than that of DHEA after intake by being incorporated to membrane lipids in our body.
In conclusion, our study has demonstrated that DHEA is a promising agent for mitigating IgE-mediated allergic reactions. In vitro experiments revealed that DHEA suppresses degranulation of RBL-2H3 cells and BMMCs without cytotoxicity by affecting intracellular signaling pathways related to mast cell degranulation. The PCA experiment indicated that the intake of DHEA could suppress mast cell degranulation in vivo. The experiment using a mouse model of Japanese cedar pollinosis suggested that DHEA could mitigate allergic reactions by affecting not only mast cells but also other immune cells and that oral administration of DHA is effective in alleviating allergic reactions of pollinosis, although DHA is less effective than DHEA. It is still uncertain whether the anti-allergy effect of DHA comes from DHA itself or from DHEA that is converted from DHA after intake. Further investigation on the anti-allergy effect of DHA is now being conducted. Taken together, this study indicates that DHEA is a promising anti-allergic agent by inhibiting mast cell degranulation and by modulating other immune cells to mitigate allergic reactions.
Materials and Methods
Reagents
DHEA and DHA dissolved in ethanol were purchased from Cayman Chemical (Ann Arbor, Michigan, USA) and used for cell-based assays shown below. Dulbecco’s modified Eagle’s medium (DMEM), RPMI 1640 medium, fetal bovine serum (FBS), penicillin, streptomycin, bovine serum albumin (BSA), mouse anti-DNP monoclonal IgE, DNP-HSA conjugate, Triton X-100, and Evans blue dye were purchased from Sigma-Aldrich (St. Louis, MO, USA). Recombinant murine IL-3 and murine stem cell factor (SCF) were purchased from PeproTech (Rocky Hill, NJ, USA). Phycoerythrin (PE)-labelled anti-mouse CD117 and fluorescein isothiocyanate (FITC)-labelled anti-mouse FcεRIα were purchased from BioLegend (San Diego, CA, USA). Horseradish peroxidase (HRP)-labelled anti-rabbit IgG antibody and rabbit antibodies against Syk (#13198), phosphorylated Syk at Tyr525/526 (#2710), Akt (#4691), phosphorylated Akt at Ser473 (#4060), PLCγ2 (#3872), and phosphorylated PLCγ2 at Tyr759 (#3874) were purchased from Cell Signaling Technology (Danvers, MA, USA). Aluminium hydroxide gel was purchased from Fujifilm Wako Pure Chemical (Osaka, Japan). Fexofenadine hydrochloride was purchased from Tokyo Chemical Industry (Tokyo, Japan). Purified Japanese cedar pollen protein (Cry j1 and Cry j2) was purchased from Hayashibara (Okayama, Japan). An enzyme-linked immunosorbent assay (ELISA) kit to measure the IgE concentration was obtained from BioLegend (San Diego, CA, USA). ELISA kits to measure the concentration of IL-4, IL-5, IL-10, IL-13, and IFN-γ were obtained from Invitrogen (Carlsbad, CA, USA). All other chemicals were purchased from Fujifilm Wako Pure Chemical or Nacalai Tesque (Kyoto, Japan) unless otherwise noted.
Cells and cell culture
RBL-2H3 cells were obtained from the American Type Culture Collection (Rockvile, MD, USA) and cultured in DMEM supplemented with 100 U/mL of penicillin, 100 µg/mL of streptomycin, and 10% heat-inactivated FBS at 37 °C under humidified 5% CO2 in air.
To generate BMMCs, bone marrow cells were harvested from femurs of a BALB/c mouse at the age of 8 weeks by repeated flushing with phosphate-buffered saline (PBS, pH 7.4) and cultured in RPMI 1640 medium supplemented with 10% FBS, 2 mM L-glutamine, 1 mM pyruvate, 100 U/mL of penicillin, 100 μg/mL of streptomycin, and 4 ng/mL of murine IL-3. Nonadherent cells were transferred to fresh medium 3 d after cell harvest and differentiated into BMMCs over 4 weeks under the influence of IL-3 at the density of 1.0 × 106 cells/mL. SCF was applied at 40 ng/ml for the last 2 weeks. The differentiation status of BMMCs was analyzed using flow cytometry (BD FACSVerse, BD Biosciences, Franklin Lakes, NJ, USA) by staining with PE-labelled anti-mouse CD117 and with FITC-labelled anti-mouse FcεRIα. The purity of BMMCs was confirmed to be higher than 90%.
β-Hexosaminidase release assay
The assay was performed as previously reported38 with some modifications. RBL-2H3 cells or BMMCs were seeded at 4.0 × 104 cells/well in a 96-well culture plate (Corning, Corning, NY, USA) and sensitized with anti-DNP IgE (50 ng/mL) at 37 °C overnight. After washing the cells with modified Tyrode’s (MT) buffer (20 mM HEPES, 135 mM NaCl, 5 mM KCl, 1.8 mM CaCl2, 1 mM MgCl2, 5.6 mM glucose, and 0.05% BSA, pH 7.4) twice, the cells were treated with 120 μL of MT buffer containing various concentrations of DHEA or 0.1% (v/v) ethanol (vehicle) for 30 min at 37 °C. The cells were then stimulated with 10 μL of DNP-HSA (625 ng/mL) for 30 min at 37 °C. After stimulation, the supernatant was collected from each well, and the cells were sonicated in 130 μL of MT buffer containing 0.1% Triton X-100 for 5 s on ice. Both of the supernatant and cell lysate were transferred to a new 96-well microplate at 50 μL/well and incubated for 5 min at 37 °C. One hundred μL of 3.3 mM 4-nitrophenyl 2-acetamido-2-deoxy-β-D-glucopyranoside dissolved in 0.1 M citrate buffer (pH 4.5) were then added to each well and incubated for 25 min at 37 °C. The enzyme reaction was terminated by adding 100 µL of 2 M glycine buffer (pH 10.4), and the absorbance was measured at 405 nm using a microplate reader (SH-8000Lab; Corona Electric, Hitachinaka, Japan). A β-hexosaminidase release rate (%) was calculated as follows:
in which “A” is the absorbance of each well.
Cell viability assay
Toxicity of DHEA to RBL-2H3 cells or to BMMCs was evaluated using Cell Count Reagent SF (Nacalai Tesque) containing 2-(2-methoxy-4-nitrophenyl)-3-(4-nitrophenyl)-5-(2,4-disulfophenyl)-2H-tetrazolium or WST-8 according to the manufacturer’s instructions. After cells were seeded into each well of a 96-well culture plate at 1.0 × 104 cells/well and cultured overnight, the cells were treated with 100 μL of DMEM containing various concentrations of DHEA or 0.1% (v/v) ethanol (vehicle) for 24 h at 37 °C. The culture medium was then aspirated, and 100 μL of DMEM containing 10% (v/v) Cell Count Reagent SF were added to each well of the 96-well microplate. The WST-8 formazan dye intensity was then monitored at the wavelength of 450 nm in a microplate reader (SH-8000Lab).
Measurement of intracellular calcium level
Intracellular calcium levels were measured using a Calcium kit Fluo 4 (Dojindo Laboratories, Mashiki, Japan) according to the manufacturer’s instructions. RBL-2H3 cells were seeded at 4.0 × 104 cells/well in a 96-well black culture plate (Sumitomo Bakelite, Tokyo, Japan) and sensitized with anti-DNP IgE (50 ng/mL) at 37 °C overnight. After washing with PBS, the cells were incubated in 100 μL of Fluo 4-AM for 1 h at 37 °C. After washing with PBS, the cells were treated with 100 μL of the recording buffer containing 34, 67, or 135 µM DHEA or 0.1% (v/v) ethanol (vehicle) and incubated at 37 °C for 30 min. The cells were then stimulated with DNP-HSA (50 ng/mL), and the fluorescent intensity was immediately monitored with an excitation wavelength of 485 nm and an emission wavelength of 535 nm using a microplate reader (Infinite 200 PRO, Tecan, Männedorf, Switzerland).
Immunoblot analysis
RBL-2H3 cells were seeded into 35 mm dishes (Corning) at 4.0 × 105 cells/well and sensitized with anti-DNP IgE (50 ng/mL) in DMEM containing 10% FBS at 37 °C overnight. After washing, the cells were treated with 17, 34, 67, or 135 µM DHEA or with 0.1% (v/v) ethanol (vehicle) for 30 min at 37 °C. The cells were then stimulated with DNP-HSA (50 ng/mL) and further incubated for 5 min. After removing the added reagents, cells were immediately lysed and immunoblotting was performed as previously reported39. Blots were developed by ImmunoStar LD (Fujifilm Wako Pure Chemical). Bands were visualized using a ChemiDoc XRS Plus apparatus (Bio-Rad Laboratories, Hercules, CA, USA), and the chemiluminescent intensity was quantified using the Quantity One software (Bio-Rad Laboratories).
Animals
Female BALB/c mice were purchased from Clea Japan (Tokyo, Japan) and housed in a temperature-controlled (24 ± 2 °C) environment under 12 h light/dark cycle. Animals received standard chow (Rodent LabDiet EQ. 5L37; Nutrition International, Brentwood, MO, USA) and water ad libitum.
Synthesis of DHEA
For synthesis of DHEA, DHA was purchased from Nu-Chek Prep (Elysian, MN, USA). 1H-NMR and 13C-NMR spectra were recorded on a JEOL JNM-EX400 spectrometer (JEOL, Japan) using tetramethylsilane (TMS) as an internal standard. High resolution mass spectra were measured by liquid chromatography/electrospray ionization quadrupole time-of-flight mass spectrometry (LC/ESI-Q-Tof-MS) (Acquity UPLC/Xevo QTof MS system; Waters, Milford, MA, USA) in the positive ion mode. Thin-layer chromatography (TLC) was performed on silica gel, and spots were visualized with basic KMnO4.
To a solution of DHA (0.30 g, 0.91 mmol), 4-dimethylaminopyridine (0.13 g, 1.09 mmol), and 2-aminoethanol (0.082 g, 1.09 mmol) in dry dichloromethane (7 mL) was added 1-[3-(dimethylamino)propyl]-3-ethylcarbodiimide hydrochloride (0.21 g, 1.09 mmol) at room temperature. The reaction mixture was stirred overnight at room temperature under nitrogen gas. The product was extracted with ethyl acetate (50 mL × 2). The combined organic solutions were washed with an aqueous solution of 1 N hydrochloric acid (15 mL) and brine (70 mL × 2), dried over magnesium sulfate, and evaporated to dryness. The residue was purified by using silica gel column chromatography eluting ethyl acetate to afford DHEA in 92% yield. 1H-NMR δ (CDCl3): 0.97 (3 H, t, J = 7.2 Hz), 2.07 (2 H, quint, J = 7.2 Hz), 2.27 (2 H, t, J = 7.2 Hz), 2.42 (2 H, q, J = 7.2 Hz), 2.65 (1 H, s), 2.80–2.88 (10 H, m), 3.43 (2 H, q, J = 7.2 Hz), 3.72 (2 H, t, J = 7.2 Hz), 5.25–5.44 (12 H, m), 5.95 (1 H, s). 13C NMR δ (CDCl3): 14.27, 20.53, 23.35, 25.51, 25.60, 36.30, 42.47, 62.56, 126.97, 127.83, 127.97, 128.03, 128.25, 128.30, 128.55, 129.46, 132.03, 173.64. HRMS (ESI) m/z calcd for C24H37NO2 [M + H]+ 372.2903, found [M + H]+ 372.2919. The purity of DHEA was confirmed to be higher than 95% by HPLC analysis.
IgE-mediated PCA in mice
An IgE-dependent PCA experiment was performed as previously reported40 with some modifications. After acclimating to their housing environment for 1 week, 8-week-old female BALB/c mice were randomly divided into 6 groups (7 or 8 mice per group) and orally administered 50, 200, or 1,000 mg/kg of DHEA, 1,000 mg/kg of DHA, 50 mg/kg of fexofenadine hydrochloride41 suspended in 0.5% methyl cellulose (Fujifilm Wako Pure Chemical), or 1,000 mg/kg of water (intact and control groups) once a day for 5 consecutive days (day 0 to day 4) as shown in Fig. 5A. On day 3, all mice were intradermally injected with 10 µL of PBS containing 0.1 μg of anti-DNP IgE into an ear. On day 4, 200 μL of PBS containing 0.2 mg of DNP-HSA and 0.5% (w/v) Evans blue dye were intravenously injected 1 h after oral administration. The mice were euthanized 30 min after intravenous injection, and their ears were collected. The dye in ear tissue after extravasation was then extracted from each ear with 400 μL of formamide at 70 °C overnight, and the absorbance was measured at 620 nm using an Ultrospec 3000 spectrophotometer (Amersham Pharmacia Biotech, Uppsala, Sweden).
A mouse model of Japanese cedar pollinosis
A mouse model of Japanese cedar pollinosis was developed by treating mice with the purified Japanese cedar pollen protein (Cry j1 and Cry j2) as scheduled in Fig. 5B. Following adaptation period for 1 week, 6-week-old female BALB/c mice were randomly divided into 4 groups as follows: intact group, control group, DHEA-administered group, and DHA-administered group (8 mice/group). All mice, except intact group, were intraperitoneally injected with 5 µg of Cry j1 and Cry j2 absorbed on 2 mg of aluminium hydroxide gel on day 0 and intranasally treated with 2 μg of Cry j1 and Cry j2 on day 7, 14, 21, and 28 and with 0.4 μg of Cry j1 and Cry j2 on day 35 to day 39. DHEA-administered and DHA-administered groups were dosed with 1,000 mg/kg of DHEA and of DHA, respectively, for 7 consecutive days from day 35 to day 41, while control and intact groups were orally administered 20 µL of water. On day 40, all mice, including intact group, were challenged by intranasally treating with 0.4 μg of Cry j1 and Cry j2 1 h after oral administration, and the sneezing frequency was subsequently counted for 10 min. On day 41, the blood and spleen were collected 2 h after the final challenge to all mice. Splenocytes were prepared by gently passing the spleen through a cell strainer (BD Falcon, Franklin Lakes, NJ, USA), hemolyzing with a lysis buffer (155 mM NH4Cl, 15 mM NaHCO3, 1 mM ethylenediaminetetraacetic acid, pH 7.3), and washing with PBS. The cells were then suspended in RPMI 1640 medium supplemented with 100 U/mL of penicillin, 100 µg/mL of streptomycin, 10% FBS, and 2 µg/mL of Cry j1 and Cry j2 and seeded into 6-well culture plates at 2.0 × 107 cells/well. After cultivation for 96 h at 37 °C, the concentrations of IgE and cytokines in the culture medium were determined using ELISA kits.
Statistical analysis
Statistical analyses were performed using GraphPad Prism version 7.02 (GraphPad Software, La Jolla, CA, USA). Statistical significance was determined via one-way analysis of variance (ANOVA) with Dunnett’s multiple comparison test as indicated. Values with *P < 0.05, **P < 0.01, or ***P < 0.001 against control were considered statistically significant.
Ethical approval
Protocols of all animal experiments were approved by the Animal Experiment Committee of Ehime University. All animal experiments were carried out in accordance with the Guidelines of Animal Experiments of Ehime University.
References
Nakae, K. & Baba, K. Update on epidemiology of pollinosis in Japan: changes over the last 10 years. Clin Exp Allergy Rev 10, 2–7 (2010).
Nwaru, B. I. et al. The epidemiology of food allergy in Europe: a systematic review and meta‐analysis. Allergy 69, 62–75 (2014).
Galli, S. J. & Tsai, M. IgE and mast cells in allergic disease. Nat Med 18, 693–704 (2012).
Wallace, D. V. et al. The diagnosis and management of rhinitis: an updated practice parameter. J Allergy Clin Immunol 122, S1–S84 (2008).
Clausen, M., Jonasson, K., Keil, T., Beyer, K. & Sigurdardottir, S. T. Fish oil in infancy protects against food allergy in Iceland-results from a birth cohort study. Allergy 73, 1305–1312 (2018).
Miyake, Y. et al. Fish and fat intake and prevalence of allergic rhinitis in Japanese females: the Osaka Maternal and Child Health Study. J Am Coll Nutr 26, 279–287 (2007).
Willemsen, L. E. M. Dietary n-3 long chain polyunsaturated fatty acids in allergy prevention and asthma treatment. Eur J Pharmacol 785, 174–186 (2016).
van den Elsen, L. W. J. et al. n-3 Long-chain PUFA reduce allergy-related mediator release by human mast cells in vitro via inhibition of reactive oxygen species. Br J Nutr 109, 1821–1831 (2013).
Wang, X., Ma, D. W. L., Kang, J. X. & Kulka, M. n-3 Polyunsaturated fatty acids inhibit Fc ε receptor I-mediated mast cell activation. J Nutr Biochem 26, 1580–1588 (2015).
Miyata, J. & Arita, M. Role of omega-3 fatty acids and their metabolites in asthma and allergic diseases. Allergol Int 64, 27–34 (2015).
Kunisawa, J. et al. Dietary ω3 fatty acid exerts anti-allergic effect through the conversion to 17,18-epoxyeicosatetraenoic acid in the gut. Sci Rep 5, 9750 (2015).
Moon, T. C., Befus, A. D. & Kulka, M. Mast cell mediators: their differential release and the secretory pathways involved. Front Immunol 5, 569 (2014).
Galli, S. J., Tsai, M. & Piliponsky, A. M. The development of allergic inflammation. Nature 454, 445–454 (2008).
Maeyama, K., Hohman, R. J., Metzger, H. & Beaven, M. A. Quantitative relationships between aggregation of IgE receptors, generation of intracellular signals, and histamine secretion in rat basophilic leukemia (2H3) cells. Enhanced responses with heavy water. J Biol Chem 261, 2583–2592 (1986).
Schwartz, L. B., Lewis, R. A., Seldin, D. & Austen, K. F. Acid hydrolases and tryptase from secretory granules of dispersed human lung mast cells. J Immunol 126, 1290–1294 (1981).
MacDonald, A. J. et al. IgE-mediated release of rat mast cell protease II, β-hexosaminidase and leukotriene C4 from cultured bone marrow-derived rat mast cells. Immunology 67, 414–418 (1989).
Pearce, F. L. Calcium and mast cell activation. Br J Clin Pharmacol 20, 267S–274S (1985).
Siraganian, R. P., Zhang, J., Suzuki, K. & Sada, K. Protein tyrosine kinase Syk in mast cell signaling. Mol Immunol 38, 1229–1233 (2002).
Metcalfe, D. D., Peavy, R. D. & Gilfillan, A. M. Mechanisms of mast cell signaling in anaphylaxis. J Allergy Clin Immunol 124, 639–646 (2009).
Wang, D. et al. Phospholipase Cγ2 is essential in the functions of B cell and several Fc receptors. Immunity 13, 25–35 (2000).
Han, E. H. et al. Inhibitory effect of Pleurotus eryngii extracts on the activities of allergic mediators in antigen-stimulated mast cells. Food Chem Toxicol 49, 1416–1425 (2011).
Korinek, M. et al. Anti-allergic potential of Typhonium blumei: inhibition of degranulation via suppression of PI3K/PLCγ2 phosphorylation and calcium influx. Phytomedicine 23, 1706–1715 (2016).
Takayama, G., Ohtani, M., Minowa, A., Matsuda, S. & Koyasu, S. Class I PI3K-mediated Akt and ERK signals play a critical role in FcεRI-induced degranulation in mast cells. Int Immunol 25, 215–220 (2013).
Finkelman, F. D. Anaphylaxis: lessons from mouse models. J Allergy Clin Immunol 120, 506–515 (2007).
Kono, R. et al. Biological and epidemiological evidence of anti-allergic effects of traditional Japanese food ume (Prunus mume). Sci Rep 8, 11638 (2018).
Wynn, T. A. Type 2 cytokines: mechanisms and therapeutic strategies. Nat Rev Immunol 15, 271–282 (2015).
Lawrence, M. G., Steinke, J. W. & Borish, L. Cytokine-targeting biologics for allergic diseases. Ann Allergy Asthma Immunol 120, 376–381 (2018).
Brown, M. A. IL-4 production by T cells: you need a little to get a lot. J Immunol 181, 2941–2942 (2008).
Spits, H. et al. Innate lymphoid cells - a proposal for uniform nomenclature. Nat Rev Immunol 13, 145–149 (2013).
Fan, Y. et al. Gallic acid alleviates nasal inflammation via activation of Th1 and inhibition of Th2 and Th17 in a mouse model of allergic rhinitis. Int Immunopharmacol 70, 512–519 (2019).
Bui, T. T., Piao, C. H., Song, C. H. & Chai, O. H. Skullcapflavone II attenuates ovalbumin-induced allergic rhinitis through the blocking of Th2 cytokine production and mast cell histamine release. Int Immunopharmacol 52, 77–84 (2017).
Kianmehr, M. et al. The effect of Zataria multiflora on Th1/Th2 and Th17/T regulatory in a mouse model of allergic asthma. Front Pharmacol 8, 458 (2017).
Sung, Y. Y., Kim, S. H., Kim, D. S., Lee, J. E. & Kim, H. K. Illicium verum extract and trans-anethole attenuate ovalbumin-induced airway inflammation via enhancement of Foxp3+ regulatory T cells and inhibition of Th2 cytokines in mice. Mediators Inflamm 2017, 7506808 (2017).
Hawrylowicz, C. M. Regulatory T cells and IL-10 in allergic inflammation. J Exp Med 202, 1459–1463 (2005).
Mäkelä, M. J. et al. IL-10 is necessary for the expression of airway hyperresponsiveness but not pulmonary inflammation after allergic sensitization. Proc Natl Acad Sci USA 97, 6007–6012 (2000).
Polukort, S. H. et al. IL-10 enhances IgE-mediated mast cell responses and is essential for the development of experimental food allergy in IL-10-deficient mice. J Immunol 196, 4865–4876 (2016).
Takagi, H. et al. A rice-based edible vaccine expressing multiple T cell epitopes induces oral tolerance for inhibition of Th2-mediated IgE responses. Proc Natl Acad Sci USA 102, 17525–17530 (2005).
Watanabe, J., Shinmoto, H. & Tsushida, T. Coumarin and flavone derivatives from estragon and thyme as inhibitors of chemical mediator release from RBL-2H3 cells. Biosci Biotechnol Biochem 69, 1–6 (2005).
Kanda, K. et al. Nobiletin suppresses adipocyte differentiation of 3T3-L1 cells by an insulin and IBMX mixture induction. Biochim Biophys Acta 1820, 461–468 (2012).
Nishi, K. et al. The major whey protein β-lactoglobulin inhibits IgE-mediated degranulation of RBL-2H3 cells and passive cutaneous anaphylaxis in mice. Int Dairy J 39, 89–95 (2014).
Lu, Y. et al. Emodin, a naturally occurring anthraquinone derivative, suppresses IgE-mediated anaphylactic reaction and mast cell activation. Biochem Pharmacol 82, 1700–1708 (2011).
Acknowledgements
We are grateful to Daisuke Nakayama, Makoto Hada, and Sakina Tokuura (Ehime University) for their technical assistance and to Dr. Jeanette E. Stok (University of Queensland) for proof reading of the manuscript. Intracellular Ca2+ monitoring and animal experiments were accomplished at the Division of Genetic Research of the Advanced Research Support Center (ADRES), Ehime University. This work was partially supported by JSPS KAKENHI, Grant-in-Aid for Scientific Research (C), grant number JP17K07792 (to K.N.) and by Ehime University.
Author information
Authors and Affiliations
Contributions
K.N. designed research; K.N., Y.K., I.-H.K., A.N., and H.N. performed experiments; K.N., Y.K., I.-H.K., H.N., and T.S. analyzed data; H.N. and T.S. provided experimental equipment; K.N. and I.-H.K. wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nishi, K., Kanayama, Y., Kim, IH. et al. Docosahexaenoyl ethanolamide mitigates IgE-mediated allergic reactions by inhibiting mast cell degranulation and regulating allergy-related immune cells. Sci Rep 9, 16213 (2019). https://doi.org/10.1038/s41598-019-52317-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-52317-z
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.