Abstract
The gender distribution in intensive care units is consistently found to be around 60% men and 40% women. This might be medically sound. Our main purpose with this study was to investigate if physicians admit men and women to the intensive care unit equally. We sought to answer this question using a blinded randomized survey study. We used an online survey tool, with a hyperlink on European society of intensive care medicine webpage. Responders were randomized to either a critical care case Jane or a critical care case John, otherwise identical. The responders were asked if they would admit Jane/John to an intensive care unit, yes or no. Possible differences in admittance rate on the basis of the gender of the patient were analysed. In addition, we analysed if the gender of the responder affected admittance rate, regardless of the gender of the patient. 70.1% of the responders randomized to the John case opted to admit, vs. 68.3% of the responders randomized to the Jane case, p = 0.341. Regardless the gender of the patient, 70.1% of male responders opted to admit the patient, vs. 69.7% of female responders, p = 0.886. In this blinded randomized multicentre survey study, we could not demonstrate any difference in willingness to admit a patient to ICU, solely based on the gender of the patient. Patient gender as a factor for ICU admittance. A blinded randomized survey.
Similar content being viewed by others
Introduction
In many hospitals resources are sparse. The intensive care unit (ICU) is in a sense at the centre of this problem. Scarcity of ICU beds leads to difficult decisions regarding who to discharge and who to admit1. Guiding principles for the physician state that health care should be provided to all citizens equally. The person with the greatest need of care should be prioritized. It is reasonable to believe that few physicians would argue against these principles. With that in mind, it is somewhat odd that the sex distribution in ICU populations consistently display roughly 60% men and 40% women2,3,4. It might be medically correct, i.e. men need more intensive care, but could there be other explanatory factors for this disparity?
Gender refers to the socially constructed characteristics of men and women, while sex implies biological differences5. Gender bias, i.e. unjustified differences in the treatment of men and women depending on their sex, has been reported numerous times in different medical fields6,7,8,9,10,11, and may also have an impact on referral rate to ICU. Our main objective was to investigate if physicians admit men and women to the intensive care unit equally. We set out to do this by creating a survey with two identical cases, bar the sex of the patient. Responders to the survey were randomized to one of the two cases, but blinded to that. They were then asked if they would admit the patient to their ICU, a simple yes or no question. Any difference in referral rate would be attributable to the only factor distinguishing the cases, namely the sex of the patient.
Methods
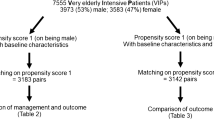
This was a randomized blinded survey study, with responders from 75 countries. It was endorsed by the European society of intensive care medicine (ESICM). The Regional Research Ethics Committee in Stockholm approved the study and all research was performed in accordance with national guidelines and regulations. Answering the survey was voluntary and informed consent was considered obtained when responders answered the survey question.
A pilot study with the same principal design was undertaken by our group in 201512. Two surveys containing eight cases were sent out to physicians working in Sweden. The responders were randomized to one of the two surveys. The only difference between the two surveys was the gender of the patient in each case. In the present study we used only one.
Of the eight cases, choosing the case that in the pilot study was most contentious. The case is presented in an additional file (additional file 1).
We used an online survey tool (SurveyMonkey, SurveyMonkey INC, San Mateo, USA) with a hyperlink on the ESICM webpage. The survey was promoted with the help of ESICMs newsletter and social media channels. Unbeknown to the responders, they were randomized, using A/B Tests (Random Assignment) 50/50 randomization feature from SurveyMonkey, to either a critical care case Jane or a critical care case John, otherwise identical. At the end of the case the responders were asked if they would admit Jane/John to an intensive care unit, yes or no. Possible differences in admittance rate on the basis of the gender of the patient were analysed. In addition, we analysed if the gender of the responder affected admittance rate, regardless of the gender of the patient.
Data analysis was performed using Stata v.14 (Stata®, StataCorp LLC, Texas, USA). Differences in proportions were compared by Chi-square test. All tests were two-sided. A p-value of <0.05 was considered as statistically significant. For the purpose of investigating if the responder’s country of residence had any impact on admittance rate, we performed a Generalized Estimation Equation (GEE) for Logistic regression, clustering on country. The dataset analysed during the current study is available from the corresponding author on reasonable request.
Results
The survey was online between 24th November 2017 until 29th January 2018 and engaged 1,004 case responders from 75 countries spread across all continents. The characteristics of the responders are presented in Table 1 and it shows that the randomization worked. There was no significant difference between John and Jane getting admitted to the ICU: John 70.1% vs. Jane 68.3% p = 0.341. The gender of the respondent did not have an impact on willingness to admit the patient to ICU, regardless of the gender of the patient: male responder 70.1% vs. female responder 69.7% P = 0.886 (Table 2). Furthermore, no difference in admittance rate between male and female patients was detected after having performed a GEE, clustering on country (OR 0.9, 95% CI: 0.7–1.2; p = 0.434).
Discussion
In this blinded randomized multicentre survey study, we could not demonstrate any difference in willingness to admit a patient to ICU, solely based on the gender of the patient. In addition, there was no significant difference between male and female physician responders in admission rate, disregarding the gender of the patient.
This study format has been applied previously. Hamberg et al.7 studied how gender of the patient would impact diagnosis and treatment in a final examination that Swedish physicians in training undertake before becoming fully licensed. Both diagnosis and treatment differed, despite the cases being identical. Their findings suggested that physicians’ stereotyped expectations are involved in creating gender differences in medicine. There are numerous examples of when reality proves them right. Arber et al.8 demonstrated that primary care doctors in the United States and United Kingdom did not ask women and elderly about risk factors for chronic heart disease as often as they asked men. An American study reported that women hospitalized for coronary heart disease underwent fewer diagnostic and therapeutic procedures than men. The authors conclude that it might represent appropriate level of care for both genders, but that it could reflect an underuse for women and overuse for men13. In a more recent study, Johnston et al.6 found that for patients in Canada and Sweden diagnosed with ST-elevation myocardial infarction, women were less likely than men to receive acute reperfusion therapy. Nguyen et al.14 demonstrated that women with acute myocardial infarction were to a less extent referred to angiography but received the same pharmacological treatment and had the same use of coronary revascularization as men. In other fields results are at variance. When investigating stroke care and outcome, one group in Canada found only small differences in use of statins and neuroimaging15. A similar European study however showed that diagnostic methods were significantly less frequently performed in female than male patients16.
In critical care, the results of prior research are also conflicting. In a study of 261,255 consecutive patients admitted to adult ICUs in the United States between 2004 to 2008 it was demonstrated that men received more of mechanical ventilation, emergent surgery, thrombolytic therapy and coronary artery bypass grafting. Men also had a higher readmission rate and longer length of ICU stay. However, women under 50 years of age had a lower ICU mortality than men; above 50 years of age the difference vanished17. In a report including 25,998 patients from 31 intensive care units in Austria no difference in mortality was noted18. After adjustment for age and severity of illness, men had a significantly higher probability of receiving mechanical ventilation, vasoactive medication, renal replacement therapy and a pulmonary artery catheter. Again, this suggests that men are either overusing resources, or women are underusing them. In Sweden, Samuelsson et al.3 came to similar conclusions. With 127,254 consecutive ICU admissions no survival advantage for premenopausal women was noted, but after adjusting for severity of illness and age men used more intensive care resources per admission than women did.
It seems clear that in large intensive care trials, differences in the care given within the ICU can be detected. It is unlikely that this is a caused by explicit gender bias, i.e. that the physician consciously neglects to treat women in the same manner as men, but it could be caused by implicit bias, which by definition is unintentional, or unconscious19,20. Given the results from previous research it is reasonable to assume that part of the discrepancy is caused by physicians stereotyping on gender, especially when working in a highly stressful environment such as the intensive care unit21. Knowing this, and keeping in mind that there is in fact a gender disparity in the ICU population, we posed the question: is the threshold for women to get access to the ICU higher? Are there women in the emergency rooms or in the wards belonging in the ICU, but not given access? We approached this question using a credible case. We had no ambition of judging if the more correct answer to our survey question is to admit or not admit. Our ambition was the opposite, to select an ambiguous case, a case that would typically be admitted by 50% and refused by 50%. We were strictly interested in deducing any difference in admittance rate between a male and female patient. Such difference would only be attributable to the one thing that separated the cases, i.e. the gender of the patient.
The strength of this study is that it tests the physician’s attitude towards admitting patients in a truly blinded randomized scenario. There is presumably no other way to do this. Using only one case, difference in admittance rate between men and women would be difficult to explain with other means than that there exists an implicit gender bias.
There are obvious limitations in this randomized survey. It is a paper case, and not a real live hospital situation. Implicit bias is “unconscious” or unintentional, and could even starkly differ from explicit beliefs20. In a paper case the name and gender of the patient might not be enough to trigger implicit bias in the responder. Further limitations include selection bias, people taking the time to answer surveys might not be the same people that let gender affect their clinical judgement. The response rate is also not clear, which obviously makes generalizability difficult. Moreover, as respondents came from 75 nations, presumably the heterogeneity of their workplaces is large. It was an open survey, and it would be possible for non-professionals to answer it. All respondents have declared their profession. It was possible for respondents to answer multiple times, however unlikely.
Conclusion
In this survey study with 1,004 responders from 75 different countries, there was no difference in admittance rate that could be attributed to the gender of the patient. Furthermore, no difference was noted in admittance rate between male and female responders. These results offer no explanation to the gender discrepancy that is described in previous research18. To further the science in this field it is important to continue to investigate whether men and women get access to and receive the same level of care within the ICU.
Data Availability
The dataset analysed during the current study is available from the corresponding author on reasonable request.
References
Bagshaw, S. M. et al. Association between strained capacity and mortality among patients admitted to intensive care: A path-analysis modeling strategy. J. Crit. Care 43, 81–87, https://doi.org/10.1016/j.jcrc.2017.08.032 (2018).
Fowler, R. A. et al. Sex-and age-based differences in the delivery and outcomes of critical care. CMAJ 177, 1513–1519, https://doi.org/10.1503/cmaj.071112 (2007).
Samuelsson, C., Sjoberg, F., Karlstrom, G., Nolin, T. & Walther, S. M. Gender differences in outcome and use of resources do exist in Swedish intensive care, but to no advantage for women of premenopausal age. Crit. Care 19, 129, https://doi.org/10.1186/s13054-015-0873-1 (2015).
Vincent, J. L. et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA 302, 2323–2329, https://doi.org/10.1001/jama.2009.1754 (2009).
Hamberg, K. Gender bias in medicine. Women’s health (London, England) 4, 237–243, https://doi.org/10.2217/17455057.4.3.237 (2008).
Johnston, N. et al. Do clinical factors explain persistent sex disparities in the use of acute reperfusion therapy in STEMI in Sweden and Canada? Eur Heart J Acute Cardiovasc Care 2, 350–358, https://doi.org/10.1177/2048872613496940 (2013).
Hamberg, K., Risberg, G., Johansson, E. E. & Westman, G. Gender bias in physicians’ management of neck pain: a study of the answers in a Swedish national examination. J. Womens Health Gend. Based Med. 11, 653–666, https://doi.org/10.1089/152460902760360595 (2002).
Arber, S. et al. Influence of patient characteristics on doctors’ questioning and lifestyle advice for coronary heart disease: a UK/US video experiment. Br. J. Gen. Pract. 54, 673–678 (2004).
Baumhakel, M., Muller, U. & Bohm, M. Influence of gender of physicians and patients on guideline-recommended treatment of chronic heart failure in a cross-sectional study. Eur. J. Heart Fail. 11, 299–303, https://doi.org/10.1093/eurjhf/hfn041 (2009).
Ohlsson, A., Lindahl, B., Hanning, M. & Westerling, R. Inequity of access to ACE inhibitors in Swedish heart failure patients: a register-based study. J. Epidemiol. Community Health 70, 97–103, https://doi.org/10.1136/jech-2015-205738 (2016).
Reeves, M. J., Fonarow, G. C., Zhao, X., Smith, E. E. & Schwamm, L. H. Quality of care in women with ischemic stroke in the GWTG program. Stroke 40, 1127–1133, https://doi.org/10.1161/strokeaha.108.543157 (2009).
Larsson, E., Zettersten, E., Jaderling, G., Ohlsson, A. & Bell, M. The influence of gender on ICU admittance. Scand. J. Trauma Resusc. Emerg. Med. 23, 108, https://doi.org/10.1186/s13049-015-0191-2 (2015).
Ayanian, J. Z. & Epstein, A. M. Differences in the use of procedures between women and men hospitalized for coronary heart disease. N. Engl. J. Med. 325, 221–225, https://doi.org/10.1056/nejm199107253250401 (1991).
Nguyen, J. T., Berger, A. K., Duval, S. & Luepker, R. V. Gender disparity in cardiac procedures and medication use for acute myocardial infarction. Am. Heart J. 155, 862–868, https://doi.org/10.1016/j.ahj.2007.11.036 (2008).
Kapral, M. K. et al. Gender differences in stroke care and outcomes in Ontario. Womens Health Issues 21, 171–176, https://doi.org/10.1016/j.whi.2010.10.002 (2011).
Di Carlo, A. et al. Sex differences in the clinical presentation, resource use, and 3-month outcome of acute stroke in Europe: data from a multicenter multinational hospital-based registry. Stroke 34, 1114–1119, https://doi.org/10.1161/01.str.0000068410.07397.d7 (2003).
Mahmood, K., Eldeirawi, K. & Wahidi, M. M. Association of gender with outcomes in critically ill patients. Crit. Care 16, R92, https://doi.org/10.1186/cc11355 (2012).
Valentin, A., Jordan, B., Lang, T., Hiesmayr, M. & Metnitz, P. G. Gender-related differences in intensive care: a multiple-center cohort study of therapeutic interventions and outcome in critically ill patients. Crit. Care Med. 31, 1901–1907, https://doi.org/10.1097/01.ccm.0000069347.78151.50 (2003).
Devine, P. G. Stereotypes and prejudice: their automatic and controlled components. J Personal Soc Psychol. 56(1), 5–18 (1989).
Chapman, E. N., Kaatz, A. & Carnes, M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J. Gen. Intern. Med. 28, 1504–1510, https://doi.org/10.1007/s11606-013-2441-1 (2013).
Croskerry, P. Achieving quality in clinical decision making: cognitive strategies and detection of bias. Acad. Emerg. Med. 9, 1184–1204 (2002).
Acknowledgements
The authors would like to thank Sherihane Bensemmane at ESICM for her valuable support in creating the online survey and promoting it. This study was funded with the help of Stockholms Läns Landsting. Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Contributions
E.Z. analyzed and interpreted the data and was a major contributor in writing the manuscript. G.J. together with E.L. and M.B. created the study protocol. G.J., E.L. and M.B. interpreted the data and had key input in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zettersten, E., Jäderling, G., Larsson, E. et al. The impact of patient sex on intensive care unit admission: a blinded randomized survey. Sci Rep 9, 14222 (2019). https://doi.org/10.1038/s41598-019-50836-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-50836-3
This article is cited by
-
Sex matters: Is it time for a SOFA makeover?
Critical Care (2024)
-
E-contact facilitated by conversational agents reduces interethnic prejudice and anxiety in Afghanistan
Communications Psychology (2024)
-
A cohort study investigating the occurrence of differences in care provided to men and women in an intensive care unit
Scientific Reports (2021)
-
Gender differences in the provision of intensive care: a Bayesian approach
Intensive Care Medicine (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.