Abstract
Extracorporeal life support (ECLS) remains the last option for cardiorespiratory stabilization of severe traumatic injured patients. Currently limited data are available and therefore, the current study assessed the survival rate and outcome of ECLS in a Level I trauma center. Between 2002 and 2016, 18 patients (7 females, 11 males) with an median age of 29.5 IQR 23.5 (range 1–64) years were treated with ECLS due to acute traumatic cardiorespiratory failure. Trauma mechanism, survival rate, ISS, SOFA, GCS, GOS, CPC, time to ECLS, hospital- and ICU stay, surgical interventions, complications and infections were retrospectively assessed. Veno-arterial ECLS was applied in 15 cases (83.3%) and veno-venous ECLS in 3 cases (16.6%). Survivors were significant younger than non-survivors (p = 0.0289) and had a lower ISS (23.5 (IQR 22.75) vs 38.5 (IQR 16.5), p = n.s.). The median time to ECLS cannulation was 2 (IQR 0,25) hours in survivors 2 (IQR 4) in non-survivors. Average GCS was 3 (IQR 9.25) at admission. Six patients (33.3%) survived and had a satisfying neurological outcome with a mean GOS of 5 (IQR 0.25) (p = n.s.). ECLS is a valuable treatment in severe injured patients with traumatic cardiorespiratory failure and improves survival with good neurological outcome. Younger patients and patients with a lower ISS are associated with a higher survival rate. Consideration of earlier cannulation in traumatic cardiorespiratory failure might be beneficial to improve survival.
Similar content being viewed by others
Introduction
Severe trauma in combination with thoracic injuries are accompanied by life-threatening conditions including cardiorespiratory failure1. The main reasons for traumatic cardiac arrest due to blunt (96,1%) or penetrating (3,9%) thoracic trauma are: hypovolaemia (48%), hypoxaemia (13%), tension pneumothorax (13%) and cardiac tamponade (10%)2,3. Advanced life support (ALS) due to acute thoracotomy with cross-clamping of the aorta and open cardiac massage had shown poor results in the past4,5,6. Severe trauma can also cause acute respiratory distress syndrome (ARDS) in up to 10% of the patients7. The common causes for traumatic ARDS mostly occurs in blunt thoracic trauma accompanied by pulmonary contusion, hypovolaemic shock, massive transfusion, flail chest due to reanimation, and an ISS (Injury Severity Score) >258,9. Extracorporeal life support (ECLS) remains the last option for acute cardiorespiratory stabilization in these patients5,7,10,11,12. However, there are only limited data on the veno-arterial or veno-venous ECLS as emergency treatment in traumatic cardiac arrest or hypoxemia5,12,13,14,15,16.
Therefore, the current study aims to report our experience on the ECLS treatment in trauma patients and addresses the following questions: (1) Which extent of injury severity makes the use of ECLS necessary. (2) How long is in average the time between trauma and ECLS-cannulation? (3) How many ECLS related complications occurred? (4) How is the neurological outcome in trauma patients requiring ECLS treatment?
Results
Clinical presentation
Eight patients were admitted to the trauma room awake or minimally sedated, respiratory stable under application of 2–4 liters of using an oxygen mask and i.v. fluid supply. Nine patients were admitted intubated, mechanically ventilated and hemodynamically stable. Out of these patients 3 became hypoxemic accompanied with rapidly decreasing peripheral oxygen saturation of <85% as well a PaCO2 > 115 mmHg/PaO2 < 50 mmHg in the blood gas analysis (BGA). Fourteen patients became hemodynamically instable and required advanced life support. At least one patient arrived in the trauma room intubated and under on going mechanical resuscitation and advanced life support.
More information on clinical presentation in Table 2.
Injury severity & survivors
One third of all patients (n = 6) that required ECLS due to acute cardiorespiratory failure survived. For further analysis, patients were allocated to survivors and non-survivors. The mean follow up was 4.8 ± 2.3 years (range 52–407 weeks). Cannulation for ECLS lead to ROSC (return of spontaneous circulation) in ten patients (55.6%) and was not successful in eight patients (44.4%). However, four patients (22.2%) died within 36 hours- 45 days on Intensity care unit (ICU) due to multi organ failure (MOF) or ICU related complications such as sepsis.
The median ISS at admission was 34.5 (IQR 26.5, range 16–50). Survivors were significantly younger than non-survivors (p = 0.0289) and had a lower ISS (23.5 IQR 22.75 vs 38.5 IQR 16.5, p = n.s.) The median SOFA score was 12 (IQR 4, range 5–15) in all patients and was comparable between survivors and non-survivors (p = n.s.).
ECLS procedure related results
Cannulation for ECLS was performed within 2 (IQR 3, range 0.5–6) hours in median from initial trauma. The median time to ECLS cannulation in survivors was 2 (IQR 0.25) hours compared to 2 (IQR 4) hours in non-survivors (p = n.s.). Earlier cannulation for ECLS (<3 hours) had no influence on overall survival (p = n.s.). The median duration of ECLS was in non-survivors 0.5 (IQR 27, range 0–264) hours and 48 (IQR 54, range 24–96) hours in survivors. The mean ICU stay was 32.7 days (±11.3) days and the average hospital stay until discharge was 50.1 days (±11.4) (Table 3).
Complications & death on ICU following initial ROSC
In one patient primary attempt for cannulation failed on the right/left side and was successfully on the contralateral lower limb.
Two patients out of those with ROSC had a local bleeding at the puncture site. After decannulation revision surgery and suture of the vessel was performed by a vascular surgeon. One patient suffered from a malpositioning of the Y-cannula causing ischemia of the affected leg and requiring fasciotomy after reperfusion.
One patient ECLS was decannulated after 11 days. After initial improving of her general state she died due to MOF and sepsis 45 days following trauma on ICU. The second patient was decannulated in consent with the patient’s family due to poor prognosis after two days and died two days later due to MOF. The third patient died 2 days after ROSC due to intravascular diffuse coagulopathy and MOF (ISS 50). Treatment with ECLS was still ongoing.
The fourth patient was cardiovascular stable, however she sustained a hypoxic cerebral edema and died on the first day on ICU.
Neurological outcome
The median GCS at admission was 3 (IQR 9.25, range 3–15). Mean GOS of the survivors was 5 (IQR 0.25, range 4–5) and the mean CPC was 1 (IQR 0.25, range 1–2) at discharge from hospital respectively. One of the survivors is hemiplegic and another one suffers from sensibility disorder at his right upper and lower limb.
Discussion
ECLS remains the last option in patients when other treatment strategies fail4,5,14,15,17. In the current study one third of the patients survived with good neurological outcome. We found a significant correlation between age and survival in favor of patients of young age. Further, we observed a trend towards better survival in patients with a lower ISS and earlier cannulation.
Due to the literature an overall survival rate of 25–80% after traumatic cardiorespiratory and following ECLS treatment is reported5,14,15,18. The differences of the overall survival rates, might be due different observation periods and adapted treatment protocols within the last years2,5,14,15. Some authors reported in comparable studies a promising initial successful treatment with ECLS in 70–80% of the patients, however the number of survivors decreased to 27% within the follow up5,15. Grubmuller et al.17 reported that a higher ISS in patients with chest trauma is not associated with inferior survival due to modern diagnosis and treatment options. In contrast, our data show that a higher ISS is indeed associated with an increased mortality rate. This finding in in accordance to the data reported by Bonacchi et al. who found that patients with a higher ISS had a higher failure rate of ECLS.
Currently, there are several recommendations for time to ECLS cannualtion in ARDS or acute cardiopulmonary failure12,14,15,19,20. Huh et al. reported an average time of 142 ± 48.2 minutes from initial trauma to veno-arterial ECLS in their patients with traumatic cardiac arrest. They suggested that the high survival of 80% was supported from early cannulation to veno-arterial ECLS5. An European group reported an average time to ECLS from trauma of about 6 hours in patients with successful and failed cannulation for ECLS15. A literature review by Bonnachi et al.14 reveals that a delayed application of ECLS in patients with cardiac impairment or shock might contribute to further tissue hypoperfusion leading to irreversible intravascular diffuse coagulopathy and death. However, the authors strongly recommend heparin-free ECLS in severely injured patients due to impaired blood coagulation14. In contrast it was reported that early cannulation (<24 h) in patients with traumatic ARDS is associated with higher risk for major bleedings or other complications and was associated with a higher mortality8,19. In comparison to the prior reported data, the time to cannulation was in average earlier in the current study5,14,15. Survivors were cannulated earlier compared to non-survivors. This might indicate that earlier cannulation in traumatic cardiorespiratory failure is beneficial to improve survival.
The most common ECLS related complications were local bleeding and malposition of the Y cannula with accompanying ischemia of an extremity. In one patient (ISS 50) intravascular diffuse coagulopathy occurred within 48 hours. Cannulation for ELCS (heparin-free) was performed 3 hours after trauma and thoracotomy. These findings, are comparable to prior reported data14,18. Moreover, ECLS related complications did not effect the overall survival in the current study.
Data on neurological outcome of patients with ECLS for traumatic cardiopulmonary failure is rare12. Huh et al. reported good general outcome and two patients with cognitive or visual impairment after resuscitation and ECLS cannulation5. Kim et al. reported satisfying neurological outcome with an average CPC of 1 (1–2.5) in patients with ECLS following traumatic cardiorespiratory or traumatic ARDS21. In contrast Ryu et al. observed good neurological outcome in 59% and poor in 41% in patients following non-traumatic cardiopulmonary failure. High serum lactic acid levels and prolonged interval from cardiac arrest to ECLS had negative impact on neurological performance at discharge22. In the present study long-term survivors of traumatic cardiac arrest had a satisfying neurological performance at discharge from hospital, which might differ from current literature due to the small sample size12,21.
In summary, there are several limitations of this study. (1) We retrospectively assessed a small patient collective. (2) During the long observation period between 2002 and 2016 treatment protocols were adapted. (3) The heterogeneous patient population with different indications for ECLS (cardiac failure or hypoxemia) might have influence on the results. However, our results showed that ECLS is a valuable treatment in severely injured patients with traumatic cardiorespiratory failure and might improve survival with good neurological outcome. Younger patients had a significantly higher survival rate. Patients with a lower ISS were also associated with a higher survival rate. One third of the patients with ECLS survived in this study. Conversely, refrain form ECLS treatment would be the certain death of these patients since it is the last option. Consideration of earlier cannulation in traumatic cardiorespiratory failure might be beneficial to improve survival.
Methods
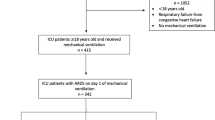
This retrospective study analyzes all patients admitted with an ISS >16 to a Level I trauma center between 2002 and 2016. Inclusion criteria were ECLS in acute trauma treatment within ≤6 hours from injury due to cardiopulmonary failure with shock or acute respiratory insufficiency with severe hypoxemia. The cut off of <6 hours was defined as timespan between accident, rescue time until admission to hospital and advanced life support at the emergency trauma room. In total 853 trauma patients with an ISS >16 were admitted to our department. Eighteen patients (2.1%, 7 females, 11 male) with an average age of 31.6 ± 17.1 (range 1–64) required ECLS for acute cardiorespiratory failure.
Out of this collective 14 patients had a traumatic cardiac arrest, three patients had traumatic hypoxemia and one patient had traumatic cardiac failure and hypoxemia. Veno-arterial cannulation was performed in 15 patients (83.3%) with traumatic cardiac failure. Veno-venous cannulation was necessary in only 3 patients (16.7%) with acute hypoxemia. Nine patients (50%) underwent thoracotomy with cross-clamping of the aorta and open cardiac massage before ECLS cannulation. Detailed information on trauma mechanism, injuries and patient demographics are given in Table 1.
Diagnosis and treatment
For acute emergency trauma room management, a standardized clinical body check, FAST ultrasound scan, computer tomography and extremity radiographs were used. Advanced life support, including vasoactive medications and endotracheal intubation, was performed in accordance with the European Resuscitation Council Guidelines23. Blood gas analysis (BGA) and basic blood samples including clothing parameters, red blood count, renal and liver function were taken within the stabilization phase in the trauma room. Shock was defined as lack of sufficient tissue oxygenation due to decreased circulating blood volume, cardiac function, or systemic vascular resistance.
Followed by drop in blood pressure to less than 60 mmHg resulting that vital organs cannot be perfused sufficiently 24. Hypoxemia was defined as peripheral oxygen saturation <85% or blood gas analysis showed a PaCO2 > 115 mmHg/PaO2 < 50 mmHg.
ECLS cannulation was indicated in the presence of following conditions: thoracic trauma with impaired oxygenation and hypoxemia, imminent or actual traumatic cardiac arrest under ongoing ALS with or without thoracotomy and open cardiac massage without signs of ROSC or improvement of oxygenation. In the presence of one of these conditions, an early cannulation to ECLS was aimed.
The final decision for cannulation was made by the trauma leader. The femoral vessels were used for the veno-arterial cannulation. The cannulation was performed using the percutaneous Seldinger technique with ultrasound guidance or by a small incision to cannulate directly the vessel. In addition, the cannulation was secured by a vascular suture. For the veno-venous-ECLS a femoro-jugular cannulation was performed using an ultrasound guided percutaneous Sedlinger’s technique. Blood clotting was checked in all patients before beginning of ECLS and heparin was used as anticoagulation. Infants requiring veno-venous ECLS, cannulation was performed femoro-jugular.
Depending on blood coagulation and severity of injuries, heparin-free ECLS, delaying heparin administration for up to 48 hours, or an initial bolus of 500IE/h heparin was started soon after transfer to ICU. A therapeutic level of the aPTT of 60–65 seconds was aimed. LDH was checked as a surrogate parameter for hemolysis to reduce heparin dose if necessary.
Outcome parameters
The analysis of ECLS included indication for ECLS, type of ECLS, time to ECLS, duration of ECLS, length of ICU and hospital stay. All ECLS treatment and trauma related complications including bleeding, thrombosis, line infection, vascular injury, cannula dislocation, pneumonia, sepsis or further surgical intervention were recorded. The Injury Severity Score (ISS) and the Glasgow Coma Scale (GCS) were routinely assessed to determine neurological status and impact of trauma at time of admission. The Sequential Organ Failure Assessment-Score (SOFA-Score) was assessed initially after the first blood samples were analyzed to predict likelihood of mortality. For neurological outcome the Glasgow Outcome Scale (GOS) and the Cerebral Performance Category Score (CPC) were done at time of hospital discharge.
Complications
All ECLS, further ALS and trauma related complications such as bleeding, thrombosis, line infection, vascular injuries and cannula dislocation were recorded.
Statistical analysis
Due to small sample size and non normally distributed variables we used the Mann-Whitney-U-Test statistical analysis of quantitative data. Statistical significance was set at α = 0.05. All calculations were performed with Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) and SPSS® (Version 24.0, SPSS Inc., Chicago, IL, USA).
Ethical approval
This article does not contain any interventional studies on human or animal participants performed by any of the authors (Ethics Committee of the Medical University of Vienna 1560/2016). All experimental protocols were approved by Ethics Committee of the Medical University of Vienna. Informed consent was not required by Ethics Committee of the Medical University of Vienna.
References
Soreide, K. et al. Epidemiology and contemporary patterns of trauma deaths: changing place, similar pace, older face. World J Surg 31, 2092–2103 (2007).
Kleber, C., Giesecke, M. T., Lindner, T., Haas, N. P. & Buschmann, C. T. Requirement for a structured algorithm in cardiac arrest following major trauma: epidemiology, management errors, and preventability of traumatic deaths in Berlin. Resuscitation 85, 405–410 (2014).
Horst, K. et al. Thoracic trauma now and then: A 10 year experience from 16,773 severely injured patients. PLoS One 12, e0186712 (2017).
Lockey, D., Crewdson, K. & Davies, G. Traumatic cardiac arrest: who are the survivors? Ann Emerg Med 48, 240–244 (2006).
Huh, U. et al. Is extracorporeal cardiopulmonary resuscitation practical in severe chest trauma? A systematic review in single center of developing country. J Trauma Acute Care Surg 83, 903–907 (2017).
Pust, G. D. & Namias, N. Resuscitative thoracotomy. Int J Surg 33, 202–208 (2016).
Bedeir, K., Seethala, R. & Kelly, E. Extracorporeal life support in trauma: Worth the risks? A systematic review of published series. J Trauma Acute Care Surg 82, 400–406 (2017).
Wu, M. Y. et al. Venovenous extracorporeal life support for posttraumatic respiratory distress syndrome in adults: the risk of major hemorrhages. Scand J Trauma Resusc Emerg Med 22, 56 (2014).
Watkins, T. R. Walking acute respiratory distress syndrome: a target for treatment and prevention*? Crit Care Med 41, 2046–2047 (2013).
Paolone, S. Extracorporeal Membrane Oxygenation (ECMO) for Lung Injury in Severe Acute Respiratory Distress Syndrome (ARDS): Review of the Literature. Clin Nurs Res 26, 747–762 (2017).
Burke, C. R., Crown, A., Chan, T. & McMullan, D. M. Extracorporeal life support is safe in trauma patients. Injury 48, 121–126 (2017).
Mosier, J. M. et al. Extracorporeal membrane oxygenation (ECMO) for critically ill adults in the emergency department: history, current applications, and future directions. Crit Care 19, 431 (2015).
Lin, C. Y., Tsai, F. C., Lee, H. A. & Tseng, Y. H. Extracorporeal membrane oxygenation support in post-traumatic cardiopulmonary failure: A 10-year single institutional experience. Medicine (Baltimore) 96, e6067 (2017).
Bonacchi, M. Extracorporeal life support in polytraumatized patients. Int J Surg 33, 213–217 (2016).
Bonacchi, M. et al. Extracorporeal life support in patients with severe trauma: an advanced treatment strategy for refractory clinical settings. J Thorac Cardiovasc Surg 145, 1617–1626 (2013).
Reynolds, J. C. et al. Prevalence, natural history, and time-dependent outcomes of a multi-center North American cohort of out-of-hospital cardiac arrest extracorporeal CPR candidates. Resuscitation 117, 24–31 (2017).
Grubmuller, M. et al. Severe thoracic trauma - still an independent predictor for death in multiple injured patients? Scand J Trauma Resusc Emerg Med 26, 6 (2018).
Ahmad, S. B. et al. Extracorporeal membrane oxygenation after traumatic injury. J Trauma Acute Care Surg 82, 587–591 (2017).
Menaker, J. et al. Veno-Venous Extracorporeal Membrane Oxygenation (VV ECMO) for Acute Respiratory Failure Following Injury: Outcomes in a High-Volume Adult Trauma Center with a Dedicated Unit for VV ECMO. World J Surg (2018).
Wu, M. Y., Chou, P. L., Wu, T. I. & Lin, P. J. Predictors of hospital mortality in adult trauma patients receiving extracorporeal membrane oxygenation for advanced life support: a retrospective cohort study. Scand J Trauma Resusc Emerg Med 26, 14 (2018).
Kim, H. S. et al. Extracorporeal Membrane Oxygenation Support in Trauma Versus Nontrauma Patients with Noninfectious Acute Respiratory Failure. Artif Organs 41, 431–439 (2017).
Ryu, J. A. et al. Predictors of neurological outcomes after successful extracorporeal cardiopulmonary resuscitation. BMC Anesthesiol 15, 26 (2015).
Perkins, G. D. et al. Cardiac Arrest and Cardiopulmonary Resuscitation Outcome Reports: Update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: A Statement for Healthcare Professionals From a Task Force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Resuscitation 96, 328–340 (2015).
Author information
Authors and Affiliations
Contributions
N.W.L. study design, data acquisition, statistical analysis, writing the manuscript. I.S. data acquisition, study design. V.W. study design, writing the manuscript. M.K. statistical analysis, writing the manuscript. J.J. data acquisition, critical review. S.H. study design, critical review. K.S. study design, statistical analysis, critical review. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lang, N.W., Schwihla, I., Weihs, V. et al. Survival rate and Outcome of extracorporeal life support (ECLS) for treatment of acute cardiorespiratory failure in trauma patients. Sci Rep 9, 12902 (2019). https://doi.org/10.1038/s41598-019-49346-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-49346-z
This article is cited by
-
Veno-arterial-venous extracorporal membrane oxygenation (V-AV ECMO) in a patient in ARDS and cardiac instability after severe polytrauma
Journal of Artificial Organs (2023)
-
ECMO Cannulation for Cardiac and Hemodynamic Support in Trauma
Current Trauma Reports (2023)
-
Outcome of post-traumatic acute respiratory distress syndrome in young patients requiring extracorporeal membrane oxygenation (ECMO)
Scientific Reports (2022)
-
Extracorporeal membrane oxygenation in trauma patients: a systematic review
World Journal of Emergency Surgery (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.