Abstract
Defibrotide is approved for the treatment of sinusoidal obstruction syndrome after allogeneic stem cell transplantation. The exact mode of action of defibrotide is unclear and human in vivo data are scarce. In this randomized, double blind, crossover trial we included 20 healthy volunteers. Four were randomized to receive placebo, while 16 received a 2 ng/kg bodyweight bolus of lipopolysaccharide (LPS). Infusion of 6.25 mg/kg defibrotide or placebo was started one hour before the injection of the LPS bolus. Plasma levels of prothrombin fragments F1 + 2, thrombin-antithrombin complexes, von Willebrand factor, E-selectin, tissue-type plasminogen activator (t-PA), plasminogen activator inhibitor-1 (PAI-1), plasmin-antiplasmin complexes (PAP), tumor necrosis factor-α, interleukin 6, and C-reactive protein were measured. Thromboelastometry was performed. Infusion of defibrotide did not reduce the LPS-induced activation of coagulation, the endothelium or the release of pro-inflammatory cytokines. However, defibrotide increased t-PA antigen levels by 31% (Quartiles: 2–49%, p = 0.026) and PAP concentrations by 13% (−4–41%, p = 0.039), while PAI-1 levels remained unaffected. Moreover, defibrotide reduced C-reactive protein levels by 13% (0–17%, p = 0.002). A transient increase in the clotting time in thromboelastometry and a decrease in F1 + 2 prothrombin fragments suggests modest anticoagulant properties. In conclusion, defibrotide infusion enhanced fibrinolysis and reduced C-reactive protein levels during experimental endotoxemia.
Similar content being viewed by others
Introduction
Defibrotide is a highly complex polydisperse mixture of single-stranded phosphodiester oligodeoxyribonucleotides derived from the controlled depolymerization of porcine intestinal mucosal DNA1. Defibrotide is approved for use in sinusoidal obstruction syndrome, which mainly occurs after high dose chemotherapy in the setting of allogeneic hematopoietic stem cell transplantation2. In the pivotal trial defibrotide improved 100-day survival in patients with sinusoidal obstruction syndrome compared to historical controls from 25% to 38%3. In a randomized, placebo-controlled phase 3 trial defibrotide was effective in the prophylaxis of sinusoidal obstruction syndrome and reduced its incidence from 20% to 12%4. Interestingly, in this trial defibrotide also reduced the development of acute graft versus host disease (GVHD) from 52 to 34%4.
However, the mode of action of defibrotide remains largely unknown and it was reported to induce multiple anti-inflammatory, pro-fibrinolytic and anticoagulant effects5. Defibrotide dose dependently increased t-PA activity and antigen, but reduced PAI-1 and tissue factor expression in vitro6. Furthermore, defibrotide reduced tumor necrosis factor (TNF)-α expression in lipopolysaccharide (LPS)-stimulated dendritic cells and it attenuated the prothrombinase activity, platelet and complement activation in in vitro malaria models7. In healthy volunteers, combined infusion of defibrotide and heparin significantly enhanced the effect of heparin alone and prolonged the activated partial thromboplastin time and increased antithrombin III levels8. Moreover, defibrotide inhibited factor Xa, increased tissue factor pathway inhibitor and decreased tissue factor in healthy volunteers9. However, human in vivo data are scarce and the exact mode of action remains to be elucidated.
The human endotoxemia model is an established model of a tissue-factor driven, self-limiting, acute inflammatory reaction in healthy human volunteers10,11. After a bolus infusion of LPS pro-inflammatory cytokines increase, which is accompanied by an activation of the coagulation system, fibrinolysis and of the endothelium10,12.
The aim of the current trial was to better define the effects of defibrotide in vivo using approved doses in an established model of acute inflammatory response in healthy volunteers10,11. The ascribed profibrinolytic and antithrombotic properties of defibrotide are mostly based on (i) in vitro experiments6,7, in which exceedingly high concentrations of defibrotide have been used compared to those concentrations found after infusion of approved doses13,14, (ii) non-randomized studies in patients undergoing hematopoietic stem cell or bone marrow transplantation15,16, or (iii) studies in healthy volunteers using bolus infusions or much higher doses than currently approved8,9,17. However, currently no such data exist for the approved doses and therefore it is unclear whether these effects are translatable in full extent. Moreover, in contrast to in vitro studies, human in vivo trials allow investigating the effects of defibrotide in the complex interplay of inflammation, coagulation, fibrinolysis and endothelial activation.
We hypothesized that defibrotide diminishes the pathophysiological changes caused by experimental endotoxemia.
Results
Twenty healthy volunteers, two females and 18 males, were included in this trial with a median age of 28.5 years (Quartiles: 24–34 years), a median height of 177 cm (174–183 cm), and a median weight of 72 kg (66–84 kg). One person randomized to the placebo group did not participate in the second period due to unexpected unavailability. In one person in the placebo period infusion of defibrotide was stopped due to the development of an urticarial rash.
Ex vivo study
The addition of defibrotide to whole blood did not affect the results of thromboelastometry. No dose dependent effects were measured with regards to clotting time or maximum lysis (Fig. 1).
Changes in Coagulation Specific Parameters. Left upper panel: Results of ex-vivo spiking study: clotting time was measured in whole blood spiked with various concentrations of defibrotide (0 µg/mL, 25 µg/mL, 50 µg/mL and 100 µg/mL; n = 8); right upper panel: clotting time measured by thromboelastometry during experimental endotoxemia; left lower panel: prothrombin complex F1 + 2 concentrations during experimental endotoxemia; right lower panel: fold-change in thrombin antithrombin complex levels during experimental endotoxemia and in the placebo period (n = 16 for LPS, n = 4 for placebo); Presented are medians ± interquartile range.
Coagulation
As expected, endotoxemia increased in vivo thrombin generation (prothrombin fragments F1 + 2 and TAT complexes), and thromboelastometry confirmed shortened clotting times (Fig. 1).
There was no difference in prothrombin fragments F1 + 2 between both study periods. The ratio of the AUCs for both periods showed a numerical 13% reduction in the defibrotide period (median 0.87, quartiles: 0.75–1.1, p = 0.38, n = 16). Also TAT levels did not differ between both trial periods. The ratio of the AUCs was 0.83 (0.56–0.9, p = 0.15, n = 16) indicating a numerical reduction (Fig. 1). Defibrotide infusion did not prevent the shortening in the clotting time compared to placebo during endotoxemia. This parameter reflects the activation of coagulation. Interestingly, in an exploratory analysis the clotting time increased transiently 1 h after start of the defibrotide infusion by a median of 12% (quartiles: 0–30%, p = 0.003, Fig. 1, n = 16). This is also reflected by a small 8% decrease in F1 + 2 prothrombin fragments from baseline (p = 0.036). Of note, in the placebo period a trend to an increased clotting time could also be observed 1 h vs. 2 h after start of the infusion. Defibrotide did not prevent the LPS-induced decrease in platelet counts, which decreased in both periods by approximately 20% (Supplementary Information, Figure S1).
Maximum concentrations of F1 + 2 correlated with maximum TAT concentrations (r = 0.59, p < 0.001, n = 16).
Fibrinolysis
Infusion of LPS activated the fibrinolytic system in both trial periods (Fig. 2).
Fibrinolysis Specific Parameters. Upper panel: fold-change in plasmin-antiplasmin complex levels (n = 16 for LPS, n = 4 for placebo); middle panel: fold-change in tissue-type plasminogen activator levels (n = 16 for LPS, n = 4 for placebo); lower panel: fold-change in plasminogen activator inhibitor-1 levels during experimental endotoxemia and after placebo (n = 16 for LPS, n = 4 for placebo); Presented are medians ± interquartile range.
PAP complexes were higher in the defibrotide period (p = 0.039). The ratio of the AUC was 1.13 in the defibrotide period (quartiles: 0.96–1.41, Fig. 2, n = 16). This was accompanied by a more pronounced increase of t-PA antigen in the defibrotide period (p = 0.026, n = 16). The median ratio of the AUC of both periods was 1.31 (1.02–1.49, Fig. 2). There was no difference in PAI levels between both study periods with a median ratio of the AUC of 1.03% (0.32–1.58, p = 0.92; Fig. 2, n = 16). Maximum lysis in thrombelastometry did not differ between both study periods.
The relationship between fibrinolysis parameters and inflammation was examined by correlation analysis. Maximum values of ML correlated well with maximum PAP concentrations (r = 0.65, p < 0.001). Likewise ML correlated with maximum levels of tPA concentrations (r = 0.41, p = 0.02) and with maximum TNF-α concentrations (r = 0.52, p = 0.02). Maximum tPA concentrations correlated well with maximum TNF-α concentrations (r = 0.68, p < 0.001). Maximum TNF-α concentrations also correlated with maximum PAP concentrations (r = 0.45, p = 0.009) and with maximum PAI concentrations (r = 0.45, p = 0.011).
Inflammation
There was no difference in pro-inflammatory cytokines IL-6 (median ratio 163% (64–231%), p = 0.33, n = 16) and TNF-α (median ratio 107% (72–138%), p = 0.5; Fig. 3, n = 16). Interestingly, C-reactive protein levels were lower in the defibrotide period (median ratio 0.87, quartiles 0.83–1, p = 0.021, n = 16). Defibrotide did not prevent the LPS-induced increase in total leukocyte counts, which increased approximately two-fold in both study periods (Supplementary information, Figure S1).
Endothelium specific parameters and pro-inflammatory cytokines. Left upper panel: fold-change in E-selectin concentrations during experimental endotoxemia (n = 16 for LPS, n = 4 for placebo); right upper panel: fold-change in von Willebrand factor levels during experimental endotoxemia (n = 16 for LPS, n = 4 for placebo); left lower panel: fold-change TNF-α concentrations during experimental endotoxemia and after infusion of placebo (n = 16 for LPS, n = 4 for placebo); right lower panel: fold-change in interleukin-6 levels during experimental endotoxemia (n = 16 for LPS, n = 4 for placebo); Presented are medians ± interquartile range.
Maximum concentrations of IL-6 correlated well with C-reactive protein levels after 24 h (r = 0.57, p = 0.001) and with maximum TNF-α concentrations (r = 0.63, p < 0.001). Maximum TNF-α concentrations correlated also well with C-reactive protein levels after 24 h (r = 0.61, p < 0.001).
Endothelium
There were no differences in biomarkers of endothelial activation. The ratio of the AUCs was in median 100% (80–116%, p = 0.88, n = 16) for vWF and 100% (77–114%, p = 0.8, n = 16) for E-sel (Fig. 3).
Maximum levels of E-sel correlated with maximum levels of vWF (r = 0.41, p = 0.019). Maximum TNF concentrations correlated with maximum levels of vWF (r = 0.58, p < 0.001) and of E-sel (r = 0.5 p = 0.004).
Adverse events
Thirteen subjects (81%) in the defibrotide/LPS period reported a total of 29 adverse events, while in the placebo/LPS period 15 subjects (94%) reported 33 adverse events. The most frequent adverse events included headache (13 in defibrotide, 11 in placebo period), flu-like symptoms (6 in defibrotide, 6 in placebo period), arthralgia (2 in defibrotide, 7 in placebo period), chills or feeling cold (3 in defibrotide, 6 in placebo period), nausea (2 defibrotide, 1 placebo) with single episodes of impaired concentration (placebo), fatigue (placebo), precollapse (defibrotide), dizziness (defibrotide), vertigo (defibrotide). In the LPS periods subjects regularly received paracetamol for symptom relieve (17 × 500 mg defibrotide, 18 × 500 mg placebo), one subject received 10 mg of metoclopramide for nausea (defibrotide and placebo period), one subject received one tablet of metamizol 500 mg (defibrotide), and one subject received a combination of paracetamol 450 mg and orphenadrincitrate 35 mg for arthralgia. All adverse events were graded mild or moderate. There were no obvious differences in frequency or severity of adverse events between both trial periods.
In the placebo/placebo period one subject reported to have headache and received 500 mg paracetamol as treatment. One subject developed an urticarial rash during the defibrotide infusion in the placebo period, the infusion was stopped and she was treated with 30 mg diphenhydramine and 50 mg aprednisolone after which the rash resolved.
Discussion
This was the first trial that investigated the effects of defibrotide on acute inflammatory responses in healthy human volunteers. The approved dosing regimen (infusion of 6.25 mg/kg bodyweight over 2 h) was used in our trial, which allows translation of the observed effects to the patient situation.
In the first part of the trial we investigated the effects of defibrotide on thromboelastometry ex vivo, while the second part studied the effects of defibrotide on experimental endotoxemia in healthy human volunteers in vivo. Our major findings were that (i) ex vivo defibrotide had no effects on thromboelastometry; (ii) in vivo, defibrotide enhanced fibrinolysis, as indicated by increased PAP complexes and increased levels of tPA, (iii) defibrotide reduced C-reactive protein levels although pro-inflammatory cytokines remained unaffected, (iv) defibrotide did not impact on the activation of coagulation assessed by F1 + 2 prothrombin complexes, TAT complexes, and thromboelastometry, and (v) defibrotide did not reduce endothelial activation.
In our trial defibrotide infusion increased t-PA antigen levels by 30% and PAP complexes by 13% during endotoxemia, while PAI-1 levels remained unchanged. The induction of fibrinolysis is commonly attributed to treatment with defibrotide, although this is based only on few in vivo data. Coccheri et al. demonstrated the profibrinolytic effects of defibrotide in 1988 showing that defibrotide infusion in healthy human volunteers decreased PAI-1 levels by 80%, while t-PA increased almost five-fold. However, similar changes occurred in the placebo period raising concerns about the real effect of defibrotide in this trial. Noteworthy, in that earlier trial a defibrotide dose of approximately 15 mg/kg bodyweight was used, which was >2-fold higher compared to the dose used in our trial18. However, dose dependent effects of defibrotide on plasmin activity, the release of t-PA and reductions in PAI-1 were also shown in vitro19,20,21. In a model of endothelial cells stimulated with LPS defibrotide also induced profibrinolytic changes. However, PAI-1 and t-PA antigen showed marked responses only at defibrotide concentrations exceeding 200 µg/mL6. According to several pharmacokinetic studies, maximum concentrations in humans do not exceed 100 µg/mL using the approved dose of 6.25 mg/kg bodyweight13,14. Thus, although in principal our findings confirm these data, the fibrinolytic response may be more pronounced at higher doses. Clinical data report that PAI-1 antigen levels decrease over time in patients with sinusoidal obstruction syndrome who are successfully treated with defibrotide, whereas in patients who do not respond to treatment, PAI-1 levels remained stable or even increased15,22. No clinical data are available for using higher defibrotide doses in patients who do not respond to treatment according to PAI-1 concentrations, although in vitro data support such an approach.
Fibrinolysis is regulated by TNF-α in human endotoxemia: reduction or inhibition of TNF-α results in a shutdown of fibrinolysis23,24. In our trial TNF-α concentrations were only numerically higher in the defibrotide period compared to placebo. Thus, our findings contrast in vitro studies, in which defibrotide significantly reduced TNF-α concentrations upon LPS stimulation already at concentrations of 30 µg/mL7,25. Furthermore, the observed increases in PAP and t-PA are relatively small with uncertain clinical relevance. However, our trial was performed in healthy volunteers and not in severely ill patients with impaired coagulation parameters and thrombocytopenia26,27. Moreover, treatment of sinusoidal obstruction syndrome is usually performed over weeks and not only for a couple of hours3,15,22. Thus, although the observed effects on fibrinolysis are small, they may be of clinical relevance in patients with sinusoidal obstruction syndrome.
TNF-α is also critically involved in the regulation of E-sel expression and the release of vWF from endothelial cells. Inhibition or reduction of TNF reduced or blunted the endothelial response assessed by vWF or E-sel23,28,29. Defibrotide did not reduce TNF-α concentrations, therefore no differences in vWF or E-sel were found. Furthermore there was no difference in IL-6 levels between both trial periods. C-reactive protein is an inflammatory marker and is largely IL-6 dependent in this model30. Thus, this may reflect decreased IL-6 dependent effects and consequently reduced production of C-reactive protein by liver cells31. However, the observed difference in C-reactive protein levels is small and may also be due to chance.
Defibrotide had no impact on the LPS-induced activation of coagulation assessed by thromboelastometry ex vivo regardless of the dose. In additional in vitro experiments concentrations up to 1000 µg/mL had no direct effects on coagulation (data not shown). Thus, we assume that any effects of defibrotide on the coagulation are not direct, but are dependent on mediators released from the endothelium or other cell types not present in whole blood. Defibrotide had no influence on coagulation parameters during experimental endotoxemia in vivo. The transient prolongation of the clotting time of ~12% may reflect modest actions of defibrotide on coagulation also observed in the ~8% decrease in F1 + 2 concentrations. In patients who receive defibrotide for sinusoidal obstruction syndrome we have performed thromboelastometry to monitor its effects and we have observed more pronounced prolongations in the clotting time by approximately 15 to 35% between trough levels (before next infusion) and at maximum concentrations (at the end of the infusion, data not shown). Noteworthy, in our trial these effects were quite variable with a coefficient of variation of 128% between baseline and after an infusion time of 1 h. In five subjects we measured a >20% prolongation of the clotting time compared to baseline. The LPS induced activation of coagulation completely blunted this observed effect. Interestingly, bolus infusion of 400 mg defibrotide increased tissue factor pathway inhibitor approximately 2-fold, reduced tissue factor by 27% and showed pronounced anti-Xa activity in healthy volunteers, which is comparable to low molecular weight heparins9. However, the tissue-factor driven activation of coagulation during endotoxemia remained unaffected in our trial, which is in contrast to danaparoid32. Thus, we assume only modest effects of defibrotide on coagulation. The present data are insufficient to draw conclusions on dose-dependency of these effects. Thromboelastometry may be of value to monitor the effects of defibrotide, to identify patients at risk of bleeding in case of an overshooting response, but maybe also identify effective doses. However, clinical data are required to support this hypothesis.
Limitations
The endotoxemia model involves healthy human volunteers and a bolus infusion of LPS to induce an acute inflammatory response, which naturally differs from the pathogenesis and the patient characteristics of sinusoidal obstruction syndrome. We have only used the authorized dose of defibrotide, although some of the effects may be dose-dependent and higher doses may be required in some subjects. The sample size was rather small and therefore small effects may not have been detected. We only infused a single dose of defibrotide, which contrasts the continuous treatment of patients for a period of three weeks. The chosen endothelial parameters reflect only part of the activation of endothelial cells during inflammation. We cannot exclude that we have missed effects related to other activation pathways.
In conclusion, defibrotide induced fibrinolysis during experimental endotoxemia and had modest effects on coagulation in vivo.
Methods
The trial was conducted in accordance with the Good Clinical Practice guidelines and the principles set forth in the Declaration of Helsinki. The National Competent Authority (Austrian Agency for Healthy and Food Safety) and the independent ethics committee of the Medical University of Vienna approved the trial before its initiation. The project was conducted at the Department of Clinical Pharmacology at the Medical University of Vienna between April 28th 2017 and February 12th 2018. The trial was ended after the last subject performed the follow-up visit. The trial was registered at the EudraCT database with the public identifier 2016-001375-77 on March 24th 2016 and at Clinicaltrials.gov with the public identifier NCT02876601 on June 27th 2016. Written and oral informed consent to participate in the trial was obtained from all healthy volunteers before any trial-related activity was performed. The protocol is available upon request to the corresponding author.
Population
Eight healthy volunteers ≥18 years of age were included in a pre-study. Exclusion criteria comprised intake of medication deemed relevant by the investigators, acute illnesses and known coagulation disorders.
For the main trial twenty healthy volunteers ≥18 years of age, <90 kg body weight, with normal findings in their medical history and their physical examination, normal baseline laboratory results were included. Exclusion criteria comprised intake of any drugs that may interfere with the trial’s endpoints: acute illnesses with systemic inflammatory reactions, positive HIV or hepatitis tests, known allergies, hypersensitivities or intolerances to any of the used substances, acute or recent bleeding episodes, participation in an endotoxemia trial within six weeks of the trial start, pregnancy or breastfeeding.
Trial Design
The pre-study was an ex-vivo spiking study using increasing concentrations of defibrotide performed in whole blood obtained from healthy human volunteers. Thromboelastometry was performed in these samples to detect any direct effects of defibrotide on this testing system.
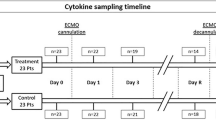
The main trial was a prospective, block-randomized, double blind, placebo-controlled, two-way crossover trial in healthy volunteers. First, healthy volunteers were randomized to receive placebo or LPS. Sixteen patients were randomized to receive LPS, while four patients were randomized to receive placebo. In a second step, all subjects were randomized to receive defibrotide at a dose of 6.25 mg/kg bodyweight or placebo during the first study period. They received the respective other substance in the second study period (Fig. 4).
On the trial days subjects reported to the ward in the morning after an overnight fast. Baseline blood sampling was performed. Thereafter the infusion of 6.25 mg/kg bodyweight defibrotide or placebo was initiated for a period of 2 h. To ensure blinding defibrotide and placebo were filled in colored syringes and colored infusion lines. One hour after the start of the infusion a 2 ng/kg bodyweight LPS bolus was infused via a separate intravenous catheter. Following the infusion of LPS all subjects received a continuous infusion of 100 mL/h 0.9% saline solution until discharge. The timing of the LPS bolus was chosen to ensure relevant defibrotide levels for the critical time of the inflammatory response. To alleviate potential LPS-triggered flu-like symptoms paracetamol (500 mg tablets) was available for all subjects, which reportedly did not impact on endpoints33. Blood samples were drawn by fresh venipunctures at baseline (=pre), 0 h (=time of LPS bolus), 1 h, 2 h, 4 h, 6 h and 24 h thereafter. Subjects received a standardized meal four hours after infusion of LPS and were discharged from the study ward six hours after infusion of LPS. The next morning, 24 h after the LPS bolus another visit was planned. After a washout period of six weeks subjects received the alternative treatment, defibrotide or placebo. All procedures were repeated in the second study period.
Coagulation, fibrinolysis, endothelial activation and inflammatory cytokines
Differential blood counts were performed by the ISO9002 accredited central laboratory of the General Hospital of Vienna using the Sysmex XE-2100/XE-500034. To measure the effects of defibrotide on the activation of coagulation and fibrinolysis in the endotoxemia model we performed commercially available enzyme linked immunoassays (ELISA) to measure levels of prothrombin fragment F1 + 2 (F1 + 2) (Enzygnost® F1 + 2, Siemens), thrombin-antithrombin complexes (TAT) (Enzygnost® TAT, Siemens), plasmin-antiplasmin complexes (PAP) (PAP Elisa, DRG® International Inc., New Jersey, USA), tissue-type plasminogen activator (Technozym t-PA Combi Actibind Elisa kit, Technoclone, Vienna, Austria) levels and plasminogen activator inhibitor-1 (Technozym PAI-1 Actibind Elisa Kit, Technoclone, Vienna, Austria) levels. To investigate the influence of defibrotide on endothelial activation during endotoxemia we measured soluble E-Selectin by ELISA (sE-Selectin/CD62E Quantikine, R&D Systems, Minneapolis, MN, USA) and vWF antigen levels (REAADS VWF:Ag ELISA, Corgenix, Broomfied, CO, USA). Furthermore we measured pro-inflammatory cytokines including tumor necrosis factor (TNF)-α (Human TNF-α Quantikine HS, R&D Systems, Minneapolis, MN, USA) and interleukin-6 (IL-6) (human IL-6 quantikine HS, R&D Systems, Minneapolis, MN, USA). C-reactive protein levels were measured as described previously35. All assays were performed according to the manufacturers’ instructions.
Thrombelastometry
Thromboelastometry (ROTEM; Pentapharm GmbH, Munich, Germany) was performed as previously described36. Thrombelastometry is sensitive to infusion of 2 ng/kg bodyweight LPS36. First, in an ex-vivo spiking study we investigated the concentration-dependent effects of defibrotide on the results of thromboelastometry at the doses 0 µg/mL, 25 µg/mL, 50 µg/mL and 100 µg/mL. The concentrations were chosen based on a previous publication13. The parameters of interest comprised the clotting time and maximum lysis.
Endpoints
The primary endpoint of this trial was the change in plasma levels of prothrombin fragments F1 + 2. Secondary endpoints included TAT complex levels, t-PA levels, PAI-1 levels, soluble E-selectin levels, vWF antigen levels, TNF-α levels, Il-6 levels, C-reactive protein levels and differential blood counts. Furthermore we analyzed parameters of thromboelastometry: the clotting time [sec] and the maximum lysis [%] were analyzed. Safety assessments included vital parameters, documentation of adverse events and intake of concomitant medication.
Randomization and blinding
First healthy volunteers were randomized to receive placebo or LPS. In a second step, they were randomized to receive defibrotide or placebo first. Randomization lists were generated by an independent statistician applying block randomization with block sizes of 8. Individual randomization codes and treatment allocation were concealed until immediately before administration. An unblinded study nurse under supervision of an unblinded physician who had access to treatment allocation codes prepared study drugs. They were not otherwise involved in the conduct of the trial. Participants, investigators and laboratory staff were blinded. Since defibrotide has a yellow color, both study drugs were filled in colored syringes and colored infusion lines were used to make them indistinguishable from each other. Subjects, treating physicians and other study staff who were involved in the study conduct were blinded.
Sample size
For the ex vivo trial a formal sample size calculation was not performed, since no data was available for the effects of defibrotide on thromboelastometry. Therefore, a first analysis was performed after eight subjects in order to re-evaluate the sample size for the main trial based on these results.
The sample size calculation for the main trial was based on the experience with prior trials using anti-coagulants in the human endotoxemia model. Ten to 15 subjects in each group were sufficient to detect significant differences in the primary outcome parameter (F1 + 2 levels) between treatment groups in a parallel-group study37,38,39. There were no data on the expectable effect size of defibrotide in the same model. In a prior LPS trial F1 + 2 levels of approximately 819 ± 173 (Standard deviation) pmol/ml were measured40. This corresponds to an approximate six-fold increase in F1 + 2 levels and was similar in other endotoxemia trials10,12,41. The median intra-individual coefficient of variation was 15% in a recent study, the mean was 25%41. Thus, a sample size of 16 volunteers was deemed sufficient to detect a 25% lower increase in the defibrotide period. The placebo group consisting of four healthy volunteers formed an additional control group, which also allows to assess the effects of defibrotide in healthy volunteers without LPS. However, this analysis is exploratory and no sample size calculation for this group was performed.
Statistical analysis
Demographics and baseline data are presented with descriptive statistics (median and quartiles).
For the analysis of the above-mentioned endpoints area under the curves (AUC) of each period normalized to the baseline (as fold increase) were calculated and compared with the non-parametric Wilcoxon test, for reasons of robustness. For the analysis of clotting time in thromboelastometry ratios compared to baseline, and in a second step deltas (difference between baseline and measuring time point) compared to baseline were calculated. Similar to other parameters, AUCs were calculated and compared. C-reactive protein levels were only measured at baseline and after 24 hours, therefore the 24 hours value was compared by the Wilcoxon test. The ratio of the AUC was calculated for both trial periods to determine effect sizes (AUC defibrotide divided by AUC placebo, medians and quartiles based on the individual ratios). Correlations were calculated by the Spearman Ranks correlation test. Adverse events and concomitant medication were documented and are reported by descriptive statistics. As this trial was of an exploratory nature, no corrections for multiple testing applied. As no corrections for multiple testing were done, even though exploratory, inferences of significance should not be made, rather p-values should be noted as nominal. Missing data were not imputed, outliers were removed from analysis.
References
Palmer, K. J. & Goa, K. L. Defibrotide. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic use in vascular disorders. Drugs 45, 259–294, https://doi.org/10.2165/00003495-199345020-00007 (1993).
Kernan, N. A. et al. Final results from a defibrotide treatment-IND study for patients with hepatic veno-occlusive disease/sinusoidal obstruction syndrome. Br J Haematol 181, 816–827, https://doi.org/10.1111/bjh.15267 (2018).
Richardson, P. G. et al. Phase 3 trial of defibrotide for the treatment of severe veno-occlusive disease and multi-organ failure. Blood 127, 1656–1665, https://doi.org/10.1182/blood-2015-10-676924 (2016).
Corbacioglu, S. et al. Defibrotide for prophylaxis of hepatic veno-occlusive disease in paediatric haemopoietic stem-cell transplantation: an open-label, phase 3, randomised controlled trial. Lancet 379, 1301–1309, https://doi.org/10.1016/S0140-6736(11)61938-7 (2012).
Keating, G. M. Defibrotide: a review of its use in severe hepatic veno-occlusive disease following haematopoietic stem cell transplantation. Clin Drug Investig 34, 895–904, https://doi.org/10.1007/s40261-014-0242-x (2014).
Falanga, A., Vignoli, A., Marchetti, M. & Barbui, T. Defibrotide reduces procoagulant activity and increases fibrinolytic properties of endothelial cells. Leukemia 17, 1636–1642, https://doi.org/10.1038/sj.leu.2403004 (2003).
Francischetti, I. M. et al. Defibrotide interferes with several steps of the coagulation-inflammation cycle and exhibits therapeutic potential to treat severe malaria. Arterioscler Thromb Vasc Biol 32, 786–798, https://doi.org/10.1161/ATVBAHA.111.240291 (2012).
Pogliani, E. M., Salvatore, M., Fowst, C., Girardello, R. & Marelli, C. Effects of a defibrotide-heparin combination on some measures of haemostasis in healthy volunteers. J Int Med Res 17, 36–40, https://doi.org/10.1177/030006058901700105 (1989).
Cella, G. et al. Tissue factor pathway inhibitor release induced by defibrotide and heparins. Clin Appl Thromb Hemost 7, 225–228 (2001).
Mayr, F. B. & Jilma, B. Coagulation interventions in experimental human endotoxemia. Transl Res 148, 263–271, https://doi.org/10.1016/j.trsl.2006.08.002 (2006).
Suffredini, A. F. & Noveck, R. J. Human endotoxin administration as an experimental model in drug development. Clin Pharmacol Ther 96, 418–422, https://doi.org/10.1038/clpt.2014.146 (2014).
Schoergenhofer, C. et al. Inhibition of Protease-Activated Receptor (PAR1) Reduces Activation of the Endothelium, Coagulation, Fibrinolysis and Inflammation during Human Endotoxemia. Thromb Haemost 118, 1176–1184, https://doi.org/10.1055/s-0038-1655767 (2018).
Tocchetti, P. et al. Pharmacokinetic profile of defibrotide in patients with renal impairment. Drug Des Devel Ther 10, 2631–2641, https://doi.org/10.2147/DDDT.S112181 (2016).
Umemura, K. et al. Pharmacokinetics and Safety of Defibrotide in Healthy Japanese Subjects. Clin Pharmacol Drug Dev 5, 548–551, https://doi.org/10.1002/cpdd.262 (2016).
Kaleelrahman, M. et al. Role of plasminogen activator inhibitor-1 (PAI-1) levels in the diagnosis of BMT-associated hepatic veno-occlusive disease and monitoring of subsequent therapy with defibrotide (DF). Hematology 8, 91–95, https://doi.org/10.1080/1024533031000084231 (2003).
Richardson, P. G. et al. Multi-institutional use of defibrotide in 88 patients after stem cell transplantation with severe veno-occlusive disease and multisystem organ failure: response without significant toxicity in a high-risk population and factors predictive of outcome. Blood 100, 4337–4343, https://doi.org/10.1182/blood-2002-04-1216 (2002).
Tobu, M. et al. Comparative tissue factor pathway inhibitor release potential of heparins. Clin Appl Thromb Hemost 11, 37–47 (2005).
Coccheri, S., Biagi, G., Legnani, C., Bianchini, B. & Grauso, F. Acute effects of defibrotide, an experimental antithrombotic agent, on fibrinolysis and blood prostanoids in man. Eur J Clin Pharmacol 35, 151–156 (1988).
Echart, C. L. et al. The fibrinolytic mechanism of defibrotide: effect of defibrotide on plasmin activity. Blood Coagul Fibrinolysis 20, 627–634, https://doi.org/10.1097/MBC.0b013e32832da1e3 (2009).
Echart, C. L. et al. Defibrotide blunts the prothrombotic effect of thalidomide on endothelial cells. Clin Appl Thromb Hemost 18, 79–86, https://doi.org/10.1177/1076029611412367 (2012).
Klocking, H. P. Acute t-PA release by defibrotide. Thromb Res 66, 779–785 (1992).
Richardson, P. G. et al. Defibrotide for the treatment of severe hepatic veno-occlusive disease and multiorgan failure after stem cell transplantation: a multicenter, randomized, dose-finding trial. Biol Blood Marrow Transplant 16, 1005–1017, https://doi.org/10.1016/j.bbmt.2010.02.009 (2010).
Schoergenhofer, C. et al. Colistin dampens fibrinolysis and endothelial activation during endotoxaemia. A randomised, double blind trial. Thromb Haemost 117, 1714–1721, https://doi.org/10.1160/TH17-03-0196 (2017).
van der Poll, T. et al. Effect of a recombinant dimeric tumor necrosis factor receptor on inflammatory responses to intravenous endotoxin in normal humans. Blood 89, 3727–3734 (1997).
Pescador, R., Capuzzi, L., Mantovani, M., Fulgenzi, A. & Ferrero, M. E. Defibrotide: properties and clinical use of an old/new drug. Vascul Pharmacol 59, 1–10, https://doi.org/10.1016/j.vph.2013.05.001 (2013).
Nurnberger, W., Kruck, H., Mauz-Korholz, C., Burdach, S. & Gobel, U. Humoral coagulation and early complications after allogeneic bone marrow transplantation. Klin Padiatr 209, 209–215, https://doi.org/10.1055/s-2008-1043952 (1997).
Jevtic, D. et al. Coagulation disturbances in paediatric patients with hepatic veno-occlusive disease after stem cells transplantation. Srp Arh Celok Lek 138(Suppl 1), 33–38 (2010).
DeLa Cadena, R. A. et al. Recombinant tumor necrosis factor receptor p75 fusion protein (TNFR:Fc) alters endotoxin-induced activation of the kinin, fibrinolytic, and coagulation systems in normal humans. Thromb Haemost 80, 114–118 (1998).
Suffredini, A. F. et al. Effects of recombinant dimeric TNF receptor on human inflammatory responses following intravenous endotoxin administration. J Immunol 155, 5038–5045 (1995).
Marsik, C. et al. The C-reactive protein (+)1444C/T alteration modulates the inflammation and coagulation response in human endotoxemia. Clin Chem 52, 1952–1957, https://doi.org/10.1373/clinchem.2006.069823 (2006).
Wang, T. M., Hsieh, S. C., Chen, J. W. & Chiang, A. N. Docosahexaenoic acid and eicosapentaenoic acid reduce C-reactive protein expression and STAT3 activation in IL-6-treated HepG2 cells. Mol Cell Biochem. 377, 97–106, https://doi.org/10.1007/s11010-013-1574-1 (2013).
Hollenstein, U. M. et al. Effect of factor X inhibition on coagulation activation and cytokine induction in human systemic inflammation. J Infect Dis 186, 1270–1276, https://doi.org/10.1086/344646 (2002).
Pernerstorfer, T. et al. Acetaminophen has greater antipyretic efficacy than aspirin in endotoxemia: a randomized, double-blind, placebo-controlled trial. Clin Pharmacol Ther 66, 51–57, https://doi.org/10.1016/S0009-9236(99)70053-6 (1999).
Ruzicka, K., Veitl, M., Thalhammer-Scherrer, R. & Schwarzinger, I. The new hematology analyzer Sysmex XE-2100: performance evaluation of a novel white blood cell differential technology. Arch Pathol Lab Med 125, 391–396, https://doi.org/10.1043/0003-9985(2001)125<0391:TNHASX>2.0.CO;2 (2001).
Derhaschnig, U. et al. Effect of interleukin-6 blockade on tissue factor-induced coagulation in human endotoxemia. Crit Care Med 32, 1136–1140 (2004).
Spiel, A. O., Mayr, F. B., Firbas, C., Quehenberger, P. & Jilma, B. Validation of rotation thrombelastography in a model of systemic activation of fibrinolysis and coagulation in humans. Journal of thrombosis and haemostasis: JTH 4, 411–416, https://doi.org/10.1111/j.1538-7836.2006.01715.x (2006).
Pernerstorfer, T. et al. Heparin blunts endotoxin-induced coagulation activation. Circulation 100, 2485–2490 (1999).
Pernerstorfer, T. et al. Lepirudin blunts endotoxin-induced coagulation activation. Blood 95, 1729–1734 (2000).
Derhaschnig, U. et al. Recombinant human activated protein C (rhAPC; drotrecogin alfa [activated]) has minimal effect on markers of coagulation, fibrinolysis, and inflammation in acute human endotoxemia. Blood 102, 2093–2098, https://doi.org/10.1182/blood-2003-02-0416 (2003).
Mayr, F. B. et al. Racial differences in endotoxin-induced tissue factor-triggered coagulation. J Thromb Haemost 7, 634–640, https://doi.org/10.1111/j.1538-7836.2009.03307.x (2009).
Schoergenhofer, C. et al. Potent irreversible P2Y12 inhibition does not reduce LPS induced coagulation activation in a randomized, double-blind, placebo-controlled trial. Clin Sci (Lond), https://doi.org/10.1042/CS20150591 (2015).
Acknowledgements
This trial was funded by an investigator initiated research grant by JAZZ Pharmaceuticals and by the Austrian Science Funds (FWF SFB054-P04). The authors would like to thank Sabine Schranz, Christa Drucker and Karin Petroczi for their invaluable help throughout the whole project.
Author information
Authors and Affiliations
Contributions
C.S. and B.J. designed the trial. C.S., N.B., G.G., U.D., C.F., K.K., M.S., P.W., W.R. and B.J. were involved in the conduct of the trial, data interpretation and analysis. C.S. and B.J. drafted the manuscript. C.S., N.B., G.G., U.D., C.F., K.K., M.S., P.W., W.R. and B.J. critically revised the manuscript and approved it for publication.
Corresponding author
Ethics declarations
Competing Interests
C.S. received honoraria and investigator initiated research grants from Jazz Pharmaceuticals. Otherwise the authors report no conflicts of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schoergenhofer, C., Buchtele, N., Gelbenegger, G. et al. Defibrotide enhances fibrinolysis in human endotoxemia – a randomized, double blind, crossover trial in healthy volunteers. Sci Rep 9, 11136 (2019). https://doi.org/10.1038/s41598-019-47630-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-47630-6
This article is cited by
-
Advances in the diagnosis and treatment of disseminated intravascular coagulation in haematological malignancies
International Journal of Hematology (2021)
-
The aptamer BT200 effectively inhibits von Willebrand factor (VWF) dependent platelet function after stimulated VWF release by desmopressin or endotoxin
Scientific Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.