Abstract
Airway collapse can occur when the forces of inhalation overpower the strength of the nasal lining flap. The authors established an animal model of the reconstructed nasal airway, and examined mechanical properties of tissue composites based on various materials. Twenty-three Sprague-Dawley rats were divided into three experimental groups: control (n = 5), irradiated homologous costal cartilage (IHCC, n = 10), and expanded polytetrafluoroethylene (ePTFE, n = 8). Two dorsal skin flaps represented nasal lining and skin envelope. No framework, an IHCC or ePTFE rim graft was used as framework. At three weeks, changes in the cross-sectional area of the lining flap were measured when negative pressure was applied. En-bloc specimens containing the graft and soft tissue were examined for histological change and tissue ingrowth. Reduction of cross-sectional area with simulated inhalation was 87.74% in the control group, 82.76% (IHCC), and 67.29% (ePTFE). Cross-sectional reduction was significantly less in ePTFE group than control group (p = 0.004) and IHCC group (p = 0.001). The difference was not significant in the control and IHCC groups. There was histologic evidence of tissue ingrowth in the ePTFE group. This novel animal model of nasal airway reconstruction supports the use and potential benefit of using ePTFE for prevention of airway collapse.
Similar content being viewed by others
Introduction
The nose is quite difficult to reconstruct with satisfactory results because of its complex topography and robust structural integrity1. Full thickness defects of the nose either after skin cancer extirpation, congenital deformity, trauma, infection, or burn injury, require three components to be replaced in reconstruction: skin, framework, and nasal lining. To achieve this, soft tissue must sandwich a framework to create form and a patent airway1,2,3,4,5,6,7,8. However, the pliable skin of the forearm, a common donor to replace soft tissue1,2,3,4,5, is prone to collapse. With inhalation, negative pressure in the airway can overcome the support of the cartilage framework and tissue, and resulted in the collapse of airway, which may lead to airway obstruction or difficulty of breathing in our clinical observation (Video 1). To treat this, we rely on nasal stents to avoid flap collapse and stenosis1,2,4. Although cartilage remains the gold standard in nasal reconstruction, alloplast support may confer better strength and airway protection. In this study, irradiated homologous costal cartilage (IHCC) was compared to expanded polytetrafluoroethylene (ePTFE, Gore-Tex) as a framework medium.
Because ePTFE is biocompatible, surrounding tissue is expected to grow into its microporous structure, and to create a bond between the lining flap and ePTFE9,10,11,12,13,14. The authors hypothesize that ePTFE is superior to cartilage for prevention of flap collapse. If the results suggest improved mechanical properties, this would support a paradigm shift in human nasal reconstruction favoring alloplast materials.
Results
There were seven rats that died or suffered flap demise that were excluded. 23 rats previously divided into experimental and control groups were included. These rats survived during the experiment and there was no partial or total flap necrosis, wound dehiscence, hematoma, cellulitis or graft extrusion.
There was a cross-sectional area reduction 87.74 ± 9.83% in control group after suction was applied to the airway. Reduction was 82.76 ± 5.34% in the IHCC group, and 67.29 ± 9.68% in the ePTFE group (Fig. 1). The ePTFE group showed significantly less reduction compared to the control group (p = 0.004) and IHCC group (p = 0.001). There was no difference in cross-sectional area reduction after negative pressure between the control and IHCC groups (p = 0.219).
Histologic evaluation demonstrated connective tissue ingrowth with abundant infiltration and deposition of fibroblasts and collagen in the ePTFE group. This was neither seen in the control nor the IHCC group (Fig. 2).
Discussion
The most important aspect of nasal reconstruction is effective reproduction of each component: skin, framework, and lining5. In complex nasal defect reconstruction, it may be necessary to transfer free tissue when the local tissue is not available or enough1,2,3,4,5,6,7,8. The radial forearm flap is favored for its thin and pliable soft tissue, and provides lining without obstructing the nasal airway1,2,3,4,5. At Chang Gung Memorial Hospital, the ulnar forearm flap is sometimes preferred for superior donor site cosmesis compared to radial forearm flap4. The literature is supportive of both options1,2,3,4,5,6,7,8, but there is rare mention of late airway collapse due to inadequate framework support. Furthermore, no animal models or clinical reports objectively address airway obstruction after nasal reconstruction15,16,17,18,19,20,21. To our knowledge, the animal model demonstrated is the first to simulate a hollow cylinder and the layer components of the wall to mimic the structure of human nasal airway and the dynamic changes that occur during inhalation. We compared different materials for construct stability and prevention of airway collapse.
The framework is crucial for restoring aesthetics and function after nasal reconstruction by fortifying the construct and maximizing airflow1. Lateral alar structural grafts are designed to prevent alar retraction and external valve collapse during inspiration. Cartilage is typically harvested from the nasal septum, auricular concha or rib1,2,4. Autologous materials are preferred, but are not immune to absorption and warping. Donor site morbidity, increased operative time and insufficient donor material are important considerations11,22,23,24. Cadaveric homograft cartilage may be used and displays similar characteristics as autologous tissue22,23,24,25,26, but the rate of absorption is greater than with autogenous tissue2,23. Despite a successful framework reconstruction using cartilage, it is possible for the framework to collapse during inhalation. Autologous rib cartilage may not be sufficiently strong to support the airway in the long term. This may be attributable to its histologic character or to inadequate soft tissue ingrowth into the cartilage.
ePTFE, marketed as Gore-Tex (W.L. Gore Associates, Inc., Phoenix, AZ), was developed by Gore in 1969, has a 20 year track record of biocompatibility and favorable results9,10,11,12,13,14,27. The material demonstrates low tissue reactivity, confers stability, does not resorb, and is chemically inert. For these reasons, it is popular in rhinoplasty surgery9,10. ePTFE has a microstructure of interconnected nodes and fibrils that create pores with diameters from 10 to 40 μm9. Morphologic and histologic changes in surrounding tissues have been reported using a Gore-Tex implant in animal models9. When connective tissue ingrowth occurs, deposition of collagen in the intermodal spaces occurs9,10,11,12,13,14. The complications in rhinoplasty using Gore-tex ranged from 1.9% to 10%, compared to silicone implants which ranged from 2 to 7% and autologous costal cartilage which ranged from 0 to 39.5%9,27,28,29.
Histologic results from this study corroborate findings from previous reports9,10,11,12,13,14. Connective tissue was incorporated into ePTFE, which is likely responsible for its bond to surrounding tissues, and for the support and stability of the lining flap. These findings support the idea that ePTFE may be superior to autograft and allograft in preventing flap airway collapse.
The authors used IHCC instead of murine rib cartilage to better simulate autologous human rib cartilage in nasal reconstruction. Autologous rib cartilage is the most common donor for framework reconstruction. There are larger, more evenly distributed, and uniform chrondrocytes, collagen, and proteoglycans in autologous costal cartilage compared to IHCC23, but there is preservation of lacunar morphology in IHCC25. The authors believe IHCC is the best substitute for autogenous rib cartilage compared to other materials24,25,26. It is readily available and murine rib cartilage is too small to simulate human nasal reconstruction. Not to mention, there is technical difficulty and increased operative time involved with murine rib harvest30,31.
Alloplasts such as porous polyethylene (PPE, Medpor®) are widely available for clinical applications. The authors chose ePTFE for this study for its well-known tissue ingrowth characteristics and softer consistency compared to PPE. In future study, the authors intend to create more elaborate airway models in larger animals that allow for autograft rib cartilage to be used, and to study other alloplasts.
Limitation
We assumed complete viability of the tubed flap in all animals. Subclinical construct breakdown would influence the outcome of the experiment. Although we standardized the dissection plane as harvesting the flap above the muscle layer for all rats, the tissue thickness was hardly to be unified. To optimize the health of the constructs, animals were studied no later than three weeks post-experiment and a protective device was placed to prevent flap destruction. Long term changes, including framework resorption and collagen replacement were not studied.
The negative pressure of 60–70 mmHg is much higher than the 150 Pa (~1 mmHg) transmural pressure that causes nasal valve collapse in human patients with nasal airway obstruction. The authors would have preferred to quantify the threshold pressure for flap collapse between the three groups, but this model did not allow for this because of a uniform vacuum pressure. Besides, drawing the airway perimeter manually and selecting the cross-sectional area manually on the Image J software were also a limitation in quantifying the reduction in lumen cross-sectional area. Moreover, this paper did not account for the different mechanical properties of ePTFE and IHCC. Still, this study supports that ePTFE rim grafts are more resilient than cartilage in a rat model. Based on these findings, additional study in human clinical trials may be warranted.
Methods
Animal Model and Study Design
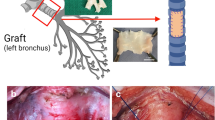
This study was performed at Chang Gung Memorial Hospital with approval from the Institutional Animal Care and Use Committee (approval number: 2014122209). All experiments were performed in accordance with relevant guidelines and regulations. Thirty Sprague-Dawley rats weighing 300–500 g were included initially. However, three rats died due to hypothermia and four rats died due to intolerance of multiple flaps harvested on the back simultaneously. Therefore, we improved the heat preservation system and modified the experiment design into harvesting one flap at one rat at a time. The remained twenty-three rats were randomly divided into three groups: a control group (n = 5) where no framework was placed, an IHCC group (Costal cartilage; LifeNet Health, Virginia Beach, VA) (n = 10), and ePTFE group (Gore-Tex, Implantech ePTFE sheeting, Implantech Associates, Inc., Ventura, CA) (n = 8). Every rat was anesthetized with isoflurane, dorsal hair was shaven and the skin was sterilized with povidone-iodine solution. A random-pattern fasciocutaneous flap measuring 4 cm x 3 cm was elevated. The donor site was closed primarily. The flap was divided longitudinally to create two flaps, each measuring 4 cm x 1.5 cm in size, one for the lining flap and the other skin cover (Fig. 3, upper). The lining flap was rolled and sutured to the flap base with the raw surface facing outwards. A 20-French silicone stent was placed to protect the simulated airway. (Fig. 3). For rats assigned to the control group, the skin cover flap was opposed to the lining flap without framework, and sutured with 5–0 chromic sutures (Fig. 3, left; Fig. 4). In the other groups, ePTFE and IHCC rim grafts measuring 3 cm long x 1 cm wide x 2 mm thick were inserted between the inner lining flap and outer skin flap (Fig. 3, middle and right). The interface was closed to prevent graft exposure. After implantation, IV antibiotics (cefazolin sodium, 15 mg/kg) and analgesics (ketoprofen, 6.25 mg/kg) were injected subcutaneously. For three days, antibiotic was administered daily to prevent infection. To control for inevitable behavior such as hindquarter rubbing and rolling in contamination, and to prevent self-destruction of the tubed flap14, a plastic cup fixed with several stiches was placed as a shield (Fig. 5).
(Upper) A random fasciocutaneous flap was elevated. The flap was divided in half, to establish a lining and skin coverage. (Left, middle, right) In the control group, no framework was placed. In the experimental groups, ePTFE (Gortex) and IHCC were inserted between the lining and skin cover flaps as a framework. The tube structure was established to imitate the airway in nasal reconstruction.
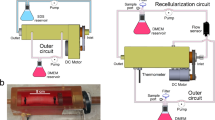
Evaluation of flap collapse
Three weeks after flap elevation, rats were anesthetized and silicone tubes were removed. A surgical suction unit providing negative pressure suction system with continuous negative pressure of 60–70 mmHg was connected to one end of the tubed flap while the opposite side was sealed with a glass slide (Fig. 6a). This model was designed to simulate the effect of negative pressure in the airway while breathing. We marked the outline of the tubed “airway” on the glass side before and after negative pressure was applied, and documented the change of the cross-sectional area of the tubed “airway” (Fig. 6b, Video 2). Cross-sectional area was measured using Image J software (version 1.50i 26 March 2016). The function of polygon selections was used for manually selecting the area of the cross-sectional area on the photos of glass slide. Then the analyze function was utilized for measuring the area which was chosen. Each measurement was performed three times and the average was used for analysis (Supplementary Fig. 1). The degree of airway collapse was calculated as a percentage of the original cross-sectional area before the application of negative pressure.
(a) The negative pressure suction system with continuous negative pressure was connected to one side of the tubing flap while the opposite side was sealed by a glass slide to create a vacuum. (b) The cross-sectional area of tube before and after simulated inhalation in three groups was documented. (upper: control group, middle: IHCC group, lower: ePTFE group).
Histological Evaluation
Rats were then sacrificed using a carbon dioxide chamber. Cross-sections of the composite flap were sectioned for hematoxylin and eosin (H&E) stain to evaluate histological change and tissue ingrowth.
Statistical Analysis
Comparison of airway collapse between the groups was analyzed using the Mann-Whitney U test. Data were analyzed using SPSS for Windows, Version 20.0 (SPSS, Inc., Chicago, IL), and values of p < 0.05 were considered statistically significant.
(Informed consent has been obtained to publish all the identifying information/images (Video 1) in an online open-access publication.)
Conclusions
This is the first animal model to simulate nasal airway reconstruction. ePTFE reinforcement is more effective in reducing cross sectional area when a vacuum is applied than irradiated cartilage.
Data Availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Taghinia, A. H. & Pribaz, J. J. Complex nasal reconstruction. Plast Reconstr Surg. 121(2), 15e–27e (2008).
Winslow, C. P. et al. Total nasal reconstruction: utility of the free radial forearm fascial flap. Arch Facial Plast Surg. 5(2), 159–163 (2003).
Walton, R. L., Burget, G. C. & Beahm, E. K. Microsurgical reconstruction of the nasal lining. Plast Reconstr Surg. 115, 1813–1829 (2005).
Hsiao, Y. C. et al. The Folded Ulnar Forearm Flap for Nasal Reconstruction. Plast Reconstr Surg. 137(2), 630–635 (2016).
Antunes, M. B. & Chalian, A. A. Microvascular reconstruction of nasal defects. Facial Plast Surg Clin North Am. 19(1), 157–162 (2011).
Burget, G. C., Walton, R. L. Optimal use of microvascular free flaps, cartilage grafts, and a paramedian forehead flap foro aesthetic reconstruction of the nose and adjacent facial units. Plast Reconstr Surg. 120, 1171–1207; discussion 1208–1116 (2007).
Menick, F. J. A new modified method for nasal lining: the Menick technique for folded lining. J Surg Oncol. 94, 509–514 (2006).
Menick, F. J. & Salibian, A. Microvascular repair of heminasal, subtotal, and total nasal defects with a folded radial forearm flap and a full-thickness forehead flap. Plast Reconstr Surg. 127, 637–651 (2011).
Kim, J. H. et al. Histologic changes in transplanted expanded polytetrafluoroethylene in an animal model. Laryngoscope. 122(1), 17–22 (2012).
Jang, T. Y. et al. Histologic study of Gore-Tex removed after rhinoplasty. Laryngoscope. 119(4), 620–627 (2009).
Batniji, R. K. et al. Tissue response to expanded polytetrafluoroethylene and silicone implants in a rabbit model. Arch Facial Plast Surg. 4(2), 111–113 (2002).
Kim, J. H. et al. Comparative study of morphological and histological changes between differently structured expanded polytetrafluoroethylene implants in an animal model. Am J Rhinol Allergy. 27(3), 162–167 (2013).
Greene, D., Pruitt, L. & Maas, C. S. Biomechanical effects of e-PTFE implant structure on soft tissue implantation stability: a study in the porcine model. Laryngoscope. 107(7), 957–962 (1997).
Maas, C. S. et al. Evaluation of expanded polytetrafluoroethylene as a soft-tissue filling substance: an analysis of design-related implant behavior using the porcine skin model. Plast Reconstr Surg. 101(5), 1307–1314 (1998).
Palesy, T. et al. Airflow and patient-perceived improvement following rhinoplastic correction of external nasal valve dysfunction. JAMA Facial Plast Surg. 17(2), 131–136 (2015).
Poirrier, A. L. et al. External nasal valve collapse: validation of novel outcome measurement tool. Rhinology. 52, 127–132 (2014).
Thulesius, H. L., Cervin, A. & Jessen, M. The importance of side difference in nasal obstruction and rhinomanometry: a retrospective correlation of symptoms and rhinomanometry in 1000 patients. Clin Otolaryngol. 37, 17–22 (2012).
Vogt, K. et al. 4-Phase-Rhinomanometry (4PR)–basics and practice 2010. Rhinol Suppl. 1–50 (2010).
Wong, E. H. & Eccles, R. Comparison of classic and 4-phase rhinomanometry methods, is there any difference? Rhinology. 52, 360–365 (2014).
Eren, S. B. et al. Objective and subjective evaluation of operation success in patients with nasal septal deviation based on septum type. Am J Rhinol Allergy. 28, e158–162 (2014).
Omranifard, M. et al. Comparison of the Effects of Spreader Graft and Overlapping Lateral Crural Technique on Rhinoplasty by Rhinomanometry. World J Plast Surg. 2, 99–103 (2013).
Lefkovits, G. Irradiated homologous costal cartilage for augmentation rhinoplasty. Ann Plast Surg. 25(4), 317–327 (1990).
Wee, J. H. et al. Autologous vs Irradiated Homologous Costal Cartilage as Graft Material in Rhinoplasty. JAMA Facial Plast Surg. 19(3), 183–188 (2017).
Kridel, R. W. et al. Long-term use and follow-up of irradiated homologous costal cartilage grafts in the nose. Arch Facial Plast Surg. 11(6), 378–394 (2009).
Suh, M. K. et al. A 2-year follow-up of irradiated homologous costal cartilage used as a septal extension graft for the correction of contracted nose in Asians. Ann Plast Surg. 71(1), 45–49 (2013).
Babin, R. W. et al. Survival of implanted irradiated cartilage. Otolaryngol Head Neck Surg. 90(1), 75–80 (1982).
Joo, Y. H. & Jang, Y. J. Comparison of the Surgical Outcomes of Dorsal Augmentation Using Expanded Polytetrafluoroethylene or Autologous Costal Cartilage. JAMA Facial Plast Surg. 18(5), 327–332 (2016).
Peled, Z. M., Warren, A. G., Johnston, P. & Yaremchuk, M. J. The use of alloplastic materials in rhinoplasty surgery: a metaanalysis. Plast Reconstr Surg 121(3), 85e–92e (2008).
Hong, J. P., Yoon, J. Y. & Choi, J. W. Are polytetrafluoroethylene(Gore-Tex) implants an alternative material for nasal dorsal augmentation in Asians? J Craniofac Surg 21(6), 1750–1754 (2010).
Tripuraneni, N. et al. A surgical procedure for resecting the mouse rib: a model for large-scale long bone repair. J Vis Exp. 95, 52375 (2015).
Srour, M. K. et al. Natural large-scale regeneration of rib cartilage in a mouse model. J Bone Miner Res. 30(2), 297–308 (2015).
Acknowledgements
This study was funded and supported by Ministry of Science and Technology (MOST 104-2314-B-182A-106 (NMRPG3E0361)). The authors thank Miss Ingrid Kuo from the Center for Big Data Analytics and Statistics at Chang Gung Memorial Hospital for illustration of Figs 3 and 5.
Author information
Authors and Affiliations
Contributions
Hsiao Y.C. conceived and designed the experiment. Yen C.I. conducted the experiment and wrote the manuscript. Chen H.C. and Yang S.Y. analyzed and interpreted data. Chang S.Y. and Yang J.Y. prepared the figures and photos. Zelken J.A., Chang C.S. and Chuang S.S. revised the manuscript. All authors reviewed drafts of the paper.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yen, CI., Zelken, J.A., Chang, CS. et al. Preventing nasal airway collapse with irradiated homologous costal cartilage versus expanded polytetrafluoroethylene: a novel animal model for nasal airway reconstruction. Sci Rep 9, 6670 (2019). https://doi.org/10.1038/s41598-019-42947-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-42947-8
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.