Abstract
We examined the temporal changes in obesity and sleep habits and their relationship in a prospective cohort of healthy Chinese adolescents. We collected data on anthropometric and questionnaire-measured sleep parameters in 2007–2008. 516 participants returned for examinations in 2013–2015. General obesity was defined as body mass index (BMI) ≥age- and sex-specific 95th percentile or ≥25 kg/m2 for participants aged <18 or ≥18 years, respectively. Central obesity was defined as waist circumference (WC) ≥ age- and sex-specific 90th percentile or using adult cut-offs. After a mean follow-up of 6.2 ± 0.5 years, the mean BMI increased from 18.5 ± 3.1 to 20.9 ± 3.4 kg/m2. The corresponding WC were 63.7 ± 8.9 and 69.8 ± 9.7 cm. General obesity rate increased from 8.3% (95% confidence interval [CI] 6.1–11.1) to 11.3% (8.7–14.4; p = 0.034). Central obesity rate decreased from 16.9% (13.7–20.4) to 13.5% (10.6–16.8; p = 0.034). During follow-up, more participants reported short sleep (<7 hours/day during weekday: 20.5% [17.1–24.2] vs. 15.3% [12.3–18.8]; p = 0.033) and bedtime after midnight (60.5% [56.2–64.8] vs. 16.2% [13.1–19.7]; p < 0.001) than baseline. The relative risk of overweight/obesity in participants with short sleep and late bedtime was 1.30 (0.48–3.47) and 1.46 (0.70–3.05), respectively. Despite rising rates of unhealthy sleep habits and general obesity, their associations were not significant at 6-year of follow-up.
Similar content being viewed by others
Introduction
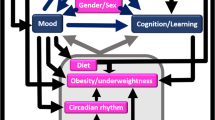
Obesity arises as a result of a complex interplay between genetic and environmental factors including diet, physical exercise and sleep behaviour1,2,3. Technology (such as prolonged television viewing and video games) and lifestyle changes contribute to the global epidemic of obesity and sleep problems4,5,6. Although a recent systematic review of 12 studies reported a decreasing trend of mean sleep duration from the 1960s until 2000s in a few Asian and European populations7, there is a dearth of data exploring temporal changes in sleep duration in children and adolescents.
In a large-scale survey conducted in mainland China involving 145,078 children from 46 kindergartens, the prevalence of obesity (defined as body mass index [BMI] z-score >2 standard deviation [SD]) in those aged 5–6 years had risen from 8.8% in 2006 to 10.1% in 2010, followed by a plateau period until 20148. By contrast, published data about the temporal changes in the rates of overweight and obesity among children in Hong Kong are lacking. Based on data from the Student Health Centre (SHC) of the Hong Kong’s Department of Health9,10, despite a progressive increase in obesity rate (defined as weight > median weight for height × 120%) since 1995, this survey had a few limitations including a lack of definition of overweight and potential overestimation of the obesity rate11. Apart from inattention to health check-ups due to competing priorities among school-going children, assessment at the SHC was available by appointment on a voluntary basis without any prior reminder. This might have caused selection bias as only very motivated parents or their children would return for assessment at SHC. Given a lack of prospective data on obesity and sleep habits in Hong Kong adolescents, we examined their temporal changes and relationship using a territory-wide population-based cohort established in 2007–2008, who returned for follow-ups in 2013–2015.
Results
The baseline characteristics of the present study cohort (n = 516) are shown in Table 1. The baseline characteristics of those who did and did not participate in the follow-up study were comparable, except for a slightly lower proportion of males in the follow-up subsample. The changes in sleep duration and patterns and cardiometabolic risk factors are shown in Table 2. At baseline, 7.3% (95% confidence interval [CI] 5.2–9.9) of the cohort had a sleep duration of <6.5 hours per day during weekdays. After a mean ± SD follow-up of 6.2 ± 0.5 years, there was a trend of an increased proportion of participants with sleep duration <6.5 hours per day during weekdays [10.7% (CI 8.2–13.7)], although there was no statistically significant difference when compared to baseline (p = 0.105). By contrast, 15.3% (CI 12.3–18.8) of the cohort had short sleep using a higher cut-off of <7 hours per day, increasing significantly to 20.5% (CI 17.1–24.2) during follow-up (p = 0.033). When using weekly average values, 2.0% (CI 1.0–3.6) of the cohort had sleep duration <6.5 hours per day, rising to more than double to 5.1% (CI 3.4–7.4) during follow-up (p = 0.016). With a higher cut-off of <7 hours, 6.3% (CI 4.4–8.8) had short sleep, increasing to 11.0% (CI 8.4–14.1) during follow-up (p = 0.01). Moreover, only 16.2% (CI 13.1–19.7) of the cohort had weekly average bedtime later than midnight at baseline, but this increased by 3.7 times to 60.5% (CI 56.2–64.8; p < 0.001) during follow-up.
In terms of cardiometabolic risk factors, 20.3% (CI 17.0–24.1) were either overweight or obese using a BMI ≥ age- and sex-specific 85th percentile, rising to 23.4% (CI 19.7–27.3) during follow-up (p < 0.001). For general obesity (BMI ≥ age- and sex-specific 95th percentile), the proportion increased from 8.3% (CI 6.1–11.1) to 11.3% (CI 8.7–14.4) (p = 0.034). Opposite to general obesity which was measured by BMI, there was a significant reduction of central obesity (WC ≥ age- and sex-specific 90th percentile) from 16.9% (CI 13.7–20.4) at baseline to 13.5% (CI 10.6–16.8) during follow-up (p = 0.034). For high triglyceride, low HDL-cholesterol, high blood pressure, high fasting plasma glucose or metabolic syndrome, there was no significant temporal change in the proportion of participants affected (all p > 0.05).
We examined the relationship between short sleep and late bedtime on the risk of developing obesity amongst normal weight adolescents at baseline (n = 411) (Table 3). Compared to adolescents with weekly average sleep duration ≥7 hours, those with <7 hours of sleep did not have a significant increase in risk of developing either overweight or obesity during follow-up, even after adjusting for age and sex (unadjusted relative risk [RR]: 1.40 [CI 0.54–3.67] and adjusted RR: 1.30 [CI 0.48–3.47]). Similarly, there was no significant increase in risk of obesity alone (unadjusted RR: 1.18 [CI 0.29–4.76] and adjusted RR: 1.27 [CI 0.29–5.50]). Comparisons were made between adolescents with weekly average bedtime after midnight to those with weekly average bedtime before midnight for overweight or obesity, but no significant increase in risk was observed (unadjusted RR: 1.48 [CI 0.76–2.88] and adjusted RR: 1.46 [0.70–3.05]). Again, for obesity alone, the risk was not statistically significant (unadjusted RR: 0.91 [CI 0.32–2.56] and adjusted RR: 0.93 [CI 0.30–2.87]).
Discussion
From this prospective cohort study in Hong Kong Chinese adolescents, we reported a significant increase in general obesity rate from 8.3% to 11.3%, but a decrease in central obesity rate from 16.9% to 13.5%. We also reported an increased proportion of adolescents reporting short sleep duration (defined as <7 hours per day during weekdays) from 15.3% to 20.5% and late bedtime after midnight from 16.2% to 60.5%. Despite the similar rising trends, the associations between unhealthy sleep habits and obesity were not statistically significant at 6-year of follow-up.
Globally, a total of 107.7 million children aged <20 years were obese in 20154. Of note, the prevalence of overweight and obesity during adolescence and young adulthood has doubled in the last three decades, with its rate of increase greater than adult obesity in most countries4. This is an important problem that needs tackling because childhood obesity is a strong predictor for cardiometabolic diseases in subsequent years of life12,13,14. Apart from slow progress in health policy targeting food environments and health systems reforms (such as personal healthcare access and quality)15, other environmental risk factors such as abnormal sleep duration and patterns may contribute to the obesity epidemic6. In this regard, a meta-analysis of randomized controlled trials showed that short sleep could possibly increase food intake and body weight, whilst sleep improvement interventions were associated with weight loss in children and adult populations16. Another meta-analysis of 17 observational studies found that children with short sleep duration had 58–92% higher odds for overweight or obesity than those with longer sleep duration17. Although an updated systematic review of 15 studies found a significant negative relationship between sleep duration and obesity risk18, the majority of included studies were cross-sectional in design and therefore, a causal relationship could not be established.
By using a prospective cohort with a mean follow-up of six years, we observed an increased rate of general obesity but not for central obesity, along with an increased proportion of adolescents with abnormal sleep habits (either short sleep or late bedtime after midnight). In adults, abnormal sleep habits contribute to an excess risk of obesity, driven by alterations in eating behaviour, satiety hormones (reduced leptin to ghrelin ratio), autonomic nervous systems and hypothalamic-pituitary-adrenal axis6. During puberty, the pathogenesis of obesity is even more complex with additional influences from sex steroids and sex steroids-stimulated growth hormone (GH) release19. Compared to boys, several studies reported that girls were more likely to have subcutaneous fat than visceral fat accumulation especially during late puberty or early adulthood20,21. This could be attributable to an increase in oestradiol levels, as well as site- and sex-specific distributions of receptors and the enzymatic activity of sex steroids within the fat depots19,22,23. Hence, the presence of a high proportion of girls (~62%) in our cohort could possibly explain the increasing rate of general obesity but not central obesity. In addition, high testosterone (which was then aromatized to oestradiol) and sex steroids-induced GH levels in boys were shown to upregulate GH/catecholamines-sensitive beta-adrenergic receptors and inhibit lipoprotein lipase activity in adipocytes, which enhanced lipolysis and the redistribution of visceral adipose tissue to subcutaneous depots during puberty19,23. Chronic short sleep was also associated with prolonged exposure to increased GH levels as sequelae of a biphasic nocturnal GH pulse6. Of note, existing evidence on the temporal onset of sex differences in fat distribution has been inconsistent, perhaps due to variations in ethnicity, methods of anthropometric measurements, the timing of puberty and hormonal status20,24,25. Taken together, these findings favoured an increasing BMI amongst adolescents with short sleep duration.
Although the age- and sex-adjusted relative risks of overweight and/or obesity were all greater than unity for short sleep duration, no statistical significance was reached. This may be due to the relatively small sample size and short duration of follow-up of our cohort which limits the statistical power of the present analysis to elucidate the relationships between sleep habits and obesity. In a prospective cohort study involving 597 pre-pubertal children conducted in Canada, after three to eight years of follow-up, there was also no significant association between sleep duration (cross-sectional assessment during the age of 1–3 years) and BMI26. On the other hand, a meta-analysis of three prospective observational studies with longer than one-year follow-up found that short sleep duration was associated with a 30% higher risk of overweight or obesity in adolescents27. In a large prospective cohort study involving >23,000 students aged 7–18 years from mainland China, short sleep was significantly associated with the development of obesity at a later stage28. Apart from nearly half of the cohort were children aged 7–12 years, more than one-third of these children and adolescents reported short sleep (defined as <7 hours per day), which was higher than the present study (15.3–20.5%)28. Taken together, the prevalence of short sleep or late bedtime, the magnitude of short sleep duration and the potential confounding elements of sleep compensation and sleep quality, might all play roles in modulating the development of obesity amongst children and adolescents. More prospective studies that address these factors will provide additional insights into this increasingly important relationship.
To our knowledge, this was the first prospective study which examined the relationship between abnormal sleep habits and risk of obesity in Hong Kong Chinese adolescents. We performed a longitudinal assessment of sleep patterns which helped to reduce recall bias. We also excluded adolescents with a known history of endocrine disorders, growth problem or obstructive sleep apnoea.
Several limitations should be acknowledged. First, given the sexual dimorphism in fat distribution, a larger cohort would allow differentiation of association by gender. However, due to limited funding and resources, only about one-quarter of the original cohort had a prospective follow-up. Second, apart from the adjustment of age and sex in the association analysis, we were not able to consider the confounding effects of other lifestyle, behavioural and socio-economic factors due to limitations in the data source. Third, there was a lack of objective assessment of pubertal timing and stages, albeit our cohort was likely to be in the early- to middle pubertal stage as the mean age of pubertal onset ranged from 9.4 to 11.7 years in Hong Kong children29. Fourth, additional hormonal assessment including sex steroids, IGF-1 and hormones modulating satiety such as leptin and ghrelin, may further explain the differences in obesity rates with abnormal sleep habits. Fifth, although we did not use either magnetic resonance imaging or dual-energy X-ray absorptiometry for the assessment of fat distribution, waist circumference has been recognized as a reliable, cost-effective and commonly adopted field technique for determining central obesity30. Last, we used a sleep-reported sleep questionnaire and did not capture information about sleep quality. Although objective sleep measurements such as actigraphy and polysomnography are the gold standards for assessing sleep duration, patterns and quality, these are labour intensive and not practically feasible for large-scale screening. Nevertheless, our prior work had indicated the reliability of the locally-validated sleep questionnaire with good correlation with actigraphy3,31.
While both rates of general obesity and unhealthy sleep habits increased in Hong Kong adolescents, their associations were not significant after six years of follow-up. Nevertheless, our observation that more than half of the present cohort reported late bedtime after midnight is alarming, calling for public health attention. Larger prospective studies allowing subgroup analyses for gender differences and categorization according to age groups and pubertal stages are needed to validate these observations, as well as to elucidate the effects of poor sleep quality and their interactions with other environmental, molecular and genetic factors, in order to facilitate obesity prevention in the youth populations.
Methods
Study populations
The present study was based on an established cohort of 2053 Hong Kong Chinese school children and adolescents aged 6–20 years who were surveyed in 2007–20083. Using available funding support and resources, we randomly selected 580 subjects from the original cohort for a prospective follow-up between 2013 and 2015. Among them, 516 subjects (89%) agreed to participate in the follow-up study. The remaining 64 subjects (11%) either declined to participate or were not contactable due to a change to the contact number or home address. At baseline and during follow-up, after an overnight fast of 8–10 hours, all participants had comprehensive clinical and biochemical assessment including anthropometric measurements and blood tests (plasma glucose, lipid profile, complete blood count, renal and liver function tests).
Sleep habits were assessed using a validated questionnaire (Supplementary Notes S1 and S2)31, which showed a good agreement with actigraphy-measured sleep duration with an intraclass correlation coefficient of 0.723. Short sleep duration was defined as <6.5 hours per day derived from our prior work3,31 or <7 hours per day as recommended by National Sleep Foundation32. We estimated the weekly average sleep duration using a weighted average: (5 × weekdays sleep duration + 2 × weekend sleep duration)/7. We used a similar equation for estimating the weekly average bedtime. General obesity was defined as body mass index (BMI) ≥ age- and sex-specific 95th percentile or ≥25 kg/m2 for participants aged < 18 or ≥18 years, respectively33,34,35. Central obesity was defined as ≥ age- and sex-specific 90th percentile of WC or adult cut-offs36,37. The BMI and WC cut-off values used in the present study were based on local population-based age- and sex-specific percentiles35,37. We defined metabolic syndrome using the International Diabetes Federation criteria, namely the presence of central obesity plus at least two of the following criteria: triglyceride ≥1.7 mmol/L, high-density lipoprotein cholesterol (HDL-cholesterol) <1.03 mmol/L, blood pressure ≥130/85 mmHg, fasting plasma glucose ≥5.6 mmol/L (adult criteria were adopted for adolescents aged 16 years or older)38. This study was approved by the Chinese University of Hong Kong-New Territories East Cluster Clinical Research Ethics Committee. Written informed consents were obtained from either a parent or a legal guardian. All methods were performed in accordance with the relevant guidelines and regulations.
Laboratory assays
Fasting plasma glucose (hexokinase method) and lipid profile including total cholesterol (enzymatic method), triglyceride (enzymatic method without glycerol blanking) and HDL-cholesterol, direct method using PEG-modified enzymes and dextran sulfate) were measured on a Roche Modular Analytics system (Roche Diagnostics GmbH, Mannheim, Germany) using standard reagent kits supplied by the manufacturer. All laboratory assays were performed using standard methods by the Department of Chemical Pathology at the Prince of Wales Hospital.
Statistical analysis
Data were presented using appropriate descriptive statistics. Normality of continuous variables was assessed on the basis of their skewness statistics and normal probability plots. Triglyceride and urinary albumin:creatinine ratio (ACR) were logarithmically-transformed before entering them into the inferential analysis. We presented the prevalence of unhealthy sleep habits, obesity and other cardiometabolic risk factors in percentages with 95% CI and compared their values at baseline and during follow-up using McNemar’s test. We used paired t-test to assess the changes in participants’ demographic, anthropometric and biochemical characteristics at baseline and during follow-up. After excluding 105 adolescents with either overweight or obesity at baseline, we used log-binomial regression model to assess the RR of developing overweight or obesity during follow-up in normal weight adolescents with either short sleep duration (defined as <6.5 hours or <7 hours per day) or bedtime later than midnight at baseline. All statistical analyses were performed using SAS (SAS Institute, Cary, NC, release 9.3). A two-sided p-value < 0.05 was considered significant.
Data Availability
Data will be made available upon reasonable request.
References
Kong, A. P., Chan, R. S., Nelson, E. A. & Chan, J. C. Role of low-glycemic index diet in management of childhood obesity. Obes Rev. 12, 492–498 (2011).
Kong, A. P. et al. Association between physical activity and cardiovascular risk in Chinese youth independent of age and pubertal stage. BMC Public Health. 10, 303 (2010).
Kong, A. P. et al. Associations of sleep duration with obesity and serum lipid profile in children and adolescents. Sleep Med. 12, 659–665 (2011).
Afshin, A. et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med. 377, 13–27 (2017).
Ward, Z. J. et al. Simulation of Growth Trajectories of Childhood Obesity into Adulthood. N Engl J Med. 377, 2145–2153 (2017).
Ding, C., Lim, L. L., Xu, L. & Kong, A. P. Sleep and Obesity. Journal of Obesity & Metabolic Syndrome. 27, 4–24 (2018).
Bin, Y. S., Marshall, N. S. & Glozier, N. Secular trends in adult sleep duration: a systematic review. Sleep Med Rev. 16, 223–230 (2012).
Xiao, Y. et al. Trends in the Prevalence of Overweight and Obesity among Chinese Preschool Children from 2006 to 2014. PLoS One. 10, e0134466 (2015).
Leung, S. S. F., Lau, J. T. F., Tse, L. Y. & Oppenheimer, S. J. Weight-for-age and weight-for height references for Hong Kong children from birth to 18 years. J Paediatr Child Health. 32, 103–109 (1996).
Wang, J. J., Gao, Y. & Lau, P. W. C. Prevalence of overweight in Hong Kong Chinese children: Its associations with family, early-life development and behaviors-related factors. J Exerc Sci Fit. 15, 89–95 (2017).
Ko, G. T. et al. The problem of obesity among adolescents in Hong Kong: a comparison using various diagnostic criteria. BMC Pediatr. 8, 10 (2008).
Sinaiko, A. R., Donahue, R. P., Jacobs, D. R. Jr. & Prineas, R. J. Relation of weight and rate of increase in weight during childhood and adolescence to body size, blood pressure, fasting insulin, and lipids in young adults. The Minneapolis Children’s Blood Pressure Study. Circulation. 99, 1471–1476 (1999).
World Health Organization. Consideration of the evidence on childhood obesity for the Commission on Ending Childhood Obesity: report of the ad hoc working group on science and evidence for ending childhood obesity. (Geneva, Switzerland, 2016).
Bjerregaard, L. G. et al. Change in Overweight from Childhood to Early Adulthood and Risk of Type 2 Diabetes. N Engl J Med. 378, 1302–1312 (2018).
Fullman, N. et al. Measuring performance on the Healthcare Access and Quality Index for 195 countries and territories and selected subnational locations: a systematic analysis from the Global Burden of Disease Study 2016. Lancet 391, 2236–2271 (2018).
Capers, P. L., Fobian, A. D., Kaiser, K. A., Borah, R. & Allison, B. D. A Systemic Review and Meta-Analysis of Randomized Controlled Trials of the Impact of Sleep Duration on Adiposity and Components of Energy Balance. Obes Rev. 16, 771–782 (2015).
Xiaoli, C., Beydoun, M. A. & Youfa, W. Is Sleep Duration Associated With Childhood Obesity? A Systematic Review and Meta‐analysis. Obesity (Silver Spring). 16, 265–274 (2008).
Fobian, A. D., Elliott, L. & Louie, T. A Systematic Review of Sleep, Hypertension, and Cardiovascular Risk in Children and Adolescents. Curr Hypertens Rep. 20, 42, https://doi.org/10.1007/s11906-018-0841-7 (2018).
Roemmich, J. N. & Rogol, A. D. Hormonal changes during puberty and their relationship to fat distribution. Am J Hum Biol. 11, 209–224 (1999).
Taylor, R. W., Grant, A. M., Williams, S. M. & Goulding, A. Sex differences in regional body fat distribution from pre- to postpuberty. Obesity (Silver Spring). 18, 1410–1416 (2010).
Hammer, L. D. et al. Impact of pubertal development on body fat distribution among white, Hispanic, and Asian female adolescents. J Pediatr. 118, 975–980 (1991).
Anderson, L. A., McTernan, P. G., Barnett, A. H. & Kumar, S. The effects of androgens and estrogens on preadipocyte proliferation in human adipose tissue: influence of gender and site. J Clin Endocrinol Metab. 86, 5045–5051 (2001).
Veldhuis, J. D. et al. Endocrine control of body composition in infancy, childhood, and puberty. Endocr Rev. 26, 114–146 (2005).
He, Q. et al. Sex-specific fat distribution is not linear across pubertal groups in a multiethnic study. Obes Res. 12, 725–733 (2004).
He, Q. et al. Sex and race differences in fat distribution among Asian, African-American, and Caucasian prepubertal children. J Clin Endocrinol Metab. 2164–2170 (2002).
Plumptre, L. et al. Longitudinal Analysis of Sleep Duration and Cardiometabolic Risk in Young Children. Child Obes. 13, 291–299 (2017).
Miller, M. A., Kruisbrink, M., Wallace, J., Ji, C. & Cappuccio, F. P. Sleep duration and incidence of obesity in infants, children, and adolescents: a systematic review and meta-analysis of prospective studies. Sleep. 41, https://doi.org/10.1093/sleep/zsy018 (2018).
Sun, Q., Bai, Y., Zhai, L., Wei, W. & Jia, L. Association between Sleep Duration and Overweight/Obesity at Age 7(-)18 in Shenyang, China in 2010 and 2014. Int J Environ Res Public Health. 15, https://doi.org/10.3390/ijerph15050854 (2018).
Wang, H., Lin, S. L., Leung, G. M. & Schooling, C. M. Age at Onset of Puberty and Adolescent Depression: “Children of 1997” Birth Cohort. Pediatrics. 137, https://doi.org/10.1542/peds.2015-3231 (2016).
Daniels, S. R., Khoury, P. R. & Morrison, J. A. Utility of different measures of body fat distribution in children and adolescents. Am J Epidemiol. 152, 1179–1184 (2000).
Li, A. M. et al. Validation of a questionnaire instrument for prediction of obstructive sleep apnea in Hong Kong Chinese children. Pediatr Pulmonol. 41, 1153–1160 (2006).
Hirshkowitz, M. et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 1, 40–43 (2015).
Ogden, C. L. & Flegal, K. M. Changes in terminology for childhood overweight and obesity. Natl Health Stat Report. 1–5 (2010).
Barlow, S. E. & Expert, C. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 120(Suppl 4), S164–192 (2007).
Leung, S. S., Cole, T. J., Tse, L. Y. & Lau, J. T. Body mass index reference curves for Chinese children. Ann Hum Biol. 25, 169–174 (1998).
Zimmet, P. et al. The metabolic syndrome in children and adolescents - an IDF consensus report. Pediatr Diabetes. 8, 299–306 (2007).
Sung, R. Y. et al. Waist circumference and waist-to-height ratio of Hong Kong Chinese children. BMC Public Health. 8, 324, https://doi.org/10.1186/1471-2458-8-324 (2008).
Alberti, K. G. M. M. et al. Harmonizing the Metabolic Syndrome. A Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 120, 1640–1645 (2009).
Acknowledgements
The work was supported by grants from the Hong Kong Association for the Study of Obesity, Health and Medical Research Fund, Food and Health Bureau (Ref. No.:12110042) and the Research Grants Council of the Hong Kong Special Administrative Region, China (Ref. No.: CUHK4055/01 M and 467410). GT is supported by the Croucher Foundation of Hong Kong. We thank all nursing, medical and research staff, especially Ms Lana Lam and Ms Candy Fong for their assistance in the recruitment of subjects. We also thank all subjects for participating in the study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the analysis and preparation of the manuscript. All authors, except J.Z., K.C.C. and M.H.M.C. contributed to the collection of the data. A.P.S.K., the corresponding author, accepts full responsibility for the content of this paper.
Corresponding author
Ethics declarations
Competing Interests
J.C.N.C. has received research grants and/or honoraria for consultancy or giving lectures, from Bayer, Boehringer Ingelheim, Daiichi-Sankyo, Eli-Lilly, Glaxo Smith Kline, Merck Sharp & Dohme, Merck Serono, Pfizer, Astra Zeneca, Sanofi, Novo-Nordisk and/or Bristol-Myers Squibb. A.P.S.K. has received honoraria for consultancy or giving lectures from Abbott, Astra Zeneca, Sanofi, Novo-Nordisk, Eli-Lilly, Merck Serono, Pfizer and Nestle. All proceeds have been donated to the Chinese University of Hong Kong, American Diabetes Association and other charity organizations to support diabetes research and education. L.L.L. has received research grants and/or honoraria for giving lectures from AstraZeneca, Boehringer Ingelheim, Merck Serono, Merck Sharp & Dohme, Novartis, Novo Nordisk, Sanofi Aventis and Servier. Other authors declared no conflict of interest with this manuscript.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lim, LL., Tse, G., Choi, K.C. et al. Temporal changes in obesity and sleep habits in Hong Kong Chinese school children: a prospective study. Sci Rep 9, 5881 (2019). https://doi.org/10.1038/s41598-019-42346-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-42346-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.