Abstract
The association between physical activity (PA) and atrial fibrillation (AF) remains unclear. We thus investigated association of PA with the development of AF. Type and duration data for PA were acquired from 211,992 AF-free individuals using the validated Korean version of the International Physical Activity Questionnaire Short From between March 2002 and December 2014. Individuals were divided into four groups according to self-reported PA level and previous international PA guidelines: no PA with a sedentary lifestyle, insufficient PA, sufficient PA, and health-enhancing PA. AF was diagnosed by annual 12-lead electrocardiogram. During a median follow-up of 5.6 years, AF occurred in 304 participants (annual AF incidence rate 2.5/10,000 person-years). After adjusting for age and sex, PA level was not associated with AF incidence (P for trend = 0.26). The multivariable-adjusted hazard ratios (95% confidence interval) for incidental AF was 1.00 (0.74–1.37) for the insufficient PA group, 1.34 (0.91–1.97) for the sufficient PA group, and 1.27 (0.72–2.23) for the health-enhancing PA group compared with the no PA group (P for trend = 0.18). Thus, our study does not support an association between the risk of AF and PA level in a young Korean population.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF) is the most commonly identified arrhythmia. It can lead to significantly increased morbidity and mortality1. Traditional risk factors for AF include advanced age, hypertension, diabetes mellitus, structural heart disease, alcohol abuse, pulmonary disease, and thyroid disease2. Vigorous long-term physical activity (PA) is reported to increase AF risk3,4,5,6, but controversy remains regarding the association between PA and AF. Previous studies found that long-term participation in endurance sports or rigorous PA increased the risk of AF in young and middle-aged men3,7,8,9. However, other studies reported that leisure-time PA at an older age was associated with decreased AF risk in the general population8. A prospective study of older men and women observed a reduction in AF risk with moderate-intensity PA but found no increase in risk with high-intensity PA10. These divergent results might be caused by the use of different definitions of PA or study population characteristics (e.g., age and sex). Most research about PA and risk of AF has focused on Caucasians, and studies on the relationship PA level and AF risk in Asians are scarce. Thus, we examined the influence of PA on the risk of developing AF in a large, general Korean population.
Methods
Study population
The Kangbuk Samsung Health Study is a cohort study of South Korean men and women 18 years of age or older who underwent a comprehensive annual health examination at Kangbuk Samsung Hospital Total Health Centers in Seoul or Suwon, South Korea11. More than 80% of participants were employees or spouses of employees of local companies or governmental organizations. In South Korea, the Industrial Safety and Health law requires annual or biennial health screening examinations of all employees. The remaining 20% of the participants voluntarily took part in the screening examinations. The study population was 234,170 individuals who participated in an annual comprehensive health screening examination at Kangbuk Samsung Hospital, Seoul, Korea, between March 2002 and December 2014. We excluded participants for whom data on smoking, alcohol intake, PA (n = 19,533), cancer history (n = 2,475), or baseline AF (n = 170) were missing. After these exclusions, 211,992 participants were eligible for analysis. The Institutional Review Board of Kangbuk Samsung Hospital approved this study. The need for informed consent was waived as we used only anonymized retrospective data routinely collected during the health screening process.
Measurements
All individuals completed self-administered questionnaires related to their medical, social, smoking, and alcohol consumption history. Individuals were asked about their duration of education (high school graduate or less, community college or university graduate), smoking history (never, former, or current) and alcohol consumption (moderate <20 g/day or high ≥20 g/day). Blood pressure (BP) was measured in a sitting position with the arm supported at heart level. Hypertension (HTN) was defined as systolic BP ≥ 140 mmHg, diastolic BP ≥ 90 mmHg or self-reported history of HTN12. Diabetes mellitus (DM) was defined as a fasting serum glucose level ≥126 mg/dl or HbA1c ≥ 6.5%, self-reported history of diabetes, or current use of diabetes medication13. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Obesity was defined according to recommendations for Asian populations14 with a BMI threshold for obesity ≥25 kg/m2. Abdominal ultrasonography was performed by experienced clinical radiologists, and fatty liver was diagnosed based on standard criteria15. Cardiovascular disease (CVD) was defined as a group of disorders of the heart and blood vessels, including coronary heart disease and stroke.
Laboratory measurements of serum biochemical parameters, including total cholesterol, triglycerides, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), glucose, insulin, insulin resistance, A1C, and high-sensitivity C reactive protein (hs-CRP) were the same as detailed elsewhere11.
Assessment of physical activity
PA levels were assessed using the validated Korean version of the International Physical Activity Questionnaire Short Form (IPAQ-SF)16. From 2011 on, the validated Korean version of the IPAQ-SF was used to assess the weekly frequency of moderate- or high-intensity PA. Although IPAQ-SF had not been officially introduced, similar questionnaires were used before 2011. The IPAQ-SF measures the frequency and duration of moderate-to-high-intensity PA for more than 10 continuous minutes across all usual activities at work and home or during leisure for middle-aged individuals during a seven-day period17. Specific questions asked to gauge the number of times per week a participant engaged in PA were: “During the past 7 days, how many days did you undertake high-intensity PA, such as heavy lifting, aerobics, or fast bicycling?” or moderate-intensity PA e.g., carrying light loads, bicycling at a steady pace, or doubles tennis?” If the answer was “1 or more”, additional questions were asked, such as “How much time did you usually spend performing moderate- or high-intensity PA on one of those days17?” The metabolic equivalents (MET) level-minutes per week were calculated by assigning standardized MET values of 4 and 8 for moderate- and high-intensity activities, respectively17. Previous international guidelines recommended at least 150 minutes per week of moderate-intensity PA and 75 minutes per week of high-intensity PA18,19. Participants were divided into four groups according to IPAQ-SF and the above-mentioned guidelines: no PA with a sedentary lifestyle, insufficient PA18,19, sufficient PA18,19 and strenuous health-enhancing PA17,19,20. Participants were categorized into the insufficient PA group if they neither meet sufficient PA nor strenuous health-enhancing PA criteria. Participants in the sufficient PA group met any of the following criteria: (1) 3 or more days of high-intensity activity of at least 20 minutes per day, (2) 5 or more days of moderate-intensity activity at least 30 minutes per day, or (3) 5 or more days of any combination of moderate- or high-intensity activities achieving at least 600 MET-minutes/week17. Participants were categorized into the health-enhancing PA group if they met either of 2 criteria: (1) high-intensity activity on at least 3 days per week accumulating at least 1500 MET-minutes/week or (2) 7 days of any combination of moderate- and high-intensity activities achieving at least 3000 MET-minutes/week17.
Follow-up and AF detection
Diagnosis of AF was based on annual 12-lead electrocardiography and was confirmed by an experienced cardiologist.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation (SD) for normally distributed variables or as median and interquartile range (IQR) if not normally distributed. Comparisons between groups were performed with one-way analysis of variance (ANOVA) with Tukey’s multiple comparison analysis for continuous variables. Categorical variables were expressed as percentages and compared between groups using the Chi-square test. We conducted a Cox proportional hazard regression to estimate the hazard ratios with 95% confidence interval (CI) for AF incidence according to PA level. The group that performed no PA with a sedentary life-style was used as the reference. We adjusted analyses for three different models. Model 1 was adjusted for age, sex, center (Seoul, Suwon), year of screening examination, smoking status (never, former, or current), alcohol intake (moderate <20 g/day or high ≥20 g/day), and education level (high school graduate or less, community college, or university graduate). Model 2 was adjusted for model 1 covariates and BMI, history of HTN, DM, and CVD. Model 3 was adjusted for the covariates of model 2 and hs-CRP. Statistical analysis of data was performed using PASW version 18 (SPSS, Chicago, IL, USA). Statistical tests were two-tailed, and p < 0.05 was considered statistically significant.
Results
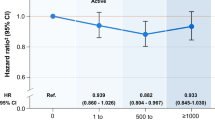
During a median follow-up of 5.6 years (IQR 2.7–8.4), 304 (0.14%) AF cases (278 men and 26 women) were diagnosed, corresponding to 2.5 cases of AF per 10,000 person-years. The mean age of participants with AF was 44.7 ± 10.4 years. Baseline characteristics of the study population according to the incidence of AF are presented in Table 1. Participants with incidental AF were more likely to be men of older age, current smokers and alcohol drinkers. They were more likely to have higher BMI, higher systolic and diastolic blood pressure, higher blood glucose, worse lipid profile, and more underlying obesity, fatty liver, HTN, and CVD than those with no AF. Table 2 shows baseline characteristics of participants according to PA level. The health-enhancing PA group was older and had fewer cardiovascular risk factors, including lower BMI, LDL-C, triglycerides, and blood insulin levels, higher HDL-C, a lower prevalence of obesity and fatty liver, and less alcohol intake than those with insufficient PA. A slightly higher proportion of people with DM, HTN, and existing CVD were included in the health-enhancing PA group compared to the no PA with a sedentary lifestyle group. Table 3 shows risk of incidental AF according to PA level. After adjusting for age and sex, PA level was not associated with AF incidence (P for trend = 0.26). After further adjustment for center, year of screening examination, smoking status, alcohol intake, education level, BMI, diabetes, HTN, CVD, and hs-CRP, PA level was not associated with AF incidence (model 3). The hazard ratio for incidental AF was 1.00 (95% CI 0.74–1.37) for the insufficient PA group, 1.34 (95% CI 0.91–1.97) for the sufficient PA group, and 1.27 (95% CI 0.72–2.23) for the health-enhancing group compared with the no PA group (P for trend = 0.18).
Discussion
Our results demonstrated that PA level was not associated with AF risk. Generally, PA protects against AF by modifying traditional cardiovascular risk factors such as HTN21, diabetes22, obesity23, and sleep apnea, which improve cardiac structure and function24. Furthermore, PA has beneficial effects on age-related declines in arterial elasticity25. Despite these favorable risk factor modifications, several studies have suggested that young athletes who participate in endurance sports long-term or people with high-intensity PA levels have increased risk for AF3,4,6,7. Some studies found that AF risk is increased from 2- to 7-fold in the endurance athlete population3,6. However, studies of PA risk for AF have varied widely with regard to study design, adopting diverse definitions and durations of PA and different study population characteristics (such as age and sex)26,27. One retrospective study found a graded dose-response relationship between regular endurance PA and risk for AF in men aged >53 years5. However, Mozaffarian et al. reported a U-shaped association between PA and AF risk in adults ≥65 years10: moderate-intensity PA was associated with significantly lower AF incidence compared with no PA, but high-intensity PA did not significantly lower risk compared to no PA. Some authors demonstrated a J-shaped relationship between PA and the risk of AF, suggesting that AF risk was negatively associated with moderate-intensity PA, but positively associated with high-intensity PA via autonomic nervous system alterations and remodeling of the heart28,29. This study also found that lower resting heart rate was associated with risk of AF and could be used as an alternative measure to overcome the methodological limitations of self-reported PA28. Similar results in a large cohort study indicated that low resting heart rate and high-intensity PA were associated with AF30. Recent meta-analysis demonstrated that sedentary lifestyle significantly increases and moderate-intensity PA reduces the risk of AF in men and women27. A large cohort study reported that higher levels of moderate- to high-intensity leisure-time PA (for more than five hours/week) at a younger age (30 years) in men was associated with increased AF risk later in life8, whereas leisure time PA in older men (mean age of 60 years) did not increase the risk of AF. Frequent high-intensity PA (5–7 times/week) has been reported to increase AF risk by 20% in men <50 years old compared to those who do not engage in PA31. These studies suggested that long-term high-intensity PA at a younger age increases risk of AF.
Potential mechanisms for increased AF with frequent high-intensity PA include left atrial enlargement, left ventricular hypertrophy, left ventricular dilation, inflammatory changes to the atrium, and increased parasympathetic tone32,33. Contrary to the findings of previous studies, our study indicated that high-intensity PA was not significantly associated with increased AF risk. Despite additional analysis after reclassification of the excessive PA group among the health-enhancing group, there were no significant associations between PA and AF risk. Our study population was not at high risk for AF because of their relatively younger age and low prevalence of HTN (14%), diabetes (2.7%), and CVD (3.3%). These baseline characteristics were not significantly different from other studies28,30. However, direct comparisons of PA level among studies is challenging due to the diverse definitions of the intensity and duration of PA used in each study. Some studies included elite skiers5,6 or marathon runners3 over a 10-year follow-up period, and the PA level of people engaging in these sports would be higher than that garnered from leisure time PA in the general population. The average degree of self-reported PA in our study might not be as intense as that of athletes, and therefore may be insufficient to cause structural remodeling of the heart that could affect AF incidence. The beneficial effects of PA on modifiable risk AF factors, including HTN21, diabetes34, and obesity could override the potential negative effects of high-intensity PA in the general population.
Some previous studies reported gender differences in the association between PA and incident AF27,35,36. They found that women did not exhibit the same increased risk of AF with high-intensity PA as men. A possible explanation was that women have less pronounced atrial remodeling and lower sympathetic tone despite comparable PA compared with men37. Whereas AF patients were predominantly men in our study, the incidence of AF in women was too small for statistical analysis. Future large-scale studies investigating gender differences between PA and the risk of AF are needed. Another study demonstrated that height was associated with AF9. Although AF patients were taller compared with those without AF in our study, the relationships between height and the incidence of AF remain unclear.
Our results were in line with the Danish Diet, Cancer, and Health study, which did not demonstrate an association between working hours or PA and AF risk38. The study proposed that the association may be weak because publication bias has led to an overemphasis on the association between risk of AF and endurance sport activities. Some meta-analyses found no significant increase in AF with high-intensity PA39,40,41.
Our study was a general Asian population-based study with a large sample size, but a small number of AF cases. Our study had several limitations. First, PA level was self-reported. Although we used the validated IPAQ-SF, recall bias was still possible, such as over-reporting or imprecise reporting of PA. More objective and accurate measures of PA such as maximal oxygen uptake (VO2 max) could be used to clarify the relationship between PA and AF risk in future studies. Second, it is possible that the incidence of AF could have been underestimated; we cannot rule out the possibility that some participants classified as non-cases had paroxysmal AF. Yearly assessment of AF with only a 12-lead ECG could miss paroxysmal AF or short-duration AF in younger (<40 years) individuals. Frequent and longer ECG monitoring such as seven-day Holter monitoring, event recording, or an implantable loop recording could be more accurate diagnostic tools for paroxysmal AF. Third, there might have been selection bias because >80% of the study population consisted of employees or spouses of employees of local companies and governmental organizations, therefore limiting generalizability to the entire Korean population. Fourth, AF incidence and prevalence will likely grow as the population continues to age. There may have been too few cases of AF to validate its association with PA level because our study cohort was not at high risk for AF. Generalization of our study to other populations should be undertaken with caution. Lastly, the relatively short follow-up period could be another limitation to fully evaluating the association between PA and the risk of AF.
In conclusion, our study does not support an association between the risk of AF and PA level in a young Korean population.
Change history
05 June 2019
A correction to this article has been published and is linked from the HTML and PDF versions of this paper. The error has been fixed in the paper.
References
Chugh, S. S. et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 129, 837–847 (2014).
Benjamin, E. J. et al. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. Jama. 271, 840–844 (1994).
Molina, L. et al. Long-term endurance sport practice increases the incidence of lone atrial fibrillation in men: a follow-up study. Europace. 10, 618–623 (2008).
Mont, L. et al. Long-lasting sport practice and lone atrial fibrillation. Eur Heart J. 23, 477–482 (2002).
Myrstad, M. et al. Effect of years of endurance exercise on risk of atrial fibrillation and atrial flutter. The American journal of cardiology. 114, 1229–1233 (2014).
Andersen, K. et al. Risk of arrhythmias in 52755 long-distance cross-country skiers: a cohort study. Eur Heart J. 34, 3624–3631 (2013).
Elosua, R. et al. Sport practice and the risk of lone atrial fibrillation: a case-control study. International journal of cardiology. 108, 332–337 (2006).
Drca, N., Wolk, A., Jensen-Urstad, M. & Larsson, S. C. Atrial fibrillation is associated with different levels of physical activity levels at different ages in men. Heart (British Cardiac. Society). 100, 1037–1042 (2014).
Mont, L. et al. Physical activity, height, and left atrial size are independent risk factors for lone atrial fibrillation in middle-aged healthy individuals. Europace. 10, 15–20 (2008).
Mozaffarian, D., Furberg, C. D., Psaty, B. M. & Siscovick, D. Physical activity and incidence of atrial fibrillation in older adults: the cardiovascular health study. Circulation. 118, 800–807 (2008).
Ryu, S. et al. Relationship of sitting time and physical activity with non-alcoholic fatty liver disease. Journal of hepatology. 63, 1229–1237 (2015).
Reisin, E., Harris, R. C. & Rahman, M. Commentary on the 2014 BP guidelines from the panel appointed to the Eighth Joint National Committee (JNC 8). Journal of the American Society of Nephrology: JASN. 25, 2419–2424 (2014).
American Diabetes Association. Erratum. Classification and diagnosis of diabetes. Sec. 2. In Standards of Medical Care in Diabetes-2016. Diabetes Care 2016;39(Suppl. 1):S13–S22. Diabetes care. 39, 1653 (2016).
Wen, C. P. et al. Are Asians at greater mortality risks for being overweight than Caucasians? Redefining obesity for Asians. Public health nutrition. 12, 497–506 (2009).
Saverymuttu, S. H., Joseph, A. E. & Maxwell, J. D. Ultrasound scanning in the detection of hepatic fibrosis and steatosis. British medical journal (Clinical research ed.). 292, 13–15 (1986).
Oh, J. Y. et al. F. M. Validity and reliability of Korean version of International Physical Activity Questionnaire (IPAQ) short form. 28, 532–541 (2007).
Craig, C. L. et al. International physical activity questionnaire: 12-country reliability and validity. Medicine and science in sports and exercise. 35, 1381–1395 (2003).
US Department of Health and Human Services. 2008 Physical activity guidelines for Americans (Office of Disease Prevention and Health Promothion: Washington, DC, 2008).
World Health Organization. Global Recommendations on Physical Activity for Health (World Health Organization: Geneva, 2010).
Chun, M. Y. Validity and reliability of korean version of international physical activity questionnaire short form in the elderly. Korean journal of family medicine. 33, 144–151 (2012).
Cornelissen, V. A. & Fagard, R. H. Effects of endurance training on blood pressure, blood pressure-regulating mechanisms, and cardiovascular risk factors. Hypertension (Dallas, Tex.: 1979). 46, 667–675 (2005).
Knowler, W. C. et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England journal of medicine. 346, 393–403 (2002).
Pathak, R. K. et al. Impact of CARDIOrespiratory FITness on Arrhythmia Recurrence in Obese Individuals With Atrial Fibrillation: The CARDIO-FIT Study. Journal of the American College of Cardiology. 66, 985–996 (2015).
Bhella, P. S. et al. Impact of lifelong exercise “dose” on left ventricular compliance and distensibility. Journal of the American College of Cardiology. 64, 1257–1266 (2014).
Yang, Z. et al. Regular exercise-induced increased number and activity of circulating endothelial progenitor cells attenuates age-related decline in arterial elasticity in healthy men. International journal of cardiology. 165, 247–254 (2013).
Wernhart, S. & Halle, M. Atrial fibrillation and long-term sports practice: epidemiology and mechanisms. Clinical research in cardiology: official journal of the German Cardiac Society. 104, 369–379 (2015).
Mohanty, S. et al. Differential Association of Exercise Intensity With Risk of Atrial Fibrillation in Men and Women: Evidence from a Meta-Analysis. Journal of cardiovascular electrophysiology. 27, 1021–1029 (2016).
Morseth, B. et al. Physical activity, resting heart rate, and atrial fibrillation: the Tromso Study. Eur Heart J. 37, 2307–2313 (2016).
Morseth, B., Lochen, M. L., Ariansen, I., Myrstad, M. & Thelle, D. S. The ambiguity of physical activity, exercise and atrial fibrillation. European journal of preventive cardiology. 25, 624–636 (2018).
Thelle, D. S. et al. Resting heart rate and physical activity as risk factors for lone atrial fibrillation: a prospective study of 309,540 men and women. Heart (British Cardiac Society). 99, 1755–1760 (2013).
Aizer, A. et al. Relation of vigorous exercise to risk of atrial fibrillation. The American journal of cardiology. 103, 1572–1577 (2009).
Lampert, R. Evaluation and management of arrhythmia in the athletic patient. Progress in cardiovascular diseases. 54, 423–431 (2012).
Wilhelm, M. et al. Atrial remodeling, autonomic tone, and lifetime training hours in nonelite athletes. The American journal of cardiology. 108, 580–585 (2011).
Kujala, U. M., Kaprio, J., Taimela, S. & Sarna, S. Prevalence of diabetes, hypertension, and ischemic heart disease in former elite athletes. Metabolism: clinical and experimental. 43, 1255–1260 (1994).
Zhu, W. G. et al. Sex Differences in the Association Between Regular Physical Activity and Incident Atrial Fibrillation: A Meta-analysis of 13 Prospective Studies. Clinical cardiology. 39, 360–367 (2016).
Drca, N., Wolk, A., Jensen-Urstad, M. & Larsson, S. C. Physical activity is associated with a reduced risk of atrial fibrillation in middle-aged and elderly women. Heart (British Cardiac Society). 101, 1627–1630 (2015).
Wilhelm, M. et al. Gender differences of atrial and ventricular remodeling and autonomic tone in nonelite athletes. The American journal of cardiology. 108, 1489–1495 (2011).
Frost, L., Frost, P. & Vestergaard, P. Work related physical activity and risk of a hospital discharge diagnosis of atrial fibrillation or flutter: the Danish Diet, Cancer, and Health Study. Occupational and environmental medicine. 62, 49–53 (2005).
Kwok, C. S., Anderson, S. G., Myint, P. K., Mamas, M. A. & Loke, Y. K. Physical activity and incidence of atrial fibrillation: a systematic review and meta-analysis. International journal of cardiology. 177, 467–476 (2014).
Ofman, P. et al. Regular physical activity and risk of atrial fibrillation: a systematic review and meta-analysis. Circulation. Arrhythmia and electrophysiology. 6, 252–256 (2013).
Muller-Riemenschneider, F., Andersohn, F., Ernst, S. & Willich, S. N. Association of physical activity and atrial fibrillation. Journal of physical activity & health. 9, 605–616 (2012).
Author information
Authors and Affiliations
Contributions
Ki-Chul Sung designed the study, Seungho Ryu conducted data analysis, Sung Ho Lee wrote the initial draft of the manuscript, Ki-Chul Sung and Byung Jin Kim critically contributed to data reanalysis and draft revision, and Jong Young Lee and Dae Chul Seo contributed to interpretation of the data and preparation of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, S.H., Ryu, S., Lee, JY. et al. Association between self-reported physical activity and incident atrial fibrillation in a young Korean population. Sci Rep 9, 4222 (2019). https://doi.org/10.1038/s41598-019-40744-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-40744-x
This article is cited by
-
Physical activity and risk of atrial fibrillation in the general population: meta-analysis of 23 cohort studies involving about 2 million participants
European Journal of Epidemiology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.