Abstract
Proton pump inhibitors, PPIs, are widely prescribed and sold globally. Although initially intended for time-limited treatment of acute disorders, such as gastric ulcers and esophagitis, PPIs are now commonly used for prolonged durations and are considered safe for over the counter access. Recent studies have raised concern over associations between PPI use and acute kidney injury, chronic kidney disease, end-stage renal disease, and electrolyte abnormalities. The growing concern over potentially serious adverse drug reactions warrants an evaluation of post marketing surveillance data. In this study of over ten million FDA Adverse Event Reporting System records, we provided evidence of kidney injury and electrolyte imbalances in an alarming number of patients taking PPIs. Additionally, we assessed differences between specific PPIs and observed significant electrolyte and renal abnormalities for each individual drug with varying magnitudes.
Similar content being viewed by others
Introduction
The World Health Organization includes proton pump inhibitors (PPIs) in the list of essential medicines and health products1. PPIs have demonstrated superior efficacy to histamine-2 receptor antagonists (H2RAs) in treatment of acid-related disorders and have replaced the H2RAs2,3. The current indications include treatment of gastroesophageal reflux disease, non-steroidal anti-inflammatory drug (NSAID) and Helicobacter pylori induced ulcers, duodenal ulcers, erosive esophagitis, and other pathological hypersecretory conditions, including Zollinger-Ellison syndrome4,5 (see Supplement-Appendix A for a more comprehensive indication list reported to FDA) and are now one of the most widely utilized medications6. The superior efficacy is credited to the mechanism of action. All currently marketed PPIs inhibit the hydrogen pump H +/K+ ATPase irreversibly, preventing the last and rate-limiting step in acid secretion by parietal cells in the stomach7,8. There are currently six Food and Drug Administration (FDA) approved PPIs: rabeprazole, lansoprazole, pantoprazole, esomeprazole, omeprazole, and dexlansoprazole. These were sequentially developed due to varying pharmacokinetic parameters, such as extended plasma half-life, routes of administration, and drug interactions9,10. The most common PPI adverse reactions (ADRs) are mild and include headache, nausea, stomach pain, diarrhea, vomiting, and flatulence. Serious allergic reactions include rash, facial swelling, throat tightness, and difficulty breathing11. Generally considered safe, PPIs are now commonly used for prophylaxis and sold over the counter in most of the industrialized countries, including the United States, with annual prescription and over the counter sales exceeding fourteen billion dollars anually12.
Recently, PPI use has come under scrutiny due to growing evidence of renal, cardiovascular, autoimmune and neurologic adverse effects. New data has revealed associations with myocardial infarction13, Clostridium difficile-associated diarrhea14, community acquired pneumonia15, bone fractures16, subacute cutaneous lupus erythematosus17,18, Alzheimer’s dementia19,20, and kidney injury21,22,23,24,25,26,27,28,29. Here we evaluated the frequencies of reported adverse events related to kidney injury and electrolyte disturbances in patients taking PPIs. We also compared the magnitude of the effects for individual PPIs.
Results
PPI “monotherapy”-related renal and electrolyte ADRs
Patients who used PPIs with no other reported concurrent medications had a significant increase in the frequency of the following renal adverse event reports compared to the H2RAs: chronic kidney disease (CKD) (OR 28.4, 95% CI [12.7, 63.5]), acute kidney injury (AKI) (4.2 [2.8, 6.3]), end-stage renal disease (ESRD) (35.5 [5.0, 250.0]), renal impairment of unspecified type (8.0 [5.0, 13.0]), and nephrolithiasis (2.8 [1.3, 6]) (Fig. 1b). The composite renal ADR frequency was 5.6% of the total PPI “monotherapy” ADRs reports and 0.7% for H2RA “monotherapy” reports (8.6 [6.6, 11]) (Fig. 1a).
Frequencies and odds ratios (ORs) of renal adverse drug reactions (ADRs). (a) Frequencies of renal adverse events for patients in FAERS/AERS who took PPIs (n = 42,537) and H2RAs (n = 8,309). (b) Odds ratios were calculated comparing adverse event frequencies of PPI and H2RA patients. Abbreviations: CKD-Chronic Kidney Disease, AKI-Acute Kidney Injury, ESRD-End Stage Renal Disease, and NOS-Not otherwise specified. Ranges represent 95% confidence intervals (95% CI) (see Methods). X-axis is presented in log scale.
Interestingly, relative frequencies for electrolyte abnormalities followed the same trend (Fig. 2a) and were also increased for PPI users: hypomagnesemia (OR 78.5 [11, 560]), hypocalcemia (25.5 [6.4, 100]), hypokalemia (6.3 [2.6, 15]), and hyponatremia (2.2 [1.1, 4.6]) (Fig. 2b).
Frequencies and ORs of electrolyte related ADRs. (a) Frequencies of electrolyte related events for patients on PPIs (n = 42,537) and H2RAs (n = 8,309). (b) Odds ratios were calculated from adverse event frequencies. Ranges represent 95% confidence intervals (see Methods). X-axis is presented in log scale.
Renal impairment and Individual PPIs
Analysis of renal and electrolyte adverse effects for each individual PPI produced the following results shown in Fig. 3.
Renal ADR ORs of individual PPIs used as “monotherapy” (Rabeprazole n = 724, Lansoprazole n = 3,360, Pantoprazole n = 3,651, Esomeprazole n = 27,053, Omeprazole n = 7,749) when compared to H2RAs (n = 8,309). Odds ratios were calculated comparing (a) AKI (b) CKD, (c) ESRD (d) Nephrolithiasis and (e) renal impairment adverse event report frequencies of individual PPIs to all H2RAs (x-axis presented in log scale). NOS = not otherwise specified.
Acute Kidney Injury
Patients who received the following PPIs as “monotherapy” had a significant increase in the frequency of AKI reports: omeprazole (OR 5.8 [3.8, 8.9]), esomeprazole (3.3 [2.2, 5]), pantoprazole (1.8 [1.01, 3.3]), and lansoprazole (10.8 [7.0, 17]). Patients who received rabeprazole as “monotherapy” had an increase in AKI frequency, but it was not significant (1.8 [0.6, 5.3]) (Fig. 3a).
Chronic Kidney Disease
Patients who received the following PPIs as “monotherapy” had a significant increase in the frequency of CKD reports: omeprazole (OR 18.1 [7.9, 41]), esomeprazole (29.9 [13, 67]), and lansoprazole (154.9 [49, 490]). Patients who received rabeprazole and pantoprazole as “monotherapy” had an increase in CKD frequency, but the significance criteria were not met (1.9 [0.2,16]) and (3.0 [0.7, 14]) respectively (Fig. 3b).
End Stage Renal Disease
ESRD is of particular concern due to the limited prognosis in the absence of receiving dialysis or a kidney transplant. Very large OR values were determined for three widely used PPIs: omeprazole (OR 30.1 [4.1, 220]), esomeprazole (34.7 [4.8, 250]), and lansoprazole (97.6 [13, 710]) demonstrating a significant association with ESRD. The frequency of ESRD with pantoprazole “monotherapy” did not reach statistical significance (4.6 [0.4, 50]). Patients who received rabeprazole did not have any ESRD reports (Fig. 3c).
Nephrolithiasis
Within the PPI cohort, patients who received the following PPIs as “monotherapy” had a significant increase in the frequency of nephrolithiasis reports: omeprazole (OR 3.4 [1.4, 7.9]), esomeprazole (2.4 [1.1, 5.3]), pantoprazole (3.3 [1.2, 8.6]), and lansoprazole (3.9 [1.5, 10.1]). Patients who received rabeprazole as “monotherapy” according to FAERS reports had an increase in nephrolithiasis frequency but did not meet the significance criteria (3.3 [0.7, 15.8]) (Fig. 3d).
Renal Impairment
A large portion of renal impairment reports did not specify acuity of the injury, marked as renal impairment NOS (not otherwise specified). It was important to see if the observed renal side effects of PPIs persisted in this category of reports. In agreement with the preceding results, the OR values were significantly increased: omeprazole (OR 11.5 [7.1, 19]), esomeprazole (7.9 [4.9, 13]), pantoprazole (2.9 [1.6, 5.4]), lansoprazole (5.0 [2.8, 8.8]) and rabeprazole (12.4 [6.5, 24]) (Fig. 3e).
Electrolyte Disturbances: magnesium, calcium, potassium, sodium
All five PPIs were associated with a dramatic increase in hypomagnesemia reports (Fig. 4a, Table 1). Additionally, all the studied PPIs were associated with a significant increase in hypocalcemia reports (Fig. 4b, Table 1). Patients who received the following PPIs had an increase in the frequency of hypokalemia reports: omeprazole, esomeprazole, pantoprazole, and lansoprazole. Patients who received rabeprazole had an increase in hypokalemia frequency, but it was not statistically significant (Fig. 4c, Table 1).
Electrolyte ADR odds ratios of individual PPIs used as “monotherapy” (Rabeprazole n = 724, Lansoprazole n = 3,360, Pantoprazole n = 3,651, Esomeprazole n = 27,053, Omeprazole n = 7,749) when compared to all H2RAs (n = 8,309). Odds ratios were calculated comparing (a) hypomagnesemia, (b) hypocalcemia, (c) hypokalemia, and (d) hyponatremia adverse event report frequencies of individual PPIs to all H2RAs.
Hyponatremia was the least pronounced, yet still significant, electrolyte disturbance associated with omeprazole, lansoprazole, and rabeprazole. In contrast, reports of hyponatremia with esomeprazole or pantoprazole did not reach statistical significance. (Fig. 4d, Table 1).
Methods
FDA Adverse Event Reporting System
The FDA Adverse Event Reporting System (FAERS) supports FDA’s post marketing surveillance on drugs and biologic therapeutics submitted to FDA through MedWatch, the FDA Safety Information and Adverse Event Reporting Program. Reporting is voluntary and is done by doctors, pharmacists, legal representatives, other healthcare providers and patients. The manufacturer is the only contributor that is legally required to forward the information to the FDA.
Over 10.3 million FAERS/AERS reports, from January 2004 to March 2018, were used for the analysis. Data sets are available online at: https://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Surveillance/AdverseDrugEffects/ucm082193.htm.
Normalizing and combining the FAERS/AERS reports
Throughout the data set, the quarterly online reports were not homologous from year to year. Each quarterly set was downloaded in dollar-separated text format (.txt) and modified, standardized, and extended. Missing columns in data sets were added with no values and the column names were homogenized. The final data set version contained over 10.3 million reports. Most of the reports were submitted from the United States, and many were submitted from all around the world with their respective country specific demographic formats. Online drug databases were used to generate a dictionary with all international brand/generic drug names and to translate them into generic names.
Study outcomes
A fraction of the observed 20,317 outcomes in FAERS and AERS were grouped into the following generalized outcomes for a priori hypothesis: chronic kidney disease (CKD: defined in FAERS and AERS data sets as chronic kidney disease, and chronic renal failure), acute kidney injury (AKI: acute kidney injury, acute prerenal failure, renal failure acute), and end-stage renal disease (ESRD: end stage renal disease, end stage kidney disease), nephrolithiasis, renal impairment NOS (renal failure, renal impairment, renal disorder, renal injury), hypomagnesemia (hypomagnesemia, decreased blood magnesium), hypocalcemia (hypocalcemia, decreased blood calcium), hypokalemia (hypokalemia, decreased blood potassium) and hyponatremia (hyponatremia, decreased blood sodium).
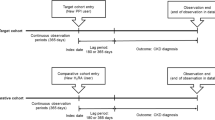
Choice of cohorts
A total of 10,324,033 FAERS and AERS reports were collected. Reports where omeprazole, esomeprazole, rabeprazole, lansoprazole, pantoprazole, and dexlansoprazole were used, excluding reports with concurrent use of any H2RAs, were selected into the PPI cohort (n = 732,696). Reports where ranitidine, famotidine, cimetidine, and nizatidine were used, excluding reports with concurrent use of any PPI, were selected into the H2RA cohort (n = 162,189). Further, reports where PPIs and H2RAs were used as monotherapy were selected into the respective cohorts. The term “monotherapy” pertains to records where PPIs and H2RAs were the only reported medications. PPIs-only cohort comprised of 42,537 reports and H2RA-only cohort comprised of 8,309 reports.
Odds ratio analysis was performed by comparing the ADR frequencies of PPIs in relation to H2RA “monotherapy” frequencies. The PPI “monotherapy” cohort was further split into individual PPI cohorts which included omeprazole (n = 7,749) esomeprazole (n = 27,053), pantoprazole (n = 3,651), lansoprazole (n = 3,360), and rabeprazole (n = 724). There were no reports where dexlansoprazole was used as “monotherapy”. Reports with two or more PPIs used were excluded (Fig. 5). Demographic analysis was performed (Tables 2 and 3). Overall distributions strongly overlap and validate the cohort choice. Each individual PPI cohort frequency of renal and electrolyte ADRs was calculated and compared to the H2RA cohort to screen for potential ADR variability within individual PPIs in the cohort (Figs 3 and 4).
Statistical analysis
Descriptive Statistics
Frequencies for each studied side effect (Figs 1a and 2a) was calculated by the equation:
Comparative Statistics
ADR report rates were compared via the Odds Ratio (OR) analysis for Figs 1b, 2b, 3 and 4 using the following equations:
where
a: Number of cases in exposed group with an adverse event.
b: Number of cases in exposed group with no adverse event.
c: Number of cases in control group with the adverse event.
d: Number of cases in control group with no adverse event.
95% Confidence Interval;
Discussion
In this study, we quantified and confirmed the association between PPI exposure and the increased risk of AKI, CKD, ESRD, and electrolyte abnormalities by utilizing updated adverse event reports in the FAERS/AERS database. Most interestingly, the extended set of reports revealed an association between PPI exposure and unexpected significant risk for nephrolithiasis and renal impairment (Fig. 1). For the first time there were sufficient records for analysis of the effects of individual PPIs and observed varying degrees of electrolyte and renal abnormalities (Figs 3 and 4).
Our analysis of renal adverse effects was in general agreement with previous studies that have documented an increased risk of incident AKI, incident CKD, CKD progression and ESRD in large observational cohorts. Klesper and colleagues performed a nested case-control study, including 184,480 patients, and found an increased risk of AKI with PPI prescription (OR 1.72, 95% confidence interval [CI] [1.27, 2.32], p < 0.001)22. In a population-based cohort study of 290,593 patients over the age of 65, Antoniou and colleagues confirmed the association of PPI use with AKI (hazard ratio [HR] 2.52, 95% CI [2.27, 2.79])29. In the Atherosclerosis Risk in Communities (ARIC) study Lazarus et al. performed a population based prospective cohort study with 10,482 patients and found an increased risk of incident AKI and CKD when comparing PPI users to H2RA users (HR, 1.58; 95% CI [1.05, 2.04]) and (HR, 1.39; 95% CI [1.01, 1.91]), respectively)21. These population-based studies utilized ICD coding data to define the outcome of incident AKI and CKD. Xie and colleagues evaluated a prospective cohort including 193,591 patients from the Veteran’s Affairs database and documented not only an increased risk of incident CKD (HR, 1.28; 95% CI [1.23, 1.34]) but also an increased risk for ESRD when comparing PPI users to H2RA users (HR, 1.96; 95% CI [1.21, 3.18])23 and in a later study demonstrated that CKD progression and ESRD can occur without intervening AKI28. The difference in values between different studies may be due to multiple factors including definitions of renal injury and the diagnostic criteria as well as the time dependent analyses using hazard ratios. The FAERS and AERS data derived frequencies are additionally influenced by the severity related threshold of the report submission. In summary we documented an OR of 4.2 for AKI with the lower 95% CI boundary of 2.9, OR values as large as 28.4, with the 95% CI between 12.7 and 63.5 for CKD and 35.5 with 95% CI between 5.0 and 250.0 for ESRD. Our results indicate significant increase in nephrolithiasis reports with (OR 2.8 (95% CI [1.3, 6.0]). Nephrolithiasis finding is of particular interest since it has been associated with AKI, CKD, and ESRD progression but it only accounts for a small subset of renal injury cases30,31,32.
Hypomagnesemia was reported in the initial clinical trials and on the FDA package insert for every PPI as a rare side effect11. Accordingly, the frequency of hypomagnesemia reports for PPI patients is low, but the relative frequency was dramatically higher, almost eighty-fold, than for the H2RA control group. Secondly, detection bias may underestimate this adverse effect, since magnesium concentrations are not routinely measured compared to sodium, potassium and calcium. All five studied PPIs had comparable and increased ORs, with omeprazole showing the largest magnitude. Omeprazole, being the first marketed and the first over-the-counter PPI, has been used for the longest time, therefore patients were likely to have longer drug exposure. It may be prudent to monitor magnesium levels in patients with ongoing PPI therapy and other risk factors for hypomagnesemia.
Previous studies examining the effect of PPIs’ on calcium levels were not consistent. Multiple small-scale studies have shown that PPIs decrease gastrointestinal calcium absorption33,34,35 and this deleterious effect is attenuated by administering acidic liquids36. However, other studies have noted that the change in gastric pH does not correlate with calcium levels37,38. In our analysis of 42,537 PPI and 8,309 H2RA cases, we found a clear increase in hypocalcemia in patients taking PPIs compared to patients receiving H2RAs. Although the mechanism for hypocalcemia is not clearly defined, we can conclude that all PPIs are significantly associated with hypocalcemia.
We evaluated alterations in serum potassium concentrations. The previous evidence for hypokalemia with PPI use was limited, mainly consisting of case reports39,40,41. We found that PPI utilization resulted in moderately increased hypokalemia, when compared to the H2RA cohort. As noted earlier, PPI utilization was correlated with CKD, known to cause fluctuations in electrolytes. While CKD can be associated with both hypokalemia (e.g. in the case of tubular dysfunction) and hyperkalemia42, we only observed a significant increase in hypokalemia. However, a small number of cases of hyperkalemia were reported out of 42,537 reports in FAERS/AERS. In conclusion, hypokalemia was more common than hyperkalemia in our analysis of patients receiving PPIs. Each PPI was shown to have increased odds of hypokalemia, except for rabeprazole which was not significant (OR 2.3 CI [0.27, 20]).
Hyponatremia has been reported as a rare post marketing adverse reaction in FDA package inserts for pantoprazole, omeprazole, and esomeprazole11,43,44. In a retrospective study of 302 individuals receiving PPIs for longer than a year, Buon and colleagues found moderate hyponatremia in 18.7–46.3% of elderly patients45. It should be noted that although dysnatremia is associated with CKD46, we observed only a minor yet significant increase in hyponatremia reports. Hypernatremia was not a significant adverse effect in PPI users. Our analysis showed hyponatremia effect to be most pronounced for omeprazole, followed by lansoprazole and rabeprazole.
The observed increased risks of renal and electrolyte adverse effects of PPIs warrant more careful consideration in clinical practice. The risk-benefit ratio should be considered for the individual patient with respect to the adverse effects. When clinically indicated, PPIs should be used for the shortest duration necessary and chronic use is not recommended except for treatment of pathological hypersecretory conditions including Zollinger-Ellison syndrome and maintenance healing of erosive esophagitis11,43,44,47,48,49,50,51,52,53,54. It should be noted that the above-mentioned indications are FDA recommendations. Off-label and over-the-counter use of PPIs for the treatment of gastroesophageal reflux disorder (GERD) should be limited to four weeks11,43,44,52,53,54 but is often continued beyond the recommended limit. Continued use can result in rebound acid hypersecretion and hypergastrinemia after 4–8 weeks of therapy55,56 leading to chronic use.
Conclusion
In our study we observed various levels of increased risk of renal and electrolyte ADRs in FAERS reports of individual PPI drugs with respect to H2RA reports. Regardless of which PPI is initiated, it may be beneficial to follow dosing and duration recommendations established by the FDA11,43,44,52,53,54, American College of Gastroenterology47,48 and World Gastroenterology Organisation Global Guidelines49. It may be beneficial to monitor renal function and electrolytes including potassium, calcium, magnesium, and sodium. Although H2RAs have not been shown to be as effective as PPIs, they might be considered as alternatives for patients who are at high risk for developing renal and electrolytes imbalances.
Study Limitations
Since the FDA FAERS/AERS reporting is voluntary, only a subset of actual cases is represented, and ADR frequencies do not represent the population incidences. A recent study found that FAERS/AERS reporting can be biased by legal and scientific variables and newsworthiness50. Another study has shown that FAERS/AERS reporting was significantly underreported for statins51. Some limitation stems from the absence of comprehensive medical records. Although the indication section in the data set was used to exclude potential comorbidities, some concurrent medications and comorbidities may be missing from the records due to underreporting. This may have introduced noise into the cohort compositions, ADR frequencies and odds ratios. The mechanism of the adverse reaction cannot be derived from the FAERS/AERS records. The odds ratios represent frequency ratios of reported adverse effects between FAERS/AERS PPI and H2RA cohorts and are not based on population incidences. As with any association study, causality cannot be inferred from association. These cases were not clinically adjudicated for causality by experts.
References
20th WHO Model List of Essential Medicines. http://apps.who.int/iris/bitstream/handle/10665/273826/EML-20-eng.pdf?ua=1. (2017).
Clissold, S. P. & Campoli-Richards, D. M. Omeprazole. A preliminary review of its pharmacodynamic and pharmacokinetic properties, and therapeutic potential in peptic ulcer disease and Zollinger-Ellison syndrome. Drugs 32, 15–47 (1986).
Walan, A. et al. Effect of omeprazole and ranitidine on ulcer healing and relapse rates in patients with benign gastric ulcer. N Engl J Med 320, 69–75, https://doi.org/10.1056/NEJM198901123200201 (1989).
Chiba, N., De Gara, C. J., Wilkinson, J. M. & Hunt, R. H. Speed of healing and symptom relief in grade II to IV gastroesophageal reflux disease: a meta-analysis. Gastroenterology 112, 1798–1810 (1997).
Strand, D. S., Kim, D. & Peura, D. A. 25 Years of Proton Pump Inhibitors: A Comprehensive Review. Gut Liver 11, 27–37, https://doi.org/10.5009/gnl15502 (2017).
Gawron, A. J. et al. Brand name and generic proton pump inhibitor prescriptions in the United States: insights from the national ambulatory medical care survey (2006–2010). Gastroenterol Res Pract 2015, 689531, https://doi.org/10.1155/2015/689531 (2015).
Shin, J. M. & Sachs, G. Pharmacology of proton pump inhibitors. Curr Gastroenterol Rep 10, 528–534 (2008).
Shin, J. M., Munson, K., Vagin, O. & Sachs, G. The gastric HK-ATPase: structure, function, and inhibition. Pflugers Arch 457, 609–622, https://doi.org/10.1007/s00424-008-0495-4 (2009).
Shi, S. & Klotz, U. Proton pump inhibitors: an update of their clinical use and pharmacokinetics. Eur J Clin Pharmacol 64, 935–951, https://doi.org/10.1007/s00228-008-0538-y (2008).
Shin, J. M. & Kim, N. Pharmacokinetics and pharmacodynamics of the proton pump inhibitors. J Neurogastroenterol Motil 19, 25–35, https://doi.org/10.5056/jnm.2013.19.1.25 (2013).
Prilosec (omeprazole) Label – FDA, https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/019810s096lbl.pdf (2012).
Shaheen, N. J. et al. The burden of gastrointestinal and liver diseases, 2006. Am J Gastroenterol 101, 2128–2138, https://doi.org/10.1111/j.1572-0241.2006.00723.x (2006).
Shah, N. H. et al. Proton Pump Inhibitor Usage and the Risk of Myocardial Infarction in the General Population. PLoS One 10, e0124653, https://doi.org/10.1371/journal.pone.0124653 (2015).
Janarthanan, S., Ditah, I., Adler, D. G. & Ehrinpreis, M. N. Clostridium difficile-associated diarrhea and proton pump inhibitor therapy: a meta-analysis. Am J Gastroenterol 107, 1001–1010, https://doi.org/10.1038/ajg.2012.179 (2012).
Lambert, A. A. et al. Risk of community-acquired pneumonia with outpatient proton-pump inhibitor therapy: a systematic review and meta-analysis. Plos One 10, e0128004, https://doi.org/10.1371/journal.pone.0128004 (2015).
Wilson, C. Bone: proton-pump inhibitors and fractures. Nat Rev Endocrinol 8, 625, https://doi.org/10.1038/nrendo.2012.170 (2012).
Reich, A. & Maj, J. Subacute cutaneous lupus erythematosus due to proton pump inhibitor intake: case report and literature review. Arch Med Sci 8, 743–747, https://doi.org/10.5114/aoms.2012.30300 (2012).
Sandholdt, L. H., Laurinaviciene, R. & Bygum, A. Proton pump inhibitor-induced subacute cutaneous lupus erythematosus. Br J Dermatol 170, 342–351, https://doi.org/10.1111/bjd.12699 (2014).
Gomm, W. et al. Association of Proton Pump Inhibitors With Risk of Dementia: A Pharmacoepidemiological Claims Data Analysis. JAMA Neurol 73, 410–416, https://doi.org/10.1001/jamaneurol.2015.4791 (2016).
Haenisch, B. et al. Risk of dementia in elderly patients with the use of proton pump inhibitors. Eur Arch Psychiatry Clin Neurosci 265, 419–428, https://doi.org/10.1007/s00406-014-0554-0 (2015).
Lazarus, B. et al. Proton Pump Inhibitor Use and the Risk of Chronic Kidney Disease. JAMA Intern Med 176, 238–246, https://doi.org/10.1001/jamainternmed.2015.7193 (2016).
Klepser, D. G., Collier, D. S. & Cochran, G. L. Proton pump inhibitors and acute kidney injury: a nested case-control study. BMC Nephrol 14, 150, https://doi.org/10.1186/1471-2369-14-150 (2013).
Xie, Y. et al. Proton Pump Inhibitors and Risk of Incident CKD and Progression to ESRD. J Am Soc Nephrol 27, 3153–3163, https://doi.org/10.1681/ASN.2015121377 (2016).
Klatte, D. C. F. et al. Association Between Proton Pump Inhibitor Use and Risk of Progression of Chronic Kidney Disease. Gastroenterology 153, 702–710, https://doi.org/10.1053/j.gastro.2017.05.046 (2017).
Toth-Manikowski, S. & Grams, M. E. Proton Pump Inhibitors and Kidney Disease - GI Upset for the Nephrologist? Kidney Int Rep 2, 297–301, https://doi.org/10.1016/j.ekir.2017.01.005 (2017).
Wijarnpreecha, K. et al. Associations of Proton-Pump Inhibitors and H2 Receptor Antagonists with Chronic Kidney Disease: A Meta-Analysis. Dig Dis Sci 62, 2821–2827, https://doi.org/10.1007/s10620-017-4725-5 (2017).
Hung, S. C. et al. Using proton pump inhibitors correlates with an increased risk of chronic kidney disease: a nationwide database-derived case-controlled study. Fam Pract, https://doi.org/10.1093/fampra/cmx102 (2017).
Xie, Y. et al. Long-term kidney outcomes among users of proton pump inhibitors without intervening acute kidney injury. Kidney Int 91, 1482–1494, https://doi.org/10.1016/j.kint.2016.12.021 (2017).
Antoniou, T. et al. Proton pump inhibitors and the risk of acute kidney injury in older patients: a population-based cohort study. CMAJ Open 3, E166–171, https://doi.org/10.9778/cmajo.20140074 (2015).
Tang, X. & Lieske, J. C. Acute and chronic kidney injury in nephrolithiasis. Curr Opin Nephrol Hypertens 23, 385–390, https://doi.org/10.1097/01.mnh.0000447017.28852.52 (2014).
Jungers, P., Joly, D., Barbey, F., Choukroun, G. & Daudon, M. ESRD caused by nephrolithiasis: prevalence, mechanisms, and prevention. Am J Kidney Dis 44, 799–805 (2004).
Alexander, R. T. et al. Kidney stones and kidney function loss: a cohort study. BMJ 345, e5287 (2012).
Graziani, G. et al. Effect of gastric acid secretion on intestinal phosphate and calcium absorption in normal subjects. Nephrol Dial Transplant 10, 1376–1380 (1995).
Hardy, P. et al. Inhibition of gastric secretion by omeprazole and efficiency of calcium carbonate on the control of hyperphosphatemia in patients on chronic hemodialysis. Artif Organs 22, 569–573 (1998).
O’Connell, M. B., Madden, D. M., Murray, A. M., Heaney, R. P. & Kerzner, L. J. Effects of proton pump inhibitors on calcium carbonate absorption in women: a randomized crossover trial. Am J Med 118, 778–781, https://doi.org/10.1016/j.amjmed.2005.02.007 (2005).
Hansen, K. E. et al. Do proton pump inhibitors decrease calcium absorption? J Bone Miner Res 25, 2786–2795, https://doi.org/10.1002/jbmr.166 (2010).
Bo-Linn, G. W. et al. An evaluation of the importance of gastric acid secretion in the absorption of dietary calcium. J Clin Invest 73, 640–647, https://doi.org/10.1172/JCI111254 (1984).
Serfaty-Lacrosniere, C. et al. Hypochlorhydria from short-term omeprazole treatment does not inhibit intestinal absorption of calcium, phosphorus, magnesium or zinc from food in humans. J Am Coll Nutr 14, 364–368 (1995).
Negri, A. L. & Valle, E. E. Hypomagnesaemia/hypokalemia associated with the use of esomeprazole. Curr Drug Saf 6, 204–206 (2011).
Maeda, Y. et al. Does a proton pump inhibitor cause hypokalemia? Intern Med 50, 1045–1050 (2011).
Chandra, A. et al. Proton Pump Inhibitor Induced Hypokalemia. J Clin Stu 2(5) (2017).
Gilligan, S. & Raphael, K. L. Hyperkalemia and Hypokalemia in CKD: Prevalence, Risk Factors, and Clinical Outcomes. Adv Chronic Kidney Dis 24, 315–318, https://doi.org/10.1053/j.ackd.2017.06.004 (2017).
Nexium (esomeprazole magnesium) Label – FDA, https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/022101s014021957s017021153s050lbl.pdf (2014).
Protonix (pantoprazole sodium) Label – FDA, https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/020987s045lbl.pdf (2012).
Buon, M. et al. Risk of proton pump inhibitor-induced mild hyponatremia in older adults. J Am Geriatr Soc 61, 2052–2054, https://doi.org/10.1111/jgs.12534 (2013).
Kovesdy, C. P. Significance of hypo- and hypernatremia in chronic kidney disease. Nephrol Dial Transplant 27, 891–898, https://doi.org/10.1093/ndt/gfs038 (2012).
Moayyedi, P. M. et al. ACG and CAG Clinical Guideline: Management of Dyspepsia. Am J Gastroenterol 112, 988–1013, https://doi.org/10.1038/ajg.2017.154 (2017).
Chey, W. D., Leontiadis, G. I., Howden, C. W. & Moss, S. F. ACG Clinical Guideline: Treatment of Helicobacter pylori Infection. Am J Gastroenterol 112, 212–239, https://doi.org/10.1038/ajg.2016.563 (2017).
Hunt, R. et al. World Gastroenterology Organisation Global Guidelines: GERD Global Perspective on Gastroesophageal Reflux Disease. J Clin Gastroenterol 51, 467–478, https://doi.org/10.1097/MCG.0000000000000854 (2017).
Alatawi, Y. M. & Hansen, R. A. Empirical estimation of under-reporting in the U.S. Food and Drug Administration Adverse Event Reporting System (FAERS). Expert Opin Drug Saf 16, 761–767, https://doi.org/10.1080/14740338.2017.1323867 (2017).
Maciejewski, M. et al. Reverse translation of adverse event reports paves the way for de-risking preclinical off-targets. Elife 6, https://doi.org/10.7554/eLife.25818 (2017).
Prevacid (lansoprazole) Label – FDA, https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/020406s078-021428s025lbl.pdf (2012).
Dexilant (dexlansoprazole) Label – FDA, https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/022287s014lbl.pdf (2012).
Aciphex (rabeprazole) Label – FDA, https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/020973s035204736s005lbl.pdf (2014).
Reimer, C., Søndergaard, B., Hilsted, L. & Bytzer, P. Proton-pump inhibitor therapy induces acid-related symptoms in healthy volunteers after withdrawal of therapy. Gastroenterology 137(80–87), 87.e81, https://doi.org/10.1053/j.gastro.2009.03.058 (2009).
Niklasson, A., Lindström, L., Simrén, M., Lindberg, G. & Björnsson, E. Dyspeptic symptom development after discontinuation of a proton pump inhibitor: a double-blind placebo-controlled trial. Am J Gastroenterol 105, 1531–1537, https://doi.org/10.1038/ajg.2010.81 (2010).
Acknowledgements
We thank Dr. Rabia Atayee for stimulating discussions and help with the project. We also thank Chris Edwards and Da Shi for contributions to processing the FAERS/AERS data files and supporting the computer environment.
Author information
Authors and Affiliations
Contributions
T.M. performed the experiments, R.A., L.A. and T.M. designed the study and, T.M., I.C., L.A. and R.A. drafted the manuscript and reviewed the final version. R.A. processed the data set.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Makunts, T., Cohen, I.V., Awdishu, L. et al. Analysis of postmarketing safety data for proton-pump inhibitors reveals increased propensity for renal injury, electrolyte abnormalities, and nephrolithiasis. Sci Rep 9, 2282 (2019). https://doi.org/10.1038/s41598-019-39335-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-39335-7
This article is cited by
-
Time-dependent association between omeprazole and esomeprazole and hospitalization due to hyponatremia
European Journal of Clinical Pharmacology (2023)
-
Proton pump inhibitors use and risk of incident nephrolithiasis
Urolithiasis (2022)
-
Hippocampal synaptic dysfunction and spatial memory impairment in omeprazole-treated rats
Metabolic Brain Disease (2022)
-
Proton pump inhibitors and osteoporosis risk: exploring the role of TRPM7 channel
European Journal of Clinical Pharmacology (2022)
-
Efficacy and safety of the Chinese herbal formula Hewei Jiangni recipe for NERD with cold-heat complex syndrome: study protocol for a double-blinded randomized controlled trial
Trials (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.