Abstract
In this study we investigated whether the metabolomic analysis could identify a specific fingerprint of coronary blood collected during primary PCI in STEMI patients. Fifteen samples was subjected to metabolomic analysis. Subsequently, the study population was divided into two groups according to the peripheral blood neutrophil-to-lymphocyte ratio (NLR), a marker of the systemic inflammatory response. Regression analysis was then applied separately to the two NLR groups. A partial least square (PLS) regression identified the most significant involved metabolites and the PLS-class analysis revealed a significant correlation between the metabolic profile and the total ischemic time only in patients with an NLR > 5.77.
Similar content being viewed by others
Introduction
Worldwide, coronary artery disease (CAD) is the single most frequent cause of death. In particular, the in-hospital mortality of ST-elevation myocardial infarction (STEMI) patients in European Society of Cardiology (ESC) countries varies between 6% and 14%, and the 6-month mortality remains at approximately 12%, with higher mortality rates in high-risk patients1.
Endothelial dysfunction and inflammation play a major role in the pathophysiology of acute coronary syndromes. Although their roles are not completely defined, they are especially important in plaque rupture, plaque erosion, and subsequent thrombus formation2. The endothelium is known to be involved in the modulation of vasoactive substances and platelet aggregation. For its part, inflammation can alter the function of endothelial cells, acting as a modulator of atherosclerotic risk factors in the impairment of arterial biology3. In this regard, the neutrophil-to-lymphocyte ratio (NLR) has recently been validated as a reliable inflammatory marker of atherosclerosis and as a predictor of clinical outcome in patients with various cardiovascular diseases4.
Furthermore, over the last ten years the use of targeted and non-targeted metabolomic approaches has allowed the identification of specific metabolic profiles for several cardiovascular diseases5,6,7, including CAD8. However, a limited number of studies have been conducted in patients with an STEMI9,10, and none have performed an analysis of coronary artery blood.
In this study, we report the preliminary findings of a metabolomic analysis performed on coronary artery blood collected during primary PCI in STEMI patients, with the aim to investigate how coronary blood fingerprint in the culprit vessels are associated with ischemic time and inflammatory state and to identify involved pathways.
Results
Coronary angiography
Patients were subjected to primary PCI with a median coronary ischemic time of 180 min (95% CI: 120–330 min). The culprit lesions were localized as follows: right coronary artery N = 6, left main/left anterior descending artery N = 5, and circumflex branch N = 4. Of the 15 coronary stents used, 12 were drug-eluting stents (5 with zetarolimus and 7 with everolimus) and 3 were bioresorbable vascular scaffold stents. Heparin (100 UI/kg, maximum dose 5000 UI) was administered intravenously before the procedure in all patients. The glycoprotein IIb/IIIa inhibitor abciximab was used in 14 patients.
Metabolomics analysis
Two patients were excluded from the final analysis because of the use of a different contrast agent.
After an unsupervised Principal Component Analysys (PCA) to visualize possible metabolic differences among the groups and to identify potential outliers, we performed a partial least square (PLS) regression (Fig. 1) using total coronary ischemic time (the time from symptom onset until reperfusion) as the Y variable, achieving a good capacity for fitting and prediction (R2x = 0.499; R2y = 0.804; Q2 = 0.500). PLS regression is a supervised extension of PCA (Principal Component Analysis) used to maximize the correlation between two sets of variables, e.g. spectral intensity values (X matrix) and ischemic time (Y matrix), so that the response variable Y can be predicted from X. The estimated predictive power of the model is expressed by R2Y and Q2Y, which represent the fraction of the variation of Y-variable and the predicted fraction of the variation of Y-variable, respectively. A good prediction model is achieved when Q2 > 0.5.
The variable interdependent parameter (VIP) analysis allowed identification of the metabolites more important in determining the culprit coronary blood fingerprint by using S-line loadings plot, which shows an increase in choline, phosphocholine, orthinitine and myo-inositol concentrations as the ischemic time increases, while lysine and 2-phosphoglycerate levels decrease.
To evaluate the effects of inflammation in modulating the endothelial response, we divided the population into two groups on the basis of the NLR, using a cut-off of 5.774, into a high NLR group (N = 6) and a medium-low NLR group (N = 7). The two NLR groups showed statistically significant differences with regard to NLR (8.09 ± 1.83 vs 3.86 ± 1.62; p = 0.01) and to anthropometrics data (Height: 165 ± 4.6 cm vs 173 ± 4.86 cm, p = 0.01; Weight: 66.4 ± 11.9 Kg vs 86.6 ± 8.1 Kg, p < 0.01; BMI: Kg/m2 24.1 ± 4.0 vs 28.6 ± 1.6 kg/m2, p < 0.01), with a negative correlation between NLR and BMI as highlighted in previous findings11.
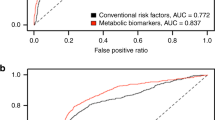
Next, we applied a PLS regression analysis separately for each group. The correlation between the metabolic pool and coronary ischemic time was not significant for the group with an NLR < 5.77. In contrast, the high NLR group showed highly significant correlations between the metabolic pool and coronary ischemic time (R2x = 0.624; R2y = 0.968; Q2 = 0.843; Fig. 2).
Discussion
The present study was designed to assess whether coronary blood fingerprint in the culprit vessels change on the basis of ischemic time and inflammatory state. Our results show that (1) coronary blood fingerprint in STEMI patients are constituted by choline, phosphocholine, myo-inositol, lysine, ornithine, and 2-phosphoglycerate and (2) a highly significant correlation was demonstrated between the metabolic pool and coronary ischemic time in patients with a high NLR, but not in those with an NLR < 5.77.
Alterations in endothelial function are the basic mechanism responsible for the development of atherosclerosis. These alterations play a key role in plaque progression and the development of plaque rupture, plaque erosion, and subsequent thrombus formation2. The metabolomic fingerprint detected in the coronary blood of our STEMI patients is characterized by a limited number of metabolites.
Choline, the immediate precursor of betaine, serves as a methyl group donor in the conversion of homocysteine to methionine and is involved in phospholipid synthesis12. In fact, choline is also a precursor of phosphocholine, another key metabolite in the metabolomic fingerprint, and an intermediate in the synthesis of phosphatidylcholine and of its derivates. Phosphocholine is the main water-soluble metabolite secreted by monocytes13 and is also the main bioactive lipid component of oxidized low density lipoprotein (LDL)14 and the major contributing factor in the atherogenic capacity of oxidized LDL15. Moreover, HDL3 subpopulations enrichment in lysophosphatidylcholine are resulted associated with deleterious biological activities during STEMI16.
Myo-inositol is an essential component of the plasma membrane that, when phosphorylated, acts as a second messenger. Myo-inositol levels are increased in mice fed a high cholesterol diet17 and in the platelets of patients with hypercholesterolemia18, suggesting its important role in arterial thrombosis19. Moreover, myo-inositol seemed to be part of the metabolic fingerprint of patients with acute coronary syndromes20.
Lysine is an essential amino acid that can negatively modulate the synthesis of nitric oxide (NO)21. In addition, ornithine is the product of the degradation of arginine by arginase. This enzyme also negatively impacts endothelial metabolism, since it degrades arginine, the precursor of NO. Higher activity of arginase II increases ornithine and reduces the production of NO, such as the inflow of lysine in endothelial cells. Higher arginase II activity has been demonstrated in the endothelial cells of patients with primary pulmonary hypertension22 and in the coronary endothelium of diabetic rats23.
2-phosphoglycerate, produced during the glycolytic process, has been shown to increase in cultured endothelial cells after the addition of LDL24 and is produced by activated macrophages in atherosclerotic lesions25, decreased as the ischemic time increases, suggesting a progressive modulation in the circulating and endothelial factors involved in the STEMI pathophysiology and a progressive impairment in energetic metabolism.
In summary, our data suggest that the systemic inflammatory state modulates the endothelial response to the occlusion, and the change of the metabolite pool becomes more intense over time. Our findings are in agreement with prior studies showing a lower patency of the infarcted artery at 60 and 90 minutes after thrombolysis in patients with neutrophilia with a relative lymphopenia26 and with studies showing a strong correlation between a high NLR and the phenomenon of no-reflow after primary PCI27. The common basis of these findings is endothelial dysfunction induced by ischemic noxa and aggravated by an imbalanced immune response, as evidenced by a high NLR.
Conclusion
Our results indicate that (1) study of the coronary metabolomic fingerprint can allow a deeper understanding of STEMI pathophysiology, identifying involved biological pathways and (2) systemic inflammation is able to modulate the endothelial response to ischemic noxa.
Study Limitations
The small number of samples included in this study is certainly a limitation, such as the lack of an independent validation cohort and our findings require validation in larger studies. Nevertheless, the statistical significance and the viability of the mechanisms suggested by the identified metabolites support the reliability of these preliminary results.
These preliminary data do not pretend to be exhaustive or conclusive, but want to stimulate further research in this direction, such as the relationship between metabolic disarrangement and no-reflow/slow-flow phenomenon or systolic function recovery after PCI.
Methods
Patients
Fifteen subjects ≥18 years of age with evidence of an STEMI according to the third universal definition of myocardial infarction28 were enrolled in the study.
The study was approved by the Azienda Ospedaliero-Universitaria di Cagliari Ethics Committee and was carried out in accordance with the Declaration of Helsinki and with approved guidelines, particularly all patients were treated according to the ESC STEMI guidelines1. Patients were informed regarding the purpose and methodology of the study, their consent was obtained and a written confirm has been collected prior to enrolment.
Exclusion criteria included previous coronary events of any type; significant (more than moderate) valvulopathy; cardiomyopathy; chronic inflammatory disease and/or cancer; and thromboembolic events or major surgery in the previous six months. Table 1 summarizes the clinical data of the study patients.
Blood samples during coronary angiography
All patients underwent coronary artery blood sampling near the culprit lesion using a micro-catheter inserted along a guide wire passed through the lesion. Blood samples were collected in heparinised tubes, immediately centrifuged at 4000 rpm for 15 min, aliquoted (800 μL) in cuvettes, and stored at −80 °C until metabolomics analysis.
Metabolomics analysis
The extraction of water-soluble metabolites from plasma samples was performed on the basis of the Folch, Lees and Sloane-Stanley procedure and has been already described in previous papers of our group29. 400 μL of plasma were dissolved in 1.2 mL of a chloroform/methanol mixture (1:1, v/v) and 175 mL of H2O. The solution was finally centrifuged at 4500 rpm and 4 °C for 30 min and ~1 mL of hydrophilic phase, containing the hydrophilic components, was separated from the lipophilic one, dried using a speed vacuum concentrator (Eppendorf, Hamburg, Germany) and then stored at −80 °C. Dried hydrophilic plasma extracts were re-dissolved in 690 μL of potassium phosphate buffer in D2O (0.1 M, pH 7.4) and 10 μL of TSP as internal standard (98 atom % D, Sigma-Aldrich, Milan). An aliquot of 650 μL was analysed by 1H-NMR.
1H-NMR experiments were conducted using a Varian UNITY INOVA® 500 spectrometer (Varian Medical Systems of Palo Alto, California, USA) operating at 499.839 MHz for protons and equipped with a 5-mm double-resonance probe (Agilent Technologies, Santa Clara, CA, USA). 1H-NMR spectra were acquired with a spectral width of 6000 Hz, a 90° pulse, an acquisition time of 2 s, a relaxation delay of 2 s, and 256 scans. A presaturation sequence was used to suppress the residual H2O signal with low power radiofrequency irradiation for 2 s. 1H-NMR spectra were imported into an ACDlab Processor Academic Edition (version 12.01, 2010, Advanced Chemistry Development, Toronto, Canada) and pre-processed with line broadening of 0.1 Hz, zero-filled to 64 K, prior to Fourier transformation. Spectra were manually phased and baseline corrected and chemical shifts referenced internally to TSP at δ = 0.0 ppm. The 1H-NMR spectra were reduced into consecutive integrated spectral regions (bins) of 0.01 ppm. Were excluded from the analysis the spectral regions between 1.87–1.99 ppm, 2.36–2.50 ppm, 3.32, 3.55 ppm, 3.68–4.14 ppm and 4.74–4.49 in order to remove the resonances of contrast agent and the effect of variation in the pre-saturation of the residual water resonance
Finally, the spectral data set was normalized to the total area and imported into the SIMCA-P + program (Version 14.0, Umetrics, Umea, Sweden). All imported data were Pareto scaled for multivariate analysis. Two 1H-NMR spectra are shown in the Electronic supplementary material.
Univariate statistical analysis
Continuous variables were compared with a non-paired t-test, and categorical variables were compared with Fisher’s exact test. A two-tailed p value < 0.05 was considered statistically significant.
References
Steg, P. G. et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 33, 2569–2619 (2012).
Kinlay, S. & Ganz, P. Role of endothelial dysfunction in coronary artery disease and implications for therapy. Am J Cardiol. 80, 11I–16I (1997).
Libby, P., Ridker, P. M., Hansson, G. K. & Leduc, Q. Transatlantic Network on Atherothrombosis. Inflammation in atherosclerosis: from pathophysiology to practice. J Am Coll Cardiol. 54, 2129–2138 (2009).
Gazi, E. et al. Prognostic Value of the Neutrophil-Lymphocyte Ratio in Patients With ST-Elevated Acute Myocardial Infarction. Clin Appl Thromb Hemost. 21, 155–159 (2015).
Deidda, M., Piras, C., Bassareo, P. P., Cadeddu Dessalvi, C. & Mercuro, G. Metabolomics, a promising approach to translational research in cardiology. IJC Metabolic and Endocrine. 9, 31–38 (2015).
Deidda, M. et al. Distinctive metabolomics fingerprint in scleroderma patients with pulmonary arterial hypertension. Int J Cardiol. 241, 401–406 (2017).
Deidda, M. et al. Metabolomic approach to profile functional and metabolic changes in heart failure. J Transl Med. 13, 297 (2015).
Deidda, M. et al. Blood metabolomic fingerprint is distinct in healthy coronary and in stenosing or microvascular ischemic heart disease. J Transl Med. 15, 112 (2017).
DeFilippis, A. P. et al. Identification of a plasma metabolomic signature of thrombotic myocardial infarction that is distinct from non-thrombotic myocardial infarction and stable coronary artery disease. PLoS One 12, e0175591 (2017).
Trainor, P. J. et al. Systems characterization of differential plasma metabolome perturbations following thrombotic and non-thrombotic myocardial infarction. J Proteomics. 160, 38–46 (2017).
Koca, T. T. Does obesity cause chronic inflammation? The association between complete blood parameters with body mass index and fasting glucose. Pak J Med Sci. 33(1), 65–69, https://doi.org/10.12669/pjms.331.11532 (2017).
Konstantinova, S. V. et al. Divergent associations of plasma choline and betaine with components of metabolic syndrome in middle age and elderly men and women. J Nutr. 138, 914–920 (2008).
Fernandez-Ruiz, I., Puchalska, P., Narasimhulu, C. A., Sengupta, B. & Parthasarathy, S. Differential lipid metabolism in monocytes and macrophages: influence of cholesterol loading. J Lipid Res. 57, 574–586 (2016).
Steinberg, D., Parthasarathy, S., Carew, T. E., Khoo, J. C. & Witztum, J. L. Beyond cholesterol. Modifications of low-density lipoprotein that increase its atherogenicity. N Engl J Med. 320, 915–924 (1989).
Matsumoto, T., Kobayashi, T. & Kamata, K. Role of lysophosphatidylcholine (LPC) in atherosclerosis. Curr Med Chem. 14, 3209–3220 (2007).
Rached, F. et al. Defective functionality of small, dense HDL3 subpopulations in ST segment elevation myocardial infarction: Relevance of enrichment in lysophosphatidylcholine, phosphatidic acid and serum amyloid A. Biochim Biophys Acta. 1851, 1254–1261 (2015).
Zha, W. et al. Metabonomic characterization of early atherosclerosis in hamsters with induced cholesterol. Biomarkers. 14, 372–80 (2009).
Shastri, K. M., Carvalho, A. C. & Lees, R. S. Platelet function and platelet lipid composition in the dyslipoproteinemias. J Lipid Res. 21, 467–472 (1980).
Holub, B. J. Metabolism and function of myo-inositol and inositol phospholipids. Annu Rev Nutr. 6, 563–597 (1986).
Teul, J. et al. Targeted and non-targeted metabolic time trajectory in plasma of patients after acute coronary syndrome. J Pharm Biomed Anal. 56, 343–51 (2011).
Kakoki, M. et al. Amino acids as modulators of endothelium-derived nitric oxide. Am J Physiol Renal Physiol. 291, F297–304 (2006).
Xu, W. et al. Increased arginase II and decreased NO synthesis in endothelial cells of patients with pulmonary arterial hypertension. FASEB J. 18, 1746–1748 (2004).
Wu, G. & Meininger, C. J. Impaired arginine metabolism and NO synthesis in coronary endothelial cells of the spontaneously diabetic BB rat. Am J Physiol. 269, H1312–H1318 (1995).
García-Heredia, A. et al. Paraoxonase-1 inhibits oxidized low-density lipoprotein-induced metabolic alterations and apoptosis in endothelial cells: a nondirected metabolomic study. Mediators Inflamm. 2013, 156053 (2013).
Sarrazy, V. et al. Maintenance of Macrophage Redox Status by ChREBP Limits Inflammation and Apoptosis and Protects against Advanced Atherosclerotic Lesion Formation. Cell Rep. 13, 132–144 (2015).
Barron, H. V., Cannon, C. P., Murphy, S. A., Braunwald, E. & Gibson, C. M. Association between white blood cell count, epicardial blood flow, myocardial perfusion, and clinical outcomes in the setting of acute myocardial infarction: a thrombolysis in myocardial infarction 10 substudy. Circulation. 102, 2329–2334 (2000).
Kurtul, A. et al. Association of lymphocyte-to-monocyte ratio with the no-reflow phenomenon in patients who underwent a primary percutaneous coronary intervention for ST-elevation myocardial infarction. Coron Artery Dis. 26, 706–712 (2015).
Thygesen, K. et al. Third universal definition of myocardial infarction. European Heart Journal. 33, 2551–2567 (2012).
Piras, C. et al. Metabolomic profile in hyperthyroid patients before and after antithyroid drug treatment: Correlation with thyroid hormone and TSH concentration. Inter J of Biochem and Cell Biol. 93, 119–128 (2017).
Author information
Authors and Affiliations
Contributions
M.D. designed the work, analysed metabolomics and clinical data, wrote the manuscript; C.P. analysed metabolomics data and wrote the manuscript; G.B. designed the work and performed patients clinical assessment; D.C. and A.P. performed patients clinical assessment and review the manuscript; A.B., F.S., A.R. and B.L. performed coronary angiography and review the manuscript; C.C.D., L.A., M.P. and G.M. supervised the study and review the data and the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Deidda, M., Piras, C., Binaghi, G. et al. Metabolomic fingerprint of coronary blood in STEMI patients depends on the ischemic time and inflammatory state. Sci Rep 9, 312 (2019). https://doi.org/10.1038/s41598-018-36415-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-36415-y
This article is cited by
-
Identification through machine learning of potential immune- related gene biomarkers associated with immune cell infiltration in myocardial infarction
BMC Cardiovascular Disorders (2023)
-
Analysis of metabolomics profile in hypothyroid patients before and after thyroid hormone replacement
Journal of Endocrinological Investigation (2021)
-
Metabolomics and psychological features in fibromyalgia and electromagnetic sensitivity
Scientific Reports (2020)
-
Metabolomic characterization of myocardial ischemia-reperfusion injury in ST-segment elevation myocardial infarction patients undergoing percutaneous coronary intervention
Scientific Reports (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.