Abstract
Locally advanced head and neck squamous cell carcinomas (HNSCC) have limited prognosis due to frequent treatment failure. Currently, TNM-classification and human papillomavirus (HPV) infection are the sole clinical prognosticators of outcome. Tumor heterogeneity and stemness based on epithelial-mesenchymal-transition reportedly associate with therapy resistance. The capacity of epithelial marker EpCAM (EpEX), stemness regulator Sox2 and mesenchymal marker vimentin to predict clinical outcome of HSNCC patients was assessed upon immunohistochemistry staining in two cohorts of HNSCC patients treated with surgery and adjuvant radio (chemo) therapy (n = 94) and primary radio (chemo) therapy (n = 94), respectively. Prognostic values with respect to overall, disease-free and disease-specific survival were assessed in uni- and multivariate cox proportional hazard models to generate integrated risk scores. EpEX, Sox2 and vimentin displayed substantial inter- and intratumoral heterogeneity. EpEXhigh and Sox2high predicted improved clinical outcome in the discovery cohort and in the HPV-negative sub-cohort. EpEXhigh and Sox2high were confirmed as prognosticators of clinical outcome in the validation cohort treated with definitive radio(chemo)therapy. Importantly, EpEXhigh identified patients with improved survival within the HPV-negative subgroup of the validation cohort. Hence, Sox2high and particularly EpEXhigh have potential as tools to predict clinical performance of HNSCC patients, foremost HPV-negative cases, in the frame of molecular-guided treatment decision-making.
Similar content being viewed by others
Introduction
Head and neck squamous cell carcinomas (HNSCC) are typically induced by carcinogenic components of alcohol and tobacco or -primarily for oropharyngeal carcinomas- through infection with high-risk human papillomaviruses (HPV)1,2. Currently, three separate HPV-negative and further two biologically differing HPV-positive subtypes of HSNCC can be distinguished2. Despite aggressive treatment, HNSCC display dismal 5-year overall survival (OS) and disease-free survival (DFS) rates of less than 45%3. The clinical outcome including OS and DFS strongly depends on tumor size, locoregional spread, resection margins, extracapsular extension (ECE), lymphovascular invasion and systemic dissemination1. Accordingly, TNM classification is an accepted prognostic factor for HNSCC that can serve to predict survival probabilities, but does not allow for a more differential, adjusted, and personalized prediction of the outcome of tumor patients with similar TNM status. More subtle differences across patients that might impact on outcome are rather neglected by merely focusing on TNM classification, hence the need for valid biomarkers. HPV-status is currently the strongest available marker identifying HPV-positive HNSCC as distinct subgroup of HNSCC with prolonged OS, which is meanwhile implemented in a new TNM classification system for p16-positive oropharyngeal carcinomas4.
Owing to a long-lasting tobacco and nicotine abuse, frequently in conjunction with alcohol abuse, and to the high mutagenic potential of these prime risk factors associated with HNSCC, the mutational burden that eventually contributes to cellular heterogeneity is very high with an average of 130 mutations per tumor5,6. Heterogeneity contributes to the emergence of aggressive and treatment-resistant cell subsets through pre-existing subpopulations in primary tumors7. Phenotypic changes along the epithelial-to-mesenchymal transition (EMT/MET) allow carcinoma cells to gradually and reversibly change phenotype from adhesive, stationary and proliferative cells (epithelial) to migratory, invasive and rather resting cells (mesenchymal)8,9,10,11. EMT is reported to increase cellular stemness, provide invasive features required for tumor progression, and enhance treatment resistance9,11,12. Accordingly, tumor-initiating cells in HNSCC can adopt either an epithelial/proliferative (E-type) or a mesenchymal/migratory (M-type) phenotype, where M-type cells within HNSCC cell lines and primary tumors bear enhanced therapeutic resistance13,14. However, a strict reliance of carcinoma cells on EMT to progress through the metastatic cascade and become treatment-resistant has been challenged in some entities such as pancreatic and lung cancers15,16. Accordingly, the central role of EMT in cancer progression has been intensely and controversially discussed in recent years9,17,18.
In the present study, we analyzed the expression levels and patterns of EpCAM, Sox2 and vimentin in primary HNSCC for association with patient outcome. EpCAM is an epithelial cell marker involved in regulation of proliferation and stem cell differentiation19,20,21,22. EpCAM down-regulation in mesodermally differentiating embryonic stem cells that undergo EMT is an early and necessary event in gastrulation22, which is likewise observed in partial EMT occurring in cancer cells23,24,25,26,27,28. Sex-determining region Y-box 2 (Sox2) is a transcription factor required for stem cell pluripotency and reprograming of somatic cells to induced pluripotent stem cells29. Owing to amplification on chromosome 3q26, Sox2 is frequently over-expressed in carcinomas including HNSCC30. Vimentin is an intermediate filament expressed by mesenchymal cells and carcinoma cells that have undergone EMT, which is involved in the regulation of cell motility and invasion31.
On the basis of protein expression patterns, we have defined high expression of Sox2 (Sox2high) and of EpCAM (measured using antibodies against the extracellular domain EpEX; EpEXhigh) as prognostic factors for improved clinical outcome of HNSCC. EpEXhigh was a significant prognostic factor for overall, disease-free and disease-specific survival in HPV-negative patients of two independent cohorts with fundamentally different clinical treatment. Hence, Sox2high and particularly EpEXhigh represent promising tools for improved stratification of HNSCC and, thus, for alternative therapeutic decision-making for patients with similar TNM status.
Results
EpEX, Sox2 and vimentin expression in the discovery HNSCC LMU cohort
Expression of epithelial marker EpCAM (detected with antibodies specific for the extracellular domain EpEX), transcription factor Sox2 and mesenchymal marker vimentin was evaluated in consecutive kryo-conserved serial sections (5 µm) of biospecimens of the retrospective LMU cohort (Table 1, upper part, and Supplementary Table 1). EpCAM and vimentin mRNA levels are major determinants of epithelial differentiation and partial EMT in HNSCC, as was recently reported using single cell RNA-sequencing data32. Therefore, EpCAM and vimentin proteins represent a pair of potential markers for EMT in HNSCC, which should have opposing expression patterns in tumors.
Vimentin-expressing cells in the interstitium and infiltrating non-tumor cells were excluded from the analyses based on their morphology combined with intense and homogeneous antigen expression. EpEX, Sox2 and vimentin were heterogeneously expressed in tumors, ranging from no expression (0), weak (1+), intermediate (2+), to strong expression (3+) and in normal mucosa (Fig. 1a–c). In normal mucosa, EpEX and Sox2 were expressed in cells of the stratum basale and stratum parabasale only, and Sox2 expression did not exceed an intermediate (2+) level (Fig. 1a,b). Vimentin expression in normal mucosa was restricted to infiltrating mesenchymal cells and was up-regulated in tumor-adjacent mucosa with hyper- and/or dysplastic cells (Fig. 1c).
EpEX, Sox2 and vimentin expression in HNSCC and normal mucosas. (a–c) Shown are examples of EpEX (a), Sox2 (b) and vimentin (c) expression ranging from no (0), weak (1), intermediate (2) to strong (3) in HNSCC (upper panels; 200×), normal mucosas and tumor-adjacent mucosas (lower panels; 100×). EpCAM, Sox2 and vimentin staining is red-brown, nuclei and cytoplasm are counter-stained with hemalaun (blue). (n/d.: not detected). Tu: tumor; Int: interstitium. (d) Upper: IHC scores of EpEX, Sox2 and vimentin expression in normal mucosas, tumor-adjacent mucosas and HNSCC are displayed as violin plots including median (open circle), 1st and 3rd interquartile range, minima and maxima, and kernel density estimation. p-values are derived from unpaired Mann-Whitney testing. Lower: IHC scores of EpEX, Sox2 and vimentin expression in HPV-positive and –negative HNSCC are displayed as violin plots including median (open circle), 1st and 3rd interquartile range, minima and maxima, and kernel density estimation (n/d: not determined). P-values are derived from paired Student´s T-test following confirmation of normal distribution of data (Levene test).
IHC scores, representing intensity and frequency of antigen expression from two to four sections of biospecimen, ranged from 0–300 with various combinations of intensities and percentages for all three antigens (Supplementary Table 1). Comparison of normal mucosa, tumor-adjacent mucosa, and tumors disclosed a strong and highly significant (p < 0.0001) up-regulation of EpEX in tumors with median IHC scores of 220 versus 60 and 50 in tumor-adjacent and healthy mucosa, respectively (Fig. 1d). Sox2 expression was strongly and highly significantly (p < 0.0001) up-regulated in tumors versus normal and tumor-adjacent mucosa (median IHC score of 150 in tumors versus 0 in normal and tumor-adjacent mucosa), whereas vimentin expression showed a moderate induction in tumor-adjacent mucosa and tumors as compared to normal mucosa (p < 0.0001) (Fig. 1d).
An association of EpEX and Sox2 IHC scores with HPV-status was observed, where increased expression levels were shown for both in HPV-positive HNSCC (Table 1 and Fig. 1d). Vimentin did not show any HPV-associated difference in expression (Fig. 1d).
EpEX, Sox2 and vimentin expression patterns in HNSCC
Two major and two minor tumor expression patterns of EpEX, Sox2 and vimentin were observed in the LMU cohort: High expression of EpCAM and Sox2, but lack of vimentin expression (EpEX/Sox2+/vimentin− 43.01%), high expression of all three antigens (EpEX/Sox2/vimentin+ 35.48%), high expression of EpCAM and vimentin, but lack of Sox2 expression (EpEX/vimentin+/Sox2− 7.53%) and high expression of EpCAM, but lack of Sox2 and vimentin expression (EpEX+/Sox2/vimentin− 3.23%). Representative staining of all four major expression patterns on consecutive sections of tumor samples are shown in Fig. 2a. Significant positive correlation of Sox2 with EpEX (Fig. 2b; rho = 0.41, p-value < 0.001) and a trend for a weak, negative correlation of Sox2 with vimentin was found (Fig. 2b; rho = −0.19, p-value = 0.062). Hence, epithelial marker EpCAM showed co-expression with reprogramming factor Sox2, but mesenchymal marker vimentin was independent from EpCAM expression and its expression negatively related to that of Sox2.
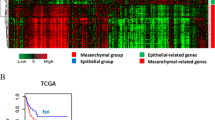
EpEX, Sox2 and vimentin expression patterns in HNSCC. (a) Examples of the major four expression patterns of EpEX, Sox2 and vimentin are shown with according frequencies in percentages. All antigen-specific staining (200×) in consecutive sections are depicted in red-brown, while nuclei and cytoplasm are counter-stained with hemalaun (blue). Tu: tumor; Int: interstitium. (b) IHC scores of EpEX, Sox2 and vimentin for HNSCC (n = 94) were plotted and displayed with linear regression curves, p-values and Spearman’s rank rho coefficient. (c) mRNA expression level z-scores for EpCAM, Sox2 and vimentin from The Cancer Genome Atlas (TCGA) HNSCC cohort (n = 279) were downloaded at cBioPortal and were depicted as an expression heat-map. Spearman correlation analysis results with rho coefficient and p-values are indicated. (d) EpEX, Sox2 and vimentin expression in serial sections of HNSCC is depicted (400×). Examples of tumor cells with reduced EpCAM and increased vimentin expression are numbered (1 to 5). (e) Simultaneous immunofluorescence staining of EpEX and vimentin are visualized in confocal laser scanning microscopy for EpEX (green), vimentin (red) and as a merged image (combined colors). Nuclear DNA is stained in blue with DAPI. The margin between tumor and interstitium, and enlarged areas are marked as doted lines and solid squares. Cells with loss of EpCAM and gain of vimentin expression are marked with white arrows. Left panel: Depicts the edge of a tumor area; center panel: depicts vimentin-positive tumor cells at the edge of a tumor area; Right panel: depicts a small tumor island surrounded by interstitium, and rightmost panel: depicts two carcinoma cells demonstrating the co-localization of EpCAM+/vimentin− and EpCAM−/vimentin+ cells at the border to the interstitium.
In order to further study the correlation of EpCAM, Sox2 and vimentin at the transcriptional level, mRNA expression data from HNSCC patients (n = 279) included in The Cancer Genome Atlas (TCGA) cohort were analyzed5. TCGA data confirmed a strong positive and significant correlation of EpCAM and Sox2 expression (rho = 0.64, p < 0.001). Furthermore, EpCAM and Sox2 negatively correlated with vimentin expression with rho = −0.25 (EpCAM, p < 0.001) and rho = −0.26 (Sox2, p < 0.001) values, respectively (Fig. 2c). Stratification according to the HPV-status (HPV-negative = 243 cases; HPV-positive = 36 cases) disclosed no correlation of EpCAM mRNA expression with HPV infection, whereas Sox2 and vimentin correlated positively (Mann-Whitney p-value = 7.9E-05) and negatively (Mann-Whitney p-value = 0.04008), respectively. Correlation of antigen expressions were only addressed in HPV-negative samples, owing to the limited number of HPV-positive specimen. EpCAM and Sox2 positively correlated (rho = 0.633, p-value < 2.2E-16), EpCAM and vimentin negatively correlated (rho = −0.267, p-value = 2.5E-05), and Sox2 and vimentin negatively correlated (rho = −0.25, p-value = 7.69E-05). Stratification of patients within the TCGA cohort according to tumor size disclosed higher expression of EpCAM expression in bigger tumors (T-classification 3–4 versus 1–2) (Mann-Whitney p-value = 0.013), whereas Sox2 and vimentin expression did not correlate with tumor size. No correlation was observed between the three antigens and tumor grade of differentiation. In summary, expression patterns of EpCAM and Sox2 positively correlated at the mRNA level in a large independent HNSCC patient cohort, whereas vimentin showed an inverse expression pattern compared to that of EpCAM and Sox2.
Heterogeneous expression patterns of EpEX, Sox2 and vimentin were analyzed in further detail at the single cell level using immunohistochemistry and immunofluorescence staining. Frequent co-expression and simultaneous lack of EpEX and Sox2 was confirmed (Fig. 2d). Mutually exclusive expression of EpEX and vimentin was recurrently observed at the interface of the tumor area to interstitium. EpCAMlow/-/vimentin+ cells lined up as agglomerates within tumor protrusions (Fig. 2d,e left panel) and as islands of vimentin+ cells at the edge of large tumor areas (Fig. 2e, central panel). Small islands of tumor cells separated from the major tumor area frequently showed loss of EpCAM expression at the edges, which was linked to gain of vimentin expression (Fig. 2e, right panel), itself suggestive of partial EMT within tumors. EMT-related phenotypes co-existed in HNSCC samples with single cells displaying exclusive expression of epithelial marker EpCAM adjacent to cells characterized by complete lack of EpCAM and gain of mesenchymal marker vimentin (Fig. 2e, most right panel). Such differences in intratumoral sub-localization of antigen expression is in accordance with reports from Puram et al.32, who reported on a predominant partial EMT at the leading edges of tumors. These might represent tumor cells with increased capacity of delamination and local invasion of surrounding stromal tissue, and are thus of potential clinical importance.
In order to exclude that vimentin+ cells in tumor areas represented infiltrating non-tumor cells, selected tumor specimens were stained with vimentin- and either CD31- (endothelial cells), CD68- (monocytes/macrophages), or CD90-specific antibodies (fibroblasts), respectively. Vimentin+ cells did neither express CD31 nor CD90, but vimentin/CD68+ macrophages/monocytes were detected (Supplementary Fig. 1). However, vimentin+ tumor cells were morphologically distinguishable from infiltrating, vimentin-expressing monocytes/macrophages.
Association of EpEX, Sox2 and vimentin with clinical outcome
IHC scores for each single antigen were analyzed for association with clinical endpoints, in order to define potential prognostic factors. Stratification according to HPV-status confirmed improved OS and DFS for HPV+ patients, while no statistical difference was observed with respect to DSS (Fig. 3a). Threshold optimization was applied to IHC scores of all antigens to define optimal cut-offs for each clinical endpoint. Accordingly, patients were separated into groups of antigenhigh and antigenlow expressors, i.e. if their antigen expression was above or below calculated thresholds, respectively. Optimized EpEX IHC score thresholds that maximized splits between high- and low expressors were thresholds of 146.7, 66.7, and 111.7 for OS, DFS, and DSS hazard ratios, respectively (Fig. 3b). Optimized IHC score thresholds for Sox2 were 195, 40, and 33.4 for OS, DFS, and DSS hazard ratios, respectively (Fig. 3b) and that of vimentin were 150, 150, and 17.5 for OS, DFS, and DSS hazard ratios, respectively (Fig. 3b). In the LMU cohort (n = 94) irrespective of the HPV-status, EpEXhigh patients showed significantly improved DFS and DSS rates, and a strong tendency towards improved OS. Significantly enhanced OS, DFS, and DSS were observed for Sox2high classified patients (Fig. 3b). Vimentinlow classified patients showed a trend towards improved clinical outcome (Fig. 3b). Since EpEX and Sox2 expression levels were associated with HPV-status, which is known as strong prognostic factor in HNSCC, we further assessed the association of EpEX, Sox2 and vimentin in the subgroup of HPV-negative patients of the LMU cohort (n = 47). Both, EpEXhigh and Sox2high were significantly associated with enhanced OS, DFS, and DSS in HPV-negative patients (Fig. 3c).
Association of single EpEX, Sox2 and vimentin IHC scores with clinical outcome in the LMU cohort. (a) Kaplan-Meier curves for the endpoints overall survival (OS), disease-free survival (DFS) and disease-specific survival (DSS) in HNSCC patients stratified according to HPV-status (HPV-positive versus HPV-negative). Hazard ratios (HR) with 95% confidence intervals (CI) and p-values (log-rank test) are indicated. (b,c) Kaplan-Meier curves for overall survival (OS), disease-free survival (DFS) and disease-specific survival (DSS) in HNSCC patients stratified into groups with low and high expression of EpEX, Sox2 and vimentin. Hazard ratios (HR) with 95% confidence intervals (CI), p-values (log-rank test) and the applied optimized threshold for the classification of patient subgroups are indicated for the entire cohort (b) and the HPV-negative sub-cohort (c).
Validation of the prognostic value of EpEx, Sox2 and vimentin
In order to independently analyze the prognostic value of EpEX, Sox2 and vimentin, expression levels of all three antigens were analyzed in an additional cohort of HNSCC that reflects the second major treatment regimen for HNSCC. The Göttingen validation cohort is composed of HNSCC samples (n = 94) from patients treated with definitive radio(chemo)therapy without prior surgery owing to the presence of distant metastases already at initial diagnosis or due to unresectable tumors with respect to localization and size. Accordingly, patients within the Göttingen cohort had significantly more advanced tumors than patients in the LMU cohort (pT3–4 87.2% versus 43.6%; Chi-square p-value < 2 × 10−9), significantly more frequently locoregional lymph node metastases (pN + 83.0% versus 63.8%; Chi-square p-value < 0.01), significantly more often distant metastases (pM + 10.6% versus 1.1%; Chi-square p-value 0.01), and significantly differed in localization (Chi-square p-value 0.04), but did not significantly differ in their HPV-status (Tables 1 and 2). Taken together, these unfavorable clinical parameters resulted in worse outcome of patients in the Göttingen cohort. Expression of EpEX, Sox2, and vimentin was assessed in two to four punches per biospecimen on tissue micro-arrays of the validation cohort. Given the lack of primary surgery, influence of all three antigens on clinical endpoints in the presence of primary tumors can be assessed.
HPV-status was a prognostic factor for all clinical endpoints analyzed within the Göttingen cohort (Fig. 4a). Patients classified as EpEXhigh showed significantly enhanced DFS and a trend towards improved OS and DSS. Patients classified as Sox2high showed significantly enhanced OS, DFS, and DSS (Fig. 4b). Vimentinlow classified patients showed a tendency of slightly improved outcome (OS and DSS; Fig. 4b). EpEXhigh, but not Sox2high, was a prognosticator of significantly improved OS, DFS, and DSS in the subgroup of HPV-negative HNSCC patients within the Göttingen cohort (Fig. 4c). Sox2high HPV-negative patients showed a strong trend towards enhanced DSS (p = 0.057) (Fig. 4c). Thus, EpEXhigh distinguished HPV-negative patients with improved clinical outcome in the discovery and validation cohorts.
Association of single EpEX, Sox2 and vimentin IHC scores with clinical outcome in the Göttingen cohort. (a) Kaplan-Meier curves for the endpoints overall survival (OS), disease-free survival (DFS) and disease-specific survival (DSS) in HNSCC patients stratified according to HPV-status (HPV-positive versus HPV-negative). Hazard ratios (HR) with 95% confidence intervals (CI) and p-values (log-rank test) are indicated. (b,c) Kaplan-Meier curves for overall survival (OS), disease-free survival (DFS) and disease-specific survival (DSS) in HNSCC patients stratified into groups with low and high expression of EpEX, Sox2 and vimentin. Hazard ratios (HR) with 95% confidence intervals (CI), p-values (log-rank test) and the applied optimized threshold for the classification of patient subgroups are indicated for the entire cohort (b) and the HPV-negative sub-cohort (c).
EpEX- and Sox2-based risk factor for the prediction of HNSCC clinical outcome
Since EpEX and Sox2 expression were prognostic in univariate analyses, we integrated measurements on both proteins in one multivariate cox proportional hazard model in order to calculate an integrated risk score for each patient. The cox model was fitted in the LMU cohort data (discovery cohort) followed by calculation of the risk scores and a median threshold, allowing assortment of patients into high- and low-risk. The fit coefficients and the threshold determined in the discovery cohort were used in combination with EpEX and Sox2 expressions measured in the validation cohort (Göttingen cohort) to calculate risk scores for subsequent assignment of patients of the Göttingen cohort to risk groups.
IHC scores of EpEX and Sox2 in relation to the risk score and Kaplan Meier plots are depicted for OS, DFS and DSS of the LMU cohort (Fig. 5a). Low risk score values reflected high expression levels of EpEX and Sox2, which were predictive of improved OS, DFS and DSS with hazard ratios of HR 0.44 (95% CI 0.2–0.96), 0.48 (95% CI 0.25–0.91), 0.23 (95% CI 0.05–1.13), and significant p-values (p = 0.034; p = 0.02; p = 0.048), for OS, DFS and DSS, respectively (Fig. 5a). The integrated risk score was furthermore prognostic for HPV-negative patients within the LMU cohort with respect to endpoints OS and DFS (Fig. 5a). In order to validate the risk score, we transferred the prognostic model that was developed using LMU data to data on the Göttingen cohort. Similarly, low risk score was associated with improved OS and DFS in the Göttingen cohort, thus confirming its prognostic power (Fig. 5b). However, the integrated risk factor was not prognostic for HPV-negative patients within the Göttingen cohort (Fig. 5b).
Risk factor as a prognosticator for HNSCC. (a,b) Optimized thresholds for Sox2 and EpEX IHC scores were implemented in an integrated risk factor to predict the clinical outcome of HSNCCs. Shown is a heat-map representation of the composition of the risk factor across HNSCC patients of the LMU cohort (a; n = 94) and the Göttingen cohort (b; n = 94). Additionally, both cohorts were subdivided into HPV-negative sub-cohorts (right panels). Stratification of patients was conducted according to the SEV-factor into high and low scores. Overall survival (OS), disease-free survival (DFS) and disease-specific survival (DSS) are depicted as Kaplan-Meier curves with hazard ratio (HR) at indicated 95% confidence interval (CI) and log-rank test p-values.
In a second set of analysis, the cox model was fitted within the HPV-negative LMU cohort data followed by calculation of the risk scores and a median threshold, allowing assortment of patients into high- and low-risk in the entire LMU cohort. IHC scores of EpEX and Sox2 in relation to the risk score and Kaplan Meier plots are depicted for OS, DFS and DSS of the LMU cohort (Fig. 6a). Low risk values (i.e. high levels of EpCAM and Sox2 in the HPV-negative LMU cohort) were predictive of improved DFS and DSS (HR 0.51, 95% CI 0.28–0.99, p = 0.043; HR 0.19, 95% CI 0.04–0.91, p = 0.02, respectively). Furthermore, low risk values had a tendency to predict improved OS, however results were not statistically significant (HR 0.51, 95% CI 0.24–1.1, p = 0.08).
Risk factor as a prognosticator for HNSCC. (a–c) Optimized thresholds for Sox2 and EpEX IHC scores were implemented in an integrated risk factor to predict the clinical outcome of HSNCCs based on HPV-negative patients of the LMU cohort. Overall survival (OS), disease-free survival (DFS) and disease-specific survival (DSS) are depicted as Kaplan-Meier curves with hazard ratio (HR) at indicated 95% confidence interval (CI) and log-rank test p-values for the entire LMU cohort (a), Göttingen cohort (b), and the pooled LMU and Göttingen cohort (c).
The fit coefficients and the threshold determined in the HPV-negative discovery cohort (LMU cohort) were transferred to the entire validation cohort (Göttingen cohort) to calculate risk scores for subsequent assignment of patients to risk groups (Fig. 6b). Low risk values were predictive of improved OS, DFS and DSS (HR 0.58, 95% CI 0.34–0.99, p = 0.043; HR 0.57, 95% CI 0.35–0.94, p = 0.02; HR 0.49, 95% CI 0.25–0.97, p = 0.036, respectively). Lastly, both cohorts of HNSCC patients were pooled and stratified using the risk score generated in the HPV-negative LMU cohort. Low risk values were predictive of improved OS, DFS and DSS (HR 0.57, 95% CI 0.38–0.87, p = 0.008; HR 0.59, 95% CI 0.41–0.87, p = 0.0062; HR 0.42, 95% CI 0.24–0.75, p = 0.0021, respectively). Hence, risk scores based on EpCAM and Sox2 expression in HPV-negative HNSCC patients allow to stratify HNSCC patients independently of their HPV-status and treatment modality.
Discussion
HNSCC display outstandingly high inter- and intratumoral heterogeneity5,6 that might account for the high rate of radio(chemo)-resistance and treatment failure. Two aspects of cellular heterogeneity are considered central to tumor progression, treatment response and, thus, clinical outcome of carcinoma patients: (i) The presence of cancer stem cells (CSC) within primary tumors, which are considered the source of primary tumors, recurrences and metastatic outspread33, (ii) and phenotypic changes along the EMT, which facilitate tumor cell dissemination and metastases formation, and the induction of stemness8,9,11,12,34. One gene locus frequently affected by mutation in HNSCC is the SOX2 gene through amplification on chromosome 3q2630. Sox2 is a pluripotency factor that regulates HNSCC CSC fate through a PI3K/mTOR/Sox2/ALDH axis, which generates a tumor-initiating population with the capacity for asymmetric division and proliferation35. Furthermore, Sox2 fosters an epithelial phenotype in lung cancer, which has an etiology comparable to HNSCC with respect to risk factors, through enhanced transcription of the pan-carcinoma marker EpCAM36. In line with this concept, loss of Sox2 expression in HNSCC resulted in up-regulated vimentin expression and migration, and reduced overall and progression-free survival30. Induction of EpCAM results in various cellular outcome including cell-cell adhesion37, enhanced tumor cell proliferation19,38 and regulation of stem cell features20,39,40,41. Itself, EpCAM is prone to substantial regulation throughout cancer progression27,42,43, stem cell differentiation22, and during EMT related to treatment resistance, e.g. in prostate cancer26. Loss of EpCAM in mesodermally differentiating embryonic stem cells (ESC) during gastrulation of mouse embryos is an early event initiating at E7.022. The resulting spatiotemporal patterning of EpCAM, with retention in endodermal but complete loss in mesodermal tissue, is mandatory for the completion of ESC differentiation22. Hence, loss of EpCAM in EMT and, generally, in mesenchymal differentiation is not only concomitant, but appears causal.
For the case of HNSCC, single cell RNA-sequencing data confirmed high inter- and intratumoral heterogeneity amongst tumor cells, but far less in associated stromal and immune cells32. Analysis of single cell transcriptomes allowed to extract cell signatures defining cell cycle progression, hypoxia, cell stress, and epithelial and mesenchymal differentiation statuses in HNSCC32. The latter two signatures were inversely correlated and characterized, amongst others, by high-level EpCAM and vimentin/slug expressions, respectively. Hence, EpCAM represents an excellent measure for the level of epithelial differentiation of carcinoma cells in head and neck tumors, whereas vimentin depicts a gradual mesenchymal switch. These molecular networks with reported functionality in tumor progression and treatment resistance prompted us to investigate protein co-expression levels and patterns of Sox2, EpCAM and vimentin in HNSCC. For all three antigens, inter- and intratumoral heterogeneity was observed, which translated into different clinical outcome. Low expression of Sox2 significantly correlated with poor OS, DFS and DSS in an univariate analysis within our discovery cohort, which is confirmatory of Bayo et al.30. Similarly, Chung et al. and Bochen et al. reported on a positive prognostic value of high-level expression of Sox2 in HNSCC44,45. However, contradicting results have been reported too, such that HNSCC patients with high-level Sox2 expression were characterized by poorer outcome46, as well as a complete lack of prognostic value of Sox2 in HNSCC47. Our own findings clearly are in support of a beneficial effect of high-level Sox2 expression on clinical outcome.
Low expression of epithelial marker EpCAM significantly correlated with decreased DFS and DSS (univariate). These findings contradict the reported poor prognosis of breast, colorectal, pancreatic, ovarian and bladder cancers over-expressing EpCAM48,49,50,51,52,53,54,55,56, but is in line with the association of high levels of EpCAM with improved prognosis of colonic, gastric and renal cancer57,58,59. We further confirmed our findings in a validation cohort composed of biospecimen obtained from HNSCC patients treated with primary radio(chemo)therapy. Limitations must be noted, as patients within the validation cohort were characterized by the presence of significantly larger tumors and generally more advanced disease, including increased locoregional and distant metastases (Table 2). Expectedly, these patients were confronted with substantially poorer outcome than patients included in the LMU cohort. Furthermore, EpCAM expression was assessed with two distinct monoclonal antibodies with slightly differing binding affinities (Vu1D9 > Ber-Ep4; own unpublished data), which might affect the quantification of antigen levels and explain generally lower levels of EpCAM in the Göttingen cohort. Nonetheless, EpCAM and Sox2 possessed prognostic value, even under these testing conditions and in the presence of the primary tumor throughout the observation period (Göttingen cohort). Hence, we could show that EpEXhigh and Sox2high are prognosticators of improved clinical outcome in two independent, retrospective clinical cohorts despite limitations and challenges arising from differing clinical cohorts and staining procedures. Both cohorts cover both major clinical treatment modalities and staining procedures (cryopreserved native samples versus FFPE routine staining), and should as such allow for more generalized findings.
Generally, our findings suggest that an epithelial, proliferative Sox2high/EpCAMhigh phenotype of HNSCC could foster survival, which might be based on enhanced therapy response. Oppositely, loss of epithelial traits during partial EMT, as measured by EpCAM reduction and gain in vimentin32, might be associated with decreased proliferation and increased migration, or primarily with increased treatment resistance as demonstrated for prostate, pancreatic, breast cancer and HNSCC15,16,26,32. Both features can promote reduced radio(chemo)sensitivity and increased local invasion, which represent potential sources of recurrence and locoregional spread, which is a common and frequent feature of HNSCC1.
HPV infection is an accepted clinical factor for HNSCC60 that predicts improved outcome and has been implemented in the AJCC 8th edition of the TNM classification of patients4,61. Although HPV-status as such is an important stratificator it is currently only used to distinguish two separate HNSCC entities for diagnostic/prognostic purposes, while its actual use for therapeutic stratification in routine remains under investigation in several clinical studies (RTOG 3311, NRG HN002). Furthermore, it currently leaves HPV-negative HNSCC patients without any further stratification options except for the TNM status and extracapsular extension. In this respect, EpEXhigh qualifies as a candidate to stratify HPV-negative HNSCC into further prognostic groups. In fact, HPV-negative patients with high levels of EpCAM displayed improved survival rates for all tested clinical endpoints that were similar to that of the HPV-positive subgroup. Thus, EpEXhigh bears the potential as a prognostic biomarker for HPV-negative HNSCC patients.
In a further step, we combined EpEX and Sox2 levels in an integrated risk factor. We deliberately did not include HPV as a parameter in the risk model owing to its impact as a strong prognostic factor in HNSCC, which might result in a risk factor that predicts HPV rather than survival. This is demonstrated by a very strong association (p < 10−12, not HPV-stratified LMU cohort, p < 2.2−16 not HPV-stratified Göttingen cohort, Fisher’s exact test) of HPV status with the risk factor generated including HPV-status and a much weaker association when not including HPV (p = 0.17, not HPV-stratified LMU cohort, 0.045 not HPV-stratified Göttingen cohort, Fisher’s exact test). In contrast, we were aiming to test whether EpCAM and Sox2 in combination are able to predict survival independent of HPV. Both EpCAM and Sox2 are only weakly associated with HPV status in the LMU cohort but not in the Göttingen cohort (p-values LMU: EpCAM 0.01, Sox2: 0.02, Göttingen: EpCAM 0.36, Sox2: 0.12). This suggests that Sox2 and EpCAM expressions are somewhat but not strongly influenced by HPV, and hence are not a strong proxy of the HPV status. Consequently, we assumed that a risk score integrating Sox2 and EpCAM but not HPV should be able to predict clinical outcome independently of HPV. In fact, the integrated risk score that combined measurements on Sox2 and EpEX expression levels significantly predicted outcome with respect to OS, DFS and DSS in both non-HPV stratified cohorts. Sox2high/EpEXhigh defined patients with better outcome, both, after standard therapy involving surgery and adjuvant radio-chemotherapy, as well as after primary radio(chemo)therapy in the absence of prior surgical tumor resection. Both therapeutic strategies represent the two major treatment regimens and, thus, the risk score is applicable to the majority of clinical HNSCC cases. Additionally, Sox2 and EpCAM are common antigens for the automated staining of formalin-fixed, paraffin-embedded specimen, which would allow for comparably simple assessment in clinical routine. It must be noted that the integrated risk score was characterized by hazard ratios and p-values similar to univariate analyses of EpEX and Sox2 in both cohorts. However, although the integrated risk score does not outperform single EpEX and Sox2 scores with respect to prognostic power, implementing two or even more independent measurements within one risk score could contribute to improve the reliability of prognosis and ease handling of otherwise singular score values in clinical routine.
Additionally, in order to rule out a contribution of the HPV-status to the risk score, the cox model to determine thresholds for optimized stratification splits was fitted within the HPV-negative patients of the discovery cohort. The determined risk scores were then applied to the entire discovery and validation cohorts as well as to a pooled cohort composed of both separate cohorts. By doing so, we demonstrated that risk scores based on EpCAM and Sox2 expression generated in HPV-negative patients have the potential to predict clinical endpoints such as OS, DFS, and DSS independently of the HPV-status of the patient and of differential treatment regimens.
The integrated risk score could be assessed from pre-operative biopsies at the time point of first diagnosis and serve as an additional molecular parameter. Together with other clinical parameters such as resection margins and extracapsular extension, it could help to identify high-risk situations and, thus, the need for intensification of multimodal therapy.
In summary, the integrated risk factor, and EpEXhigh more specifically, presented herein have the potential to contribute to improve HNSCC stratification of HNSCC patients, including HPV-negative cases, and might open novel options for therapy decisions.
Methods
Human biospecimen
Biospecimen are reported according to BRISQ and REMARK standards62. The Ludwig-Maximilians-University of Munich (LMU) cohort (discovery cohort) is composed of 94 patients with HNSCC of whom tumor biomaterial has been collected. The cohort comprises primary tumors (n = 81), recurrences (n = 3), residual carcinoma (n = 1) and secondary carcinomas of the head and neck (n = 9). Furthermore, distant normal mucosa and tumor-adjacent normal mucosa were available for 87 and 19 of these patients, respectively. Patients were treated with surgery and adjuvant radio(chemo)therapy upon indication. Age, sex, tumor localization, smoking habits, TNM and p16 status, as a surrogate marker for HPV infection63,64, are compiled in Table 1. P16 status will be referred to as HPV-status in the following. The most prevalent HNSCC subgroup within the cohort comprised oropharyngeal squamous carcinomas (57.4%), with 30.9% HPV-positive samples, thus conforming to overall frequencies worldwide65. All patients of the LMU cohort received surgical treatment and adjuvant radiotherapy (radiation doses: 50.4–70 Gy; mean 63.07 Gy; median 64.0 Gy; three patients obtained increased doses up to 70 Gy based on clinical requirements such as uncertain resection margins with residual tumor in situ) with or without simultaneous chemotherapy. Most patients received cisplatin/5-fluorouracil (CDDP/5-FU). In selected cases, mitomycin C (MMC), 5-FU/MMC, or Cetuximab replaced platin-based chemotherapy. Macroscopically normal mucosa was obtained after surgical removal of the primary tumor beyond the resection margins with >5 mm distance to the initial tumor bed. Tumor-adjacent mucosa was defined as areas of histologically normally structured but hyper- to dysplastic epithelium in the close vicinity of tumor fields. All biospecimens were stabilized through embedment in tissue-Tek® (Sakura, Finetek, The Netherlands), snap-frozen in liquid nitrogen, and preserved at −80 °C before further processing.
The Göttingen cohort (validation cohort) is composed of 94 patients with HNSCC, who received definitive radiotherapy with or without simultaneous chemotherapy. The cohort comprises 94 primary tumors. Age, sex, tumor localization, smoking habits, TNM and p16 status are compiled in Table 1. Intended total radiation dose in this primary setting was 70.0 and 66.0 for 87 and 7 patients, respectively. Complete radiation as planned was administered in 85 individuals (90.4%); total dose was reduced in six patients by <10.0 and in three by 10.0–20.0 Gy due to medical reasons or according to patient willingness. Concomitant chemotherapy was given in 75 out of the 94 patients of whom 41 received 5-FU/MMC, 30 cisplatin as single agent, and four received Cetuximab. Biospecimens of the Göttingen cohort were formalin-fixed and paraffin-embedded before processing as tissue microarrays.
Immunohistochemistry and immunofluorescence staining
Immunohistochemistry intensity scores (IHC score) were calculated as the product of intensity (0 to 3 +) and percentage of expressing tumor cells within biospecimens. IHC scores represent averages of values independently assessed by minimum two experimenters, who were blinded with respect to clinical staging and outcome of patients. Staining was analyzed separately for each individual antigen in order to preclude potential bias with respect to correlation of antigen expression. Antigen expression in the LMU cohort was assessed in 2–4 sections (≥10 × 10 mm) of primary specimens and represented average IHC scores across all entire sections considering tumor areas only. Antigen expression in the Göttingen cohort was assessed in tissue microarrays of biopsies from primary tumor specimens and represented the average of 2–4 punches of 1.5 mm diameter taken randomly from different regions within each specimen. The comparably large size of sample within the LMU cohort and the number of punches and diversity of areas for samples within the Göttingen cohort were chosen to allow for the most adequate coverage of tumor heterogeneity.
EpEX- (LMU cohort: VU1D9, Cell Signaling Technology, NEB, Frankfurt, Germany, #2929; Göttingen cohort: Ber-Ep4, Dako, Hamburg, Germany, #M080429), Sox2- (D6D9, Cell Signaling Technology, NEB, Frankfurt, Germany, #3579), vimentin- (3B4, Dako, Hamburg, Germany, #M702001), CD31- (JC70A, Dako, Hamburg, Germany, #IR61061), CD68- (KP1, Dako, Hamburg, Germany, #M081401), and CD90-specific antibodies (2Q1469, DCS Immuno Line, Hamburg, Germany, #CI921C002) were used for immunohistochemistry and immunofluorescence detection of antigens. Immunostaining was performed using the avidin-biotin-peroxidase method (Vectastain, Vector laboratories, Burlingame, CA, USA) according to the manufacturers’ protocol. For immunofluorescence, Alexa Fluor®−488- and Alexa Fluor®−594-conjugated secondary antibodies were used to visualize specific primary antibodies. Laser scanning confocal microscopy images were recorded with a TCS-SP5 system (Leica Microsystems; Wetzlar, Germany).
Clinical endpoints and survival analysis
Overall survival (OS), disease-free survival (DFS) and disease-specific survival (DSS) were chosen as clinical endpoints. We calculated OS (months) from the date of diagnosis to death due to any cause, DFS to the first observation of any recurrence or death, and DSS to the date of HNSCC-related death. In the absence of an event, patients were censored at the date of the last follow-up visit.
Data analysis was performed in R (R Core Team, R: A Language and Environment for Statistical Computing, R Foundation for Statistical Computing, 2017; version 3.4.0) in combination with R-survival package (CRAN). For univariate analysis, the IHC expression scores were included into cox-proportional hazard models after binarization into high- and low expressors. The threshold for binarization was the value picked from the whole range of expression scores that resulted in a maximum split of high- and low-expressors with regard to hazard-ratio. In order to prevent artificially extreme hazard-ratios resulting from very small groups only thresholds were allowed that split patients in groups containing at least 5 patients. Hazard ratios, 95% confidence interval ratios, median survival times and log-rank p-values were calculated and included in Kaplan-Meier plots. In order to generate prognostic models integrating EpEX and Sox2, in a first step a multivariate model was built with the continuous expression values of the two proteins included as covariates. The resulting fit coefficients were extracted from the model and multiplied with the appropriate expression values of each patient before building the sum, which was then used as risk score. The risk scores were binarised into high- and low-risk by a threshold that was maximized for hazard-ratio as described above. Hazard ratios, 95% confidence interval ratios, median survival times and log-rank p-values were calculated and included in Kaplan-Meier plots along with distribution plots of risk scores and expression heatmaps. Statistical tests for all figures are justified as appropriate. Visual inspection of distribution shapes of comparison groups revealed no obvious differences. Normality was tested with the Kolgomorov-Smirnov test and assumptions for the test were met. Equal variances between the groups were tested using the Levene test with no differences observed.
Analysis of the TCGA HNSCC cohort
The results are based upon data generated by the TCGA Research Network: http://cancergenome.nih.gov. mRNA expression level z-scores for EpCAM, Sox2 and Vimentin were downloaded for the Nature published HNSCC TCGA cohort (n = 279) at cBioPortal5,66,67. Spearman correlation analyses of mRNA expression z-scores were performed, and results were considered statistically significant when p < 0.05.
Ethics approval and consent to participate
All clinical samples were obtained after written informed consent during routine surgery or biopsy based on the approval by the ethics committee of the local medical faculties (Ethikkomission der Medizinischen Fakultät der Ludwig-Maximilians-Universität; #087-03; #197-11; #426-11; Ethikkomission der Medizinischen Fakultät der Universität Göttingen; #7/4/2012) and in compliance with the WMA Declaration of Helsinki and the Department of Health and Human Services Belmont Report.
Availability of Data and Material
Data availability is restricted as required by the ethics obligations and relevant medical and legal issues.
References
Leemans, C. R., Braakhuis, B. J. & Brakenhoff, R. H. The molecular biology of head and neck cancer. Nat Rev Cancer 11, 9–22, nrc2982 (2011).
Keck, M. K. et al. Integrative analysis of head and neck cancer identifies two biologically distinct HPV and three non-HPV subtypes. Clin Cancer Res 21, 870–881, https://doi.org/10.1158/1078-0432.CCR-14-2481 (2015).
Ferlay, J. et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136, E359–386, https://doi.org/10.1002/ijc.29210 (2015).
O’Sullivan, B. et al. Development and validation of a staging system for HPV-related oropharyngeal cancer by the International Collaboration on Oropharyngeal cancer Network for Staging (ICON-S): a multicentre cohort study. Lancet Oncol 17, 440–451, https://doi.org/10.1016/S1470-2045(15)00560-4 (2016).
Cancer Genome Atlas, N. Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature 517, 576–582, https://doi.org/10.1038/nature14129 (2015).
Stransky, N. et al. The mutational landscape of head and neck squamous cell carcinoma. Science 333, 1157–1160, https://doi.org/10.1126/science.1208130 (2011).
Mroz, E. A., Tward, A. D., Hammon, R. J., Ren, Y. & Rocco, J. W. Intra-tumor genetic heterogeneity and mortality in head and neck cancer: analysis of data from the Cancer Genome Atlas. PLoS Med 12, e1001786, https://doi.org/10.1371/journal.pmed.1001786 (2015).
Lambert, A. W., Pattabiraman, D. R. & Weinberg, R. A. Emerging Biological Principles of Metastasis. Cell 168, 670–691, https://doi.org/10.1016/j.cell.2016.11.037 (2017).
Brabletz, T., Kalluri, R., Nieto, M. A. & Weinberg, R. A. EMT in cancer. Nat Rev Cancer, https://doi.org/10.1038/nrc.2017.118 (2018).
Yang, J. & Weinberg, R. A. Epithelial-mesenchymal transition: at the crossroads of development and tumor metastasis. Dev Cell 14, 818–829, S1534-5807(08)00209-8 (2008).
Ye, X. & Weinberg, R. A. Epithelial-Mesenchymal Plasticity: A Central Regulator of Cancer Progression. Trends Cell Biol 25, 675–686, https://doi.org/10.1016/j.tcb.2015.07.012 (2015).
Thiery, J. P. & Lim, C. T. Tumor dissemination: an EMT affair. Cancer Cell 23, 272–273, https://doi.org/10.1016/j.ccr.2013.03.004 (2013).
Biddle, A., Gammon, L., Liang, X., Costea, D. E. & Mackenzie, I. C. Phenotypic Plasticity Determines Cancer Stem Cell Therapeutic Resistance in Oral Squamous Cell Carcinoma. EBioMedicine 4, 138–145, https://doi.org/10.1016/j.ebiom.2016.01.007 (2016).
Biddle, A. et al. Cancer stem cells in squamous cell carcinoma switch between two distinct phenotypes that are preferentially migratory or proliferative. Cancer Res 71, 5317–5326, 0008-5472.CAN-11-1059 (2011).
Zheng, X. et al. Epithelial-to-mesenchymal transition is dispensable for metastasis but induces chemoresistance in pancreatic cancer. Nature 527, 525–530, https://doi.org/10.1038/nature16064 (2015).
Fischer, K. R. et al. Epithelial-to-mesenchymal transition is not required for lung metastasis but contributes to chemoresistance. Nature 527, 472–476, https://doi.org/10.1038/nature15748 (2015).
Aiello, N. M. et al. Upholding a role for EMT in pancreatic cancer metastasis. Nature 547, E7–E8, https://doi.org/10.1038/nature22963 (2017).
Ye, X. et al. Upholding a role for EMT in breast cancer metastasis. Nature 547, E1–E3, https://doi.org/10.1038/nature22816 (2017).
Maetzel, D. et al. Nuclear signalling by tumour-associated antigen EpCAM. Nat Cell Biol 11, 162–171 (2009).
Lu, T. Y. et al. Epithelial cell adhesion molecule regulation is associated with the maintenance of the undifferentiated phenotype of human embryonic stem cells. J Biol Chem 285, 8719–8732, M109.077081 (2010).
Baeuerle, P. A. & Gires, O. EpCAM (CD326) finding its role in cancer. Br J Cancer 96, 417–423 (2007).
Sarrach, S. et al. Spatiotemporal patterning of EpCAM is important for murine embryonic endo- and mesodermal differentiation. Sci Rep 8, 1801, https://doi.org/10.1038/s41598-018-20131-8 (2018).
Driemel, C. et al. Context-dependent adaption of EpCAM expression in early systemic esophageal cancer. Oncogene 33, 4904–4915, https://doi.org/10.1038/onc.2013.441 (2014).
Gorges, T. M. et al. Circulating tumour cells escape from EpCAM-based detection due to epithelial-to-mesenchymal transition. BMC Cancer 12, 178, 1471-2407-12-178 (2012).
Hyun, K. A. et al. Epithelial-to-mesenchymal transition leads to loss of EpCAM and different physical properties in circulating tumor cells from metastatic breast cancer. Oncotarget. https://doi.org/10.18632/oncotarget.8250 (2016).
Massoner, P. et al. EpCAM is overexpressed in local and metastatic prostate cancer, suppressed by chemotherapy and modulated by MET-associated miRNA-200c/205. Br J Cancer 111, 955–964, https://doi.org/10.1038/bjc.2014.366 (2014).
Sankpal, N. V., Fleming, T. P., Sharma, P. K., Wiedner, H. J. & Gillanders, W. E. A double-negative feedback loop between EpCAM and ERK contributes to the regulation of epithelial-mesenchymal transition in cancer. Oncogene, https://doi.org/10.1038/onc.2016.504 (2017).
Wang, M. H. et al. Epithelial cell adhesion molecule overexpression regulates epithelial-mesenchymal transition, stemness and metastasis of nasopharyngeal carcinoma cells via the PTEN/AKT/mTOR pathway. Cell Death Dis 9, 2, https://doi.org/10.1038/s41419-017-0013-8 (2018).
Takahashi, K. et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 131, 861–872, https://doi.org/10.1016/j.cell.2007.11.019 (2007).
Bayo, P. et al. Loss of SOX2 expression induces cell motility via vimentin up-regulation and is an unfavorable risk factor for survival of head and neck squamous cell carcinoma. Mol Oncol 9, 1704–1719, https://doi.org/10.1016/j.molonc.2015.05.006 (2015).
Satelli, A. & Li, S. Vimentin in cancer and its potential as a molecular target for cancer therapy. Cell Mol Life Sci 68, 3033–3046, https://doi.org/10.1007/s00018-011-0735-1 (2011).
Puram, S. V. et al. Single-Cell Transcriptomic Analysis of Primary and Metastatic Tumor Ecosystems in Head and Neck. Cancer. Cell 171, 1611–1624 e1624, https://doi.org/10.1016/j.cell.2017.10.044 (2017).
Visvader, J. E. & Lindeman, G. J. Cancer stem cells in solid tumours: accumulating evidence and unresolved questions. Nat Rev Cancer 8, 755–768 (2008).
Mani, S. A. et al. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell 133, 704–715, S0092-8674(08)00444-3 (2008).
Keysar, S. B. et al. Regulation of Head and Neck Squamous Cancer Stem Cells by PI3K and SOX2. J Natl Cancer Inst 109, https://doi.org/10.1093/jnci/djw189 (2017).
Lin, S. C. et al. Epigenetic Switch between SOX2 and SOX9 Regulates Cancer Cell Plasticity. Cancer Res, https://doi.org/10.1158/0008-5472.CAN-15-3178 (2016).
Litvinov, S. V., Velders, M. P., Bakker, H. A., Fleuren, G. J. & Warnaar, S. O. Ep-CAM: a human epithelial antigen is a homophilic cell-cell adhesion molecule. J Cell Biol 125, 437–446 (1994).
Chaves-Perez, A. et al. EpCAM regulates cell cycle progression via control of cyclin D1 expression. Oncogene 32, 641–650, https://doi.org/10.1038/onc.2012.75 (2013).
Gonzalez, B., Denzel, S., Mack, B., Conrad, M. & Gires, O. EpCAM Is Involved in Maintenance of the Murine Embryonic Stem Cell Phenotype. Stem Cells 27, 1782–1791, https://doi.org/10.1002/stem.97 (2009).
Ng, V. Y., Ang, S. N., Chan, J. X. & Choo, A. B. Characterization of Epithelial Cell Adhesion Molecule as a Surface Marker on Undifferentiated Human Embryonic Stem Cells. Stem Cells, https://doi.org/10.1002/stem.221 (2009).
Huang, H. P. et al. Epithelial Cell Adhesion Molecule (EpCAM) Complex Proteins Promote Transcription Factor-mediated Pluripotency Reprogramming. J Biol Chem 286, 33520–33532, M111.256164 (2011).
Gires, O. & Stoecklein, N. H. Dynamic EpCAM expression on circulating and disseminating tumor cells: causes and consequences. Cell Mol Life Sci 71, 4393–4402, https://doi.org/10.1007/s00018-014-1693-1 (2014).
Sankpal, N. V., Willman, M. W., Fleming, T. P., Mayfield, J. D. & Gillanders, W. E. Transcriptional Repression of Epithelial Cell Adhesion Molecule Contributes to p53 Control of Breast Cancer Invasion. Cancer Res (2009).
Chung, J. H. et al. SOX2 activation predicts prognosis in patients with head and neck squamous cell carcinoma. Sci Rep 8, 1677, https://doi.org/10.1038/s41598-018-20086-w (2018).
Bochen, F. et al. Effect of 3q oncogenes SEC. 62 and SOX2 on lymphatic metastasis and clinical outcome of head and neck squamous cell carcinomas. Oncotarget 8, 4922–4934, https://doi.org/10.18632/oncotarget.13986 (2017).
Schrock, A. et al. Expression and role of the embryonic protein SOX2 in head and neck squamous cell carcinoma. Carcinogenesis 35, 1636–1642, https://doi.org/10.1093/carcin/bgu094 (2014).
Gonzalez-Marquez, R. et al. SOX2 expression in hypopharyngeal, laryngeal, and sinonasal squamous cell carcinoma. Hum Pathol 45, 851–857, https://doi.org/10.1016/j.humpath.2013.12.004 (2014).
Stoecklein, N. H. et al. EpCAM expression in squamous cell carcinoma of the esophagus: a potential therapeutic target and prognostic marker. BMC Cancer 6, 165 (2006).
Varga, M. et al. Overexpression of epithelial cell adhesion molecule antigen in gallbladder carcinoma is an independent marker for poor survival. Clin Cancer Res 10, 3131–3136 (2004).
Fong, D. et al. Loss of membranous expression of the intracellular domain of EpCAM is a frequent event and predicts poor survival in patients with pancreatic cancer. Histopathology 64, 683–692, https://doi.org/10.1111/his.12307 (2014).
Fong, D. et al. Ep-CAM expression in pancreatic and ampullary carcinomas: frequency and prognostic relevance. J Clin Pathol (2006).
Gastl, G., Spizzo, G., Obrist, P., Dunser, M. & Mikuz, G. Ep-CAM overexpression in breast cancer as a predictor of survival. Lancet 356, 1981–1982 (2000).
Brunner, A. et al. EpCAM is predominantly expressed in high grade and advanced stage urothelial carcinoma of the bladder. J Clin Pathol 61, 307–310, https://doi.org/10.1136/jcp.2007.049460 (2008).
Spizzo, G. et al. High Ep-CAM expression is associated with poor prognosis in node-positive breast cancer. Breast Cancer Res Treat 86, 207–213 (2004).
Spizzo, G. et al. Prognostic significance of Ep-CAM AND Her-2/neu overexpression in invasive breast cancer. Int J Cancer 98, 883–888 (2002).
Seeber, A. et al. Predominant expression of truncated EpCAM is associated with a more aggressive phenotype and predicts poor overall survival in colorectal cancer. Int J Cancer 139, 657–663, https://doi.org/10.1002/ijc.30099 (2016).
Went, P. et al. Frequent high-level expression of the immunotherapeutic target Ep-CAM in colon, stomach, prostate and lung cancers. Br J Cancer 94, 128–135 (2006).
Songun, I. et al. Loss of Ep-CAM (CO17-1A) expression predicts survival in patients with gastric cancer. Br J Cancer 92, 1767–1772 (2005).
Went, P. et al. Expression of epithelial cell adhesion molecule (EpCam) in renal epithelial tumors. Am J Surg Pathol 29, 83–88 (2005).
Wang, M. B., Liu, I. Y., Gornbein, J. A. & Nguyen, C. T. HPV-Positive Oropharyngeal Carcinoma: A Systematic Review of Treatment and Prognosis. Otolaryngol Head Neck Surg 153, 758–769, https://doi.org/10.1177/0194599815592157 (2015).
Lydiatt, W. M. et al. Head and Neck cancers-major changes in the American Joint Committee on cancereighth edition cancer staging manual. CA Cancer J Clin 67, 122–137, https://doi.org/10.3322/caac.21389 (2017).
Moore, H. M. et al. Biospecimen reporting for improved study quality (BRISQ). J Proteome Res 10, 3429–3438, https://doi.org/10.1021/pr200021n (2011).
Langendijk, J. A. & Psyrri, A. The prognostic significance of p16 overexpression in oropharyngeal squamous cell carcinoma: implications for treatment strategies and future clinical studies. Ann Oncol 21, 1931–1934, https://doi.org/10.1093/annonc/mdq439 (2010).
Ragin, C. C. et al. 11q13 amplification status and human papillomavirus in relation to p16 expression defines two distinct etiologies of head and neck tumours. Br J Cancer 95, 1432–1438, https://doi.org/10.1038/sj.bjc.6603394 (2006).
Siegel, R., Ma, J., Zou, Z. & Jemal, A. Cancer statistics, 2014. CA Cancer J Clin 64, 9–29, https://doi.org/10.3322/caac.21208 (2014).
Gao, J. et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal 6, pl1, https://doi.org/10.1126/scisignal.2004088 (2013).
Cerami, E. et al. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov 2, 401–404, https://doi.org/10.1158/2159-8290.CD-12-0095 (2012).
Acknowledgements
The work was supported partly by the Wilhelm-Sander-Stiftung to OG (#2012.051.1), the Deutsche Forschungsgemeinschaft to OG (Gi 540-3/1 and Gi 540-3/2), and institutional funding.
Author information
Authors and Affiliations
Contributions
P.B., A.H., J.K., F.S., C.B., U.G., M.J. have organized the patient cohort and controlled the clinical data at the L.M.U.; M.C., M.L., M.A.S. did that correspondingly for the Göttingen cohort; B.M., P.B., A.H., J.K., J.S., A.A., G.K., D.L. have performed staining and quantification; J.H., A.H., H.Z., K.U. have performed statistical evaluations and correlation to clinical outcome; P.B., A.H., C.B., J.H., M.J., K.U. interpreted data and assisted in the generation of figures and writing of the manuscript; O.G. has supervised the study, interpreted data, generated figures with the help of A.H., J.H. and K.U., and written the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Baumeister, P., Hollmann, A., Kitz, J. et al. High Expression of EpCAM and Sox2 is a Positive Prognosticator of Clinical Outcome for Head and Neck Carcinoma. Sci Rep 8, 14582 (2018). https://doi.org/10.1038/s41598-018-32178-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-32178-8
Keywords
This article is cited by
-
5ʹ-Ectonucleotidase CD73/NT5E supports EGFR-mediated invasion of HPV-negative head and neck carcinoma cells
Journal of Biomedical Science (2023)
-
Prognostic and predictive roles of cancer stem cell markers in head and neck squamous cell carcinoma patients receiving chemoradiotherapy with or without nimotuzumab
British Journal of Cancer (2022)
-
X-change symposium: status and future of modern radiation oncology—from technology to biology
Radiation Oncology (2021)
-
Role of cancer stem cell markers ALDH1, BCL11B, BMI-1, and CD44 in the prognosis of advanced HNSCC
Strahlentherapie und Onkologie (2021)
-
Definitive chemoradiotherapy in patients with squamous cell cancers of the head and neck - results from an unselected cohort of the clinical cooperation group “Personalized Radiotherapy in Head and Neck Cancer”
Radiation Oncology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.