Abstract
This study aimed to assess the situation of postpartum depression and maternal bonding in Nagoya, a city distant from the epicenter of the Great East Japan Earthquake that occurred on March 11, 2011. Among the participants at 1 month after childbirth between March 11, 2010 and March 10, 2013 (n = 188), 152 fully responded to the Edinburgh Postnatal Depression Scale (EPDS) and Mother–Infant Bonding Questionnaire (MIBQ). They were divided into pre-quake (n = 58), and 0–6, 6–12, 12–18, and 18–24 months after the earthquake groups (n = 20, 26, 29, and 19, respectively). The rate of mothers who scored above the cutoff point for the EPDS increased from 12.1% in the pre-quake to 35.0% in the 0–6 months group (p = 0.022). The EPDS total and anxiety subscale scores (mean ± standard error) were also significantly different between the pre-quake and 0–6 months after the earthquake groups (4.45 ± 0.50 vs. 7.95 ± 1.47, p = 0.024; 2.16 ± 0.26 vs. 3.65 ± 0.57, p = 0.021, respectively). The EPDS total and anxiety scores were the highest for the 0–6 months group, followed by the 6–12, 12–18, 18–24 months groups (p = 0.019, p = 0.022). MIBQ scores did not differ between the pre-quake and 0–6 months groups. Depressive symptoms, mainly explained by anxiety, increased after the earthquake with no changes in maternal bonding.
Similar content being viewed by others
Introduction
The Great East Japan Earthquake that occurred on March 11, 2011 severely damaged vast areas of Japan. It caused the deaths of approximately 16,000 people, and the subsequent tsunami destroyed as many as 300,000 homes. Such a large-scale disaster increases the risk of mental illness1, including postpartum depression (PPD).
A systematic review of 49 papers indicated a significant correlation between the severity of the damage from disasters and PPD2. Other than direct destruction by the disaster, psychosocial stress owing to the death of victims, secondary economic damage, witnessing terrifying scenes via media coverage, and so on may be associated with the risk of PPD.
A previous study reported that 21.3% of mothers were suspected of having PPD in Miyagi Prefecture, including those living close to the epicenter of the Great East Japan Earthquake3; however, it remains unclear to what degree the Great East Japan Earthquake affected PPD. For example, questions remain regarding the impact of a disaster such as the Great East Japan Earthquake on maternal childcare. PPD is associated with maternal bonding failure4,5,6. Maternal bonding refers to the mother’s loving attitude toward her infant and is an indication of maternal childcare function. Although PPD may be differently related to maternal bonding failure, no previous reports have focused on maternal bonding after a disaster.
Since 2004, we have established a cohort of perinatal women in Nagoya city. Nagoya is about 700 km from the epicenter and was not directly damaged by the Great East Japan Earthquake. However, a massive earthquake (magnitude of 8 or higher) is expected to strike the Tokai area, including Nagoya, with a probability of 70–80% within the next 30 years. After the earthquake, the Fukushima Daiichi nuclear disaster released a large amount of radioactive materials into the environment. Pregnant and postpartum women may more seriously fear the possible exposure of their fetus or newborn children to radiation from contaminated water or food. We hypothesized that perinatal women in this high-risk area might become anxious and depressed more easily because of media coverage or other factors associated with the earthquake. To examine whether such a disaster could affect perinatal women in distant areas from the epicenter, we investigated the relationship between PPD and maternal bonding after the Great East Japan Earthquake.
The strengths of our study are as follows. First, in our previous observational study, we validated the Japanese version of the Edinburgh Postnatal Depression Scale (EPDS)7 and revealed its three-factor structure consisting of anxiety, depression, and anhedonia8. As a result, the symptomatological features of PPD could be clarified using the EPDS. Second, we also validated the Japanese version of the Mother–Infant Bonding Questionnaire (MIBQ)9. Using the MIBQ, we could evaluate the maternal childcare function indicated by maternal bonding after a disaster. Third, we investigated whether the earthquake could affect perinatal women in distant areas from the epicenter.
The aim of this study was to reveal the symptomatological features of PPD and the maternal childcare function indicated by maternal bonding after the disaster in distant areas from the epicenter.
Methods
Participants
Our perinatal cohort was established in 2004 at two maternity facilities in Nagoya (Nagoya Teishin Hospital and Kaseki Hospital). Pregnant women attending perinatal class (starting before the 25th week) were given detailed information about the study design and methods. This information was provided both orally and in written form, and informed consent was obtained from each participant. The eligibility criteria were as follows: 20 years of age or older and able to read and write Japanese. Women who agreed to cooperate in the study were asked to complete the EPDS, a self-report questionnaire used for assessing PPD, at 1 month after childbirth and to return it by mail. We also asked participants about their psychosocial backgrounds, including age, years of schooling, income, and parity, at 1 month postpartum.
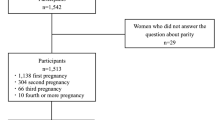
In the present study, we included those who were at 1 month after childbirth between March 11, 2010 and March 10, 2013 because the Great East Japan Earthquake occurred on March 11, 2011. Among 188 participants who were at 1 month after childbirth during this period, 152 returned completed questionnaires. Participants with more than one childbirth were included only at the first chance to participate in the study. The participants were then divided into five groups based on when they answered the questionnaire: pre-quake (0–12 months before the earthquake), and 0–6, 6–12, 12–18, and 18–24 months after the earthquake.
EPDS
The EPDS is a 10-item questionnaire developed as a self-report screening tool for PPD7. Each question is scored from 0–3, and the total score can range from 0–30. The EPDS has shown good internal consistency (Cronbach’s alpha coefficient = 0.87) and reliability (split-half reliability = 0.88)7.
The Japanese version of the EPDS translated by Okano et al.9 was used in the present study. It was retranslated into English and ascertained to be equivalent to the original. It has also shown good internal consistency (Cronbach’s alpha coefficient = 0.78) and test–retest reliability (Spearman’s correlation = 0.92). Its cutoff point of 8/9 has good sensitivity (75%) and specificity (93%)9. Its positive predictive value is 50%. An examination of its factor structure indicated that the three-factor model of anxiety (items 3, 4, and 5), depression (items 7, 8, and 9), and anhedonia (items 1 and 2) was the best-fit model8. The cutoff point of 8/9 and the depression, anxiety, and anhedonia subscales were used in the present study.
MIBQ
The MIBQ was developed by Taylor et al. to evaluate maternal bonding between a mother and her baby10. It is composed of nine questions, and the total score can range from 0–27. A lower total score indicates better maternal bonding. The MIBQ has shown good internal consistency. Pearson’s correlation coefficients for MIBQ scores can range from 0.77–0.9511.
The Japanese version of the MIBQ, which was retranslated into English and ascertained to be equivalent to the original by Yamashita12, was used in the present study. The Japanese version of the MIBQ has been validated and found to have good internal consistency (Cronbach’s alpha coefficients: 0.879 and 0.584)13.
Statistical analysis
The participants were divided into the following five groups based on when they answered the questionnaire, either before or sometime after the earthquake: pre-quake group, 0–6 months group, 6–12 months group, 12–18 months group, and 18–24 months group.
Using data from each group, including total EPDS score, scores for each EPDS subscale, and total MIBQ scores, we calculated the mean and standard error (SE) of the scores for each group.
The Kruskal−Wallis test was used to compare age, years of education, and proportion of primiparas between the five groups. The Mann–Whitney U test was used to compare the mean total and subscale (anxiety, depression, and anhedonia) EPDS scores, and the mean MIBQ scores between the pre-quake and 0–6 months groups. The Jonckheere–Terpstra test was used to examine changes over time in the EPDS total and anxiety subscale scores.
Ethics statement
The study was described to all participants both verbally and in writing, and written informed consent was obtained from each participant. This study protocol was approved by the Ethics Committees of the Nagoya University Graduate School of Medicine, the Ethics Committees of Nagoya Teishin Hospital, and the Ethics Committees of Kaseki Hospital. This study was conducted in accordance with the established ethical standards of all institutions.
Data availability
The datasets analyzed in the current study are available from the corresponding author on reasonable request.
Results
Among 188 women who were at 1 month after childbirth between March 11, 2010 and March 10, 2013, 152 returned completed both the EPDS and the MIBQ. The number of participants in each group based on when they answered the questionnaire was as follows; pre-quake (n = 58), 0–6 months (n = 20), 6–12 months (n = 26), 12–18 months (n = 29), and 18–24 months (n = 19).
The average number of days postpartum of the participants was 30.4 (standard deviation [SD]: ± 6.1). Their mean age was 32.1 (SD: ± 6.4) years, and they had a mean of 14.9 (SD: ± 1.5) years of schooling. As for economic status, the most frequent annual income ranged from 4–6 million yen. The mean age, years of schooling, and annual income were almost identical to national averages. Regarding birth history before the most recent birth, 81.3% of the participants were nulliparous, 12.5% were primiparous, 5.3% had second births and 0.7% had third births. None of the women had four or more births. The mean total EPDS score was 5.39 (SE: ± 0.39). The mean EPDS factor subscale scores were 2.56 (SE: ± 0.19) for anxiety, 1.03 (SE: ± 0.12) for depression, and 0.39 (SE: ± 0.87) for anhedonia.
The demographic data for each participant group are shown in Table 1. No significant differences were observed in terms of age, years of education, or proportion of primiparas between the five groups (p = 0.679, 0.297, and 0.933, respectively; Kruskal–Wallis test).
Regarding mothers who scored above the cutoff point for the EPDS and were identified as being at high risk for PPD, there were 12.1% in the pre-quake group, 35.0% in the 0–6 months group, 34.6% in the 6–12 months group, 24.1% in the 12–18 months group, and 10.5% in the 18–24 months group. The proportion of mothers who scored above the cutoff point (8/9) for the EPDS (high risk for PPD) in the 0–6 months group was significantly higher than that in the pre-quake group (p = 0.022; Mann–Whitney U test).
Figure 1 shows the mean EPDS total and subscale scores in each group. The Mann–Whitney U test was used to compare the EPDS total and subscale (anxiety, depression, and anhedonia) scores between the pre-quake and 0–6 months group; the p values were 0.024, 0.021, 0.059, and 0.078, respectively. The differences in total EPDS and anxiety subscale scores were significant (p = 0.024 and p = 0.021; Mann–Whitney U test).
The total MIBQ score was 1.80 (SE: ± 0.18), and the mean scores of each group were 1.95 (SE: ± 0.29) in the pre-quake group, 1.85 (SE: ± 0.70) in the 0–6 months group, 1.73 (SE: ± 0.40) in the 6–12 months group, 1.69 (SE: ± 0.36) in the 12–18 months group, and 1.58 (SE: ± 0.39) in the 18–24 months group. The total MIBQ score did not differ between the pre-quake and 0–6 months groups (p = 0.338; Mann–Whitney U test).
Based on the results of the Jonckheere–Terpstra test, the 0–6 months group had the highest total EPDS and anxiety scores, followed by the 6–12 months group, the 12–18 months group, and the 18–24 months group (p = 0.019 and 0.022, respectively).
Discussion
To our knowledge, this is the first observational, cross-sectional study to examine the symptomatological features of PPD and maternal bonding in areas indirectly exposed to the Great East Japan Earthquake.
The four main findings of the present can be summarized as follows: 1) The rate of mothers suspected of having PPD increased after the earthquake; 2) The EPDS total scores increased sharply in participants within 6 months after the earthquake, but then decreased over the subsequent 18 months; 3) The anxiety subscale scores increased after the earthquake, but then decreased over the subsequent 18 months (the differences in scores for depression and anhedonia before and after the earthquake were not significant); and 4) The MIBQ scores before and after the earthquake were not significantly different.
As expected, the rate of women suspected of having PPD increased after the Great East Japan Earthquake. Similar results were found in a study of PPD in Miyagi Prefecture, including the epicenter, after the Great East Japan Earthquake3. However, that study did not examine the EPDS subscales. It should be noted that in the present study, only symptoms of anxiety increased the rate of PPD. Consequently, it may be necessary to distinguish disaster-related PPD from general PPD.
The increase in anxiety scores after the earthquake was as expected. Some studies have shown a relationship between depression and anxiety symptoms during the postpartum period after a disaster. Victims of serious flooding in the United States were reported to have anxiety symptoms14, and a cohort study revealed that women who had severe symptoms of anxiety were more vulnerable to PPD (odds ratio = 3.75) after an earthquake in Armenia15. Similar to these previous studies, our findings show that mothers affected by the Great East Japan Earthquake exhibited anxiety symptoms.
However, our results showed that the severity of anxiety decreases to pre-earthquake levels after 2 years. As no particular psychotherapeutic interventions were required to improve the anxiety symptoms, and no changes were seen in the depression and anhedonia symptoms, depressive symptoms after the earthquake could be explained by anxiety as a reaction to a disaster.
Unexpectedly, our findings showed that maternal bonding did not change after the earthquake. According to our previous study, PPD significantly affects bonding between a mother and child in non-disaster situations4. It is possible that stronger maternal bonding is a natural reaction, as mothers attempt to protect their children during unexpected situations. Some studies have pointed out that maternal bonding improves during some stressful situations. For example, in a systematic review, five of 18 studies showed an equal or higher quality of mother–infant bonding in preterm groups compared with full-term groups16. Another study showed that mothers with pregnancy complications exhibited better bonding17. The Great East Japan Earthquake may be a similar stressful situation in terms of enhancing maternal bonding.
As PPD after the earthquake did not affect maternal bonding in the present study, the anxiety experienced after the disaster could have been a normal reaction to an unexpected situation and therefore may not have required psychotherapeutic intervention. The need of mothers for mental health care to improve the mother–infant relationship is considered low. However, the cause-and-effect relationship between maternal bonding and PPD remains unclear.
Although the compared groups did not differ in terms of several sociodemographic characteristics, possible major determinants of PPD were not adjusted for in this study. A meta-analysis revealed that the predictors of PPD include prenatal depression, self-esteem, childcare stress, prenatal anxiety, life stress, social support, marital relationship, history of previous depression, infant temperament, maternity blues, marital status, socioeconomic status, and unplanned/unwanted pregnancy18. Some of these sociodemographic characteristics may have changed after the disaster, even in indirectly affected areas. In addition, neonate characteristics (gender, gender satisfaction, child number, infant weight, health problems in infant) may affect PPD19. In the present study, we did not collect data on psychosocial status, history of mental illness, physical health conditions, family history of mental illness, or health of the neonate. For a more comprehensive examination of PPD after a disaster, psychiatric statuses other than a depressive state and other possible confounding factors in regard to psychosocial backgrounds should be considered in future studies.
The present study had some additional limitations. First, the sample size of the groups after the earthquake was small, which increases the possibility of a type II error. Second, we did not measure what kind of earthquake-related adversities were experienced by the perinatal women. Therefore, the adversities affecting perinatal women remain unclear, as is the relationship between EPDS scores and specific adversities related to the earthquake. Third, some confounding factors may be possible, which makes it difficult to conclude that the observed tendencies were solely the result of the devastating earthquake. Fourth, there was a possibility of selection bias. The participants in this study were recruited from two standard medical facilities in the central area of Nagoya. This geographical characteristic may have had some influence on the results. However, the participants’ demographics did not differ much from national averages. Fifth, we did not obtain any PPD data after the earthquake in other distant areas from the epicenter. Therefore, we cannot conclude whether our findings are specific to Nagoya or common to other distant areas. Lastly, we cannot compare our results with the data sampled in the directly affected area because the data collection time points differed.
In conclusion, an increase in the rate of PPD was observed in areas indirectly exposed to the Great East Japan Earthquake. This was thought to be the result of anxiety as a reaction to the disaster and was not associated with any changes in maternal bonding.
References
Fergusson, D. M., Horwood, L. J., Boden, J. M. & Mulder, R. T. Impact of a major disaster on the mental health of a well-studied cohort. JAMA Psychiatry 71, 1025–1031, https://doi.org/10.1001/jamapsychiatry.2014.652 (2014).
Harville, E., Xiong, X. & Buekens, P. Disasters and perinatal health: a systematic review. Obstet. Gynecol. Surv. 65, 713–728, https://doi.org/10.1097/OGX.0b013e31820eddbe (2010).
Nishigori, H. et al. Surveys of postpartum depression in Miyagi, Japan, after the Great East Japan Earthquake. Arch. Womens Ment. Health 17, 579–581, https://doi.org/10.1007/s00737-014-0459-y (2014).
Ohoka, H. et al. Effects of maternal depressive symptomatology during pregnancy and the postpartum period on infant-mother attachment. Psychiatry Clin. Neurosci. 68, 631–639, https://doi.org/10.1111/pcn.12171 (2014).
Muzik, M. et al. Mother–infant bonding impairment across the first 6 months postpartum: the primacy of psychopathology in women with childhood abuse and neglect histories. Arch. Womens Ment. Health 16, 29–38, https://doi.org/10.1007/s00737-012-0312-0 (2013).
Klier, C. M. Mother–infant bonding disorders in patients with postnatal depression: The Postpartum Bonding Questionnaire in clinical practice. Arch. Womens Ment. Health 9, 289–291, https://doi.org/10.1007/s00737-006-0150-z (2006).
Cox, J. L., Holden, J. M. & Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry. 150, 782–786 (1987).
Kubota, C. et al. Factor structure of the Japanese version of the Edinburgh Postnatal Depression Scale in the postpartum period. PLoS One 9, e103941, https://doi.org/10.1371/journal.pone.0103941 (2014).
Okano, S. et al. Validation and Reliability of Japanese Version of the EPDS. Archives of Psychiatric Diagnostics and Clinical Evaluation 7, 525–533 (1996).
Robson, K. M. & Kumar, R. Delayed onset of maternal affection after childbirth. Br. J. Psychiatry 136, 347–353 (1980).
Brockington, I. F. et al. A screening questionnaire for mother-infant bonding disorders. Arch. Womens Ment. Health 3, 133–140, https://doi.org/10.1007/s007370170010 (2001).
Yamashita, Y. Relationship between postpartum depression and bonding disorder. Archives of Psychiatric Diagnostics and Clinical Evaluation 14, 41–48 (2003).
Ohara, M. et al. Validation and factor analysis of mother-infant bonding questionnaire in pregnant and postpartum women in Japan. BMC Psychiatry 16, 212, https://doi.org/10.1186/s12888-016-0933-3 (2016).
Norris, F. H. & Murrell, S. A. Prior experience as a moderator of disaster impact on anxiety symptoms in older adults. Am. J. Community Psychol. 16, 665–683, https://doi.org/10.1007/BF00930020 (1988).
Demirchyan, A., Petrosyan, D. & Armenian, H. K. Rate and predictors of postpartum depression in a 22-year follow-up of a cohort of earthquake survivors in Armenia. Arch. Womens Ment. Health 17, 229–237, https://doi.org/10.1007/s00737-013-0404-5 (2014).
Tooten, A. et al. Maternal and paternal infant representations: a comparison between parents of term and preterm infants. Infant Behav. Dev. 37, 366–379, https://doi.org/10.1016/j.infbeh.2014.05.004 (2014).
Korja, R., Latva, R. & Lehtonen, L. The effects of preterm birth on mother-infant interaction and attachment during the infant’s first two years. Acta Obstet. Gynecol. Scand. 91, 164–173, https://doi.org/10.1111/j.1600-0412.2011.01304.x (2012).
Beck, C. T. Predictors of postpartum depression: an update. Nurs Res. 50, 275–85 (2001).
Özcan, N. K., Boyacıoğlu, N. E. & Dinç, H. Postpartum depression prevalence and risk factors in Turkey: a systematic review and meta-analysis. Arch Psychiatr Nurs. 31, 420–428, https://doi.org/10.1016/j.apnu.2017.04.006 (2017).
Acknowledgements
We would like to express our gratitude to the staff members at Nagoya Teishin Hospital and Kaseki Hospital. Funding for this study was provided by research grants from the Ministry of Education, Culture, Sports, Science and Technology of Japan; the Ministry of Health, Labour and Welfare of Japan; The Academic Frontier Project for Private Universities, Comparative Cognitive Science Institutes, Meijo University; the Core Research for Evolutional Science and Technology; Intramural Research Grant (21B‐2) for Neurological and Psychiatric Disorders from the National Center of Neurology and Psychiatry, the Specific Research Fund 2012 for East Japan Great Earthquake Revival by The New Technology Development Foundation and the Japan Agency for Medical Research and Development, AMED; and research and development grants for Comprehensive Research for Persons with Disabilities, Japan Agency for Medical Research and Development, AMED, under grant number JP18dk0307077.
Author information
Authors and Affiliations
Contributions
Satomi Murase, Setsuko Goto, Atsuko Kanai, Tomoko Masuda, and Norio Ozaki conceived and designed the experiments. Chika Kubota, Aya Yamauchi, Masako Ohara, Yukako Nakamura, Tomoko Shiino, and Mako Morikawa performed the experiments. Chika Kubota, Yukako Nakamura, and Tomoko Shiino contributed reagents, materials, and analysis tools. Chika Kubota, Mako Morikawa, Masahiko Ando, Takashi Okada, Aya Yamauchi, and Norio Ozaki conducted the statistical analysis. Chika Kubota, Takashi Okada, Mako Morikawa, Branko Aleksic, and Norio Ozaki wrote the paper. All authors contributed to and have approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kubota, C., Okada, T., Morikawa, M. et al. Postpartum depression among women in Nagoya indirectly exposed to the Great East Japan Earthquake. Sci Rep 8, 11624 (2018). https://doi.org/10.1038/s41598-018-30065-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-30065-w
This article is cited by
-
Breastfeeding and humanitarian emergencies: the experiences of pregnant and lactating women during the earthquake in Abruzzo, Italy
International Breastfeeding Journal (2022)
-
Education level and risk of postpartum depression: results from the Japan Environment and Children’s Study (JECS)
BMC Psychiatry (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.