Abstract
This study investigated the clinicopathological characteristics of Henoch-Schönlein purpura nephritis (HSPN) in Chinese adult patients and analyzed the renal outcomes and prognostic risk factors for progression to end-stage renal disease (ESRD). Adult patients who had biopsy-proven HSPN were studied. Their clinicopathological data, renal prognoses and related risk factors were assessed. A total of 698 patients were studied, including 363 men (52.0%) and 335 women (48.0%). Most of the patients had hematuria (85.8%) and/or proteinuria (82.1%). During a median follow-up of 54.0 months, 32 patients (4.6%) progressed to ESRD. The 5- and 10-year cumulative renal survival rates from ESRD were 96.4% and 88.6%, respectively. Baseline urinary protein, renal insufficiency, glomerular sclerosis and tubular atrophy/interstitial fibrosis were independent predictors of renal outcomes. Both the time-average mean arterial pressure and proteinuria during follow-up also influenced the renal prognosis. The patients with a time-average proteinuria <0.4 g/day had the lowest rates of ESRD or a 50% decline in renal function. In conclusion, identifying of clinical and histological prognostic factors may permit the prediction of renal outcomes. The optimal goal of therapy for HSPN patients may be to lower proteinuria to <0.4 g/day and control hypertension to achieve an ideal renal outcome.
Similar content being viewed by others
Introduction
Henoch-Schönlein purpura (HSP) affects people of all ages, but 90% of cases occur in those less than 10 years of age1. The course of HSP is generally benign and self-limited in children2. Kidney involvement occurs in approximately 30–50% of children with HSP3,4. Microscopic hematuria is the most common finding. Macroscopic hematuria, proteinuria, nephrotic syndrome and reduced kidney function are also common manifestations1,5,6. Henoch-Schönlein purpura nephritis (HSPN) has increasingly been identified as a major cause of chronic renal failure in the pediatric patient group7, with approximately 5–15% of children with HSPN progressing to chronic renal failure8.
Adults with HSP present with renal involvement (49–83%) of variable significance9. As shown in previous studies, the clinical presentations and renal outcomes can be more severe in adults than in children with HSPN10, with an estimated 25% to 30% risk of progression to chronic renal insufficiency11. Considerably fewer reports have investigated the renal outcomes of HSPN in adults than those in children. In addition, the study sample sizes are relatively small12,13, and the follow-up time is not sufficient to predict renal prognosis accurately14,15.
As a result, we retrospectively analyzed adult patients who suffered from HSP and had biopsy-proven renal involvement in our center. The aim of our study was to describe the clinical, laboratory and histological characteristics of HSPN in a Chinese adult patient cohort. Long-term renal survival and prognostic factors were also evaluated.
Materials and Methods
Adult patients (age at biopsy ≥18 years old) with biopsy-proven HSPN who were treated in Nanjing Jinling Hospital between January 2003 and December 2013 were reviewed. HSPN was diagnosed when hematuria or proteinuria was associated with a palpable purpuric eruption and/or abdominal and/or joint pain16,17. Patients who suffered from diabetes mellitus, chronic liver disease, acute interstitial nephritis, malignancy and other autoimmune disorders were excluded. Patients without complete clinicopathological data and with <12 months of follow-up were also excluded except for patients who reached end-stage renal disease (ESRD) within 12 months. All follow-up data were updated to November 2016. This study followed the tenets of the Declaration of Helsinki.
General characteristics were recorded, including gender, age at onset and at biopsy, duration and stimulus. Clinical features, including the presence of hypertension, renal involvement and extra-renal manifestations, were assessed. Blood and urine samples were obtained from individual patients at the time of biopsy for routine testing. The laboratory data included hematuria, 24-hour urinary protein, hemoglobin, serum creatinine, urea nitrogen, serum uric acid, serum albumin and cholesterol. Pathological changes were evaluated, including glomerular sclerosis, segmental sclerosis, crescents, glomerulus-Bowman’s capsule adhesion, capillary necrosis and tubular atrophy/interstitial fibrosis. Tubular atrophy/interstitial fibrosis was semi-quantitatively graded as none, mild, moderate and severe18. Immunofluorescence for immunoglobulin G (IgG), immunoglobulin A (IgA), immunoglobulin M (IgM), complement 3 (C3), and complement 1q (C1q) deposits was semi-quantitatively graded from 0 to 3 according to the fluorescence intensity19.
The renal survival time was calculated from the biopsy to the last follow-up. The time-average mean arterial pressure (TA-MAP), time-average proteinuria (TA-P) and microscopic hematuria (TA-RBC) were calculated. Two clinical outcomes were defined. The primary end point was ESRD, and the secondary end point was a composite of ESRD or a 50% reduction in renal function.
Hypertension was diagnosed according to the standards recommended by the World Health Organization Expert Committee12. Microscopic hematuria was measured as counts of erythrocytes per millimeter of urinary sediment and was between 10 and 1000 × 104/mL. Macroscopic hematuria was defined as >1000 × 104/mL. Proteinuria was defined as proteinuria >0.4 g/day. Nephrotic syndrome was defined as plasma albumin <35 g/L and proteinuria >3.5 g/day; patients with albumin <30 g/L were also included in this category if their proteinuria was between 3.0 and 3.5 g/day. The estimated glomerular filtration rate (eGFR) was calculated using the chronic kidney disease epidemiology collaboration (CKD-EPI) formula. Renal insufficiency was defined as an eGFR <60 mL/min/1.73 m2. ESRD was defined as an eGFR <15 mL/min/1.73 m2, initiation of dialysis or transplantation for over three months. Hypoproteinemia and hypercholesterolemia were defined as serum albumin <30 g/L and cholesterol >6.2 mmol/L, respectively. TA-MAP was evaluated as the ratio of the area under the MAP curve during follow-up. TA-P and TA-RBC were calculated using the same method20.
Statistical Analysis
The SPSS 18.0 software (SPSS, Chicago, IL, USA) was used for the statistical analysis. Normally distributed variables were expressed as the means ± SDs. Non-parametric variables are expressed as medians and ranges. Categorical variables were expressed as percentages. Renal survival was estimated using the Kaplan–Meier method. The relationship between the parameters and renal survival was assessed using Cox regression. Receiver operating characteristic (ROC) curves were drawn for variables to determine the optimal cut-off values to predict an endpoint. All P-values were two-tailed, and values <0.05 were considered statistically significant.
Data availability statement
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
Statement of Ethics
The protocol followed in the present study was approved by the Jinling Hospital Ethics Committee on Human Experimentation. Due to the retrospective nature of the study, written informed consent for participation in the study was waived.
Results
Demographic Characteristics of the Adult HSPN Patients at Biopsy
A total of six hundred and ninety-eight patients with adult HSPN were included with 363 men (52.0%) and 335 women (48.0%). The median ages at onset and renal biopsy were 25.0 and 29.0 years, respectively. The intervals between onset and renal biopsy were skewed (median 11.5 months, interquartile range 2.0–48.0 months). The common stimuli associating with the initial clinical manifestations of HSP were infection (11.6%), drugs (7.4%) and food (19.2%); however, 57.9% of the patients had no clear reason for HSP induction (Table 1).
Clinical and Laboratory Data for the Adult HSPN Patients at Biopsy
All the enrolled patients had manifestations of renal involvement and purpura. Gastrointestinal symptoms and arthritis were present in 27.4% and 29.7% of the patients, respectively. The renal involvement was variable. Macroscopic hematuria occurred in 7.4% of the patients, and 78.4% of the patients had microscopic hematuria at biopsy. The incidence of proteinuria was 82.1%, and 9.9% of the patients presented with nephrotic syndrome. In addition, 7.3% of the patients suffered from renal insufficiency. Hypertension occurred in 21.1% of the patients (Table 1).
The median proteinuria at biopsy was 0.88 g/day (interquartile range 0.51–1.79 g/day). The median serum creatinine and blood urea nitrogen levels were 0.77 mg/dL (interquartile range 0.63–0.97 mg/dL) and 13.3 mg/dL (interquartile range 10.6–17.0 mg/dL), respectively. The mean uric acid levels were 333.1 ± 89.0 µmol/L. A total of 65 patients (9.3%) suffered from hypoproteinemia, and 155 patients (22.2%) had hypercholesterolemia (Table 2).
Renal Pathological Findings of the Adult HSPN Patients at Biopsy
The renal pathological evaluation focused on renal components including the glomeruli, tubules and interstitium. The median percentage of glomerular sclerosis was 5.0% (interquartile range 0–13.7%). Glomerular sclerosis of >10% was seen in 192 patients (27.5%). Segmental sclerosis was also observed and involved more than 10% of the glomeruli in 118 patients (16.9%). The median proportion of crescents was 5.0% (interquartile range 0–12.6%), and 60 patients (8.6%) had more than 25% crescents. Bowman’s capsule adhesion was present in 47.4% of the patients, and the incidence of capillary necrosis was 23.8%. A total of 82 patients (11.7%) suffered from moderate and severe lesion of tubular atrophy/interstitial fibrosis lesions. The occurrence of immune complex deposits was as follows: 15.6% with IgG, 36.1% with IgM, 87.0% with C3, and 2.3% with C1q. (Table 2).
Follow-up and Renal Outcomes of the Adult HSPN Patients
The therapies after biopsy were analyzed and shown in Table 3. A total of 166 patients (23.8%) received methylprednisolone pulse treatment and 474 patients (67.9%) were treated with oral prednisone/methylprednisolone. Corticosteroid combined with other immunosuppressive agents was administered as follows: 272 patients (39.0%) with prednisone and tripterysium glycosides, 98 patients (14.0%) with prednisone and mycophenolate mofetil, and 14 patients (2.0%) with prednisone and leflunomide.
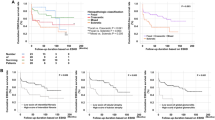
During a median follow-up of 54.0 months (interquartile range, 34.0–78.0 months), the median TA-P measurement of the enrolled adult HSPN patients was 0.45 g/day (interquartile range, 0.30–0.74 g/day). The median TA-MAP value during follow-up was 91.0 mmHg (interquartile range, 85.0–97.0 mmHg). Ultimately, 32 patients (4.6%) developed ESRD, and 53 patients (7.6%) achieved a composite of ESRD or a 50% decline in renal function (Table 3). The 5- and 10-year cumulative renal survival rates from ESRD after renal biopsy as calculated using the Kaplan-Meier methods were 96.4% [95% confidence interval (CI), 94.6–98.2%] and 88.6% (95% CI, 83.5–93.7%), respectively (Fig. 1A). The 5- and 10-year cumulative rates for the composite of ESRD or a 50% decline in renal function were 95.8% (95% CI, 94.0–97.6%) and 79.6% (95% CI, 72.5–86.6%), respectively (Fig. 1B).
Risk Factors at Biopsy and During Follow-up of the Adult HSPN Patients
Hypertension, urinary protein >1.0 g/day, an eGFR <60 mL/min/1.73 m2, and hypoproteinemia predicted an increased risk of ESRD in the univariate analysis. Renal pathological parameters, including glomerular sclerosis >10%, segmental sclerosis >10%, and moderate and severe tubular atrophy/interstitial fibrosis, were also significantly associated with disease progression. Parameters that were significant in the univariate analysis were further considered in a multivariate Cox regression model. This model confirmed that urinary protein >1.0 g/day [hazard ratio (HR) 2.486, P = 0.031], an eGFR <60 mL/min/1.73 m2 (HR 5.344, P < 0.001), glomerular sclerosis >10% (HR 2.397, P = 0.044) and moderate and severe tubular atrophy/interstitial fibrosis (HR 5.239, P < 0.001) were independent predictors of renal outcomes, whereas the other parameters failed to reach statistical significance (Table 4). As shown in Table 5, TA-P, TA-MAP during follow-up, baseline hypertension, baseline proteinuria and an eGFR <60 mL/min/1.73 m2 at biopsy were analyzed in the multivariate Cox model. This analysis confirmed that both TA-P (HR 2.193, P < 0.001) and TA-MAP (HR 1.043, P = 0.041) were independent predictors of renal survival from ESRD. The multivariate Cox analysis also revealed that interval increase of 100 mg/day in TA-P increased the risk of ESRD by 1.082 (P < 0.001).
The area under the ROC curve (AUC) for TA-P was 0.966. The optimal cut-off for TA-P was 1.045 g/day (sensitivity, 93.8%; specificity, 88.9%), which was estimated as 1.0 g/day (Fig. 2A). The renal survival rates from ESRD in each group are shown in Fig. 2B. We analyzed the renal outcomes based on categorical grouping of TA-P excretion by Cox regression. Multivariate analyses with TA-P, TA-MAP, baseline hypertension, baseline proteinuria and an eGFR <60 mL/min/1.73 m2 at biopsy revealed that the patients with TA-P >1.0 g/day were associated with a higher risk (HR 59.689, P < 0.001) of ESRD than those with TA-P <1.0 g/day, which predicted a poor renal outcome. We also set the TA-P cut-offs at 0.4 g/day and 1.0 g/day to divide the patients into three groups. The univariate and multivariate Cox analysis indicated that the patients with TA-P 0.4–1.0 g/day were not associated with a higher risk of ESRD than those with TA-P <0.4 g/day (Table 6). Moreover, the renal survival rates from ESRD or a 50% decline in renal function were significantly different among the three groups, as shown in Fig. 2C. The multivariate Cox analysis indicated that patients with both TA-P levels >1.0 g/day (HR 42.629, P < 0.001) and 0.4–1.0 g/day (HR 3.715, P = 0.045) were associated with higher risks of ESRD or a 50% decline in renal function than those with TA-P <0.4 g/day (Table 6).
Cumulative renal survival rates stratified according to TA-P in the adult HSPN patients. (A) ROC analysis of TA-P; (B) Renal survival rates from ESRD in two groups based on TA-P >1.0 g/day and TA-P <1.0 g/day; (C) Renal survival rates from ESRD or a 50% decline in renal function in three groups based on TA-P >1.0 g/day, 0.4–1.0 g/day and TA-P <0.4 g/day.
Discussion
Although numerous long-term renal survival analyses have been reported for pediatric HSPN patients in developed countries8,21,22, few studies have calculated the clinical features and long-term renal survival rates in adult HSPN patients. Data on this disease in adults are confined to small series with relatively short follow-ups9,13,14,23,24,25, especially in adult Chinese patients. In this study, we reported the epidemiology and spectrum of clinicopathological features in adult HSPN patients and identified the 10-year cumulative renal survival rate in a Chinese cohort with a larger number of patients and longer follow-up and analyzed the risk factors for ESRD in those patients.
The patients enrolled in this study had a slight male predominance. In most previous studies in both children and adults, the proportion of male patients has been higher12,26. However, some studies showed a female predominance22,27. Concerning the induction of HSP, several patients had a recent history of infection, mostly of the upper respiratory tract, but 57.9% of the patients in our cohort had no clear reason for disease induction. However, 46% of the patients in an adult population in the UK had histories of infection preceding presentation13. These variations in general and clinical features may be attributable to the different sample sizes, reporting standards, time frames, races and geographical areas. Due to the limitations of the study candidates, all the patients in our study had purpura and renal involvement. The other extra-renal manifestations, incidences of gastrointestinal symptoms and presence of arthritis were lower than those of the pediatric group, which was confirmed by previous reports13,28.
Microscopic hematuria and proteinuria were the most common renal manifestations in this study. However, hematuria failed to predict the renal prognosis. These findings are consistent with those from previous reports23,24. In other studies, hypertension was an independent predictor of the renal prognosis9,13. Hypertension did not reach statistical significance for predicting renal outcome in our analysis. However, our study demonstrated that TA-MAP during follow-up was a risk factor for predicting renal outcomes. Thus, controlled hypertension predicted good renal prognosis for patients. Moreover, approximately one-quarter of patients had reduced renal function. The multivariate analysis demonstrated that renal insufficiency was an independent predictor of the renal outcome, which was consistent with other studies13,23.
Regarding the renal pathology of HSPN patients, the multivariate analysis showed that glomerular sclerosis >10% was an independent predictor of the renal outcome, and other studies also found that glomerular lesions had a prognostic value13,23. Several acute renal pathological injury manifestations, such as crescents, glomerulus-Bowman’s capsule adhesion and capillary necrosis, failed to associate with the renal outcome. The pathological classification of HSPN in children is widely conducted according to the International study of Kidney Disease in Children (ISKDC) pathology grade, which is based in detail on the degree of mesangial proliferation and the presence of crescents. Most patients in our study had fewer than 10% crescents, which was similar to the results of other studies9,14,29. In a Korean HSPN cohort, 25% of the patients were within ISKDC IV and 8% were within ISKDC V with a higher proportion of crescents30. However, the duration between symptom onset of and the biopsy procedure was 112 (35–293) days30, which was shorter than the duration in our study. Therefore, duration may be an important factor that influences the proportion of crescents and glomerular and segmental sclerosis at biopsy. Moreover, the presence of crescents may not be a sign of irreversible damage in patients with HSPN and thus may not be predictive of the long-term outcome9,30. However, some studies investigating the predictors of outcomes in children and adults with HSPN demonstrated that crescentic nephritis was significantly related to functional decline9,31. In addition, chronic injury to the tubules and interstitium was significantly associated with the outcome in the multivariate analysis, which was consistent with other related studies23,30.
During the follow-up period in our study, 4.6% of all the patients developed ESRD. The 10-year cumulative renal survival rate from ESRD was 88.6%. Several previous studies have shown that renal survival rates in adult HSPN patients can reach 80% at 10 years9,13,23. In a study with thirty-seven patients in a UK population, 27% of the patients progressed to end-stage renal failure with a 72% survival rate at 5 years, a 68% at 10 years and a 46% rate at final review13. A French study with a 14.8-year follow-up period reported that only 11% of the patients proceeded to ESRD, and similar results were found in other populations23,24,32. Compared with previous studies, a lower percentage of the patients progressed to ESRD in our cohort. Thus, the sample size, race, geographical area and treatment may have influenced the results. The follow-up time was relatively short, which could lead to a better apparent prognosis.
Some independent risk factors at biopsy, such as hypertension, renal function impairment, glomerular sclerosis and tubular atrophy/interstitial fibrosis, have been associated with a poor renal prognosis in most studies9,13,23,31. However, not all prognostic factors are the same, and the parameters incorporated into the analysis may also matter. Moreover, variables during follow-up are seldom identified. A previous study that enrolled thirty-seven adult patients with HSPN reported that both proteinuria over 1.0 g/day and hypertension during follow-up were risk factors for ESRD13. Another study also reported that the risk for progression of HSPN was associated with increasing mean proteinuria levels during follow-up9. Our study also suggests that TA-P levels should be controlled optimally to <1.0 g/day. Moreover, we found that patients who achieved TA-P <0.4 g/day benefited more than those with TA-P between 0.4 and 1.0 g/day. Thus, the optimal goal of anti-proteinuric therapy for Chinese adult HSPN patients is to lower proteinuria <0.4 g/day during follow-up.
In conclusion, identifying of clinical and histological prognostic factors may permit the prediction of renal outcomes. The optimal goal of therapy for patients may be to lower proteinuria to <0.4 g/day and to control hypertension to predict a good renal prognosis for HSPN patients.
References
Saulsbury, F. T. Clinical update: Henoch-Schonlein purpura. Lancet (London, England) 369, 976–978, https://doi.org/10.1016/s0140-6736(07)60474-7 (2007).
Edstrom Halling, S., Soderberg, M. P. & Berg, U. B. Predictors of outcome in Henoch-Schonlein nephritis. Pediatric nephrology (Berlin, Germany) 25, 1101–1108, https://doi.org/10.1007/s00467-010-1444-y (2010).
Rai, A., Nast, C. & Adler, S. Henoch-Schonlein purpura nephritis. Journal of the American Society of Nephrology: JASN 10, 2637–2644 (1999).
Narchi, H. Risk of long term renal impairment and duration of follow up recommended for Henoch-Schonlein purpura with normal or minimal urinary findings: a systematic review. Archives of disease in childhood 90, 916–920, https://doi.org/10.1136/adc.2005.074641 (2005).
Kidney Disease: Improving Global Outcomes. Chapter 11: Henoch-Schonlein purpura nephritis. Kidney international supplements 2, 218–220, https://doi.org/10.1038/kisup.2012.24 (2012).
Hahn, D., Hodson, E. M., Willis, N. S. & Craig, J. C. Interventions for preventing and treating kidney disease in Henoch-Schonlein Purpura (HSP). The Cochrane database of systematic reviews 8, CD005128, https://doi.org/10.1002/14651858.CD005128.pub3 (2015).
Guo, Y. N., Wang, Z. & Lu, J. The relationship between children kidney diseases and adult ESRD–an epidemiological investigation of 700 cases. Renal failure 35, 1353–1357, https://doi.org/10.3109/0886022x.2013.828262 (2013).
Scharer, K. et al. Clinical outcome of Schonlein-Henoch purpura nephritis in children. Pediatric nephrology (Berlin, Germany) 13, 816–823, https://doi.org/10.1007/s004670050707 (1999).
Coppo, R. et al. Predictors of outcome in Henoch-Schonlein nephritis in children and adults. American journal of kidney diseases: the official journal of the National Kidney Foundation 47, 993–1003, https://doi.org/10.1053/j.ajkd.2006.02.178 (2006).
Rieu, P. & Noel, L. H. Henoch-Schonlein nephritis in children and adults. Morphological features and clinicopathological correlations. Annales de medecine interne 150, 151–159 (1999).
Kanaan, N. et al. Recurrence and graft loss after kidney transplantation for henoch-schonlein purpura nephritis: a multicenter analysis. Clinical journal of the American Society of Nephrology: CJASN 6, 1768–1772, https://doi.org/10.2215/cjn.00520111 (2011).
Lu, S. et al. Comparison between adults and children with Henoch-Schonlein purpura nephritis. Pediatric nephrology (Berlin, Germany) 30, 791–796, https://doi.org/10.1007/s00467-014-3016-z (2015).
Shrestha, S. et al. Henoch Schonlein purpura with nephritis in adults: adverse prognostic indicators in a UK population. QJM: monthly journal of the Association of Physicians 99, 253–265, https://doi.org/10.1093/qjmed/hcl034 (2006).
Hung, S. P. et al. Clinical manifestations and outcomes of Henoch-Schonlein purpura: comparison between adults and children. Pediatrics and neonatology 50, 162–168, https://doi.org/10.1016/s1875-9572(09)60056-5 (2009).
Xuan, P. et al. Presentation and outcome analysis of 205 adult patients with Henoch-Schönlein purpura nephritis. Chin. J Nephrol 30, 161–165 (2013).
Ozen, S. et al. EULAR/PRINTO/PRES criteria for Henoch-Schonlein purpura, childhood polyarteritis nodosa, childhood Wegener granulomatosis and childhood Takayasu arteritis: Ankara 2008. Part II: Final classification criteria. Ann Rheum Dis 69, 798–806, https://doi.org/10.1136/ard.2009.116657 (2010).
Oh, H. J. et al. Clinical outcomes, when matched at presentation, do not vary between adult-onset Henoch-Schonlein purpura nephritis and IgA nephropathy. Kidney Int 82, 1304–1312, https://doi.org/10.1038/ki.2012.302 (2012).
Chen, S. et al. Pathological spectrums and renal prognosis of severe lupus patients with rapidly progressive glomerulonephritis. Rheumatol Int 35, 709–717, https://doi.org/10.1007/s00296-014-3140-x (2015).
Hilhorst, M., van Paassen, P., van Breda Vriesman, P. & Cohen Tervaert, J. W. Immune complexes in acute adult-onset Henoch-Schonlein nephritis. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association 26, 3960–3967, https://doi.org/10.1093/ndt/gfr149 (2011).
Le, W. et al. Long-term renal survival and related risk factors in patients with IgA nephropathy: results from a cohort of 1155 cases in a Chinese adult population. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association 27, 1479–1485, https://doi.org/10.1093/ndt/gfr527 (2012).
Mao, S. et al. Clinico-pathological association of Henoch-Schoenlein purpura nephritis and IgA nephropathy in children. International journal of clinical and experimental pathology 8, 2334–2342 (2015).
Calvino, M. C. et al. Henoch-Schonlein purpura in children from northwestern Spain: a 20-year epidemiologic and clinical study. Medicine (Baltimore) 80, 279–290 (2001).
Pillebout, E. et al. Henoch-Schonlein Purpura in adults: outcome and prognostic factors. Journal of the American Society of Nephrology: JASN 13, 1271–1278 (2002).
Rauta, V., Tornroth, T. & Gronhagen-Riska, C. Henoch-Schoenlein nephritis in adults-clinical features and outcomes in Finnish patients. Clin Nephrol 58, 1–8 (2002).
Blanco, R., Martinez-Taboada, V. M., Rodriguez-Valverde, V., Garcia-Fuentes, M. & Gonzalez-Gay, M. A. Henoch-Schonlein purpura in adulthood and childhood: two different expressions of the same syndrome. Arthritis Rheum 40, 859–864, https://doi.org/10.1002/1529-0131(199705)40:5<859::AID-ART12>3.0.CO;2-J (1997).
Yang, Y. H. et al. A nationwide survey on epidemiological characteristics of childhood Henoch-Schonlein purpura in Taiwan. Rheumatology (Oxford, England) 44, 618–622, https://doi.org/10.1093/rheumatology/keh544 (2005).
Ghrahani, R., Ledika, M. A., Sapartini, G. & Setiabudiawan, B. Age of onset as a risk factor of renal involvement in Henoch-Schonlein purpura. Asia Pacific allergy 4, 42–47, https://doi.org/10.5415/apallergy.2014.4.1.42 (2014).
Coppo, R., Mazzucco, G., Cagnoli, L., Lupo, A. & Schena, F. P. Long-term prognosis of Henoch-Schonlein nephritis in adults and children. Italian Group of Renal Immunopathology Collaborative Study on Henoch-Schonlein purpura. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association 12, 2277–2283 (1997).
Ye, Q. et al. 24h Urinary Protein Levels and Urine Protein/Creatinine Ratios Could Probably Forecast the Pathological Classification of HSPN. Plos One 10, e0127767, https://doi.org/10.1371/journal.pone.0127767 (2015).
Kim, C. H. et al. Using the Oxford classification of IgA nephropathy to predict long-term outcomes of Henoch-Schonlein purpura nephritis in adults. Modern pathology: an official journal of the United States and Canadian Academy of Pathology, Inc 27, 972–982, https://doi.org/10.1038/modpathol.2013.222 (2014).
Ronkainen, J., Nuutinen, M. & Koskimies, O. The adult kidney 24 years after childhood Henoch-Schonlein purpura: a retrospective cohort study. Lancet (London, England) 360, 666–670, https://doi.org/10.1016/s0140-6736(02)09835-5 (2002).
Calvo-Rio, V. et al. Henoch-Schonlein purpura in northern Spain: clinical spectrum of the disease in 417 patients from a single center. Medicine (Baltimore) 93, 106–113, https://doi.org/10.1097/md.0000000000000019 (2014).
Acknowledgements
This work was supported by the grants funded by the National Natural Science Foundation of China (81500547), the Natural Science Foundation of Jiangsu Province (BK20150560) and the Foundation for Young key Medical Scientists of JiangSu Province, China (QNRC2016894).
Author information
Authors and Affiliations
Contributions
Xiao Huang and Prof. Zheng Tang designed this program. Xiao Huang, Xiaomei Wu and Yaxin Hao took responsibility for the analysis and data interpretation. Weibo Le and Jing Wu helped review the analysis and first draft of the manuscript. Prof. Caihong Zeng provided pathological support and helped draft the pathology part. Prof. Zhihong Liu and Prof. Zheng Tang provided intellectual content of critical importance to the work and approved the final version of the manuscript. The authors thank the patients for their participation in the study and acknowledge the statistical support of MinLin Zhou.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, X., Wu, X., Le, W. et al. Renal Prognosis and Related Risk Factors for Henoch-Schönlein Purpura Nephritis: A Chinese Adult Patient Cohort. Sci Rep 8, 5585 (2018). https://doi.org/10.1038/s41598-018-23638-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-23638-2
This article is cited by
-
Association of Pediatric Vasculitis Activity Score with immunoglobulin A vasculitis with nephritis
Pediatric Nephrology (2023)
-
MEST-C pathological score and long-term outcomes of child and adult patients with Henoch-Schönlein purpura nephritis
BMC Nephrology (2020)
-
Crescent lesions are not a predictive factor in adult-onset Henoch–Schönlein purpura nephritis
Clinical and Experimental Medicine (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.