Abstract
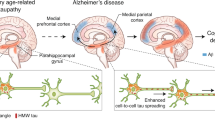
Alzheimer disease (AD) is the most common cause of dementia in older individuals. AD is characterized pathologically by amyloid-β (Aβ) plaques and tau neurofibrillary tangles in the brain, with associated loss of synapses and neurons, which eventually results in dementia. Many of the early attempts to develop treatments for AD focused on Aβ, but a lack of efficacy of these treatments in terms of slowing disease progression led to a change of strategy towards targeting of tau pathology. Given that tau shows a stronger correlation with symptom severity than does Aβ, targeting of tau is more likely to be efficacious once cognitive decline begins. Anti-tau therapies initially focused on post-translational modifications, inhibition of tau aggregation and stabilization of microtubules. However, trials of many potential drugs were discontinued because of toxicity and/or lack of efficacy. Currently, the majority of tau-targeting agents in clinical trials are immunotherapies. In this Review, we provide an update on the results from the initial immunotherapy trials and an overview of new therapeutic candidates that are in clinical development, as well as considering future directions for tau-targeting therapies.
Key points
-
The limited success of amyloid-β-targeting therapies for Alzheimer disease (AD) has led to a shift in focus towards the tau protein — the main component of the neurofibrillary tangles that comprise the other major pathological hallmark of AD.
-
Therapies targeting the expression, post-translational modifications, aggregation and clearance of tau have advanced to testing in humans. These therapies have been largely safe and well tolerated.
-
The clinical efficacy of tau-targeting therapies has yet to be established and some trials have failed; however, multiple trials are ongoing and new candidates continue to enter trials.
-
Antisense oligonucleotides have shown promising results in testing in humans for reducing tau expression, and larger studies will determine whether these findings translate into clinical benefits.
-
Most of the tau-targeting therapies in ongoing trials are immunotherapies, which can target tau intracellularly and/or extracellularly, although extracellular targeting alone is less likely to be effective.
-
The choice of epitope, the antibody subclass and its charge, the patient population and the mechanism of action must all be carefully considered when selecting antibodies and vaccines for clinical trials. Ideally, antibodies should be thoroughly retested after humanization, as this process might alter their properties.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Congdon, E. E. & Sigurdsson, E. M. Tau-targeting therapies for Alzheimer disease. Nat. Rev. Neurol. 14, 399–415 (2018).
[No authors listed] 2022 Alzheimer’s disease facts and figures. Alzheimers Dement. 18, 700–789 (2022).
GBD 2019 Dementia Forecasting Collaborators. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. Lancet Public. Health 7, e105–e125 (2022).
Panza, F., Lozupone, M., Logroscino, G. & Imbimbo, B. P. A critical appraisal of amyloid-β-targeting therapies for Alzheimer disease. Nat. Rev. Neurol. 15, 73–88 (2019).
Jeremic, D., Jimenez-Diaz, L. & Navarro-Lopez, J. D. Past, present and future of therapeutic strategies against amyloid-β peptides in Alzheimer’s disease: a systematic review. Ageing Res. Rev. 72, 101496 (2021).
van Dyck, C. H. et al. Lecanemab in early Alzheimer’s disease. N. Engl. J. Med. 388, 9–21 (2023).
Alzforum. U.S. FDA gives green light to Leqembi, aka lecanemab. Alzforum https://www.alzforum.org/news/research-news/us-fda-gives-green-light-leqembi-aka-lecanemab (2023).
Sims, J. R. et al. Donanemab in early symptomatic Alzheimer disease. JAMA 330, 512–527 (2023).
Lilly. Lilly’s donanemab significantly slowed cognitive and functional decline in phase 3 study of early Alzheimer’s disease. Lilly https://investor.lilly.com/news-releases/news-release-details/lillys-donanemab-significantly-slowed-cognitive-and-functional (2023).
Tissot, C. et al. Association between regional tau pathology and neuropsychiatric symptoms in aging and dementia due to Alzheimer’s disease. Alzheimers Dement. 7, e12154 (2021).
Ossenkoppele, R. et al. Tau PET patterns mirror clinical and neuroanatomical variability in Alzheimer’s disease. Brain 139, 1551–1567 (2016).
Ge, X. et al. Association of tau pathology with clinical symptoms in the subfields of hippocampal formation. Front. Aging Neurosci. 13, 672077 (2021).
Arriagada, P. V., Growdon, J. H., Hedley-Whyte, E. T. & Hyman, B. T. Neurofibrillary tangles but not senile plaques parallel duration and severity of Alzheimer’s disease. Neurology 42, 631–639 (1992).
Arriagada, P. V., Marzloff, K. & Hyman, B. T. Distribution of Alzheimer-type pathologic changes in nondemented elderly individuals matches the pattern in Alzheimer’s disease. Neurology 42, 1681–1688 (1992).
Nelson, P. T. et al. Correlation of Alzheimer disease neuropathologic changes with cognitive status: a review of the literature. J. Neuropathol. Exp. Neurol. 71, 362–381 (2012).
Dronse, J. et al. In vivo patterns of tau pathology, amyloid-β burden, and neuronal dysfunction in clinical variants of Alzheimer’s disease. J. Alzheimers Dis. 55, 465–471 (2017).
Robinson, J. L. et al. Primary tau pathology, not copathology, correlates with clinical symptoms in PSP and CBD. J. Neuropathol. Exp. Neurol. 79, 296–304 (2020).
Chung, D. C., Roemer, S., Petrucelli, L. & Dickson, D. W. Cellular and pathological heterogeneity of primary tauopathies. Mol. Neurodegener. 16, 57 (2021).
Zhang, Y., Wu, K. M., Yang, L., Dong, Q. & Yu, J. T. Tauopathies: new perspectives and challenges. Mol. Neurodegener. 17, 28 (2022).
Braak, H., Alafuzoff, I., Arzberger, T., Kretzschmar, H. & Del Tredici, K. Staging of Alzheimer disease-associated neurofibrillary pathology using paraffin sections and immunocytochemistry. Acta Neuropathol. 112, 389–404 (2006).
Ferreira, D. et al. The hippocampal sparing subtype of Alzheimer’s disease assessed in neuropathology and in vivo tau positron emission tomography: a systematic review. Acta Neuropathol. Commun. 10, 166 (2022).
Ferreira, D., Nordberg, A. & Westman, E. Biological subtypes of Alzheimer disease: a systematic review and meta-analysis. Neurology 94, 436–448 (2020).
Crary, J. F. et al. Primary age-related tauopathy (PART): a common pathology associated with human aging. Acta Neuropathol. 128, 755–766 (2014).
Arima, K. Ultrastructural characteristics of tau filaments in tauopathies: immuno-electron microscopic demonstration of tau filaments in tauopathies. Neuropathology 26, 475–483 (2006).
Jin, N. et al. Truncation and activation of GSK-3β by calpain I: a molecular mechanism links to tau hyperphosphorylation in Alzheimer’s disease. Sci. Rep. 5, 8187 (2015).
Leroy, K., Yilmaz, Z. & Brion, J. P. Increased level of active GSK-3β in Alzheimer’s disease and accumulation in argyrophilic grains and in neurones at different stages of neurofibrillary degeneration. Neuropathol. Appl. Neurobiol. 33, 43–55 (2007).
Pei, J. J. et al. Accumulation of cyclin-dependent kinase 5 (cdk5) in neurons with early stages of Alzheimer’s disease neurofibrillary degeneration. Brain Res. 797, 267–277 (1998).
Tseng, H. C., Zhou, Y., Shen, Y. & Tsai, L. H. A survey of Cdk5 activator p35 and p25 levels in Alzheimer’s disease brains. FEBS Lett. 523, 58–62 (2002).
Patrick, G. N. et al. Conversion of p35 to p25 deregulates Cdk5 activity and promotes neurodegeneration. Nature 402, 615–622 (1999).
Yarza, R., Vela, S., Solas, M. & Ramirez, M. J. c-Jun N-terminal kinase (JNK) signaling as a therapeutic target for Alzheimer’s disease. Front. Pharmacol. 6, 321 (2015).
Sontag, J. M. & Sontag, E. Protein phosphatase 2A dysfunction in Alzheimer’s disease. Front. Mol. Neurosci. 7, 16 (2014).
Taleski, G. & Sontag, E. Protein phosphatase 2A and tau: an orchestrated ‘pas de deux’. FEBS Lett. 592, 1079–1095 (2018).
Frautschy, S. A., Baird, A. & Cole, G. M. Effects of injected Alzheimer beta-amyloid cores in rat brain. Proc. Natl Acad. Sci. USA 88, 8362–8366 (1991).
Kowall, N. W., McKee, A. C., Yankner, B. A. & Beal, M. F. In vivo neurotoxicity of beta-amyloid [β(1-40)] and the β(25-35) fragment. Neurobiol. Aging 13, 537–542 (1992).
Hernandez, P., Lee, G., Sjoberg, M. & Maccioni, R. B. Tau phosphorylation by cdk5 and Fyn in response to amyloid peptide Aβ25–35: involvement of lipid rafts. J. Alzheimers Dis. 16, 149–156 (2009).
Kirouac, L., Rajic, A. J., Cribbs, D. H. & Padmanabhan, J. Activation of Ras-ERK signaling and GSK-3 by amyloid precursor protein and amyloid beta facilitates neurodegeneration in Alzheimer’s disease. eNeuro 4, ENEURO.0149-16.2017 (2017).
Ma, Q. L. et al. β-Amyloid oligomers induce phosphorylation of tau and inactivation of insulin receptor substrate via c-Jun N-terminal kinase signaling: suppression by omega-3 fatty acids and curcumin. J. Neurosci. 29, 9078–9089 (2009).
Nassif, M. et al. β-Amyloid peptide toxicity in organotypic hippocampal slice culture involves Akt/PKB, GSK-3β, and PTEN. Neurochem. Int. 50, 229–235 (2007).
Otth, C. et al. AβPP induces cdk5-dependent tau hyperphosphorylation in transgenic mice Tg2576. J. Alzheimers Dis. 4, 417–430 (2002).
Sigurdsson, E. M., Lee, J. M., Dong, X. W., Hejna, M. J. & Lorens, S. A. Bilateral injections of amyloid-β 25-35 into the amygdala of young Fischer rats: behavioral, neurochemical, and time dependent histopathological effects. Neurobiol. Aging 18, 591–608 (1997).
Sigurdsson, E. M., Lorens, S. A., Hejna, M. J., Dong, X. W. & Lee, J. M. Local and distant histopathological effects of unilateral amyloid-β 25-35 injections into the amygdala of young F344 rats. Neurobiol. Aging 17, 893–901 (1996).
Takashima, A. et al. Exposure of rat hippocampal neurons to amyloid β peptide (25-35) induces the inactivation of phosphatidyl inositol-3 kinase and the activation of tau protein kinase I/glycogen synthase kinase-3β. Neurosci. Lett. 203, 33–36 (1996).
Terwel, D. et al. Amyloid activates GSK-3β to aggravate neuronal tauopathy in bigenic mice. Am. J. Pathol. 172, 786–798 (2008).
Town, T. et al. p35/Cdk5 pathway mediates soluble amyloid-β peptide-induced tau phosphorylation in vitro. J. Neurosci. Res. 69, 362–372 (2002).
Augustinack, J. C., Schneider, A., Mandelkow, E. M. & Hyman, B. T. Specific tau phosphorylation sites correlate with severity of neuronal cytopathology in Alzheimer’s disease. Acta Neuropathol. 103, 26–35 (2002).
Luna-Munoz, J., Chavez-Macias, L., Garcia-Sierra, F. & Mena, R. Earliest stages of tau conformational changes are related to the appearance of a sequence of specific phospho-dependent tau epitopes in Alzheimer’s disease. J. Alzheimers Dis. 12, 365–375 (2007).
Wesseling, H. et al. Tau PTM profiles identify patient heterogeneity and stages of Alzheimer’s disease. Cell 183, 1699–1713.e13 (2020).
Moloney, C. M. et al. Phosphorylated tau sites that are elevated in Alzheimer’s disease fluid biomarkers are visualized in early neurofibrillary tangle maturity levels in the post mortem brain. Alzheimers Dement. https://doi.org/10.1002/alz.12749 (2022).
Braak, H., Thal, D. R., Ghebremedhin, E. & Del Tredici, K. Stages of the pathologic process in Alzheimer disease: age categories from 1 to 100 years. J. Neuropathol. Exp. Neurol. 70, 960–969 (2011).
Neddens, J. et al. Phosphorylation of different tau sites during progression of Alzheimer’s disease. Acta Neuropathol. Commun. 6, 52 (2018).
Kimura, S. & Shiota, K. Sequential changes of programmed cell death in developing fetal mouse limbs and its possible roles in limb morphogenesis. J. Morphol. 229, 337–346 (1996).
Mair, W. et al. FLEXITau: quantifying post-translational modifications of tau protein in vitro and in human disease. Anal. Chem. 88, 3704–3714 (2016).
Regalado-Reyes, M. et al. Phospho-tau changes in the human CA1 during Alzheimer’s disease progression. J. Alzheimers Dis. 69, 277–288 (2019).
Samimi, N. et al. Distinct phosphorylation profiles of tau in brains of patients with different tauopathies. Neurobiol. Aging 108, 72–79 (2021).
Falcon, B. et al. Structures of filaments from Pick’s disease reveal a novel tau protein fold. Nature 561, 137–140 (2018).
Noble, W., Hanger, D. P., Miller, C. C. & Lovestone, S. The importance of tau phosphorylation for neurodegenerative diseases. Front. Neurol. 4, 83 (2013).
Xia, Y., Prokop, S. & Giasson, B. I. “Don’t phos over tau”: recent developments in clinical biomarkers and therapies targeting tau phosphorylation in Alzheimer’s disease and other tauopathies. Mol. Neurodegener. 16, 37 (2021).
Caballero, B. et al. Acetylated tau inhibits chaperone-mediated autophagy and promotes tau pathology propagation in mice. Nat. Commun. 12, 2238 (2021).
Alquezar, C. et al. TSC1 loss increases risk for tauopathy by inducing tau acetylation and preventing tau clearance via chaperone-mediated autophagy. Sci. Adv. 7, eabg3897 (2021).
Alquezar, C., Arya, S. & Kao, A. W. Tau post-translational modifications: dynamic transformers of tau function, degradation, and aggregation. Front. Neurol. 11, 595532 (2020).
Min, S. W. et al. Critical role of acetylation in tau-mediated neurodegeneration and cognitive deficits. Nat. Med. 21, 1154–1162 (2015).
Shin, M. K. et al. Reducing acetylated tau is neuroprotective in brain injury. Cell 184, 2715–2732 (2021).
Vlad, S. C., Miller, D. R., Kowall, N. W. & Felson, D. T. Protective effects of NSAIDs on the development of Alzheimer disease. Neurology 70, 1672–1677 (2008).
de Craen, A. J., Gussekloo, J., Vrijsen, B. & Westendorp, R. G. Meta-analysis of nonsteroidal antiinflammatory drug use and risk of dementia. Am. J. Epidemiol. 161, 114–120 (2005).
Camu, F., Van de Velde, A. & Vanlersberghe, C. Nonsteroidal anti-inflammatory drugs and paracetamol in children. Acta Anaesthesiol. Belg. 52, 13–20 (2001).
Quinn, J. P., Corbett, N. J., Kellett, K. A. B. & Hooper, N. M. Tau proteolysis in the pathogenesis of tauopathies: neurotoxic fragments and novel biomarkers. J. Alzheimers Dis. 63, 13–33 (2018).
Plouffe, V. et al. Hyperphosphorylation and cleavage at D421 enhance tau secretion. PLoS ONE 7, e36873 (2012).
Noble, W. et al. Minocycline reduces the development of abnormal tau species in models of Alzheimer’s disease. FASEB J. 23, 739–750 (2009).
Tan, M. S., Liu, Y., Hu, H., Tan, C. C. & Tan, L. Inhibition of caspase-1 ameliorates tauopathy and rescues cognitive impairment in SAMP8 mice. Metab. Brain Dis. 37, 1197–1205 (2022).
Flores, J., Noel, A., Foveau, B., Beauchet, O. & LeBlanc, A. C. Pre-symptomatic caspase-1 inhibitor delays cognitive decline in a mouse model of Alzheimer disease and aging. Nat. Commun. 11, 4571 (2020).
Flores, J. et al. Caspase-1 inhibition alleviates cognitive impairment and neuropathology in an Alzheimer’s disease mouse model. Nat. Commun. 9, 3916 (2018).
Cantrelle, F. X. et al. Phosphorylation and O-GlcNAcylation of the PHF-1 epitope of tau protein induce local conformational changes of the C-terminus and modulate tau self-assembly into fibrillar aggregates. Front. Mol. Neurosci. 14, 661368 (2021).
Arakhamia, T. et al. Posttranslational modifications mediate the structural diversity of tauopathy strains. Cell 180, 633–644.e12 (2020).
Oakley, S. S. et al. Tau filament self-assembly and structure: tau as a therapeutic target. Front. Neurol. 11, 590754 (2020).
Sanders, D. W. et al. Distinct tau prion strains propagate in cells and mice and define different tauopathies. Neuron 82, 1271–1288 (2014).
Ferrer, I., Andres-Benito, P., Carmona, M. & Del Rio, J. A. Common and specific marks of different tau strains following intra-hippocampal injection of AD, PiD, and GGT inoculum in hTau transgenic mice. Int. J. Mol. Sci. 23, 15940 (2022).
Weitzman, S. A. et al. Insoluble tau from human FTDP-17 cases exhibit unique transmission properties in vivo. J. Neuropathol. Exp. Neurol. 79, 941–949 (2020).
Kaufman, S. K. et al. Tau prion strains dictate patterns of cell pathology, progression rate, and regional vulnerability in vivo. Neuron 92, 796–812 (2016).
Clavaguera, F. et al. Brain homogenates from human tauopathies induce tau inclusions in mouse brain. Proc. Natl Acad. Sci. USA 110, 9535–9540 (2013).
Niewiadomska, G., Niewiadomski, W., Steczkowska, M. & Gasiorowska, A. Tau oligomers neurotoxicity. Life 11, 28 (2021).
Gerson, J. E., Mudher, A. & Kayed, R. Potential mechanisms and implications for the formation of tau oligomeric strains. Crit. Rev. Biochem. Mol. Biol. 51, 482–496 (2016).
Shafiei, S. S., Guerrero-Munoz, M. J. & Castillo-Carranza, D. L. Tau oligomers: cytotoxicity, propagation, and mitochondrial damage. Front. Aging Neurosci. 9, 83 (2017).
Cardenas-Aguayo Mdel, C., Gomez-Virgilio, L., DeRosa, S. & Meraz-Rios, M. A. The role of tau oligomers in the onset of Alzheimer’s disease neuropathology. ACS Chem. Neurosci. 5, 1178–1191 (2014).
Guerrero-Munoz, M. J., Gerson, J. & Castillo-Carranza, D. L. Tau oligomers: the toxic player at synapses in Alzheimer’s disease. Front. Cell. Neurosci. 9, 464 (2015).
Cheng, Y. & Bai, F. The association of tau with mitochondrial dysfunction in Alzheimer’s disease. Front. Neurosci. 12, 163 (2018).
Montalbano, M. et al. Tau oligomers mediate aggregation of RNA-binding proteins Musashi1 and Musashi2 inducing Lamin alteration. Aging Cell 18, e13035 (2019).
Otero-Garcia, M. et al. Molecular signatures underlying neurofibrillary tangle susceptibility in Alzheimer’s disease. Neuron 110, 2929–2948.e8 (2022).
Vazquez, A. Metabolic states following accumulation of intracellular aggregates: implications for neurodegenerative diseases. PLoS ONE 8, e63822 (2013).
Mandelkow, E. M., Stamer, K., Vogel, R., Thies, E. & Mandelkow, E. Clogging of axons by tau, inhibition of axonal traffic and starvation of synapses. Neurobiol. Aging 24, 1079–1085 (2003).
Brion, J. P. & Flament-Durand, J. Distribution and expression of the α-tubulin mRNA in the hippocampus and the temporal cortex in Alzheimer’s disease. Pathol. Res. Pract. 191, 490–498 (1995).
Cisek, K., Cooper, G. L., Huseby, C. J. & Kuret, J. Structure and mechanism of action of tau aggregation inhibitors. Curr. Alzheimer Res. 11, 918–927 (2014).
Dominguez-Meijide, A., Vasili, E. & Outeiro, T. F. Pharmacological modulators of tau aggregation and spreading. Brain Sci. 10, 858 (2020).
Aillaud, I. & Funke, S. A. Tau aggregation inhibiting peptides as potential therapeutics for Alzheimer disease. Cell. Mol. Neurobiol. 43, 951–961 (2023).
Martinez-Hernandez, J. et al. Crosstalk between acetylation and the tyrosination/detyrosination cycle of α-tubulin in Alzheimer’s disease. Front. Cell Dev. Biol. 10, 926914 (2022).
Zhang, F. et al. Posttranslational modifications of α-tubulin in alzheimer disease. Transl. Neurodegener. 4, 9 (2015).
Rajaei, S. et al. Conformational change and GTPase activity of human tubulin: a comparative study on Alzheimer’s disease and healthy brain. J. Neurochem. 155, 207–224 (2020).
Peris, L. et al. Tubulin tyrosination regulates synaptic function and is disrupted in Alzheimer’s disease. Brain 145, 2486–2506 (2022).
Vu, H. T., Akatsu, H., Hashizume, Y., Setou, M. & Ikegami, K. Increase in α-tubulin modifications in the neuronal processes of hippocampal neurons in both kainic acid-induced epileptic seizure and Alzheimer’s disease. Sci. Rep. 7, 40205 (2017).
Caponio, D. et al. Compromised autophagy and mitophagy in brain ageing and Alzheimer’s diseases. Aging Brain 2, 100056 (2022).
Filippone, A., Esposito, E., Mannino, D., Lyssenko, N. & Pratico, D. The contribution of altered neuronal autophagy to neurodegeneration. Pharmacol. Ther. 238, 108178 (2022).
Nixon, R. A. The aging lysosome: an essential catalyst for late-onset neurodegenerative diseases. Biochim. Biophys. Acta Proteins Proteom. 1868, 140443 (2020).
Bourdenx, M. et al. Chaperone-mediated autophagy prevents collapse of the neuronal metastable proteome. Cell 184, 2696–2714.e25 (2021).
Lee, J. H. et al. Lysosomal proteolysis and autophagy require presenilin 1 and are disrupted by Alzheimer-related PS1 mutations. Cell 141, 1146–1158 (2010).
Urbanelli, L. et al. Cathepsin D expression is decreased in Alzheimer’s disease fibroblasts. Neurobiol. Aging 29, 12–22 (2008).
Mori, H., Kondo, J. & Ihara, Y. Ubiquitin is a component of paired helical filaments in Alzheimer’s disease. Science 235, 1641–1644 (1987).
Keller, J. N., Hanni, K. B. & Markesbery, W. R. Impaired proteasome function in Alzheimer’s disease. J. Neurochem. 75, 436–439 (2000).
Perry, G., Friedman, R., Shaw, G. & Chau, V. Ubiquitin is detected in neurofibrillary tangles and senile plaque neurites of Alzheimer disease brains. Proc. Natl Acad. Sci. USA 84, 3033–3036 (1987).
Perez, M. et al. Tau – an inhibitor of deacetylase HDAC6 function. J. Neurochem. 109, 1756–1766 (2009).
Li, M. Z. et al. Intracellular accumulation of tau inhibits autophagosome formation by activating TIA1-amino acid-mTORC1 signaling. Mil. Med. Res. 9, 38 (2022).
Feng, Q. et al. MAPT/tau accumulation represses autophagy flux by disrupting IST1-regulated ESCRT-III complex formation: a vicious cycle in Alzheimer neurodegeneration. Autophagy 16, 641–658 (2020).
Funk, K. E., Mrak, R. E. & Kuret, J. Granulovacuolar degeneration (GVD) bodies of Alzheimer’s disease (AD) resemble late-stage autophagic organelles. Neuropathol. Appl. Neurobiol. 37, 295–306 (2011).
Midani-Kurcak, J. S., Dinekov, M., Puladi, B., Arzberger, T. & Kohler, C. Effect of tau-pathology on charged multivesicular body protein 2b (CHMP2B). Brain Res. 1706, 224–236 (2019).
Yamazaki, Y. et al. Immunopositivity for ESCRT-III subunit CHMP2B in granulovacuolar degeneration of neurons in the Alzheimer’s disease hippocampus. Neurosci. Lett. 477, 86–90 (2010).
Jones, E. M. et al. Interaction of tau protein with model lipid membranes induces tau structural compaction and membrane disruption. Biochemistry 51, 2539–2550 (2012).
Calafate, S., Flavin, W., Verstreken, P. & Moechars, D. Loss of Bin1 promotes the propagation of tau pathology. Cell Rep. 17, 931–940 (2016).
Caballero, B. et al. Interplay of pathogenic forms of human tau with different autophagic pathways. Aging Cell 17, e12692 (2018).
Polanco, J. C., Hand, G. R., Briner, A., Li, C. & Gotz, J. Exosomes induce endolysosomal permeabilization as a gateway by which exosomal tau seeds escape into the cytosol. Acta Neuropathol. 141, 235–256 (2021).
Flavin, W. P. et al. Endocytic vesicle rupture is a conserved mechanism of cellular invasion by amyloid proteins. Acta Neuropathol. 134, 629–653 (2017).
Chen, J. J. et al. Compromised function of the ESCRT pathway promotes endolysosomal escape of tau seeds and propagation of tau aggregation. J. Biol. Chem. 294, 18952–18966 (2019).
Scoles, D. R., Minikel, E. V. & Pulst, S. M. Antisense oligonucleotides: a primer. Neurol. Genet. 5, e323 (2019).
Alzforum. Antisense therapy stifles CSF tau in mild Alzheimer’s disease. Alzforum https://www.alzforum.org/news/conference-coverage/antisense-therapy-stifles-csf-tau-mild-alzheimers-disease-0 (2021).
Alzforum. First hit on aggregated tau: antisense oligonucleotide lowers tangles. Alzforum https://www.alzforum.org/news/conference-coverage/first-hit-aggregated-tau-antisense-oligonucleotide-lowers-tangles (2023).
Mummery, C. J. et al. Tau-targeting antisense oligonucleotide MAPT(Rx) in mild Alzheimer’s disease: a phase 1b, randomized, placebo-controlled trial. Nat. Med. 29, 1437–1447 (2023).
Chohan, M. O., Khatoon, S., Iqbal, I. G. & Iqbal, K. Involvement of I2PP2A in the abnormal hyperphosphorylation of tau and its reversal by memantine. FEBS Lett. 580, 3973–3979 (2006).
Corcoran, N. M. et al. Sodium selenate specifically activates PP2A phosphatase, dephosphorylates tau and reverses memory deficits in an Alzheimer’s disease model. J. Clin. Neurosci. 17, 1025–1033 (2010).
Rueli, R. H. L. H. et al. Selenprotein S reduces endoplasmic reticulum stress-induced phosphorylation of tau: potential selenate mitigation of tau pathology. J. Alzheimers Dis. 55, 749–762 (2017).
van Eersel, J. et al. Sodium selenate mitigates tau pathology, neurodegeneration, and functional deficits in Alzheimer’s disease models. Proc. Natl Acad. Sci. USA 107, 13888–13893 (2010).
Malpas, C. B. et al. A phase IIa randomized control trial of VEL015 (sodium selenate) in mild-moderate Alzheimer’s disease. J. Alzheimers Dis. 54, 223–232 (2016).
Vivash, L. et al. A phase 1b open-label study of sodium selenate as a disease-modifying treatment for possible behavioral variant frontotemporal dementia. Alzheimers Dement. 8, e12299 (2022).
Vivash, L. et al. A study protocol for a phase II randomised, double-blind, placebo-controlled trial of sodium selenate as a disease-modifying treatment for behavioural variant frontotemporal dementia. BMJ Open. 10, e040100 (2020).
Vivash, L. et al. Sodium selenate as a disease-modifying treatment for progressive supranuclear palsy: protocol for a phase 2, randomised, double-blind, placebo-controlled trial. BMJ Open. 11, e055019 (2021).
Muñoz-B, S., Tornero-Écija, A. R., Vincent, O. & Escalante, R. VPS13A is closely associated with mitochondria and is required for efficient lysosomal degradation. Dis. Model. Mech. 12, dmm036681 (2019).
Fu, Z.-Q. et al. LiCl attenuates thapsigargin-induced tau hyperphosphorylation by inhibiting GSK-3β in vivo and in vitro. J. Alzheimers Dis. 21, 1107–1117 (2010).
Duthie, A. et al. Recruitment, retainment, and biomarkers of response; a pilot trial of lithium in humans with mild cognitive impairment. Front. Mol. Neurosci. 12, 163 (2019).
VandeVrede, L. et al. Open‐label phase 1 futility studies of salsalate and young plasma in progressive supranuclear palsy. Mov. Disord. Clin. Pract. 7, 440–447 (2020).
Robertson, L. A., Moya, K. L. & Breen, K. C. The potential role of tau protein O-glycosylation in Alzheimer’s disease. J. Alzheimers Dis. 6, 489–495 (2004).
Liu, F., Iqbal, K., Grundke-Iqbal, I., Hart, G. W. & Gong, C.-X. O-GlcNAcylation regulates phosphorylation of tau: a mechanism involved in Alzheimer’s disease. Proc. Natl Acad. Sci. USA 101, 10804–10809 (2004).
Alzforum. Therapeutics: ASN90. Alzforum https://www.alzforum.org/therapeutics/asn90 (2022).
Ryan, J. M. et al. Phase 1 study in healthy volunteers of the O-GlcNAcase inhibitor ASN120290 as a novel therapy for progressive supranuclear palsy and related tauopathies [abstract O1-12-05]. Alzheimers Dement. 14 (7S Part 4), 251 (2018).
Shcherbinin, S. et al. Brain target occupancy of LY3372689, an inhibitor of the O‐GlcNAcase (OGA) enzyme: translation from rat to human: neuroimaging/evaluating treatments. Alzheimers Dement. 16, e040558 (2020).
Alzforum. Therapeutics: LY3372689. Alzforum https://www.alzforum.org/therapeutics/ly3372689 (2022).
Kielbasa, W. et al. Brain target occupancy of LY3372689, an inhibitor of the O‐GlcNAcase (OGA) enzyme, following administration of single and multiple doses to healthy volunteers. Alzheimers Dement. 17, e057774 (2021).
Kielbasa, W. et al. A single ascending dose study in healthy volunteers to assess the safety and PK of LY3372689, an inhibitor of O‐GlcNAcase (OGA) enzyme. Human/human trials: anti‐tau. Alzheimers Dement. 16, e040473 (2020).
Lowe, S. L. et al. Single and multiple ascending dose studies in healthy volunteers to assess the safety and PK of LY3372689, an inhibitor of the O‐GlcNAcase (OGA) enzyme. Alzheimers Dement. 17, e057728 (2021).
Howard, R. et al. Minocycline at 2 different dosages vs placebo for patients with mild Alzheimer disease: a randomized clinical trial. JAMA Neurol. 77, 164–174 (2020).
Ma, Q.-L. et al. Curcumin suppresses soluble tau dimers and corrects molecular chaperone, synaptic, and behavioral deficits in aged human tau transgenic mice. J. Biol. Chem. 288, 4056–4065 (2013).
Rane, J. S., Bhaumik, P. & Panda, D. Curcumin inhibits tau aggregation and disintegrates preformed tau filaments in vitro. J. Alzheimers Dis. 60, 999–1014 (2017).
Goel, A., Kunnumakkara, A. B. & Aggarwal, B. B. Curcumin as “Curecumin”: from kitchen to clinic. Biochem. Pharmacol. 75, 787–809 (2008).
Small, G. W. et al. Memory and brain amyloid and tau effects of a bioavailable form of curcumin in non-demented adults: a double-blind, placebo-controlled 18-month trial. Am. J. Geriatr. Psychiatry 26, 266–277 (2018).
Hosokawa, M. et al. Methylene blue reduced abnormal tau accumulation in P301L tau transgenic mice. PLoS ONE 7, e52389 (2012).
Hochgräfe, K. et al. Preventive methylene blue treatment preserves cognition in mice expressing full-length pro-aggregant human Tau. Acta Neuropathol. Commun. 3, 25 (2015).
Gauthier, S. et al. Efficacy and safety of tau-aggregation inhibitor therapy in patients with mild or moderate Alzheimer’s disease: a randomised, controlled, double-blind, parallel-arm, phase 3 trial. Lancet 388, 2873–2884 (2016).
Wilcock, G. K. et al. Potential of low dose leuco-methylthioninium bis(hydromethanesulphonate) (LMTM) monotherapy for treatment of mild Alzheimer’s disease: cohort analysis as modified primary outcome in a phase III clinical trial. J. Alzheimers Dis. 61, 435–457 (2018).
Alzforum. Tau inhibitor fails again – subgroup analysis irks clinicians at CTAD. Alzforum https://www.alzforum.org/news/conference-coverage/tau-inhibitor-fails-again-subgroup-analysis-irks-clinicians-ctad (2016).
Alzforum. In first phase 3 trial, the Tau drug LMTM did not work. Period. Alzforum http://www.alzforum.org/news/conference-coverage/first-phase-3-trial-tau-drug-lmtm-did-not-work-period#show-more (2016).
Alzforum. First round of FTD therapeutics fell short, but many more are up and running. Alzforum https://www.alzforum.org/news/conference-coverage/first-round-ftd-therapeutics-fell-short-many-more-are-and-running (2016).
Alzforum. Therapeutics: ACI-3024. Alzforum https://www.alzforum.org/therapeutics/aci-3024 (2021).
Fitzgerald, D. P. et al. TPI-287, a new taxane family member, reduces the brain metastatic colonization of breast cancer cells. Mol. Cancer Ther. 11, 1959–1967 (2012).
Tsai, R. M. et al. Reactions to multiple ascending doses of the microtubule stabilizer TPI-287 in patients with Alzheimer disease, progressive supranuclear palsy, and corticobasal syndrome: a randomized clinical trial. JAMA Neurol. 77, 215–224 (2020).
Magen, I. & Gozes, I. Microtubule-stabilizing peptides and small molecules protecting axonal transport and brain function: focus on davunetide (NAP). Neuropeptides 47, 489–495 (2013).
Asuni, A. A., Quartermain, D. & Sigurdsson, E. M. Tau-based immunotherapy for dementia. Alzheimers Dement. 2, S40–S41 (2006).
Asuni, A. A., Boutajangout, A., Quartermain, D. & Sigurdsson, E. M. Immunotherapy targeting pathological tau conformers in a tangle mouse model reduces brain pathology with associated functional improvements. J. Neurosci. 27, 9115–9129 (2007).
Boutajangout, A., Ingadottir, J., Davies, P. & Sigurdsson, E. M. Passive tau immuntherapy diminishes functional decline and clears tau aggregates in a mouse model of tauopathy [abstract P3-427]. Alzheimers Dement. 6 (4S Part 19), S578 (2010).
Boutajangout, A., Ingadottir, J., Davies, P. & Sigurdsson, E. M. Passive immunization targeting pathological phospho-tau protein in a mouse model reduces functional decline and clears tau aggregates from the brain. J. Neurochem. 118, 658–667 (2011).
Bittar, A., Bhatt, N. & Kayed, R. Advances and considerations in AD tau-targeted immunotherapy. Neurobiol. Dis. 134, 104707 (2020).
Colin, M. et al. From the prion-like propagation hypothesis to therapeutic strategies of anti-tau immunotherapy. Acta Neuropathol. 139, 3–25 (2020).
Congdon, E. E., Jiang, Y. & Sigurdsson, E. M. Targeting tau only extracellularly is likely to be less efficacious than targeting it both intra- and extracellularly. Semin. Cell Dev. Biol. 126, 125–137 (2022).
Ji, C. & Sigurdsson, E. M. Current status of clinical trials on tau immunotherapies. Drugs 81, 1135–1152 (2021).
Sandusky-Beltran, L. A. & Sigurdsson, E. M. Tau immunotherapies: lessons learned, current status and future considerations. Neuropharmacology 175, 108104 (2020).
Ng, P. Y., Chang, I. S., Koh, R. Y. & Chye, S. M. Recent advances in tau-directed immunotherapy against Alzheimer’s disease: an overview of pre-clinical and clinical development. Metab. Brain Dis. 35, 1049–1066 (2020).
Karimi, N., Bayram, C. F., Arslan, E., Saghazadeh, A. & Rezaei, N. Tau immunotherapy in Alzheimer’s disease and progressive supranuclear palsy. Int. Immunopharmacol. 113, 109445 (2022).
Guo, Y., Li, S., Zeng, L.-H. & Tan, J. Tau-targeting therapy in Alzheimer’s disease: critical advances and future opportunities. Ageing Neurodegener. Dis. 2, 11 (2022).
Rosenmann, H. et al. Tauopathy-like abnormalities and neurologic deficits in mice immunized with neuronal tau protein. Arch. Neurol. 63, 1459–1467 (2006).
Rozenstein-Tsalkovich, L. et al. Repeated immunization of mice with phosphorylated-tau peptides causes neuroinflammation. Exp. Neurol. 248, 451–456 (2013).
Rajamohamedsait, H., Rasool, S., Rajamohamedsait, W., Lin, Y. & Sigurdsson, E. M. Prophylactic active tau immunization leads to sustained reduction in both tau and amyloid-β pathologies in 3xTg mice. Sci. Rep. 7, 17034 (2017).
Nicholls, S. B. et al. Characterization of TauC3 antibody and demonstration of its potential to block tau propagation. PLoS ONE 12, e0177914 (2017).
Nobuhara, C. K. et al. Tau antibody targeting pathological species blocks neuronal uptake and interneuron propagation of tau in vitro. Am. J. Pathol. 187, 1399–1412 (2017).
Roberts, M. et al. Pre-clinical characterisation of E2814, a high-affinity antibody targeting the microtubule-binding repeat domain of tau for passive immunotherapy in Alzheimer’s disease. Acta Neuropathol. Commun. 8, 13 (2020).
Rosenqvist, N. et al. Highly specific and selective anti-pS396-tau antibody C10.2 targets seeding-competent tau. Alzheimers Dement. 4, 521–534 (2018).
Yanamandra, K. et al. Anti-tau antibodies that block tau aggregate seeding in vitro markedly decrease pathology and improve cognition in vivo. Neuron 80, 402–414 (2013).
Funk, K. E., Mirbaha, H., Jiang, H., Holtzman, D. M. & Diamond, M. I. Distinct therapeutic mechanisms of tau antibodies: promoting microglial clearance versus blocking neuronal uptake. J. Biol. Chem. 290, 21652–21662 (2015).
Congdon, E. E. et al. Tau antibody chimerization alters its charge and binding, thereby reduces its cellular uptake and efficacy. eBioMedicine 42, 157–173 (2019).
Congdon, E. E. et al. Affinity of tau antibodies for solubilized pathological tau species but not their immunogen or insoluble tau aggregates predicts in vivo and ex vivo efficacy. Mol. Neurodegener. 11, 62–86 (2016).
Shamir, D. B. et al. Dynamics of internalization and intracellular interaction of tau antibodies and human pathological tau protein in a human neuron-like model. Front. Neurol. 11, 602292 (2020).
Kfoury, N., Holmes, B. B., Jiang, H., Holtzman, D. M. & Diamond, M. I. Trans-cellular propagation of Tau aggregation by fibrillar species. J. Biol. Chem. 287, 19440–19451 (2012).
Bright, J. et al. Human secreted tau increases amyloid-beta production. Neurobiol. Aging 36, 693–709 (2015).
Castillo-Carranza, D. L. et al. Passive immunization with Tau oligomer monoclonal antibody reverses tauopathy phenotypes without affecting hyperphosphorylated neurofibrillary tangles. J. Neurosci. 34, 4260–4272 (2014).
d’Abramo, C. et al. Detecting tau in serum of transgenic animal models after tau immunotherapy treatment. Neurobiol. Aging 37, 58–65 (2016).
Yanamandra, K. et al. Anti-tau antibody reduces insoluble tau and decreases brain atrophy. Ann. Clin. Transl. Neurol. 2, 278–288 (2015).
Luo, W. et al. Microglial internalization and degradation of pathological tau is enhanced by an anti-tau monoclonal antibody. Sci. Rep. 5, 11161 (2015).
Andersson, C. R. et al. Antibody-mediated clearance of tau in primary mouse microglial cultures requires Fcγ-receptor binding and functional lysosomes. Sci. Rep. 9, 4658 (2019).
Zilkova, M. et al. Humanized tau antibodies promote tau uptake by human microglia without any increase of inflammation. Acta Neuropathol. Commun. 8, 74 (2020).
Lee, S. H. et al. Antibody-mediated targeting of tau in vivo does not require effector function and microglial engagement. Cell Rep. 16, 1690–1700 (2016).
Mukadam, A. S. et al. Cytosolic antibody receptor TRIM21 is required for effective tau immunotherapy in mouse models. Science 379, 1336–1341 (2023).
Kim, B. et al. Tau immunotherapy is associated with glial responses in FTLD-tau. Acta Neuropathol. 142, 243–257 (2021).
Leyns, C. E. G. & Holtzman, D. M. Glial contributions to neurodegeneration in tauopathies. Mol. Neurodegener. 12, 50 (2017).
Leng, F. & Edison, P. Neuroinflammation and microglial activation in Alzheimer disease: where do we go from here? Nat. Rev. Neurol. 17, 157–172 (2021).
Uddin, M. S. & Lim, L. W. Glial cells in Alzheimer’s disease: from neuropathological changes to therapeutic implications. Ageing Res. Rev. 78, 101622 (2022).
Serrano-Pozo, A. et al. Reactive glia not only associates with plaques but also parallels tangles in Alzheimer’s disease. Am. J. Pathol. 179, 1373–1384 (2011).
Dani, M. et al. Microglial activation correlates in vivo with both tau and amyloid in Alzheimer’s disease. Brain 141, 2740–2754 (2018).
Ismail, R. et al. The relationships between neuroinflammation, beta-amyloid and tau deposition in Alzheimer’s disease: a longitudinal PET study. J. Neuroinflammation 17, 151 (2020).
Maeda, J. et al. In vivo positron emission tomographic imaging of glial responses to amyloid-β and tau pathologies in mouse models of Alzheimer’s disease and related disorders. J. Neurosci. 31, 4720–4730 (2011).
Appleton, J. et al. Neuroinflammation co-localizes highly with tau in amnestic mild cognitive impairment. Alzheimers Dement. 18, e068025 (2022).
Hamelin, L. et al. Early and protective microglial activation in Alzheimer’s disease: a prospective study using 18F-DPA-714 PET imaging. Brain 139, 1252–1264 (2016).
Hamelin, L. et al. Distinct dynamic profiles of microglial activation are associated with progression of Alzheimer’s disease. Brain 141, 1855–1870 (2018).
Fan, Z., Brooks, D. J., Okello, A. & Edison, P. An early and late peak in microglial activation in Alzheimer’s disease trajectory. Brain 140, 792–803 (2017).
Femminella, G. D. et al. Microglial activation in early Alzheimer trajectory is associated with higher gray matter volume. Neurology 92, e1331–e1343 (2019).
Congdon, E. E., Gu, J., Sait, H. B. & Sigurdsson, E. M. Antibody uptake into neurons occurs primarily via clathrin-dependent Fcγ receptor endocytosis and is a prerequisite for acute tau protein clearance. J. Biol. Chem. 288, 35452–35465 (2013).
Gu, J., Congdon, E. E. & Sigurdsson, E. M. Two novel tau antibodies targeting the 396/404 region are primarily taken up by neurons and reduce tau protein pathology. J. Biol. Chem. 288, 33081–33095 (2013).
Wu, Q., Lin, Y., Gu, J. & Sigurdsson, E. M. Dynamic assessment of tau immunotherapies in the brains of live animals by two-photon imaging. eBioMedicine 35, 270–278 (2018).
Collin, L. et al. Neuronal uptake of tau/pS422 antibody and reduced progression of tau pathology in a mouse model of Alzheimer’s disease. Brain 137, 2834–2846 (2014).
McEwan, W. A. et al. Cytosolic Fc receptor TRIM21 inhibits seeded tau aggregation. Proc. Natl Acad. Sci. USA 114, 574–579 (2017).
Krishnamurthy, P. K., Deng, Y. & Sigurdsson, E. M. Mechanistic studies of antibody-mediated clearance of tau aggregates using an ex vivo brain slice model. Front. Psychiatry 2, 59 (2011).
Kondo, A. et al. Antibody against early driver of neurodegeneration cis P-tau blocks brain injury and tauopathy. Nature 523, 431–436 (2015).
Krishnaswamy, S. et al. Antibody-derived in vivo imaging of tau pathology. J. Neurosci. 34, 16835–16850 (2014).
Shamir, D. B., Rosenqvist, N., Rasool, S., Pedersen, J. T. & Sigurdsson, E. M. Internalization of tau antibody and pathological tau protein detected with a flow cytometry multiplexing approach. Alzheimers Dement. 12, 1098–1107 (2016).
Fuller, J. P., Stavenhagen, J. B. & Teeling, J. L. New roles for Fc receptors in neurodegeneration – the impact on immunotherapy for Alzheimer’s disease. Front. Neurosci. 8, 235 (2014).
van der Kleij, H. et al. Evidence for neuronal expression of functional Fc (ε and γ) receptors. J. Allergy Clin. Immunol. 125, 757–760 (2010).
Nakamura, K. et al. CD3 and immunoglobulin G Fc receptor regulate cerebellar functions. Mol. Cell. Biol. 27, 5128–5134 (2007).
Stamou, M., Grodzki, A. C., van Oostrum, M., Wollscheid, B. & Lein, P. J. Fc gamma receptors are expressed in the developing rat brain and activate downstream signaling molecules upon cross-linking with immune complex. J. Neuroinflammation 15, 7 (2018).
Suemitsu, S. et al. Fcγ receptors contribute to pyramidal cell death in the mouse hippocampus following local kainic acid injection. Neuroscience 166, 819–831 (2010).
Andoh, T. & Kuraishi, Y. Direct action of immunoglobulin G on primary sensory neurons through Fc gamma receptor I. FASEB J. 18, 182–184 (2004).
Andoh, T. & Kuraishi, Y. Expression of Fc epsilon receptor I on primary sensory neurons in mice. Neuroreport 15, 2029–2031 (2004).
Qu, L., Zhang, P., LaMotte, R. H. & Ma, C. Neuronal Fc-gamma receptor I mediated excitatory effects of IgG immune complex on rat dorsal root ganglion neurons. Brain. Behav. Immun. 25, 1399–1407 (2011).
Jiang, H. et al. Nociceptive neuronal Fc-gamma receptor I is involved in IgG immune complex induced pain in the rat. Brain. Behav. Immun. 62, 351–361 (2017).
Wang, L. et al. Neuronal FcγRI mediates acute and chronic joint pain. J. Clin. Invest. 129, 3754–3769 (2019).
Chandupatla, R. R., Flatley, A., Feederle, R., Mandelkow, E. M. & Kaniyappan, S. Novel antibody against low-n oligomers of tau protein promotes clearance of tau in cells via lysosomes. Alzheimers Dement. 6, e12097 (2020).
Masliah, E. et al. Effects of α-synuclein immunization in a mouse model of Parkinson’s disease. Neuron 46, 857–868 (2005).
Masliah, E. et al. Passive immunization reduces behavioral and neuropathological deficits in an alpha-synuclein transgenic model of Lewy body disease. PLoS ONE 6, e19338 (2011).
Pozzi, S. et al. Monoclonal full-length antibody against TAR DNA binding protein 43 reduces related proteinopathy in neurons. JCI Insight 5, e140420 (2020).
Karpiak, S. E. & Mahadik, S. P. Selective uptake by Purkinje neurons of antibodies to S-100 protein. Exp. Neurol. 98, 453–457 (1987).
Fabian, R. H. & Ritchie, T. C. Intraneuronal IgG in the central nervous system. J. Neurol. Sci. 73, 257–267 (1986).
Greenlee, J. E., Burns, J. B., Rose, J. W., Jaeckle, K. A. & Clawson, S. Uptake of systemically administered human anticerebellar antibody by rat Purkinje cells following blood-brain barrier disruption. Acta Neuropathol. 89, 341–345 (1995).
Graus, F. et al. Effect of intraventricular injection of an anti-Purkinje cell antibody (anti-Yo) in a guinea pig model. J. Neurol. Sci. 106, 82–87 (1991).
Hill, K. E., Clawson, S. A., Rose, J. W., Carlson, N. G. & Greenlee, J. E. Cerebellar Purkinje cells incorporate immunoglobulins and immunotoxins in vitro: implications for human neurological disease and immunotherapeutics. J. Neuroinflammation 6, 31 (2009).
Greenlee, J. E. et al. Neuronal uptake of anti-Hu antibody, but not anti-Ri antibody, leads to cell death in brain slice cultures. J. Neuroinflammation 11, 160 (2014).
Greenlee, J. E. et al. Purkinje cell death after uptake of anti-Yo antibodies in cerebellar slice cultures. J. Neuropathol. Exp. Neurol. 69, 997–1007 (2010).
Rocchi, A. et al. Autoantibodies to synapsin I sequestrate synapsin I and alter synaptic function. Cell Death Dis. 10, 864 (2019).
Goldwaser, E. L. et al. Evidence that brain-reactive autoantibodies contribute to chronic neuronal internalization of exogenous amyloid-β1-42 and key cell surface proteins during Alzheimer’s disease pathogenesis. J. Alzheimers Dis. 74, 345–361 (2020).
Gustafsson, G. et al. Cellular uptake of α-synuclein oligomer-selective antibodies is enhanced by the extracellular presence of α-synuclein and mediated via Fcγ receptors. Cell. Mol. Neurobiol. 37, 121–131 (2017).
Nguyen, L. et al. Antibody therapy targeting RAN proteins rescues C9 ALS/FTD phenotypes in C9orf72 mouse model. Neuron 105, 645–662.e11 (2020).
Benkler, C. et al. Aggregated SOD1 causes selective death of cultured human motor neurons. Sci. Rep. 8, 16393 (2018).
Zaretsky, D. V., Zaretskaia, M. V. & Molkov, Y. I. Membrane channel hypothesis of lysosomal permeabilization by beta-amyloid. Neurosci. Lett. 770, 136338 (2022).
Umeda, T. et al. Intraneuronal amyloid β oligomers cause cell death via endoplasmic reticulum stress, endosomal/lysosomal leakage, and mitochondrial dysfunction in vivo. J. Neurosci. Res. 89, 1031–1042 (2011).
Yang, A. J., Chandswangbhuvana, D., Margol, L. & Glabe, C. G. Loss of endosomal/lysosomal membrane impermeability is an early event in amyloid Aβ1-42 pathogenesis. J. Neurosci. Res. 52, 691–698 (1998).
Lee, J. H. et al. Faulty autolysosome acidification in Alzheimer’s disease mouse models induces autophagic build-up of Aβ in neurons, yielding senile plaques. Nat. Neurosci. 25, 688–701 (2022).
Ling, D., Song, H. J., Garza, D., Neufeld, T. P. & Salvaterra, P. M. Abeta42-induced neurodegeneration via an age-dependent autophagic-lysosomal injury in Drosophila. PLoS ONE 4, e4201 (2009).
Dingjan, I. et al. Lipid peroxidation causes endosomal antigen release for cross-presentation. Sci. Rep. 6, 22064 (2016).
Zehner, M. et al. The translocon protein Sec61 mediates antigen transport from endosomes in the cytosol for cross-presentation to CD8+ T cells. Immunity 42, 850–863 (2015).
Embgenbroich, M. & Burgdorf, S. Current concepts of antigen cross-presentation. Front. Immunol. 9, 1643 (2018).
Gros, M. & Amigorena, S. Regulation of antigen export to the cytosol during cross-presentation. Front. Immunol. 10, 41 (2019).
Abskharon, R. et al. Crystal structure of a conformational antibody that binds tau oligomers and inhibits pathological seeding by extracts from donors with Alzheimer’s disease. J. Biol. Chem. 295, 10662–10676 (2020).
Li, S. et al. A single-chain variable fragment antibody inhibits aggregation of phosphorylated tau and ameliorates tau toxicity in vitro and in vivo. J. Alzheimers Dis. 79, 1613–1629 (2021).
Krishnaswamy, S., Huang, H. W., Marchal, I. S., Ryoo, H. D. & Sigurdsson, E. M. Neuronally expressed anti-tau scFv prevents tauopathy-induced phenotypes in Drosophila models. Neurobiol. Dis. 137, 104770 (2020).
Kontsekova, E., Zilka, N., Kovacech, B., Novak, P. & Novak, M. First-in-man tau vaccine targeting structural determinants essential for pathological tau-tau interaction reduces tau oligomerisation and neurofibrillary degeneration in an Alzheimer’s disease model. Alzheimers Res. Ther. 6, 44 (2014).
Novak, P. et al. Safety and immunogenicity of the tau vaccine AADvac1 in patients with Alzheimer’s disease: a randomised, double-blind, placebo-controlled, phase 1 trial. Lancet Neurol. 16, 123–134 (2017).
Grossman, M. The non-fluent/agrammatic variant of primary progressive aphasia. Lancet Neurol. 11, 545–555 (2012).
Novak, P. et al. FUNDAMANT: an interventional 72-week phase 1 follow-up study of AADvac1, an active immunotherapy against tau protein pathology in Alzheimer’s disease. Alzheimers Res. Ther. 10, 108 (2018).
Axon Neuroscience. Axon announces positive results from phase II ADAMANT trial for Aadvac1 in Alzheimer’s disease. Axon Neuroscience https://www.axon-neuroscience.eu/docs/press_release_Axon_announces_positive_result_9-9-2019.pdf (2019).
Novak, P. et al. ADAMANT: a placebo-controlled randomized phase 2 study of AADvac1, an active immunotherapy against pathological tau in Alzheimer’s disease. Nat. Aging 1, 521–534 (2021).
Alzforum. Active tau vaccine: hints of slowing neurodegeneration. Alzforum https://www.alzforum.org/news/conference-coverage/active-tau-vaccine-hints-slowing-neurodegeneration (2020).
Hickman, D. T. et al. Sequence-independent control of peptide conformation in liposomal vaccines for targeting protein misfolding diseases. J. Biol. Chem. 286, 13966–13976 (2011).
AC Immune. AC Immune announces interim phase 1b/2a data showing that its ACI-35.030 anti-Ptau Alzheimer’s vaccine generates a potent immune response. AC Immune https://ir.acimmune.com/news-releases/news-release-details/ac-immune-announces-interim-phase-1b2a-data-showing-its-aci (2021).
AC Immune. AC Immune ACI-35.030 phase 1b/2a trial interim data confirm consistent safety and potent immunogenicity of pTau Alzheimer’s vaccine in high-dose cohort. AC Immune https://ir.acimmune.com/news-releases/news-release-details/ac-immune-aci-35030-phase-1b2a-trial-interim-data-confirm (2022).
AC Immune. AC Immune advances phospho-Tau Alzheimer’s vaccine in phase 1b/2a study. AC Immune https://ir.acimmune.com/news-releases/news-release-details/ac-immune-advances-phospho-tau-alzheimers-vaccine-phase-1b2a (2020).
AC Immune. AC Immune announces expansion of phase 1b/2a phospho-Tau Alzheimer’s vaccine trial and provides a program update. AC Immune https://ir.acimmune.com/news-releases/news-release-details/ac-immune-announces-expansion-phase-1b2a-phospho-tau-alzheimers (2021).
AC Immune. AC Immune’s Alzheimer’s vaccine generates potent anti-Ptau antibody response in a phase 1b/2a study. AC Immune https://ir.acimmune.com/news-releases/news-release-details/ac-immunes-alzheimers-vaccine-generates-potent-anti-ptau (2021).
AC Immune. AC Immune’s Alzheimer’s disease vaccine-candidate ACI-35.030 selected for further development. AC Immune https://ir.acimmune.com/news-releases/news-release-details/ac-immunes-alzheimers-disease-vaccine-candidate-aci-35030 (2022).
Tai, H. C. et al. The tau oligomer antibody APNmAb005 detects early-stage pathological tau enriched at synapses and rescues neuronal loss in long-term treatments. Preprint at bioRxiv https://www.biorxiv.org/content/10.1101/2022.06.24.497452v1 (2022).
Courade, J. P. et al. Epitope determines efficacy of therapeutic anti-tau antibodies in a functional assay with human Alzheimer tau. Acta Neuropathol. 136, 729–745 (2018).
Albert, M. et al. Prevention of tau seeding and propagation by immunotherapy with a central tau epitope antibody. Brain 142, 1736–1750 (2019).
Buchanan, T. et al. A randomised, placebo-controlled, first-in-human study with a central Tau epitope antibody – UCB0107 [abstract LBA3]. International Congress of the Parkinson’s Disease and Movement Disorders: 2019 Late-Breaking Abstracts (International Parkinson and Movement Disorder Society, 2019).
UCB. UCB presents UCB0107 anti-Tau immunotherapy Phase I study Results at World Movement Disorders Conference®. UCB https://www.ucb.com/stories-media/Press-Releases/article/UCB-presents-UCB0107-anti-Tau-immunotherapy-Phase-I-study-results-at-World-Movement-Disorders-Conference (2019).
Alzforum. N-terminal tau antibodies fade, mid-domain ones push to the fore. Alzforum https://www.alzforum.org/news/conference-coverage/n-terminal-tau-antibodies-fade-mid-domain-ones-push-fore (2021).
Alzforum. More tau antibodies bid adieu; semorinemab keeps foot in door. Alzforum https://www.alzforum.org/news/conference-coverage/more-tau-antibodies-bid-adieu-semorinemab-keeps-foot-door (2021).
Alzforum. Therapeutics: BIIB076. Alzforum https://www.alzforum.org/therapeutics/biib076 (2022).
Motley Fool Transcribing. Biogen (BIIB) Q2 2022 earnings call transcript. The Motley Fool https://www.fool.com/earnings/call-transcripts/2022/07/20/biogen-biib-q2-2022-earnings-call-transcript/ (2022).
Eisai. Eisai presents data showing quantification of tau microtubule binding region in cerebrospinal fluid and the identification of a target engagement biomarker for the new anti-tau antibody E2814 at Alzheimer’s Association International Conference (AAIC) 2019. Eisai https://www.eisai.com/news/2019/news201955.html (2019).
Talma, S. et al. Efficacy of the murine version of E2814 in a validated AD brain seed-injection model in hTau mice [abstract P4-673]. Presented at the Alzheimer’s Association International Conference, Amsterdam, Netherlands, and Online (2023).
Horie, K., Barthelemy, N. R., Sato, C. & Bateman, R. J. CSF tau microtubule binding region identifies tau tangle and clinical stages of Alzheimer’s disease. Brain 144, 515–527 (2021).
Horie, K. et al. Quantification of the tau microtubule binding region (MTBR) in cerebrospinal fluid and subsequent validation of target engagement assay for E2814, a novel anti-tau therapeutic antibody. Alzheimers Dement. 15(7S Part 31), 1598–1599 (2019).
Alzforum. Aiming at the tangle’s heart? DIAN-TU trial to torpedo tau’s core. Alzforum https://www.alzforum.org/news/research-news/aiming-tangles-heart-dian-tu-trial-torpedo-taus-core (2021).
Zhou, J. et al. E2814: an anti-tau therapy engages its CNS target and affects the downstream tangle-specific biomarker MTBR-tau243 in dominantly inherited Alzheimer’s disease [abstract]. Presented at the Alzheimer’s Association International Conference, Amsterdam, Netherlands, and Online 2023 (2023).
Rawal, S. et al. Safety, pharmacokinetics and immunogenicity of single and multiple ascending doses of the anti-tau therapeutic antibody E2814: a phase 1, first-in-human (FIH) study in healthy subjects [abstract P1-909]. Presented at the Alzheimer’s Association International Conference, Amsterdam, Netherlands, and Online (2023).
Horie, K. et al. CSF MTBR-tau243 is a specific biomarker of tau tangle pathology in Alzheimer’s disease. Nat. Med. 29, 1954–1963 (2023).
Sopko, R. et al. Characterization of tau binding by gosuranemab. Neurobiol. Dis. 146, 105120 (2020).
Alzforum. Therapeutics: Gosuranemab. Alzforum https://www.alzforum.org/therapeutics/gosuranemab (2022).
Qureshi, I. A. et al. A randomized, single ascending dose study of intravenous BIIB092 in healthy participants. Alzheimers Dement. 4, 746–755 (2018).
Boxer, A. L. et al. Safety of the tau-directed monoclonal antibody BIIB092 in progressive supranuclear palsy: a randomised, placebo-controlled, multiple ascending dose phase 1b trial. Lancet Neurol. 18, 549–558 (2019).
Dam, T. et al. Safety and efficacy of anti-tau monoclonal antibody gosuranemab in progressive supranuclear palsy: a phase 2, randomized, placebo-controlled trial. Nat. Med. 27, 1451–1457 (2021).
Biogen. Biogen reports top-line results from phase 2 study in progressive supranuclear palsy. Biogen https://investors.biogen.com/news-releases/news-release-details/biogen-reports-top-line-results-phase-2-study-progressive (2019).
Alzforum. Gosuranemab, Biogen’s anti-tau immunotherapy, does not fly for PSP. Alzforum https://www.alzforum.org/news/research-news/gosuranemab-biogens-anti-tau-immunotherapy-does-not-fly-psp (2019).
Biogen. Biogen announces topline results from phase 2 study of gosuranemab, an anti-tau antibody, for Alzheimer’s disease. Biogen https://investors.biogen.com/news-releases/news-release-details/biogen-announces-topline-results-phase-2-study-gosuranemab-anti (2021).
Alzforum. Therapeutics: JNJ-63733657. Alzforum https://www.alzforum.org/therapeutics/jnj-63733657 (2022).
Galpern, W. R. et al. A single ascending dose study to evaluate the safety, tolerability, pharmacokinetics, and pharmacodynamics of the anti-phospho-tau antibody JNJ-63733657 in healthy subjects [abstract P1-052]. Alzheimers Dement. 15 (7S Part 5), 252–253 (2019).
Helboe, L. et al. Highly specific and sensitive target binding by the humanized pS396-tau antibody hC10.2 across a wide spectrum of Alzheimer’s disease and primary tauopathy postmortem brains. J. Alzheimers Dis. 88, 207–228 (2022).
Umeda, T. et al. Passive immunothrapy of tauopathy targeting pSer413-tau: a pilot study in mice. Ann. Clin. Transl. Neurol. 2, 241–255 (2015).
Alzforum. Therapeutics: MK-2214. Alzforum https://www.alzforum.org/therapeutics/mk-2214 (2023).
Naserkhaki, R. et al. cis pT231-tau drives neurodegeneration in bipolar disorder. ACS Chem. Neurosci. 10, 1214–1221 (2019).
Albayram, O. et al. Cis P-tau is induced in clinical and preclinical brain injury and contributes to post-injury sequelae. Nat. Commun. 8, 1000 (2017).
Mohsenian Sisakht, A. et al. Pathogenic cis p-tau levels in CSF reflects severity of traumatic brain injury. Neurol. Res. 44, 496–502 (2022).
Nakamura, K. et al. Proline isomer-specific antibodies reveal the early pathogenic tau conformation in Alzheimer’s disease. Cell 149, 232–244 (2012).
Qiu, C. et al. Cis P-tau underlies vascular contribution to cognitive impairment and dementia and can be effectively targeted by immunotherapy in mice. Sci. Transl. Med. 13, eaaz7615 (2021).
Alzforum. Therapeutics: PRX005. Alzforum https://www.alzforum.org/therapeutics/prx005 (2023).
Prothena. Prothena reports topline phase 1 single ascending dose study results of PRX005, a novel anti-MTBR-tau antibody for the potential treatment of Alzheimer’s disease. Prothena https://ir.prothena.com/investors/press-releases/news-details/2023/Prothena-Reports-Topline-Phase-1-Single-Ascending-Dose-Study-Results-of-PRX005-a-Novel-Anti-MTBR-Tau-Antibody-for-the-Potential-Treatment-of-Alzheimers-Disease/default.aspx (2023).
Martenyi, F. et al. PRX005, a novel anti-MTBR tau monoclonal antibody: results from a first-in-human double-blind, placebo-controlled, single ascending dose phase 1 study [abstract P1-727]. Presented at the Alzheimer’s Association International Conference, Amsterdam, Netherlands, and Online (2023).
Hasegawa, M. et al. Characterization of mAb AP422, a novel phosphorylation-dependent monoclonal antibody against tau protein. FEBS Lett. 384, 25–30 (1996).
Bussiere, T. et al. Phosphorylated serine422 on tau proteins is a pathological epitope found in several diseases with neurofibrillary degeneration. Acta Neuropathol. 97, 221–230 (1999).
Alzforum. Therapeutics: RG7345. Alzforum https://www.alzforum.org/therapeutics/rg7345 (2015).
Ayalon, G. et al. Antibody semorinemab reduces tau pathology in a transgenic mouse model and engages tau in patients with Alzheimer’s disease. Sci. Transl. Med. 13, eabb2639 (2021).
Kerchner, G. A. et al. A phase I study to evaluate the safety and tolerability of RO7105705 in healthy volunteers and patients with mild-to-moderate AD. Alzheimers Dement. https://doi.org/10.1016/j.jalz.2017.07.243 (2017).
AC Immune. AC Immune reports top line results from TAURIEL phase 2 trial evaluating semorinemab in early Alzheimer’s disease. AC Immune https://ir.acimmune.com/news-releases/news-release-details/ac-immune-reports-top-line-results-tauriel-phase-2-trial (2020).
Alzforum. First cognitive signal that tau immunotherapy works? Alzforum https://www.alzforum.org/news/research-news/first-cognitive-signal-tau-immunotherapy-works (2021).
Monteiro, C. et al. Randomized phase II study of the safety and efficacy of semorinemab in participants with mild-to-moderate Alzheimer disease: Lauriet. Neurology 101, e1391–e1401 (2023).
Alzforum. Therapeutics: Tilvonemab. Alzforum https://www.alzforum.org/therapeutics/tilavonemab (2023).
West, T. et al. Preclinical and clinical development of ABBV-8E12, a humanized anti-tau antibody, for treatment of Alzheimer’s disease and other tauopathies. J. Prev. Alzheimers Dis. 4, 236–241 (2017).
Hoglinger, G. U. et al. Safety and efficacy of tilavonemab in progressive supranuclear palsy: a phase 2, randomised, placebo-controlled trial. Lancet Neurol. 20, 182–192 (2021).
Koga, S., Dickson, D. W. & Wszolek, Z. K. Neuropathology of progressive supranuclear palsy after treatment with tilavonemab. Lancet Neurol. 20, 786–787 (2021).
Alzforum. AbbVie’s tau antibody flops in progressive supranuclear palsy. Alzforum https://www.alzforum.org/news/research-news/abbvies-tau-antibody-flops-progressive-supranuclear-palsy (2019).
Florian, H. et al. Tilavonemab in early Alzheimer’s disease: results from a phase 2, randomized, double-blind study. Brain 146, 2275–2284 (2023).
Chai, X. et al. Passive immunization with anti-tau antibodies in two transgenic models: reduction of tau pathology and delay of disease progression. J. Biol. Chem. 286, 34457–34467 (2011).
Jicha, G. A., Bowser, R., Kazam, I. G. & Davies, P. Alz-50 and MC-1, a new monoclonal antibody raised to paired helical filaments, recognize conformational epitopes on recombinant tau. J. Neurosci. Res. 48, 128–132 (1997).
Vitale, F. et al. Anti-tau conformational scFv MC1 antibody efficiently reduces pathological tau species in adult JNPL3 mice. Acta Neuropathol. Commun. 6, 82 (2018).
Lilly. Q3 2021 earnings call. Lilly https://investor.lilly.com/events/event-details/q3-2021-earnings-call (2021).
Sigurdsson, E. M. Alzheimer’s therapy development: a few points to consider. Prog. Mol. Biol. Transl. Sci. 168, 205–217 (2019).
Han, P. et al. A quantitative analysis of brain soluble tau and the tau secretion factor. J. Neuropathol. Exp. Neurol. 76, 44–51 (2017).
Sato, C. et al. Tau kinetics in neurons and the human central nervous system. Neuron 97, 1284–1298.e7 (2018).
Barthelemy, N. R. et al. Differential mass spectrometry profiles of tau protein in the cerebrospinal fluid of patients with Alzheimer’s disease, progressive supranuclear palsy, and dementia with Lewy bodies. J. Alzheimers Dis. 51, 1033–1043 (2016).
Barthelemy, N. R. et al. Tau protein quantification in human cerebrospinal fluid by targeted mass spectrometry at high sequence coverage provides insights into its primary structure heterogeneity. J. Proteome Res. 15, 667–676 (2016).
Barthelemy, N. R., Mallipeddi, N., Moiseyev, P., Sato, C. & Bateman, R. J. Tau phosphorylation rates measured by mass spectrometry differ in the intracellular brain vs. extracellular cerebrospinal fluid compartments and are differentially affected by Alzheimer’s disease. Front. Aging Neurosci. 11, 121 (2019).
Wagshal, D. et al. Divergent CSF tau alterations in two common tauopathies: Alzheimer’s disease and progressive supranuclear palsy. J. Neurol. Neurosurg. Psychiatry 86, 244–250 (2015).
Hall, S. et al. Accuracy of a panel of 5 cerebrospinal fluid biomarkers in the differential diagnosis of patients with dementia and/or parkinsonian disorders. Arch. Neurol. 69, 1445–1452 (2012).
Hu, W. T., Trojanowski, J. Q. & Shaw, L. M. Biomarkers in frontotemporal lobar degenerations – progress and challenges. Prog. Neurobiol. 95, 636–648 (2011).
Olsson, B. et al. CSF and blood biomarkers for the diagnosis of Alzheimer’s disease: a systematic review and meta-analysis. Lancet Neurol. 15, 673–684 (2016).
Bian, H. et al. CSF biomarkers in frontotemporal lobar degeneration with known pathology. Neurology 70, 1827–1835 (2008).
Grossman, M. et al. Cerebrospinal fluid profile in frontotemporal dementia and Alzheimer’s disease. Ann. Neurol. 57, 721–729 (2005).
Horie, K. et al. CSF tau microtubule-binding region identifies pathological changes in primary tauopathies. Nat. Med. 28, 2547–2554 (2022).
Kanmert, D. et al. C-terminally truncated forms of tau, but not full-length tau or its C-terminal fragments, are released from neurons independently of cell death. J. Neurosci. 35, 10851–10865 (2015).
Jadhav, S. et al. A walk through tau therapeutic strategies. Acta Neuropathol. Commun. 7, 22 (2019).
Zhang, W. et al. Novel tau filament fold in corticobasal degeneration. Nature 580, 283–287 (2020).
Falcon, B. et al. Novel tau filament fold in chronic traumatic encephalopathy encloses hydrophobic molecules. Nature 568, 420–423 (2019).
Scheres, S. H., Zhang, W., Falcon, B. & Goedert, M. Cryo-EM structures of tau filaments. Curr. Opin. Struct. Biol. 64, 17–25 (2020).
Wu, L., Gilyazova, N., Ervin, J. F., Wang, S. J. & Xu, B. Site-specific phospho-tau aggregation-based biomarker discovery for AD diagnosis and differentiation. ACS Chem. Neurosci. 13, 3281–3290 (2022).
Reid, M. J., Beltran-Lobo, P., Johnson, L., Perez-Nievas, B. G. & Noble, W. Astrocytes in tauopathies. Front. Neurol. 11, 572850 (2020).
Kahlson, M. A. & Colodner, K. J. Glial tau pathology in tauopathies: functional consequences. J. Exp. Neurosci. 9, 43–50 (2015).
Ferrer, I. et al. Involvement of oligodendrocytes in tau seeding and spreading in tauopathies. Front. Aging Neurosci. 11, 112 (2019).
Narasimhan, S. et al. Human tau pathology transmits glial tau aggregates in the absence of neuronal tau. J. Exp. Med. 217, e20190783 (2020).
Congdon, E. E. et al. Single domain antibodies targeting pathological tau protein: influence of four IgG subclasses on efficacy and toxicity. eBioMedicine 84, 104249 (2022).
Morell, A., Terry, W. D. & Waldmann, T. A. Metabolic properties of IgG subclasses in man. J. Clin. Invest. 49, 673–680 (1970).
Handlogten, M. W. et al. Prevention of Fab-arm exchange and antibody reduction via stabilization of the IgG4 hinge region. MAbs 12, 1779974 (2020).
Heads, J. T. et al. Electrostatic interactions modulate the differential aggregation propensities of IgG1 and IgG4P antibodies and inform charged residue substitutions for improved developability. Protein Eng. Des. Sel. 32, 277–288 (2019).
Pepinsky, R. B. et al. Improving the solubility of anti-LINGO-1 monoclonal antibody Li33 by isotype switching and targeted mutagenesis. Protein Sci. 19, 954–966 (2010).
Cooper, L. J. et al. Role of heavy chain constant domains in antibody–antigen interaction. Apparent specificity differences among streptococcal IgG antibodies expressing identical variable domains. J. Immunol. 150, 2231–2242 (1993).
Pritsch, O. et al. Can immunoglobulin C(H)1 constant region domain modulate antigen binding affinity of antibodies? J. Clin. Invest. 98, 2235–2243 (1996).
Pritsch, O. et al. Can isotype switch modulate antigen-binding affinity and influence clonal selection? Eur. J. Immunol. 30, 3387–3395 (2000).
Hovenden, M. et al. IgG subclass and heavy chain domains contribute to binding and protection by mAbs to the poly γ-D-glutamic acid capsular antigen of Bacillus anthracis. PLoS Pathog. 9, e1003306 (2013).
Motley, M. P., Diago-Navarro, E., Banerjee, K., Inzerillo, S. & Fries, B. C. The role of IgG subclass in antibody-mediated protection against carbapenem-resistant Klebsiella pneumoniae. mBio 11, e02059-20 (2020).
Tudor, D. et al. Isotype modulates epitope specificity, affinity, and antiviral activities of anti-HIV-1 human broadly neutralizing 2F5 antibody. Proc. Natl Acad. Sci. USA 109, 12680–12685 (2012).
Xia, Y., Janda, A., Eryilmaz, E., Casadevall, A. & Putterman, C. The constant region affects antigen binding of antibodies to DNA by altering secondary structure. Mol. Immunol. 56, 28–37 (2013).
Dam, T. K., Torres, M., Brewer, C. F. & Casadevall, A. Isothermal titration calorimetry reveals differential binding thermodynamics of variable region-identical antibodies differing in constant region for a univalent ligand. J. Biol. Chem. 283, 31366–31370 (2008).
Janda, A. & Casadevall, A. Circular dichroism reveals evidence of coupling between immunoglobulin constant and variable region secondary structure. Mol. Immunol. 47, 1421–1425 (2010).
Kato, K. et al. Carbon-13 NMR study of switch variant anti-dansyl antibodies: antigen binding and domain–domain interactions. Biochemistry 30, 6604–6610 (1991).
McLean, G. R., Torres, M., Elguezabal, N., Nakouzi, A. & Casadevall, A. Isotype can affect the fine specificity of an antibody for a polysaccharide antigen. J. Immunol. 169, 1379–1386 (2002).
Torres, M., Fernandez-Fuentes, N., Fiser, A. & Casadevall, A. The immunoglobulin heavy chain constant region affects kinetic and thermodynamic parameters of antibody variable region interactions with antigen. J. Biol. Chem. 282, 13917–13927 (2007).
Torres, M., Fernandez-Fuentes, N., Fiser, A. & Casadevall, A. Exchanging murine and human immunoglobulin constant chains affects the kinetics and thermodynamics of antigen binding and chimeric antibody autoreactivity. PLoS ONE 2, e1310 (2007).
Torres, M., May, R., Scharff, M. D. & Casadevall, A. Variable-region-identical antibodies differing in isotype demonstrate differences in fine specificity and idiotype. J. Immunol. 174, 2132–2142 (2005).
Xia, Y. et al. The constant region contributes to the antigenic specificity and renal pathogenicity of murine anti-DNA antibodies. J. Autoimmun. 39, 398–411 (2012).
Yuan, R. R. et al. Isotype switching increases efficacy of antibody protection against Cryptococcus neoformans infection in mice. Infect. Immun. 66, 1057–1062 (1998).
Labrijn, A. F. et al. Therapeutic IgG4 antibodies engage in Fab-arm exchange with endogenous human IgG4 in vivo. Nat. Biotechnol. 27, 767–771 (2009).
Young, E. et al. Estimation of polyclonal IgG4 hybrids in normal human serum. Immunology 142, 406–413 (2014).
Boutajangout, A., Quartermain, D. & Sigurdsson, E. M. Immunotherapy targeting pathological tau prevents cognitive decline in a new tangle mouse model. J. Neurosci. 30, 16559–16566 (2010).
d’Abramo, C., Acker, C. M., Jimenez, H. T. & Davies, P. Tau passive immunotherapy in mutant P301L mice: antibody affinity versus specificity. PLoS ONE 8, e62402 (2013).
Hintersteiner, B. et al. Charge heterogeneity: basic antibody charge variants with increased binding to Fc receptors. MAbs 8, 1548–1560 (2016).
Schoch, A. et al. Charge-mediated influence of the antibody variable domain on FcRn-dependent pharmacokinetics. Proc. Natl Acad. Sci. USA 112, 5997–6002 (2015).
Khawli, L. A., Glasky, M. S., Alauddin, M. M. & Epstein, A. L. Improved tumor localization and radioimaging with chemically modified monoclonal antibodies. Cancer Biother. Radiopharm. 11, 203–215 (1996).
Kobayashi, H. et al. The pharmacokinetic characteristics of glycolated humanized anti-Tac Fabs are determined by their isoelectric points. Cancer Res. 59, 422–430 (1999).
Datta-Mannan, A. et al. Balancing charge in the complementarity-determining regions of humanized mAbs without affecting pI reduces non-specific binding and improves the pharmacokinetics. MAbs 7, 483–493 (2015).
Li, B. et al. Framework selection can influence pharmacokinetics of a humanized therapeutic antibody through differences in molecule charge. MAbs 6, 1255–1264 (2014).
Chatterjee, D. et al. Proteasome-targeted nanobodies alleviate pathology and functional decline in an α-synuclein-based Parkinson’s disease model. NPJ Parkinsons Dis. 4, 25 (2018).
Butler, D. C. et al. Bifunctional anti-non-amyloid component α-synuclein nanobodies are protective in situ. PLoS ONE 11, e0165964 (2016).
Lim, S. et al. bioPROTACs as versatile modulators of intracellular therapeutic targets including proliferating cell nuclear antigen (PCNA). Proc. Natl Acad. Sci. USA 117, 5791–5800 (2020).
Ibrahim, A. F. M. et al. Antibody RING-mediated destruction of endogenous proteins. Mol. Cell 79, 155–166.e9 (2020).
Roth, S. et al. Targeting endogenous K-RAS for degradation through the affinity-directed protein missile system. Cell Chem. Biol. 27, 1151–1163.e6 (2020).
Wang, W. et al. A novel small-molecule PROTAC selectively promotes tau clearance to improve cognitive functions in Alzheimer-like models. Theranostics 11, 5279–5295 (2021).
Silva et al. Targeted degradation of aberrant tau in frontotemporal dementia patient-derived neuronal cell models. Elife 8, e45457 (2019).
Chu, T. T. et al. Specific knockdown of endogenous tau protein by peptide-directed ubiquitin-proteasome degradation. Cell Chem. Biol. 23, 453–461 (2016).
Lu, M. et al. Discovery of a Keap1-dependent peptide PROTAC to knockdown Tau by ubiquitination-proteasome degradation pathway. Eur. J. Med. Chem. 146, 251–259 (2018).
Bhatia, S., Singh, M., Singh, T. & Singh, V. Scrutinizing the therapeutic potential of PROTACs in the management of Alzheimer’s disease. Neurochem. Res. 48, 13–25 (2023).
Gallardo, G. et al. Targeting tauopathy with engineered tau-degrading intrabodies. Mol. Neurodegener. 14, 38 (2019).
Butler, D. C. & Messer, A. Bifunctional anti-huntingtin proteasome-directed intrabodies mediate efficient degradation of mutant huntingtin exon 1 protein fragments. PLoS ONE 6, e29199 (2011).
Igawa, T., Haraya, K. & Hattori, K. Sweeping antibody as a novel therapeutic antibody modality capable of eliminating soluble antigens from circulation. Immunol. Rev. 270, 132–151 (2016).
Banik, S. M. et al. Lysosome-targeting chimaeras for degradation of extracellular proteins. Nature 584, 291–297 (2020).
Ahn, G. et al. LYTACs that engage the asialoglycoprotein receptor for targeted protein degradation. Nat. Chem. Biol. 17, 937–946 (2021).
Takahashi, D. et al. AUTACs: cargo-specific degraders using selective autophagy. Mol. Cell 76, 797–810.e10 (2019).
Takahashi, D. & Arimoto, H. Targeting selective autophagy by AUTAC degraders. Autophagy 16, 765–766 (2020).
Sawa, T. et al. Protein S-guanylation by the biological signal 8-nitroguanosine 3′,5′-cyclic monophosphate. Nat. Chem. Biol. 3, 727–735 (2007).
Cotton, A. D., Nguyen, D. P., Gramespacher, J. A., Seiple, I. B. & Wells, J. A. Development of antibody-based PROTACs for the degradation of the cell-surface immune checkpoint protein PD-L1. J. Am. Chem. Soc. 143, 593–598 (2021).
Cha-Molstad, H. et al. p62/SQSTM1/sequestosome-1 is an N-recognin of the N-end rule pathway which modulates autophagosome biogenesis. Nat. Commun. 8, 102 (2017).
Ji, C. H. et al. The AUTOTAC chemical biology platform for targeted protein degradation via the autophagy-lysosome system. Nat. Commun. 13, 904 (2022).
Song, W. et al. Ceria nanoparticles stabilized by organic surface coatings activate the lysosome-autophagy system and enhance autophagic clearance. ACS Nano 8, 10328–10342 (2014).
Sun, H. et al. A tauopathy-homing and autophagy-activating nanoassembly for specific clearance of pathogenic tau in Alzheimer’s disease. ACS Nano 15, 5263–5275 (2021).
Zheng, J. et al. A novel dephosphorylation targeting chimera selectively promoting tau removal in tauopathies. Signal. Transduct. Target. Ther. 6, 269 (2021).
Krishnaswamy, S. et al. In vivo imaging of tauopathy in mice. Methods Mol. Biol. 1779, 513–526 (2018).
Ising, C. et al. AAV-mediated expression of anti-tau scFvs decreases tau accumulation in a mouse model of tauopathy. J. Exp. Med. 214, 1227–1238 (2017).
Nisbet, R. M. et al. Combined effects of scanning ultrasound and a tau-specific single chain antibody in a tau transgenic mouse model. Brain 140, 1220–1230 (2017).
Spencer, B. et al. Selective targeting of 3 repeat Tau with brain penetrating single chain antibodies for the treatment of neurodegenerative disorders. Acta Neuropathol. 136, 69–87 (2018).
Jiang, Y. et al. Single-domain antibody-based noninvasive in vivo imaging of α-synuclein or tau pathology. Sci. Adv. 9, eadf3775 (2023).
Danis, C. et al. Inhibition of Tau seeding by targeting Tau nucleation core within neurons with a single domain antibody fragment. Mol. Ther. 30, 1484–1499 (2022).
Li, T. et al. Camelid single-domain antibodies: a versatile tool for in vivo imaging of extracellular and intracellular brain targets. J. Control. Rel. 243, 1–10 (2016).
Marino, M. & Holt, M. G. AAV vector-mediated antibody delivery (A-MAD) in the central nervous system. Front. Neurol. 13, 870799 (2022).
Chen, Y. H. et al. Administration of AAV-alpha synuclein NAC antibody improves locomotor behavior in rats overexpressing alpha synuclein. Genes 12, 948 (2021).
Butler, Y. R. et al. α-Synuclein fibril-specific nanobody reduces prion-like α-synuclein spreading in mice. Nat. Commun. 13, 4060 (2022).
Chen, Y. H. et al. Downregulation of α-synuclein protein levels by an intracellular single-chain antibody. J. Parkinsons Dis. 10, 573–590 (2020).
Zhou, C., Emadi, S., Sierks, M. R. & Messer, A. A human single-chain Fv intrabody blocks aberrant cellular effects of overexpressed α-synuclein. Mol. Ther. 10, 1023–1031 (2004).
Wang, J. et al. Research progress and applications of multivalent, multispecific and modified nanobodies for disease treatment. Front. Immunol. 12, 838082 (2021).
Jovcevska, I. & Muyldermans, S. The therapeutic potential of nanobodies. Biodrugs 34, 11–26 (2020).
Ghosh, P., Dahms, N. M. & Kornfeld, S. Mannose 6-phosphate receptors: new twists in the tale. Nat. Rev. Mol. Cell Biol. 4, 202–212 (2003).
Gary-Bobo, M., Nirde, P., Jeanjean, A., Morere, A. & Garcia, M. Mannose 6-phosphate receptor targeting and its applications in human diseases. Curr. Med. Chem. 14, 2945–2953 (2007).
Kyttala, A., Heinonen, O., Peltonen, L. & Jalanko, A. Expression and endocytosis of lysosomal aspartylglucosaminidase in mouse primary neurons. J. Neurosci. 18, 7750–7756 (1998).
Hawkes, C. & Kar, S. Insulin-like growth factor-II/mannose-6-phosphate receptor: widespread distribution in neurons of the central nervous system including those expressing cholinergic phenotype. J. Comp. Neurol. 458, 113–127 (2003).
Couce, M. E., Weatherington, A. J. & McGinty, J. F. Expression of insulin-like growth factor-II (IGF-II) and IGF-II/mannose-6-phosphate receptor in the rat hippocampus: an in situ hybridization and immunocytochemical study. Endocrinology 131, 1636–1642 (1992).
Jabbari, E. & Duff, K. E. Tau-targeting antibody therapies: too late, wrong epitope or wrong target? Nat. Med. 27, 1341–1342 (2021).
Bespalov, A., Courade, J. P., Khiroug, L., Terstappen, G. C. & Wang, Y. A call for better understanding of target engagement in Tau antibody development. Drug. Discov. Today 27, 103338 (2022).
Sigurdsson, E. M. T. Immunotherapies for Alzheimer’s disease and related tauopathies: progress and potential pitfalls. J. Alzheimers Dis. 64, S555–S565 (2018).
Wu, Q. et al. Increased neuronal activity in motor cortex reveals prominent calcium dyshomeostasis in tauopathy mice. Neurobiol. Dis. 147, 105165 (2021).
Giacobini, E. & Gold, G. Alzheimer disease therapy – moving from amyloid-β to tau. Nat. Rev. Neurol. 9, 677–686 (2013).
Acknowledgements
The authors were supported by NIH grants R01 AG032611, NS077239, RF1 NS120488, R21 AG069475 and T32 AG052909, and Alzheimer’s Association grants AARF-22-926735 and AARF-22-924783.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
E.M.S. in an inventor on various patents related to the topic of this review that are assigned to New York University. Some of the patents on tau immunotherapies are licensed to H. Lundbeck. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Neurology thanks S. Fowler, who co-reviewed with S. Bez; R. Kayed; and L. Vivash for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Congdon, E.E., Ji, C., Tetlow, A.M. et al. Tau-targeting therapies for Alzheimer disease: current status and future directions. Nat Rev Neurol 19, 715–736 (2023). https://doi.org/10.1038/s41582-023-00883-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41582-023-00883-2
This article is cited by
-
Immunological aspects of central neurodegeneration
Cell Discovery (2024)