Abstract
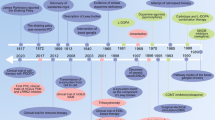
Parkinson disease (PD) treatment options have conventionally focused on dopamine replacement and provision of symptomatic relief. Current treatments cause undesirable adverse effects, and a large unmet clinical need remains for treatments that offer disease modification and that address symptoms resistant to levodopa. Advances in high-throughput drug screening methods for small molecules, developments in disease modelling and improvements in analytical technologies have collectively contributed to the emergence of novel compounds, repurposed drugs and new technologies. In this Review, we focus on disease-modifying and symptomatic therapies under development for PD. We review cellular therapies and repurposed drugs, such as nilotinib, inosine, isradipine, iron chelators and anti-inflammatories, and discuss how their success in preclinical models has paved the way for clinical trials. We provide an update on immunotherapies and vaccines. In addition, we review non-pharmacological interventions targeting motor symptoms, including gene therapy, adaptive deep brain stimulation (DBS) and optogenetically inspired DBS. Given the many clinical phenotypes of PD, individualization of therapy and precision of treatment are likely to become important in the future.
Key points
-
Emerging therapies for Parkinson disease (PD) have focused largely on disease modification and on dopamine resistance symptoms, which are both important unmet needs.
-
Some new disease-modifying therapies target α-synuclein and its pathways, whereas others target different genes and proteins implicated in PD pathogenesis, including leucine-rich repeat kinase 2, parkin and glucocerebrosidase.
-
Disease-modifying pharmacotherapies (such as nilotinib, inosine and isradipine) are being repurposed to treat PD; antibody therapies, vaccines and immune-mediated therapies that aim to clear abnormal proteins have also emerged as promising approaches.
-
Cellular therapies can be divided into rescue and restoration therapies; rescue therapy aims to salvage neurons and slow the progression of the disease whereas restoration therapy focuses on replacing neurons.
-
Adaptive deep brain stimulation is an alternative symptomatic therapy that can be used to target dopamine-responsive and dopamine-resistant symptoms.
-
Current efforts to overcome challenges in therapeutic development have focused on individualization of therapy and precision in treatment; these principles are especially important given the heterogeneity of clinical PD subtypes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Kalia, L. V. & Lang, A. E. Parkinson’s disease. Lancet 386, 896–912 (2015).
Lang, A. E. & Espay, A. J. Disease modification in Parkinson’s disease: current approaches, challenges, and future considerations. Mov. Disord. 33, 660–677 (2018).
Van Rooden, S. M. et al. The identification of Parkinson’s disease subtypes using cluster analysis: a systematic review. Mov. Disord. 25, 969–978 (2010).
Marras, C. & Lang, A. Parkinson’s disease subtypes: lost in translation? J. Neurol. Neurosurg. Psychiatry 84, 409–415 (2013).
Schapira, A. H. V., Chaudhuri, K. R. & Jenner, P. Non-motor features of Parkinson disease. Nat. Rev. Neurosci. 18, 435–450 (2017).
Chaudhuri, K. R., Healy, D. G. & Schapira, A. H. V. Non-motor symptoms of Parkinson’s disease: diagnosis and management. Lancet Neurol. 5, 235–245 (2006).
Pfeiffer, R. F. Non-motor symptoms in Parkinson’s disease. Parkinsonism Relat. Disord. 22, S119–S122 (2016).
Polymeropoulos, M. H. et al. Mutation in the α-synuclein gene identified in families with Parkinson’s disease. Science 276, 2045–2047 (1997).
Spillantini, M. G. et al. α-Synuclein in Lewy bodies. Nature 388, 839–840 (1997).
Bendor, J. T., Logan, T. P. & Edwards, R. H. The function of α-synuclein. Neuron 79, 1044–1066 (2013).
Wong, Y. C. & Krainc, D. α-Synuclein toxicity in neurodegeneration: mechanism and therapeutic strategies. Nat. Med. 23, 1–13 (2017).
Dehay, B. et al. Targeting α-synuclein for treatment of Parkinson’s disease: mechanistic and therapeutic considerations. Lancet Neurol. 14, 855–866 (2015).
Conway, K. A., Harper, J. D. & Lansbury, P. T. Accelerated in vitro fibril formation by a mutant α-synuclein linked to early-onset Parkinson disease. Nat. Med. 4, 1318–1320 (1998).
Cuervo, A. M., Stefanis, L., Fredenburg, R., Lansbury, P. T. & Sulzer, D. Impaired degradation of mutant α-synuclein by chaperone-mediated autophagy. Science 305, 1292–1295 (2004).
Martinez-Vicente, M. et al. Dopamine-modified α-synuclein blocks chaperone-mediated autophagy. J. Clin. Invest. 118, 777–788 (2008).
Chinta, S. J., Mallajosyula, J. K., Rane, A. & Andersen, J. K. Mitochondrial alpha-synuclein accumulation impairs complex I function in dopaminergic neurons and results in increased mitophagy in vivo. Neurosci. Lett. 486, 235–239 (2010).
Guardia-Laguarta, C. et al. α-Synuclein is localized to mitochondria-associated ER membranes. J. Neurosci. 34, 249–259 (2014).
Paillusson, S. et al. α-Synuclein binds to the ER–mitochondria tethering protein VAPB to disrupt Ca2+ homeostasis and mitochondrial ATP production. Acta Neuropathol. 134, 129–149 (2017).
Olanow, C. W. & Kordower, J. H. Targeting α-synuclein as a therapy for Parkinson’s disease: the battle begins. Mov. Disord. 32, 203–207 (2017).
Mittal, S. et al. β2-Adrenoreceptor is a regulator of the alpha-synuclein gene driving risk of Parkinson’s disease. Science 357, 891–898 (2017).
Searles Nielsen, S., Gross, A., Camacho-Soto, A., Willis, A. W. & Racette, B. A. β2-adrenoreceptor medications and risk of Parkinson disease. Ann. Neurol. 84, 683–693 (2018).
Webb, J. L., Ravikumar, B., Atkins, J., Skepper, J. N. & Rubinsztein, D. C. α-Synuclein is degraded by both autophagy and the proteasome. J. Biol. Chem. 278, 25009–25013 (2003).
Lee, B. H. et al. Enhancement of proteasome activity by a small-molecule inhibitor of USP14. Nature 467, 179–184 (2010).
Dehay, B. et al. Pathogenic lysosomal depletion in Parkinson’s disease. J. Neurosci. 30, 12535–12544 (2010).
Torra, A. et al. Overexpression of TFEB drives a pleiotropic neurotrophic effect and prevents Parkinson’s disease-related neurodegeneration. Mol. Ther. 26, 1552–1567 (2018).
Xilouri, M., Brekk, O. R., Kirik, D. & Stefanis, L. LAMP2A as a therapeutic target in Parkinson disease. Autophagy 9, 2166–2168 (2013).
Spencer, B. et al. Beclin 1 gene transfer activates autophagy and ameliorates the neurodegenerative pathology in -synuclein models of Parkinson’s and Lewy body diseases. J. Neurosci. 29, 13578–13588 (2009).
Malagelada, C., Jin, Z. H., Jackson-Lewis, V., Przedborski, S. & Greene, L. A. Rapamycin protects against neuron death in in vitro and in vivo models of Parkinson’s disease. J. Neurosci. 30, 1166–1175 (2010).
Karuppagounder, S. S. et al. The c-Abl inhibitor, nilotinib, protects dopaminergic neurons in a preclinical animal model of Parkinson’s disease. Sci. Rep. 4, 4874 (2014).
Pagan, F. et al. Nilotinib effects in Parkinson’s disease and dementia with lewy bodies. J. Parkinsons Dis. 6, 503–517 (2016).
Simuni, T. et al. A phase 2a study of nilotinib in patients with advanced and early Parkinson’s disease. study design [abstract]. Mov. Disord. 33 (Suppl. 2), 238 (2018).
Savolainen, M. H. et al. The beneficial effect of a prolyl oligopeptidase inhibitor, KYP-2047, on α-synuclein clearance and autophagy in A30P transgenic mouse. Neurobiol. Dis. 68, 1–15 (2014).
Myöhänen, T. T. et al. A prolyl oligopeptidase inhibitor, KYP-2047, reduces α-synuclein protein levels and aggregates in cellular and animal models of Parkinson’s disease. Br. J. Pharmacol. 166, 1097–1113 (2012).
Perni, M. et al. A natural product inhibits the initiation of α-synuclein aggregation and suppresses its toxicity. Proc. Natl Acad. Sci. USA 114, E1009–E1017 (2017).
Richter, F. et al. A molecular tweezer ameliorates motor deficits in mice overexpressing α-synuclein. Neurotherapeutics 14, 1107–1119 (2017).
Recasens, A. et al. Lewy body extracts from Parkinson disease brains trigger α-synuclein pathology and neurodegeneration in mice and monkeys. Ann. Neurol. 75, 351–362 (2014).
Kordower, J. H., Chu, Y., Hauser, R. A., Freeman, T. B. & Olanow, C. W. Lewy body-like pathology in long-term embryonic nigral transplants in Parkinson’s disease. Nat. Med. 14, 504–506 (2008).
Volpicelli-Daley, L. A. et al. Exogenous α-synuclein fibrils induce Lewy body pathology leading to synaptic dysfunction and neuron death. Neuron 72, 57–71 (2011).
Paumier, K. L. et al. Intrastriatal injection of pre-formed mouse α-synuclein fibrils into rats triggers α-synuclein pathology and bilateral nigrostriatal degeneration. Neurobiol. Dis. 82, 185–199 (2015).
Mao, X. et al. Pathological α-synuclein transmission initiated by binding lymphocyte-activation gene 3. Science 353, aah3374 (2016).
Masliah, E. et al. Effects of α-synuclein immunization in a mouse model of Parkinson’s disease. Neuron 46, 857–868 (2005).
Masliah, E. et al. Passive immunization reduces behavioral and neuropathological deficits in an alpha-synuclein transgenic model of lewy body disease. PLOS ONE 6, e19338 (2011).
Bae, E.-J. et al. Antibody-aided clearance of extracellular -synuclein prevents cell-to-cell aggregate transmission. J. Neurosci. 32, 13454–13469 (2012).
Mandler, M. et al. Next-generation active immunization approach for synucleinopathies: Implications for Parkinson’s disease clinical trials. Acta Neuropathol. 127, 861–879 (2014).
Jankovic, J. et al. Safety and tolerability of multiple ascending doses of PRX002/RG7935, an anti—synuclein monoclonal antibody, in patients with Parkinson disease: a randomized clinical trial. JAMA Neurol. 75, 1206–1214 (2018).
Schneeberger, A., Tierney, L. & Mandler, M. Active immunization therapies for Parkinson’s disease and multiple system atrophy. Mov. Disord. 31, 214–224 (2016).
Poulopoulos, M., Levy, O. A. & Alcalay, R. N. The neuropathology of genetic Parkinson’s disease. Mov. Disord. 27, 831–842 (2012).
Doherty, K. M. et al. Parkin disease: a clinicopathologic entity? JAMA Neurol. 70, 571–579 (2013).
Blanz, J. & Saftig, P. Parkinson’s disease: acid-glucocerebrosidase activity and alpha-synuclein clearance. J. Neurochem. 139 (Suppl. 1), 198–215 (2016).
Frigerio, R. et al. Incidental Lewy body disease: do some cases represent a preclinical stage of dementia with Lewy bodies? Neurobiol. Aging 32, 857–863 (2011).
West, A. B. Achieving neuroprotection with LRRK2 kinase inhibitors in Parkinson disease. Exp. Neurol. 298, 236–245 (2017).
Satake, W. et al. Genome-wide association study identifies common variants at four loci as genetic risk factors for Parkinson’s disease. Nat. Genet. 41, 1303–1307 (2009).
Simón-Sánchez, J. et al. Genome-wide association study reveals genetic risk underlying Parkinson’s disease. Nat. Genet. 41, 1308–1312 (2009).
Nalls, M. A. et al. Large-scale meta-analysis of genome-wide association data identifies six new risk loci for Parkinson’s disease. Nat. Genet. 46, 989–993 (2014).
Martin, I., Kim, J. W., Dawson, V. L. & Dawson, T. M. LRRK2 pathobiology in Parkinson’s disease. J. Neurochem. 131, 554–565 (2014).
Esteves, A. R., Swerdlow, R. H. & Cardoso, S. M. LRRK2, a puzzling protein: insights into Parkinson’s disease pathogenesis. Exp. Neurol. 261, 206–216 (2014).
Cresto, N. et al. The unlikely partnership between LRRK2 and α-synuclein in Parkinson’s disease. Eur. J. Neurosci. https://doi.org/10.1111/ejn.14182 (2018).
Henderson, M. X., Peng, C., Trojanowski, J. Q. & Lee, V. M. Y. LRRK2 activity does not dramatically alter α-synuclein pathology in primary neurons. Acta Neuropathol. Commun. 6, 45 (2018).
Healy, D. G. et al. Phenotype, genotype, and worldwide genetic penetrance of LRRK2-associated Parkinson’s disease: a case-control study. Lancet Neurol. 7, 583–590 (2008).
Sardi, S. P., Cedarbaum, J. M. & Brundin, P. Targeted therapies for Parkinson’s disease: from genetics to the clinic. Mov. Disord. 33, 684–696 (2018).
Ness, D. et al. Leucine-rich repeat kinase 2 (LRRK2)-deficient rats exhibit renal tubule injury and perturbations in metabolic and immunological homeostasis. PLOS ONE 8, e66164 (2013).
Herzig, M. C. et al. LRRK2 protein levels are determined by kinase function and are crucial for kidney and lung homeostasis in mice. Hum. Mol. Genet. 20, 4209–4223 (2011).
Fuji, R. N. et al. Effect of selective LRRK2 kinase inhibition on nonhuman primate lung. Sci. Transl Med. 7, 273ra15 (2015).
Fan, Y. et al. Interrogating Parkinson’s disease LRRK2 kinase pathway activity by assessing Rab10 phosphorylation in human neutrophils. Biochem. J. 475, 23–44 (2017).
Di Maio, R. et al. LRRK2 activation in idiopathic Parkinson’s disease. Sci. Transl Med. 10, eaar5429 (2018).
Tayebi, N. et al. Gaucher disease with parkinsonian manifestations: Does glucocerebrosidase deficiency contribute to a vulnerability to parkinsonism? Mol. Genet. Metab. 79, 104–109 (2003).
Sidransky, E. et al. Multicenter analysis of glucocerebrosidase mutations in Parkinson’s disease. N. Engl. J. Med. 361, 1651–1661 (2009).
Brockmann, K. et al. GBA-associated Parkinson’s disease: reduced survival and more rapid progression in a prospective longitudinal study. Mov. Disord. 30, 407–411 (2015).
Choi, J. H. et al. Aggregation of α-synuclein in brain samples from subjects with glucocerebrosidase mutations. Mol. Genet. Metab. 104, 185–188 (2011).
Mazzulli, J. R. et al. Gaucher disease glucocerebrosidase and α-synuclein form a bidirectional pathogenic loop in synucleinopathies. Cell 146, 37–52 (2011).
Bendikov-Bar, I., Maor, G., Filocamo, M. & Horowitz, M. Ambroxol as a pharmacological chaperone for mutant glucocerebrosidase. Blood Cells Mol. Dis. 50, 141–145 (2013).
Lieberman, R. L., D’Aquino, J. A., Ringe, D. & Petsko, G. A. Effects of pH and iminosugar pharmacological chaperones on lysosomal glycosidase structure and stability. Biochemistry 48, 4816–4827 (2009).
McNeill, A. et al. Ambroxol improves lysosomal biochemistry in glucocerebrosidase mutation-linked Parkinson disease cells. Brain 137, 1481–1495 (2014).
Sardi, S. P. et al. Glucosylceramide synthase inhibition alleviates aberrations in synucleinopathy models. Proc. Natl Acad. Sci. USA 114, 2699–2704 (2017).
Double, D. L., Reyes, R., Werry, W. L. & Halliday, H. M. Selective cell death in neurodegeneration: why are some neurons spared in vulnerable regions? Prog. Neurobiol. 92, 316–329 (2010).
Surmeier, D. J., Obeso, J. A. & Halliday, G. M. Selective neuronal vulnerability in Parkinson disease. Nat. Rev. Neurosci. 18, 101–113 (2017).
Pacelli, C. et al. Elevated mitochondrial bioenergetics and axonal arborization size are key contributors to the vulnerability of dopamine neurons. Curr. Biol. 25, 2349–2360 (2015).
Surmeier, D. J. & Schumacker, P. T. Calcium, bioenergetics, and neuronal vulnerability in Parkinson’s disease. J. Biol. Chem. 288, 10736–10741 (2013).
Sanchez-Padilla, J. et al. Mitochondrial oxidant stress in locus coeruleus is regulated by activity and nitric oxide synthase. Nat. Neurosci. 17, 832–840 (2014).
Guzman, J. N. et al. Oxidant stress evoked by pacemaking in dopaminergic neurons is attenuated by DJ-1. Nature 468, 696–700 (2010).
Goldberg, J. A. et al. Calcium entry induces mitochondrial oxidant stress in vagal neurons at risk in Parkinson’s disease. Nat. Neurosci. 15, 1414–1421 (2012).
Gudala, K., Kanukula, R. & Bansal, D. Reduced risk of Parkinson’s disease in users of calcium channel blockers: a meta-analysis. Int. J. Chronic Dis. 2015, 697404 (2015).
Oakley, A. E. et al. Individual dopaminergic neurons show raised iron levels in Parkinson disease. Neurology 68, 1820–1825 (2007).
Ward, R. J., Zucca, F. A., Duyn, J. H., Crichton, R. R. & Zecca, L. The role of iron in brain ageing and neurodegenerative disorders. Lancet Neurol. 13, 1045–1060 (2014).
Dexter, D. T. et al. Clinically available iron chelators induce neuroprotection in the 6-OHDA model of Parkinson’s disease after peripheral administration. J. Neural Transm. 118, 223–231 (2011).
Martin-Bastida, A. et al. Brain iron chelation by deferiprone in a phase 2 randomised double-blinded placebo controlled clinical trial in Parkinson’s disease. Sci. Rep. 7, 1398 (2017).
Ton, T. G. et al. Nonsteroidal anti-inflammatory drugs and risk of Parkinson’s disease. Mov. Disord. 21, 964–969 (2006).
Gagne, J. J. & Power, M. C. Anti-inflammatory drugs and risk of Parkinson disease: a meta-analysis. Neurology 74, 995–1002 (2010).
McGeer, P. L., Itagaki, S., Boyes, B. E. & McGeer, E. G. Reactive microglia are positive for HLA-DR in the substantia nigra of Parkinson’s and Alzheimer’s disease brains. Neurology 38, 1285–1285 (1988).
Mogi, M. et al. Interleukin-1β, interleukin-6, epidermal growth factor and transforming growth factor-α are elevated in the brain from parkinsonian patients. Neurosci. Lett. 180, 147–150 (1994).
Hirsch, E. C. & Hunot, S. Neuroinflammation in Parkinson’s disease: a target for neuroprotection? Lancet Neurol. 8, 382–397 (2009).
Dobbs, R. J. et al. Association of circulating TNF-α and IL-6 with ageing and parkinsonism. Acta Neurol. Scand. 100, 34–41 (1999).
Blum-Degena, D. et al. Interleukin-1β and interleukin-6 are elevated in the cerebrospinal fluid of Alzheimer’s and de novo Parkinson’s disease patients. Neurosci. Lett. 202, 17–20 (1995).
Mosley, R. L., Hutter-Saunders, J. A., Stone, D. K. & Gendelman, H. E. Inflammation and adaptive immunity in Parkinson’s disease. Cold Spring Harb. Perspect. Med. 2, a009381 (2012).
Wahner, A. D., Bronstein, J. M., Bordelon, Y. M. & Ritz, B. Nonsteroidal anti-inflammatory drugs may protect against Parkinson disease. Neurology 69, 1836–1842 (2007).
Samii, A., Etminan, M., Wiens, M. O. & Jafari, S. NSAID use and the risk of parkinsons disease: systematic review and meta-analysis of observational studies. Drugs Aging 26, 769–779 (2009).
Gao, X., Chen, H., Schwarzschild, M. A. & Ascherio, A. Use of ibuprofen and risk of Parkinson disease. Neurology 76, 863–869 (2011).
Shameli, A. et al. A critical role for α-synuclein in development and function of T lymphocytes. Immunobiology 221, 333–340 (2016).
Smith, T. J. et al. 2006 update of recommendations for the use of white blood cell growth factors: an evidence-based clinical practice guideline. J. Clin. Oncol. 24, 3187–3205 (2006).
Gendelman, H. E. et al. Evaluation of the safety and immunomodulatory effects of sargramostim in a randomized, double-blind phase 1 clinical Parkinson’s disease trial. NPJ Parkinsons Dis. 3, 10 (2017).
Gellhaar, S., Sunnemark, D., Eriksson, H., Olson, L. & Galter, D. Myeloperoxidase-immunoreactive cells are significantly increased in brain areas affected by neurodegeneration in Parkinson’s and Alzheimer’s disease. Cell Tissue Res. 369, 445–454 (2017).
Ouchi, Y. et al. Microglial activation and dopamine terminal loss in early Parkinson’s disease. Ann. Neurol. 57, 168–175 (2005).
Gerhard, A. et al. In vivo imaging of microglial activation with [11C](R)-PK11195 PET in idiopathic Parkinson’s disease. Neurobiol. Dis. 21, 404–412 (2006).
Posener, J. A. et al. Safety, tolerability, and pharmacodynamics of AZD3241, a myeloperoxidase inhibitor, in Parkinson’s disease [abstract]. Mov. Disord. 29 (Suppl. 1), 698 (2014).
Jucaite, A. et al. Effect of the myeloperoxidase inhibitor AZD3241 on microglia: a PET study in Parkinson’s disease. Brain 138, 2687–2700 (2015).
Harkavyi, A. et al. Glucagon-like peptide 1 receptor stimulation reverses key deficits in distinct rodent models of Parkinson’s disease. J. Neuroinflammation 5, 19 (2008).
Athauda, D. & Foltynie, T. The glucagon-like peptide 1 (GLP) receptor as a therapeutic target in Parkinson’s disease: mechanisms of action. Drug Discov. Today 21, 802–818 (2016).
Athauda, D. et al. Exenatide once weekly versus placebo in Parkinson’s disease: a randomised, double-blind, placebo-controlled trial. Lancet 390, 1664–1675 (2017).
Yin, F., Boveris, A. & Cadenas, E. Mitochondrial energy metabolism and redox signaling in brain aging and neurodegeneration. Antioxid. Redox Signal. 20, 353–371 (2014).
Twig, G. & Shirihai, O. S. The interplay between mitochondrial dynamics and mitophagy. Antioxid. Redox Signal. 14, 1939–1951 (2011).
Wang, W. et al. Parkinson’s disease-associated mutant VPS35 causes mitochondrial dysfunction by recycling DLP1 complexes. Nat. Med. 22, 54–63 (2016).
Corona, J. C. & Duchen, M. R. PPARγ and PGC-1α as therapeutic targets in Parkinson’s. Neurochem. Res. 40, 308–316 (2014).
Pinto, M. et al. Pioglitazone ameliorates the phenotype of a novel Parkinson’s disease mouse model by reducing neuroinflammation. Mol. Neurodegener. 11, 25 (2016).
Simuni, T. et al. Pioglitazone in early Parkinson’s disease: a phase 2, multicentre, double-blind, randomised trial. Lancet Neurol. 14, 795–803 (2015).
De Lau, L. M. L., Koudstaal, P. J., Hofman, A. & Breteler, M. M. B. Serum uric acid levels and the risk of Parkinson disease. Ann. Neurol. 58, 797–800 (2005).
Weisskopf, M. G., O’Reilly, E., Chen, H., Schwarzschild, M. A. & Ascherio, A. Plasma urate and risk of Parkinson’s disease. Am. J. Epidemiol. 166, 561–567 (2007).
Gong, L. et al. Neuroprotection by urate on 6-OHDA-lesioned rat model of Parkinson’s disease: linking to Akt/GSK3β signaling pathway. J. Neurochem. 123, 876–885 (2012).
Schwarzschild, M. A. et al. Inosine to increase serum and cerebrospinal fluid urate in parkinson disease a randomized clinical trial. JAMA Neurol. 71, 141–150 (2014).
Helmich, R. C., Janssen, M. J. R., Oyen, W. J. G., Bloem, B. R. & Toni, I. Pallidal dysfunction drives a cerebellothalamic circuit into Parkinson tremor. Ann. Neurol. 69, 269–281 (2011).
Doder, M., Rabiner, E. A., Turjanski, N., Lees, A. J. & Brooks, D. J. Tremor in Parkinson’s disease and serotonergic dysfunction: An11C-WAY 100635 PET study. Neurology 60, 601–605 (2003).
Katzenschlager, R., Sampaio, C., Costa, J. & Lees, A. Anticholinergics for symptomatic management of Parkinson’s disease. Cochrane Database Syst. Rev. 2, CD003735 (2002).
Friedman, J. H. et al. Benztropine versus clozapine for the treatment of tremor in Parkinson’s disease. Neurology 48, 1077–1081 (1997).
Thomas, A. A. & Friedman, J. H. Current use of clozapine in Parkinson disease and related disorders. Clin. Neuropharmacol. 33, 14–16 (2010).
Yaw, T. K., Fox, S. H. & Lang, A. E. Clozapine in Parkinsonian rest tremor: a review of outcomes, adverse reactions, and possible mechanisms of action. Mov. Disord. Clin. Pract. 3, 116–124 (2016).
Foster, N. L. et al. Peripheral beta-adrenergic blockade treatment of parkinsonian tremor. Ann. Neurol. 16, 505–508 (1984).
Connolly, B. S. & Lang, A. E. Pharmacological treatment of Parkinson disease: a review. JAMA 311, 1670–1683 (2014).
Snijders, A. H. et al. Physiology of freezing of gait. Ann. Neurol. 80, 644–659 (2016).
Henderson, E. J. et al. Rivastigmine for gait stability in patients with Parkinson’s disease (ReSPonD): a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Neurol. 15, 249–258 (2016).
Chung, K. A., Lobb, B. M., Nutt, J. G. & Horak, F. B. Effects of a central cholinesterase inhibitor on reducing falls in Parkinson disease. Neurology 75, 1263–1269 (2010).
Moreau, C. et al. Methylphenidate for gait hypokinesia and freezing in patients with Parkinson’s disease undergoing subthalamic stimulation: a multicentre, parallel, randomised, placebo-controlled trial. Lancet Neurol. 11, 589–596 (2012).
Ahlskog, J. E. & Muenter, M. D. Frequency of levodopa-related dyskinesias and motor fluctuations as estimated from the cumulative literature. Mov. Disord. 16, 448–458 (2001).
Hodgson, R. A. et al. Preladenant, a selective A2Areceptor antagonist, is active in primate models of movement disorders. Exp. Neurol. 225, 384–390 (2010).
Hauser, R. et al. Phase-3 clinical trials of adjunctive therapy with preladenant, an adenosine 2a antagonist, in patients with Parkinson’s disease [abstract]. Neurology 82 (Suppl. 10), P7.087 (2014).
Hauser, R. A. et al. Preladenant as an adjunctive therapy with levodopa in Parkinson disease: two randomized clinical trials and lessons learned. JAMA Neurol. 72, 1491–1500 (2015).
Stocchi, F. et al. Randomized trial of preladenant, given as monotherapy, in patients with early Parkinson disease. Neurology 88, 2198–2206 (2017).
Fernandez, H. H. et al. Istradefylline as monotherapy for Parkinson disease: results of the 6002-US-051 trial. Parkonsonism Relat. Disord. 16, 16–20 (2010).
LeWitt, P. A. et al. Adenosine A2A receptor antagonist istradefylline (KW-6002) reduces off time in Parkinson’s disease: a double-blind, randomized, multicenter clinical trial (6002-US-005). Ann. Neurol. 63, 295–302 (2008).
Hauser, R. A. et al. Study of istradefylline in patients with Parkinson’s disease on levodopa with motor fluctuations. Mov. Disord. 23, 2177–2185 (2008).
Sako, W., Murakami, N., Motohama, K., Izumi, Y. & Kaji, R. The effect of istradefylline for Parkinson’s disease: a meta-analysis. Sci. Rep. 7, 18018 (2017).
Carta, M., Carlsson, T., Muñoz, A., Kirik, D. & Björklund, A. Role of serotonin neurons in the induction of levodopa- and graft-induced dyskinesias in Parkinson’s disease. Mov. Disord. 25, S174–179 (2010).
Bibbiani, F., Oh, J. D. & Chase, T. N. Serotonin 5-HT1A agonist improves motor complications in rodent and primate parkinsonian models. Neurology 57, 1829–1834 (2001).
Luginger, E., Wenning, G., Bösch, S. & Poewe, W. Beneficial effects of amantadine on L-dopa-induced dyskinesias in Parkinson’s disease. Mov. Disord. 15, 873–878 (2000).
Picconi, B., Hernández, L. F., Obeso, J. A. & Calabresi, P. Motor complications in Parkinson’s disease: striatal molecular and electrophysiological mechanisms of dyskinesias. Mov. Disord. 33, 867–876 (2018).
Lentz, T. B., Gray, S. J. & Samulski, R. J. Viral vectors for gene delivery to the central nervous system. Neurobiol. Dis. 48, 179–188 (2012).
Eberling, J. L. et al. Results from a phase I safety trial of hAADC gene therapy for Parkinson disease. Neurology 70, 1980–1983 (2008).
LeWitt, P. A. et al. AAV2-GAD gene therapy for advanced Parkinson’s disease: a double-blind, sham-surgery controlled, randomised trial. Lancet Neurol. 10, 309–319 (2011).
Christine, C. W. et al. Safety and tolerability of putaminal AADC gene therapy for Parkinson disease. Neurology 73, 1662–1669 (2009).
Sánchez-Pernaute, R., Harvey-White, J., Cunningham, J. & Bankiewicz, K. S. Functional effect of adeno-associated virus mediated gene transfer of aromatic L-amino acid decarboxylase into the striatum of 6-OHDA-lesioned rats. Mol. Ther. 4, 324–330 (2001).
Fan, D.-S. et al. Behavioral recovery in 6-hydroxydopamine-lesioned rats by cotransduction of striatum with tyrosine hydroxylase and aromatic-amino acid decarboxylase genes using two separate adeno-associated virus vectors. Hum. Gene Ther. 9, 2527–2535 (1998).
Christine, C. W. et al. VY-AADC01 in medically refractory Parkinson’s disease: safety and efficacy of a phase 1b dose-ranging study 12 months and beyond [abstract]. Ann. Neurol. 84, S1–S280 (2018).
Emborg, M. E. et al. Subthalamic glutamic acid decarboxylase gene therapy: changes in motor function and cortical metabolism. J. Cereb. Blood Flow Metab. 27, 501–509 (2007).
Niethammer, M. et al. Long-term follow-up of a randomized AAV2- GAD gene therapy trial for Parkinson’s disease. JCI Insight 2, e90133 (2017).
Rosenblad, C. Protection and regeneration of nigral dopaminergic neurons by neurturin or GDNF in a partial lesion model of Parkinson’s disease after administration into the striatum or the lateral ventricle. Eur. J. Neurosci. 11, 1554–1566 (1999).
Rosenblad, C., Kirik, D. & Bjorklund, A. Neurturin enhances the survival of intrastriatal fetal dopaminergic transplants. Neuroreport 10, 1783–1787 (1999).
Lin, L. F. H., Doherty, D. H., Lile, J. D., Bektesh, S. & Collins, F. GDNF: a glial cell line - derived neurotrophic factor for midbrain dopaminergic neurons. Science 260, 1130–1132 (1993).
Miyoshi, Y. et al. Glial cell line-derived neurotrophic factor-levodopa interactions and reduction of side effects in parkinsonian monkeys. Ann. Neurol. 42, 208–214 (1997).
Zhang, Z. et al. Dose response to intraventricular glial cell line-derived neurotrophic factor administration in parkinsonian monkeys. J. Pharmacol. Exp. Ther. 282, 1396–1401 (1997).
Kotzbauer, P. T. et al. Neurturin, a relative of glial-cell-line-derived neurotrophic factor. Nature 384, 467–470 (1996).
Gasmi, M. et al. AAV2-mediated delivery of human neurturin to the rat nigrostriatal system: Long-term efficacy and tolerability of CERE-120 for Parkinson’s disease. Neurobiol. Dis. 27, 67–76 (2007).
Herzog, C. D. et al. Striatal delivery of CERE-120, an AAV2 vector encoding human neurturin, enhances activity of the dopaminergic nigrostriatal system in aged monkeys. Mov. Disord. 22, 1124–1132 (2007).
Kordower, J. H. et al. Delivery of neurturin by AAV2 (CERE-120)-mediated gene transfer provides structural and functional neuroprotection and neurorestoration in MPTP-treated monkeys. Ann. Neurol. 60, 706–715 (2006).
Marks, W. J. et al. Safety and tolerability of intraputaminal delivery of CERE-120 (adeno-associated virus serotype 2-neurturin) to patients with idiopathic Parkinson’s disease: an open-label, phase I trial. Lancet Neurol. 7, 400–408 (2008).
Marks, W. J. et al. Gene delivery of AAV2-neurturin for Parkinson’s disease: a double-blind, randomised, controlled trial. Lancet Neurol. 9, 1164–1172 (2010).
Lindholm, P. et al. Novel neurotrophic factor CDNF protects and rescues midbrain dopamine neurons in vivo. Nature 448, 73–77 (2007).
Tsukahara, T., Takeda, M., Shimohama, S., Ohara, O. & Hashimoto, N. Effects of brain-derived neurotrophic factor on 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-induced parkinsonism in monkeys. Neurosurgery 37, 733–741 (1995).
Yasuhara, T. et al. Neuroprotective effects of vascular endothelial growth factor (VEGF) upon dopaminergic neurons in a rat model of Parkinson’s disease. Eur. J. Neurosci. 19, 1494–1504 (2004).
Barker, R. A., Drouin-Ouellet, J. & Parmar, M. Cell-based therapies for Parkinson disease-past insights and future potential. Nat. Rev. Neurol. 11, 492–503 (2015).
Barker, R. A., Barrett, J., Mason, S. L. & Björklund, A. Fetal dopaminergic transplantation trials and the future of neural grafting in Parkinson’s disease. Lancet Neurol. 12, 85–91 (2013).
Lindvall, O. et al. Grafts of fetal dopamine neurons survive and improve motor function in Parkinson’s disease. Science 247, 574–577 (1990).
Ma, Y. et al. Dyskinesia after fetal cell transplantation for parkinsonism: a PET study. Ann. Neurol. 52, 628–634 (2002).
Freed, C. R. et al. Transplantation of embryonic dopamine neurons for severe Parkinson’s disease. N. Engl. J. Med. 344, 710–719 (2001).
Olanow, C. W. et al. A double-blind controlled trial of bilateral fetal nigral transplantation in Parkinson’s disease. Ann. Neurol. 54, 403–414 (2003).
Roy, N. S. et al. Functional engraftment of human ES cell-derived dopaminergic neurons enriched by coculture with telomerase-immortalized midbrain astrocytes. Nat. Med. 12, 1259–1268 (2006).
Kriks, S. et al. Dopamine neurons derived from human ES cells efficiently engraft in animal models of Parkinson’s disease. Nature 480, 547–551 (2011).
Grealish, S. et al. Human ESC-derived dopamine neurons show similar preclinical efficacy and potency to fetal neurons when grafted in a rat model of Parkinson’s disease. Cell Stem Cell 15, 653–665 (2014).
Takahashi, K. & Yamanaka, S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126, 663–676 (2006).
Kikuchi, T. et al. Human iPS cell-derived dopaminergic neurons function in a primate Parkinson’s disease model. Nature 548, 592–596 (2017).
Barker, R. A., Parmar, M., Studer, L. & Takahashi, J. Human trials of stem cell-derived dopamine neurons for Parkinson’s disease: dawn of a new era. Cell Stem Cell 21, 569–573 (2017).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03119636 (2017).
Okun, M. S. Deep-brain stimulation — entering the era of human neural-network modulation. N. Engl. J. Med. 371, 1369–1373 (2014).
Williams, A. et al. Deep brain stimulation plus best medical therapy versus best medical therapy alone for advanced Parkinson’s disease (PD SURG trial): a randomised, open-label trial. Lancet Neurol. 9, 581–591 (2010).
Weaver, F. M. et al. Bilateral deep brain stimulation versus best medical therapy for patients with advanced Parkinson disease: a randomized controlled trial. JAMA 301, 63–73 (2009).
Okun, M. S. et al. Cognition and mood in Parkinson’s disease in subthalamic nucleus versus globus pallidus interna deep brain stimulation: the COMPARE trial. Ann. Neurol. 65, 586–595 (2009).
Deuschl, G. et al. A randomized trial of deep-brain stimulation for Parkinson’s disease. N. Engl. J. Med. 355, 896–908 (2006).
Follett, K. A. et al. Pallidal versus subthalamic deep-brain stimulation for Parkinson’s disease. N. Engl. J. Med. 362, 2077–2091 (2010).
Grabli, D. et al. Gait disorders in parkinsonian monkeys with pedunculopontine nucleus lesions: a tale of two systems. J. Neurosci. 33, 11986–11993 (2013).
Hickey, P. & Stacy, M. Deep brain stimulation: a paradigm shifting approach to treat Parkinson’s disease. Front. Neurosci. 10, 173 (2016).
Jenkinson, N., Nandi, D., Miall, R. C., Stein, J. F. & Aziz, T. Z. Pedunculopontine nucleus stimulation improves akinesia in a Parkinsonian monkey. Neuroreport 15, 2621–2624 (2004).
Stefani, A. et al. Bilateral deep brain stimulation of the pedunculopontine and subthalamic nuclei in severe Parkinson’s disease. Brain 130, 1596–1607 (2007).
Plaha, P. & Gill, S. S. Bilateral deep brain stimulation of the pedunculopontine nucleus for Parkinson’s disease. Neuroreport 16, 1883–1887 (2005).
Chastan, N. et al. Effects of nigral stimulation on locomotion and postural stability in patients with Parkinson’s disease. Brain 132, 172–184 (2009).
Weiss, D. et al. Nigral stimulation for resistant axial motor impairment in Parkinson’s disease? A randomized controlled trial. Brain 136, 2098–2108 (2013).
Quinn, E. J. et al. Beta oscillations in freely moving Parkinson’s subjects are attenuated during deep brain stimulation. Mov. Disord. 30, 1750–1758 (2015).
Grossman, N. et al. Noninvasive deep brain stimulation via temporally interfering electric fields. Cell 169, 1029–1041 (2017).
Gittis, A. Probing new targets for movement disorders. Science 361, 462 (2018).
Chen, S. et al. Near-infrared deep brain stimulation via upconversion nanoparticle–mediated optogenetics. Science 359, 679–684 (2018).
Fischer, D. L. et al. Subthalamic nucleus deep brain stimulation does not modify the functional deficits or axonopathy induced by nigrostriatal α-synuclein overexpression. Sci. Rep. 7, 16356 (2017).
van Horne, C. G. et al. Implantation of autologous peripheral nerve grafts into the substantia nigra of subjects with idiopathic Parkinson’s disease treated with bilateral STN DBS: a report of safety and feasibility. J. Neurosurg. 126, 1140–1147 (2017).
Braak, H. et al. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol. Aging 24, 197–211 (2003).
Mortiboys, H., Aasly, J. & Bandmann, O. Ursocholanic acid rescues mitochondrial function in common forms of familial Parkinson’s disease. Brain 136, 3038–3050 (2013).
Park, J. et al. Mitochondrial dysfunction in Drosophila PINK1 mutants is complemented by parkin. Nature 441, 1157–1161 (2006).
Tain, L. S. et al. Rapamycin activation of 4E-BP prevents parkinsonian dopaminergic neuron loss. Nat. Neurosci. 12, 1129–1135 (2009).
Clark, I. E. et al. Drosophila pink1 is required for mitochondrial function and interacts genetically with parkin. Nature 441, 1162–1166 (2006).
Pickrell, A. M. & Youle, R. J. The roles of PINK1, Parkin, and mitochondrial fidelity in parkinson’s disease. Neuron 85, 257–273 (2015).
Shin, J. H. et al. PARIS (ZNF746) repression of PGC-1α contributes to neurodegeneration in parkinson’s disease. Cell 144, 689–702 (2011).
Ottolini, D., Calì, T., Negro, A. & Brini, M. The Parkinson disease-related protein DJ-1 counteracts mitochondrial impairment induced by the tumour suppressor protein p53 by enhancing endoplasmic reticulum-mitochondria tethering. Hum. Mol. Genet. 22, 2152–2168 (2013).
Feng, C. W. et al. Neuroprotective effect of the marine-derived compound 11-dehydrosinulariolide through DJ-1-related pathway in in vitro and in vivo models of Parkinson’s disease. Mar. Drugs 14, E187 (2016).
Ablat, N. et al. Neuroprotective effects of a standardized flavonoid extract from safflower against a rotenone-induced rat model of Parkinson’s disease. Molecules 21, E1107 (2016).
Zavodszky, E. et al. Mutation in VPS35 associated with Parkinson’s disease impairs WASH complex association and inhibits autophagy. Nat. Commun. 5, 3828 (2014).
Temkin, P. et al. The retromer supports AMPA receptor trafficking during LTP. Neuron 94, 74–82 (2017).
Kim, S. et al. GBA1 deficiency negatively affects physiological α-synuclein tetramers and related multimers. Proc. Natl Acad. Sci. USA 115, 798–803 (2018).
Shults, C. W. et al. Effects of coenzyme Q 10 in early Parkinson disease: evidence of slowing of the functional decline. Arch. Neurol. 59, 1541–1550 (2002).
Beal, M. F. et al. A randomized clinical trial of high-dosage coenzyme Q10 in early parkinson disease no evidence of benefit. JAMA Neurol. 75, 543–552 (2014).
Poulter, M. O., Payne, K. B. & Steiner, J. P. Neuroimmunophilins: a novel drug therapy for the reversal of neurodegenerative disease? Neuroscience 128, 1–6 (2004).
Kieburtz, K. et al. A randomized clinical trial of coenzyme Q10 and GPI-1485 in early Parkinson disease. Neurology 68, 20–28 (2007).
Mischley, L. K., Lau, R. C., Shankland, E. G., Wilbur, T. K. & Padowski, J. M. Phase IIb study of intranasal glutathione in Parkinson’s disease. J. Parkinsons Dis. 7, 289–299 (2017).
Monti, D. A. et al. N-Acetyl cysteine may support dopamine neurons in Parkinson’s disease: preliminary clinical and cell line data. PLOS ONE 11, e0157602 (2016).
Lin, K. Der et al. Statin therapy prevents the onset of Parkinson disease in patients with diabetes. Ann. Neurol. 80, 532–540 (2016).
Liu, G. et al. Statins may facilitate Parkinson’s disease: insight gained from a large, national claims database. Mov. Disord. 32, 913–917 (2017).
Ravina, B. et al. A randomized, double-blind, futility clinical trial of creatine and minocycline in early Parkinson disease. Neurology 66, 664–671 (2006).
Jin, H. et al. Mitochondria-targeted antioxidants for treatment of Parkinson’s disease: preclinical and clinical outcomes. Biochim. Biophys. Acta 1842, 1282–1294 (2014).
Snow, B. J. et al. A double-blind, placebo-controlled study to assess the mitochondria- targeted antioxidant MitoQ as a disease-modifying therapy in Parkinson’s disease. Mov. Disord. 25, 1670–1674 (2010).
Bido, S., Soria, F. N., Fan, R. Z., Bezard, E. & Tieu, K. Mitochondrial division inhibitor-1 is neuroprotective in the A53T-α-synuclein rat model of Parkinson’s disease. Sci. Rep. 7, 7495 (2017).
Shaltouki, A., Hsieh, C. H., Kim, M. J. & Wang, X. Alpha-synuclein delays mitophagy and targeting Miro rescues neuron loss in Parkinson’s models. Acta Neuropathol. 136, 607–620 (2018).
Di Paolo, T. et al. AQW051, a novel and selective nicotinic acetylcholine receptor α7 partial agonist, reduces l-Dopa-induced dyskinesias and extends the duration of l-Dopa effects in parkinsonian monkeys. Parkinsonism Relat. Disord. 20, 1119–1123 (2014).
Tison, F. et al. A phase 2A trial of the novel mGluR5-negative allosteric modulator dipraglurant for levodopa-induced dyskinesia in Parkinson’s disease. Mov. Disord. 31, 1373–1380 (2016).
Muramatsu, S. I. et al. A phase i study of aromatic l-amino acid decarboxylase gene therapy for parkinson’s disease. Mol. Ther. 18, 1731–1735 (2010).
Mittermeyer, G. et al. Long-term evaluation of a phase 1 study of AADC gene therapy for Parkinson’s disease. Hum. Gene Ther. 23, 377–381 (2012).
Palfi, S. et al. Long-term safety and tolerability of ProSavin, a lentiviral vector-based gene therapy for Parkinson’s disease: a dose escalation, open-label, phase 1/2 trial. Lancet 383, 1138–1146 (2014).
Kaplitt, M. G. et al. Safety and tolerability of gene therapy with an adeno-associated virus (AAV) borne GAD gene for Parkinson’s disease: an open label, phase I trial. Lancet 369, 2097–2105 (2007).
Gill, S. S. et al. Direct brain infusion of glial cell line-derived neurotrophic factor in Parkinson disease. Nat. Med. 9, 589–595 (2003).
Slevin, J. T. et al. Improvement of bilateral motor functions in patients with Parkinson disease through the unilateral intraputaminal infusion of glial cell line—derived neurotrophic factor. J. Neurosurg. 102, 216–222 (2005).
Lang, A. E. et al. Randomized controlled trial of intraputamenal glial cell line-derived neurotrophic factor infusion in Parkinson disease. Ann. Neurol. 59, 459–466 (2006).
Patel, N. K. et al. Intraputamenal infusion of glial cell line-derived neurotrophic factor in PD: A two-year outcome study. Ann. Neurol. 57, 298–302 (2005).
T. G. Study Group. Randomized Parkinson’s trial of GDNF administered via intermittent intraputamenal convection-enhanced delivery [abstract]. Mov. Disord. 32 (Suppl. 2), 1420 (2017).
Bartus, R. T. et al. Safety/feasibility of targeting the substantia nigra with AAV2-neurturin in Parkinson patients. Neurology 80, 1698–1701 (2013).
Warren Olanow, C. et al. Gene delivery of neurturin to putamen and substantia nigra in Parkinson disease: a double-blind, randomized, controlled trial. Ann. Neurol. 78, 248–257 (2015).
Acknowledgements
The authors are supported by NIH grants R01 NR014852 and R01NS096008; NIH/National Center for Advancing Translational Sciences Clinical and Translational Science Awards to the University of Florida (UL1TR001427, KL2TR001429 and TL1TR001428); and the Parkinson's Foundation.
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, wrote the article and reviewed the manuscript before submission. A.E., V.V.-M. and M.S.O. made a substantial contribution to discussion of article content.
Corresponding author
Ethics declarations
Competing interests
V.V.-M. is supported by a grant for the deep brain stimulation brain bank from Abbott. M.S.O. serves as a consultant for the Parkinson's Foundation and has received research grants from NIH, NPF, the Michael J. Fox Foundation, the Parkinson Alliance, the Smallwood Foundation, the Bachmann–Strauss Foundation, the Tourette Syndrome Association and the UF Foundation. M.S.O. has previously received honoraria but in the past >60 months has received no support from industry. M.S.O. has received royalties for publications with Demos, Manson, Amazon, Smashwords, Books4Patients and Cambridge (movement disorder books). M.S.O. is an associate editor for the New England Journal of Medicine: Journal Watch Neurology. M.S.O. has participated in continuing medical education and educational activities on movement disorders (in the past 36 months) sponsored by PeerView, Prime, QuantiaMD, WebMD, Medicus, MedNet, Henry Stewart and Vanderbilt University. M.S.O. has participated as a site principal investigator (PI) and/or co-PI for several NIH, foundation and industry-sponsored trials over the years but has not received honoraria. A.E. and R.S.E. have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Elkouzi, A., Vedam-Mai, V., Eisinger, R.S. et al. Emerging therapies in Parkinson disease — repurposed drugs and new approaches. Nat Rev Neurol 15, 204–223 (2019). https://doi.org/10.1038/s41582-019-0155-7
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41582-019-0155-7
This article is cited by
-
Immunological aspects of central neurodegeneration
Cell Discovery (2024)
-
Tetramethylpyrazine Nitrone Promotes the Clearance of Alpha-Synuclein via Nrf2-Mediated Ubiquitin–Proteasome System Activation
NeuroMolecular Medicine (2024)
-
Motor and non-motor symptoms, drugs, and their mode of action in Parkinson’s disease (PD): a review
Medicinal Chemistry Research (2024)
-
Unravelling the Parkinson’s puzzle, from medications and surgery to stem cells and genes: a comprehensive review of current and future management strategies
Experimental Brain Research (2024)
-
HMGB1 Mediates Inflammation-Induced DMT1 Increase and Dopaminergic Neurodegeneration in the Early Stage of Parkinsonism
Molecular Neurobiology (2024)