Abstract
Precision medicine is the treatment of patients with therapy targeted to their specific pathophysiology. This lofty ideal currently has limited application in clinical practice. However, new technological advances in epilepsy models and genomics suggest that the precision medicine revolution is closer than ever before. We are gaining an improved understanding of the true complexity underlying the pathophysiology of genetic epilepsies and the sources of phenotypic variation that continue to frustrate efforts at genotype–phenotype correlation. Conventional experimental models of epilepsy, such as mouse models and heterologous expression systems, have provided many of the advances in our understanding of genetic epilepsies, but fail to account for some of these complexities. Novel high-throughput models of epilepsy such as zebrafish and induced pluripotent stems cells can be combined with CRISPR–Cas9 gene editing techniques to explore the pathogenesis of a specific gene change and rapidly screen drug libraries for potential therapeutics. The knowledge gained from these models must be combined with thorough natural history studies to determine appropriate patient populations for pragmatic clinical trials. Advances in the ‘omics’, genetic epilepsy models and deep-phenotyping techniques have revolutionary translational research potential that can bring precision medicine to the forefront of clinical practice in the coming decade.
Key points
-
Efforts to develop precision medicine for epilepsy have been limited by the complexity of the pathophysiology underlying genotype–phenotype correlations.
-
A complete picture of genetic epilepsy pathogenesis recognizes the contribution of intragenic, cellular and network-level variability that is influenced by genomic and environmental differences between patients.
-
Conventional models of epilepsy (heterologous expression systems and mouse models) can address some of these layers of complexity but fail to address others.
-
New models of epilepsy (such as zebrafish and induced pluripotent stem cells) offer insights that were previously not possible.
-
Complementary preclinical approaches that include both conventional and novel models of epilepsy have the power to advance research in precision medicine like never before.
-
The combination of these robust preclinical developments with collaborative clinical research, including deep phenotyping and pragmatic clinical trials, has the potential to improve precision treatment of the genetic epilepsies.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Online Mendelian Inheritance in Man. OMIM Entry Search–epilepsy. OMIM https://www.omim.org/search/?index=entry&sort=score+desc%2C+prefix_sort+desc&start=1&limit=10&search=epilepsy (2017).
Hutchison, C. A. III. DNA sequencing: bench to bedside and beyond. Nucleic Acids Res. 35, 6227–6237 (2007).
Greenberg, D. A. & Subaran, R. Blinders, phenotype, and fashionable genetic analysis: a critical examination of the current state of epilepsy genetic studies. Epilepsia 52, 1–9 (2011).
Takahashi, K. & Yamanaka, S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126, 663–676 (2006).
Takahashi, K. et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 131, 861–872 (2007).
Chamberlain, S. J., Li, X. J. & Lalande, M. Induced pluripotent stem (iPS) cells as in vitro models of human neurogenetic disorders. Neurogenetics 9, 227–235 (2008).
Smith, L. A. et al. A model program for translational medicine in epilepsy genetics. J. Child Neurol. 32, 429–436 (2017).
Gussow, A. B., Petrovski, S., Wang, Q., Allen, A. S. & Goldstein, D. B. The intolerance to functional genetic variation of protein domains predicts the localization of pathogenic mutations within genes. Genome Biol. 17, 9 (2016).
Petrovski, S., Wang, Q., Heinzen, E. L., Allen, A. S. & Goldstein, D. B. Genic intolerance to functional variation and the interpretation of personal genomes. PLOS Genet. 9, e1003709 (2013).
Millichap, J. J. et al. KCNQ2 encephalopathy: features, mutational hot spots, and ezogabine treatment of 11 patients. Neurol. Genet. 2, e96 (2016).
Miceli, F. et al. Genotype-phenotype correlations in neonatal epilepsies caused by mutations in the voltage sensor of K(v)7.2 potassium channel subunits. Proc. Natl Acad. Sci. USA 110, 4386–4391 (2013).
Soldovieri, M. V. et al. Novel KCNQ2 and KCNQ3 mutations in a large cohort of families with benign neonatal epilepsy: first evidence for an altered channel regulation by syntaxin-1A. Hum. Mutat. 35, 356–367 (2014).
Miceli, F. et al. Early-onset epileptic encephalopathy caused by gain-of-function mutations in the voltage sensor of Kv7.2 and Kv7.3 potassium channel subunits. J. Neurosci. 35, 3782–3793 (2015).
Mulkey, S. B. et al. Neonatal nonepileptic myoclonus is a prominent clinical feature of KCNQ2 gain-of-function variants R201C and R201H. Epilepsia 58, 436–445 (2017).
Millichap, J. J. et al. Infantile spasms and encephalopathy without preceding neonatal seizures caused by KCNQ2 R198Q, a gain-of-function variant. Epilepsia 58, e10–e15 (2017).
Kole, M. H. & Cooper, E. C. Axonal Kv7.2/7.3 channels: caught in the act. Channels (Austin) 8, 288–289 (2014).
Kanaumi, T. et al. Developmental changes in KCNQ2 and KCNQ3 expression in human brain: possible contribution to the age-dependent etiology of benign familial neonatal convulsions. Brain Dev. 30, 362–369 (2008).
Safiulina, V. F., Zacchi, P., Taglialatela, M., Yaari, Y. & Cherubini, E. Low expression of Kv7/M channels facilitates intrinsic and network bursting in the developing rat hippocampus. J. Physiol. 586, 5437–5453 (2008).
Rubinstein, M. et al. Genetic background modulates impaired excitability of inhibitory neurons in a mouse model of Dravet syndrome. Neurobiol. Dis. 73, 106–117 (2015).
Casillas-Espinosa, P. M. et al. Evaluating whole genome sequence data from the genetic absence epilepsy rat from Strasbourg and its related non-epileptic strain. PLOS ONE 12, e0179924 (2017).
Weaving, L. S. et al. Mutations of CDKL5 cause a severe neurodevelopmental disorder with infantile spasms and mental retardation. Am. J. Hum. Genet. 75, 1079–1093 (2004).
Valli, E. et al. CDKL5, a novel MYCN-repressed gene, blocks cell cycle and promotes differentiation of neuronal cells. Biochim. Biophys. Acta 1819, 1173–1185 (2012).
Zhu, Y. C. et al. Palmitoylation-dependent CDKL5-PSD-95 interaction regulates synaptic targeting of CDKL5 and dendritic spine development. Proc. Natl Acad. Sci. USA 110, 9118–9123 (2013).
Fuchs, C. et al. Loss of CDKL5 impairs survival and dendritic growth of newborn neurons by altering AKT/GSK-3beta signaling. Neurobiol. Dis. 70, 53–68 (2014).
Livide, G. et al. GluD1 is a common altered player in neuronal differentiation from both MECP2-mutated and CDKL5-mutated iPS cells. Eur. J. Hum. Genet. 23, 195–201 (2015).
Della Sala, G. et al. Dendritic spine instability in a mouse model of CDKL5 disorder is rescued by insulin-like growth factor 1. Biol. Psychiatry 80, 302–311 (2016).
Hector, R. D. et al. Characterisation of CDKL5 transcript isoforms in human and mouse. PLOS ONE 11, e0157758 (2016).
Nawaz, M. S. et al. CDKL5 and Shootin1 interact and concur in regulating neuronal polarization. PLOS ONE 11, e0148634 (2016).
Sivilia, S. et al. CDKL5 knockout leads to altered inhibitory transmission in the cerebellum of adult mice. Genes Brain Behav. 15, 491–502 (2016).
Bahi-Buisson, N. & Bienvenu, T. CDKL5-related disorders: from clinical description to molecular genetics. Mol. Syndromol. 2, 137–152 (2011).
Bahi-Buisson, N. et al. Recurrent mutations in the CDKL5 gene: genotype-phenotype relationships. Am. J. Med. Genet. A 158A, 1612–1619 (2012).
Moseley, B. D., Dhamija, R., Wirrell, E. C. & Nickels, K. C. Historic, clinical, and prognostic features of epileptic encephalopathies caused by CDKL5 mutations. Pediatr. Neurol. 46, 101–105 (2012).
Fehr, S. et al. There is variability in the attainment of developmental milestones in the CDKL5 disorder. J. Neurodev. Disord. 7, 2 (2015).
Fehr, S. et al. Seizure variables and their relationship to genotype and functional abilities in the CDKL5 disorder. Neurology 87, 2206–2213 (2016).
Ishii, A., Watkins, J. C., Chen, D., Hirose, S. & Hammer, M. F. Clinical implications of SCN1A missense and truncation variants in a large Japanese cohort with Dravet syndrome. Epilepsia 58, 282–290 (2017).
Dilena, R. et al. Efficacy of sodium channel blockers in SCN2A early infantile epileptic encephalopathy. Brain Dev. 39, 345–348 (2017).
Wolff, M. et al. Genetic and phenotypic heterogeneity suggest therapeutic implications in SCN2A-related disorders. Brain 140, 1316–1336 (2017).
Yamagata, T., Ogiwara, I., Mazaki, E., Yanagawa, Y. & Yamakawa, K. Nav1.2 is expressed in caudal ganglionic eminence-derived disinhibitory interneurons: mutually exclusive distributions of Nav1.1 and Nav1.2. Biochem. Biophys. Res. Commun. 491, 1070–1076 (2017).
Tai, C., Abe, Y., Westenbroek, R. E., Scheuer, T. & Catterall, W. A. Impaired excitability of somatostatin- and parvalbumin-expressing cortical interneurons in a mouse model of Dravet syndrome. Proc. Natl Acad. Sci. USA 111, E3139–E3148 (2014).
Kalume, F. et al. Sleep impairment and reduced interneuron excitability in a mouse model of Dravet Syndrome. Neurobiol. Dis. 77, 141–154 (2015).
Kurbatova, P. et al. Dynamic changes of depolarizing GABA in a computational model of epileptogenic brain: insight for Dravet syndrome. Exp. Neurol. 283, 57–72 (2016).
Milh, M. et al. Variable clinical expression in patients with mosaicism for KCNQ2 mutations. Am. J. Med. Genet. A 167, 2314–2318 (2015).
McElroy, P. B., Liang, L. P., Day, B. J. & Patel, M. Scavenging reactive oxygen species inhibits status epilepticus-induced neuroinflammation. Exp. Neurol. 298, 13–22 (2017).
Pauletti, A. et al. Targeting oxidative stress improves disease outcomes in a rat model of acquired epilepsy. Brain 140, 1885–1899 (2017).
Pearson-Smith, J. N., Liang, L. P., Rowley, S. D., Day, B. J. & Patel, M. Oxidative stress contributes to status epilepticus associated mortality. Neurochem. Res. 42, 2024–2032 (2017).
Pearson-Smith, J. N. & Patel, M. Metabolic dysfunction and oxidative stress in epilepsy. Int. J. Mol. Sci. 18, E2365 (2017).
Kumar, M. G. et al. Altered glycolysis and mitochondrial respiration in a zebrafish model of Dravet syndrome. eNeuro https://doi.org/10.1523/eneuro.0008-16.2016 (2016).
Veeramah, K. R. et al. De novo pathogenic SCN8A mutation identified by whole-genome sequencing of a family quartet affected by infantile epileptic encephalopathy and SUDEP. Am. J. Hum. Genet. 90, 502–510 (2012).
Vaher, U. et al. De novo SCN8A mutation identified by whole-exome sequencing in a boy with neonatal epileptic encephalopathy, multiple congenital anomalies, and movement disorders. J. Child Neurol. 29, 202–206 (2014).
Wagnon, J. L. & Meisler, M. H. Recurrent and non-recurrent mutations of SCN8A in epileptic encephalopathy. Front. Neurol. 6, 104 (2015).
Wagnon, J. L. et al. Convulsive seizures and SUDEP in a mouse model of SCN8A epileptic encephalopathy. Hum. Mol. Genet. 24, 506–515 (2015).
Lopez-Santiago, L. F. et al. Neuronal hyperexcitability in a mouse model of SCN8A epileptic encephalopathy. Proc. Natl Acad. Sci. USA 114, 2383–2388 (2017).
Barcia, G. et al. De novo gain-of-function KCNT1 channel mutations cause malignant migrating partial seizures of infancy. Nat. Genet. 44, 1255–1259 (2012).
Lim, C. X., Ricos, M. G., Dibbens, L. M. & Heron, S. E. KCNT1 mutations in seizure disorders: the phenotypic spectrum and functional effects. J. Med. Genet. 53, 217–225 (2016).
Vanderver, A. et al. Identification of a novel de novo p. Phe932Ile KCNT1 mutation in a patient with leukoencephalopathy and severe epilepsy. Pediatr. Neurol. 50, 112–114 (2014).
Evely, K. M., Pryce, K. D. & Bhattacharjee, A. The Phe932Ile mutation in KCNT1 channels associated with severe epilepsy, delayed myelination and leukoencephalopathy produces a loss-of-function channel phenotype. Neuroscience 351, 65–70 (2017).
Bearden, D. et al. Targeted treatment of migrating partial seizures of infancy with quinidine. Ann. Neurol. 76, 457–461 (2014).
Milligan, C. J. et al. KCNT1 gain of function in 2 epilepsy phenotypes is reversed by quinidine. Ann. Neurol. 75, 581–590 (2014).
Mikati, M. A. et al. Quinidine in the treatment of KCNT1-positive epilepsies. Ann. Neurol. 78, 995–999 (2015).
Fukuoka, M. et al. Quinidine therapy for West syndrome with KCNTI mutation: a case report. Brain Dev. 39, 80–83 (2017).
McTague, A. et al. Clinical and molecular characterization of KCNT1-related severe early-onset epilepsy. Neurology 90, e55–e66 (2017).
Mullen, S. A. et al. Precision therapy for epilepsy due to KCNT1 mutations: a randomized trial of oral quinidine. Neurology 90, e67–e72 (2017).
Chong, P. F., Nakamura, R., Saitsu, H., Matsumoto, N. & Kira, R. Ineffective quinidine therapy in early onset epileptic encephalopathy with KCNT1 mutation. Ann. Neurol. 79, 502–503 (2016).
Griffin, A., Krasniak, C. & Baraban, S. C. Advancing epilepsy treatment through personalized genetic zebrafish models. Prog. Brain Res. 226, 195–207 (2016).
Hong, S., Lee, P., Baraban, S. C. & Lee, L. P. A novel long-term, multi-channel and non-invasive electrophysiology platform for zebrafish. Sci. Rep. 6, 28248 (2016).
Meyer, M. et al. Microarray noninvasive neuronal seizure recordings from intact larval zebrafish. PLOS ONE 11, e0156498 (2016).
Hunyadi, B., Siekierska, A., Sourbron, J., Copmans, D. & de Witte, P. A. M. Automated analysis of brain activity for seizure detection in zebrafish models of epilepsy. J. Neurosci. Methods 287, 13–24 (2017).
Turrini, L. et al. Optical mapping of neuronal activity during seizures in zebrafish. Sci. Rep. 7, 3025 (2017).
Baraban, S. C., Dinday, M. T. & Hortopan, G. A. Drug screening in Scn1a zebrafish mutant identifies clemizole as a potential Dravet syndrome treatment. Nat. Commun. 4, 2410 (2013).
Mahmood, F. et al. A zebrafish model of CLN2 disease is deficient in tripeptidyl peptidase 1 and displays progressive neurodegeneration accompanied by a reduction in proliferation. Brain 136, 1488–1507 (2013).
Mahmood, F. et al. Generation and validation of a zebrafish model of EAST (epilepsy, ataxia, sensorineural deafness and tubulopathy) syndrome. Dis. Model. Mech. 6, 652–660 (2013).
Colin, E. et al. Biallelic variants in UBA5 reveal that disruption of the UFM1 cascade can result in early-onset encephalopathy. Am. J. Hum. Genet. 99, 695–703 (2016).
Cooper, S. R., Jontes, J. D. & Sotomayor, M. Structural determinants of adhesion by Protocadherin-19 and implications for its role in epilepsy. eLife 5, e18529 (2016).
Sicca, F. et al. Gain-of-function defects of astrocytic Kir4.1 channels in children with autism spectrum disorders and epilepsy. Sci. Rep. 6, 34325 (2016).
Wager, K. et al. Neurodegeneration and epilepsy in a zebrafish model of CLN3 disease (Batten disease). PLOS ONE 11, e0157365 (2016).
Anttonen, A. K. et al. ZNHIT3 is defective in PEHO syndrome, a severe encephalopathy with cerebellar granule neuron loss. Brain 140, 1267–1279 (2017).
Cao, S. et al. Homozygous EEF1A2 mutation causes dilated cardiomyopathy, failure to thrive, global developmental delay, epilepsy and early death. Hum. Mol. Genet. 26, 3545–3552 (2017).
Pena, I. A. et al. Pyridoxine-dependent epilepsy in zebrafish caused by Aldh7a1 deficiency. Genetics 207, 1501–1518 (2017).
Scheldeman, C. et al. mTOR-related neuropathology in mutant tsc2 zebrafish: phenotypic, transcriptomic and pharmacological analysis. Neurobiol. Dis. 108, 225–237 (2017).
Zabinyakov, N. et al. Characterization of the first knock-out aldh7a1 zebrafish model for pyridoxine-dependent epilepsy using CRISPR-Cas9 technology. PLOS ONE 12, e0186645 (2017).
Griffin, A. et al. Clemizole and modulators of serotonin signalling suppress seizures in Dravet syndrome. Brain 140, 669–683 (2017).
Schoonjans, A. et al. Low-dose fenfluramine significantly reduces seizure frequency in Dravet syndrome: a prospective study of a new cohort of patients. Eur. J. Neurol. 24, 309–314 (2017).
Son, D. et al. Generation of two induced pluripotent stem cell (iPSC) lines from X-linked adrenoleukodystrophy (X-ALD) patients with adrenomyeloneuropathy (AMN). Stem Cell Res. 25, 46–49 (2017).
Bershteyn, M. et al. Human iPSC-derived cerebral organoids model cellular features of lissencephaly and reveal prolonged mitosis of outer radial glia. Cell Stem Cell 20, 435–449.e4 (2017).
Marinowic, D. R. et al. Induced pluripotent stem cells from patients with focal cortical dysplasia and refractory epilepsy. Mol. Med. Rep. 15, 2049–2056 (2017).
Chen, W. et al. Generation of the SCN1A epilepsy mutation in hiPS cells using the TALEN technique. Sci. Rep. 4, 5404 (2014).
Maeda, H. et al. Establishment of isogenic iPSCs from an individual with SCN1A mutation mosaicism as a model for investigating neurocognitive impairment in Dravet syndrome. J. Hum. Genet. 61, 565–569 (2016).
Sun, Y. et al. A deleterious Nav1.1 mutation selectively impairs telencephalic inhibitory neurons derived from Dravet Syndrome patients. eLife 5, e13073 (2016).
Yamashita, S. et al. Mislocalization of syntaxin-1 and impaired neurite growth observed in a human iPSC model for STXBP1-related epileptic encephalopathy. Epilepsia 57, e81–e86 (2016).
Ricciardi, S. et al. CDKL5 ensures excitatory synapse stability by reinforcing NGL-1-PSD95 interaction in the postsynaptic compartment and is impaired in patient iPSC-derived neurons. Nat. Cell Biol. 14, 911–923 (2012).
Spampanato, J., Escayg, A., Meisler, M. H. & Goldin, A. L. Functional effects of two voltage-gated sodium channel mutations that cause generalized epilepsy with febrile seizures plus type 2. J. Neurosci. 21, 7481–7490 (2001).
Lossin, C. et al. Epilepsy-associated dysfunction in the voltage-gated neuronal sodium channel SCN1A. J. Neurosci. 23, 11289–11295 (2003).
Liu, Y. et al. Dravet syndrome patient-derived neurons suggest a novel epilepsy mechanism. Ann. Neurol. 74, 128–139 (2013).
Tidball, A. M. et al. Rapid generation of human genetic loss-of-function iPSC lines by simultaneous reprogramming and gene editing. Stem Cell Rep. 9, 725–731 (2017).
Hadoux, J. et al. Transcriptional landscape of a RET(C634Y)-mutated iPSC and its CRISPR-corrected isogenic control reveals the putative role of EGR1 transcriptional program in the development of multiple endocrine neoplasia type 2A-associated cancers. Stem Cell Res. 26, 8–16 (2017).
Tidball, A. M. & Parent, J. M. Concise review: exciting cells: modeling genetic epilepsies with patient-derived induced pluripotent stem cells. Stem Cells 34, 27–33 (2016).
Lee, G. et al. Large-scale screening using familial dysautonomia induced pluripotent stem cells identifies compounds that rescue IKBKAP expression. Nat. Biotechnol. 30, 1244–1248 (2012).
Kaufmann, M. et al. High-throughput screening using iPSC-derived neuronal progenitors to identify compounds counteracting epigenetic gene silencing in Fragile X syndrome. J. Biomol. Screen. 20, 1101–1111 (2015).
Darville, H. et al. Human pluripotent stem cell-derived cortical neurons for high throughput medication screening in autism: a proof of concept study in SHANK3 haploinsufficiency Syndrome. EBioMedicine 9, 293–305 (2016).
Li, R. et al. Recapitulating cortical development with organoid culture in vitro and modeling abnormal spindle-like (ASPM related primary) microcephaly disease. Protein Cell 8, 823–833 (2017).
Quadrato, G. & Arlotta, P. Present and future of modeling human brain development in 3D organoids. Curr. Opin. Cell Biol. 49, 47–52 (2017).
Tomaskovic-Crook, E. & Crook, J. M. Clinically amendable, defined, and rapid induction of human brain organoids from induced pluripotent stem cells. Methods Mol. Biol. https://doi.org/10.1007/7651_2017_95 (2017).
Zhang, S. C., Wernig, M., Duncan, I. D., Brustle, O. & Thomson, J. A. In vitro differentiation of transplantable neural precursors from human embryonic stem cells. Nat. Biotechnol. 19, 1129–1133 (2001).
Maroof, A. M. et al. Directed differentiation and functional maturation of cortical interneurons from human embryonic stem cells. Cell Stem Cell 12, 559–572 (2013).
DeRosa, B. A. et al. hVGAT-mCherry: a novel molecular tool for analysis of GABAergic neurons derived from human pluripotent stem cells. Mol. Cell. Neurosci. 68, 244–257 (2015).
Chen, Z., Brodie, M. J., Liew, D. & Kwan, P. Treatment outcomes in patients with newly diagnosed epilepsy treated with established and new antiepileptic drugs: a 30-year longitudinal cohort study. JAMA Neurol. 75, 279–286 (2018).
Schulz, A. et al. Study of intraventricular cerliponase Alfa for CLN2 disease. N. Engl. J. Med. 378, 1898–1907 (2018).
Rosenow, F. et al. Personalized translational epilepsy research - novel approaches and future perspectives: part I: clinical and network analysis approaches. Epilepsy Behav. 76, 13–18 (2017).
Kohler, S. et al. The human phenotype ontology in 2017. Nucleic Acids Res. 45, D865–D876 (2017).
Robinson, P. N., Mungall, C. J. & Haendel, M. Capturing phenotypes for precision medicine. Cold Spring Harb. Mol. Case Stud. 1, a000372 (2015).
Robinson, P. N. Deep phenotyping for precision medicine. Hum. Mutat. 33, 777–780 (2012).
Haring, R. & Wallaschofski, H. Diving through the “-omics”: the case for deep phenotyping and systems epidemiology. OMICS 16, 231–234 (2012).
Tracy, R. P. ‘Deep phenotyping’: characterizing populations in the era of genomics and systems biology. Curr. Opin. Lipidol. 19, 151–157 (2008).
Moeller, F. et al. EEG-fMRI in atypical benign partial epilepsy. Epilepsia 54, e103–e108 (2013).
Warren, A. E. L., Abbott, D. F., Jackson, G. D. & Archer, J. S. Thalamocortical functional connectivity in Lennox-Gastaut syndrome is abnormally enhanced in executive-control and default-mode networks. Epilepsia 58, 2085–2097 (2017).
Siniatchkin, M. & Capovilla, G. Functional neuroimaging in epileptic encephalopathies. Epilepsia 54 (Suppl. 8), 27–33 (2013).
Frey, L. J., Lenert, L. & Lopez-Campos, G. EHR big data deep phenotyping. Contribution of the IMIA Genomic Medicine Working Group. Yearb. Med. Inform. 9, 206–211 (2014).
Underhill, M. L. et al. A state-wide initiative to promote genetic testing in an underserved population. Cancer Med. 6, 1837–1844 (2017).
Childers, K. K., Maggard-Gibbons, M., Macinko, J. & Childers, C. P. National distribution of cancer genetic testing in the united states: evidence for a gender disparity in hereditary breast and ovarian cancer. JAMA Oncol. 4, 876–879 (2018).
Gerhard, G. S., Fisher, S. G. & Feldman, A. M. Genetic testing for inherited cardiac diseases in underserved populations of non-european ancestry: double disparity. JAMA Cardiol. 3, 273–274 (2018).
Manrriquez, E., Chapman, J. S., Mak, J., Blanco, A. M. & Chen, L. M. Disparities in genetics assessment for women with ovarian cancer: can we do better? Gynecol. Oncol. 149, 84–88 (2018).
Sayani, A. Inequities in genetic testing for hereditary breast cancer: implications for public health practice. J. Community Genet. https://doi.org/10.1007/s12687-018-0370-8 (2018).
Acknowledgements
Reviewer information
Nature Reviews Neurology thanks A. Poduri, X. Wang and E. Russo for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
Both authors contributed to the discussion of content, writing and editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
S.D. has consulted for Upsher-Smith on an unrelated subject matter. A.B.K. has no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Demarest, S.T., Brooks-Kayal, A. From molecules to medicines: the dawn of targeted therapies for genetic epilepsies. Nat Rev Neurol 14, 735–745 (2018). https://doi.org/10.1038/s41582-018-0099-3
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41582-018-0099-3
This article is cited by
-
Degeneracy in epilepsy: multiple routes to hyperexcitable brain circuits and their repair
Communications Biology (2023)
-
Steps to Improve Precision Medicine in Epilepsy
Molecular Diagnosis & Therapy (2023)
-
Genetische Diagnostik der Epilepsien: Empfehlung der Kommission Epilepsie und Genetik der Deutschen Gesellschaft für Epileptologie (DGfE)
Clinical Epileptology (2023)
-
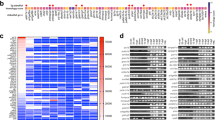
Phenotypic analysis of catastrophic childhood epilepsy genes
Communications Biology (2021)
-
Multimodal electrophysiological analyses reveal that reduced synaptic excitatory neurotransmission underlies seizures in a model of NMDAR antibody-mediated encephalitis
Communications Biology (2021)