Abstract
Health inequity refers to the existence of unnecessary and unfair differences in the ability of an individual or community to achieve optimal health and access appropriate care. Kidney diseases, including acute kidney injury and chronic kidney disease, are the epitome of health inequity. Kidney disease risk and outcomes are strongly associated with inequities that occur across the entire clinical course of disease. Insufficient investment across the spectrum of kidney health and kidney care is a fundamental source of inequity. In addition, social and structural inequities, including inequities in access to primary health care, education and preventative strategies, are major risk factors for, and contribute to, poorer outcomes for individuals living with kidney diseases. Access to affordable kidney care is also highly inequitable, resulting in financial hardship and catastrophic health expenditure for the most vulnerable. Solutions to these injustices require leadership and political will. The nephrology community has an important role in advocacy and in identifying and implementing solutions to dismantle inequities that affect kidney health.
Key points
-
Insufficient investment across the spectrum of kidney health and kidney care (from raising awareness of kidney disease, to its prevention, diagnosis and treatment) is a fundamental source of inequity, and affects all people at risk of, or living with, kidney diseases.
-
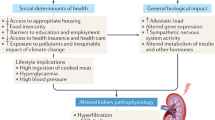
Social and structural inequities are major risk factors for, and contribute to, poor outcomes for individuals living with kidney diseases.
-
Access to essential diagnostics and medications for kidney disease is inequitable and insufficient, as are programmes to track their burden; these insufficiencies disadvantage patients in low- and middle-income countries from early in their disease course.
-
The ability to access kidney care across the spectrum of disease without exposure to financial hardship is very inequitable; this inequity results in vastly different outcomes and life courses for patients who have the same diseases but live under different circumstances.
-
Novel therapies for rare (orphan) diseases are often only available at extremely high prices; their use in children is often not adequately documented and the cost of these medications exacerbates inequities.
-
All nephrology professionals should become skilled at advocating on behalf of their patients to communities, policy makers, administrators and insurers to develop constructive strategies and collectively reach optimal solutions to improve equity in the accessibility of quality kidney care locally and across the globe.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Kawachi, I., Subramanian, S. V. & Almeida-Filho, N. A glossary for health inequalities. J. Epidemiol. Community Health 56, 647–652 (2022).
World Health Organisation. Health Topics — Health Equity. https://www.who.int/health-topics/health-equity (2010).
Nicholas, S. B., Kalantar-Zadeh, K. & Norris, K. C. Socioeconomic disparities in chronic kidney disease. Adv. Chronic Kidney Dis. 22, 6–15 (2015).
Martin, D. E. et al. Ethical challenges in nephrology: a call for action. Nat. Rev. Nephrol. 16, 603–613 (2020).
The Health Foundation. A Communications Toolkit for People Working in Public Health. https://www.health.org.uk/publications/how-to-talk-about-the-building-blocks-of-health (2022).
Lynch, J. W., Kaplan, G. A. & Salonen, J. T. Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Soc. Sci. Med. 44, 809–819 (1997).
Luyckx, V. A., Cherney, D. Z. I. & Bello, A. K. Preventing CKD in developed countries. Kidney Int. Rep. 5, 263–277 (2020).
Sawhney, S. et al. Care processes and outcomes of deprivation across the clinical course of kidney disease: findings from a high-income country with universal healthcare. Nephrol. Dial. Transpl. 38, 1170–1182 (2023).
Vanholder, R. et al. Reducing the costs of chronic kidney disease while delivering quality health care: a call to action. Nat. Rev. Nephrol. 13, 393–409 (2017).
The International Society of Nephrology. Global Kidney Health Atlas. https://www.theisn.org/initiatives/global-kidney-health-atlas/ (2023).
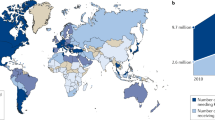
Collaboration GBDCKD. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet 395 709-733 (2020).
Minutolo, R. et al. Detection and awareness of moderate to advanced CKD by primary care practitioners: a cross-sectional study from Italy. Am. J. Kidney Dis. 52, 444–453 (2008).
Levin, A. et al. Global kidney health 2017 and beyond: a roadmap for closing gaps in care, research, and policy. Lancet 390, 1888–1917 (2017).
Matsushita, K. et al. Estimated glomerular filtration rate and albuminuria for prediction of cardiovascular outcomes: a collaborative meta-analysis of individual participant data. Lancet Diabetes Endocrinol. 3, 514–525 (2015).
Thomas, B. et al. Global cardiovascular and renal outcomes of reduced GFR. J. Am. Soc. Nephrol. 28, 2167–2179 (2017).
Luyckx, V. A. Equity is key to build back better after COVID-19: prioritize noncommunicable diseases and kidney health. Kidney360 2, 747–750 (2021).
Vanholder, R. et al. Fighting the unbearable lightness of neglecting kidney health: the decade of the kidney. Clin. Kidney J. 14, 1719–1730 (2021).
European Commission. Research and Innovation. https://ec.europa.eu/info/research-and-innovation/research-area/health-research-and-innovation_en (accessed 31 July 2023).
World Health Organisation Europe. Health topics. https://www.who.int/europe/health-topics (accessed 31 July 2023).
EuroHealthNet. EuroHealthNet provides input for the EU NCD initiative. “Healthier Together”. https://eurohealthnet.eu/publication/eurohealthnet-provides-input-for-the-eu-ncd-initiative-healthier-together/?gclid=CjwKCAjwpKyYBhB7EiwAU2Hn2X2DCd8zG1iKjcvo8EsmpZmOhfnEcqmgzQd9egkTXxml5HMr451FdBoCbmAQAvD_BwE (2022).
NHS. Understanding what the public know about about their kidneys and what they do. thinkkidneys.nhs.uk, http://www.thinkkidneys.nhs.uk/aki/wp-content/uploads/sites/2/2015/01/Understanding-what-the-public-know-about-their-kidneys-and-what-they-do.pdf (2022).
Tonelli, M. et al. Risk of coronary events in people with chronic kidney disease compared with those with diabetes: a population-level cohort study. Lancet 380, 807–814 (2012).
Institute for Health Metrics and Evaluation. Global Burden of Disease Results. https://vizhub.healthdata.org/gbd-results/ (2019).
Liyanage, T. et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet 385, 1975–1982 (2015).
Lewington, A. J., Cerda, J. & Mehta, R. L. Raising awareness of acute kidney injury: a global perspective of a silent killer. Kidney Int. 84, 457–467 (2013).
Luyckx, V. Getting chronic kidney disease on the map. NSAP 22, 115–120 (2022).
Mehta, R. L. et al. International Society of Nephrology’s 0by25 initiative for acute kidney injury (zero preventable deaths by 2025): a human rights case for nephrology. Lancet 385, 2616–2643 (2015).
Mora, C. et al. Over half of known human pathogenic diseases can be aggravated by climate change. Nat. Clim. Chang. 12, 869–875 (2022).
Mills, K. T. et al. A systematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int. 88, 950–957 (2015).
Lameire, N. The definitions and staging systems of acute kidney injury and their limitations in practice. Arab. J. Nephrol. Transpl. 6, 145–152 (2013).
Susantitaphong, P. et al. World incidence of AKI: a meta-analysis. Clin. J. Am. Soc. Nephrol. 8, 1482–1493 (2013).
Institute for Health Metrics and Evaluation. Global Burden of Disease - Compare. https://vizhub.healthdata.org/gbd-compare (2020).
Vart, P., Reijneveld, S. A., Bultmann, U. & Gansevoort, R. T. Added value of screening for CKD among the elderly or persons with low socioeconomic status. Clin. J. Am. Soc. Nephrol. 10, 562–570 (2015).
van Rijn, M. H. C., Alencar de Pinho, N., Wetzels, J. F., van den Brand, J. & Stengel, B. Worldwide disparity in the relation between CKD prevalence and kidney failure risk. Kidney Int. Rep. 5, 2284–2291 (2020).
Xie, Y. et al. Analysis of the Global Burden of Disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int. 94, 567–581 (2018).
Sever, M. et al. A roadmap for optimizing chronic kidney disease patient care and patient-oriented research in the Eastern European nephrology community. Clin. Kidney J. 14, 23–35 (2020).
de Jong, R. W. et al. Results of the European EDITH nephrologist survey on factors influencing treatment modality choice for end-stage kidney disease. Nephrol. Dial. Transpl. 37, 126–38 (2021).
Lunney, M. et al. Availability, accessibility, and quality of conservative kidney management worldwide. Clin. J. Am. Soc. Nephrol. 16, 79–87 (2020).
Kevin Tucker, J. Social justice as a tool to eliminate inequities in kidney disease. Semin. Nephrol. 41, 203–10 (2021).
Etheredge, H. & Fabian, J. Challenges in expanding access to dialysis in South Africa-expensive modalities, cost constraints and human rights. Healthcare 5, 38 (2017).
The World Bank. Gini index. data.worldbank.org, https://data.worldbank.org/indicator/SI.POV.GINI (2023).
Institute for Health Metrics and Evaluation. Epi Visualization, https://vizhub.healthdata.org/epi/ (2019).
Ashuntantang, G. et al. Outcomes in adults and children with end-stage kidney disease requiring dialysis in sub-Saharan Africa: a systematic review. Lancet Glob. Health 5, e408–e417 (2017).
Caskey, F. J. et al. Global variation in renal replacement therapy for end-stage renal disease. Nephrol. Dial. Transpl. 26, 2604–2610 (2011).
Stel, V. S. et al. Supplemented ERA-EDTA Registry data evaluated the frequency of dialysis, kidney transplantation, and comprehensive conservative management for patients with kidney failure in Europe. Kidney Int. 100, 182–195 (2021).
Norton, J. M. et al. Social determinants of racial disparities in CKD. J. Am. Soc. Nephrol. 27, 2576–2595 (2016).
Htay, H. et al. Global access of patients with kidney disease to health technologies and medications: findings from the Global Kidney Health Atlas project. Kidney Int. Suppl. 8, 64–73 (2018).
Francis, A. et al. Barriers to accessing essential medicines for kidney disease in low- and lower middle-income countries. Kidney Int. 102, 969–973 (2022).
Sharif, M. U., Elsayed, M. E. & Stack, A. G. The global nephrology workforce: emerging threats and potential solutions! Clin. Kidney J. 9, 11–22 (2016).
Kalantar-Zadeh, K. et al. Living well with kidney disease by patient and care-partner empowerment: kidney health for everyone everywhere. Kidney Int. 99, 278–284 (2021).
Carter, S. A. et al. Identifying outcomes important to patients with glomerular disease and their caregivers. Clin. J. Am. Soc. Nephrol. 15, 673–684 (2020).
Morton, R. L. et al. Impact of CKD on household income. Kidney Int. Rep. 3, 610–618 (2018).
Garcia-Garcia, G. et al. Chronic kidney disease (CKD) in disadvantaged populations. Clin. Kidney J. 8, 3–6 (2015).
Banerjee, T. et al. Food insecurity, CKD, and subsequent ESRD in US adults. Am. J. Kidney Dis. 70, 38–47 (2017).
Wilkinson, E., Brettle, A., Waqar, M. & Randhawa, G. Inequalities and outcomes: end stage kidney disease in ethnic minorities. BMC Nephrol. 20, 234 (2097).
Mohottige, D., Diamantidis, C. J., Norris, K. C. & Boulware, L. E. Racism and kidney health: turning equity into a reality. Am. J. Kidney Dis. 77, 951–962 (2021).
Mohottige, D. & Lunn, M. R. Advancing equity in nephrology: enhancing care for LGBTQ+ patients and our workforce. Clin. J. Am. Soc. Nephrol. 14, 1094–1096 (2019).
Norris, K. C. & Beech, B. M. Social determinants of kidney health: focus on poverty. Clin. J. Am. Soc. Nephrol. 16, 809–811 (2021).
Hall, Y. N. Social determinants of health: addressing unmet needs in nephrology. Am. J. Kidney Dis. 72, 582–591 (2018).
Crews, D. C. & Novick, T. K. Social determinants of CKD hotspots. Semin. Nephrol. 39, 256–262 (2019).
Brandt, E. J., Chang, T., Leung, C., Ayanian, J. Z. & Nallamothu, B. K. Food insecurity among individuals with cardiovascular disease and cardiometabolic risk factors across race and ethnicity in 1999-2018. JAMA Cardiol. 7, 1218–1226 (2012).
Crews, D. C., Bello, A. K. & Saadi, G. 2019 World Kidney Day editorial — burden, access, and disparities in kidney disease. J. Bras. Nefrol. 41, 1–9 (2019).
Tannor, E. K., Awaku, Y. A., Boima, V. & Antwi, S. The geographical distribution of dialysis services in Ghana. Ren. Repl. Ther. 4, 3 (2018).
Furia, F. F. et al. Developing nephrology services in low income countries: a case of Tanzania. BMC Nephrol. 20, 378 (2019).
Naicker, S., Eastwood, J. B., Plange-Rhule, J. & Tutt, R. C. Shortage of healthcare workers in sub-Saharan Africa: a nephrological perspective. Clin. Nephrol. 74, S129–S133 (2010).
van Zwieten, A., Wong, G. & Qader, M. A. Tackling health inequities for children and adolescents with CKD-A call to advocacy and action across the life course. Kidney Int. Rep. 7, 671–674 (2022).
Swartling, O. et al. Sex differences in the recognition, monitoring, and management of CKD in health care: an observational cohort study. J. Am. Soc. Nephrol. 33, 1903–1914 (2022).
Ravani, P. et al. Association of age with risk of kidney failure in adults with stage IV chronic kidney disease in Canada. JAMA Netw. Open. 3, e2017150 (2020).
O’Hare, A. M. How useful is an age-neutral model of chronic kidney disease? JAMA Netw. Open. 3, e2017592 (2020).
Scholes-Robertson, N. et al. Australian rural caregivers’ experiences in supporting patients with kidney failure to access dialysis and kidney transplantation: a qualitative study. Am. J. Kidney Dis. 80, 773–782.e1 (2022).
Arici, M. Refugees with kidney disease: an increasing global challenge. Nat. Rev. Nephrol. 7, 366–367 (2021).
Van Biesen, W., Vanholder, R., Ernandez, T., Drewniak, D. & Luyckx, V. Caring for migrants and refugees with end-stage kidney disease in Europe. Am. J. Kidney Dis. 71, 701–709 (2018).
Cervantes, L., Hasnain-Wynia, R., Steiner, J. F., Chonchol, M. & Fischer, S. Patient navigation: addressing social challenges in dialysis patients. Am. J. Kidney Dis. 76, 121–129 (2020).
Sachs, J., Lafortune, G., Kroll, C., Fuller, G., Woelm, F. Sustainable Development Report 2022. From Crisis to Sustainable Development: the SDGs as Roadmap to 2030 and Beyond (Cambridge Univ. Press, 2022).
Morton, R. L. et al. Impact of educational attainment on health outcomes in moderate to severe CKD. Am. J. Kidney Dis. 67, 31–39 (2016).
Arogundade, F. A. et al. Burden of end-stage renal disease in sub-Saharan Africa. Clin. Nephrol. 93, 3–7 (2020).
Kretchy, I. A. et al. Prevalence, patterns and beliefs about the use of herbal medicinal products in Ghana: a multi-centre community-based cross-sectional study. Trop. Med. Int. Health 26, 410–420 (2021).
Luyckx, V. A., Miljeteig, I., Ejigu, A. M. & Moosa, M. R. Ethical challenges in the provision of dialysis in resource-constrained environments. Semin. Nephrol. 37, 273–286 (2017).
Sever, M. S. et al. Armed conflicts and kidney patients: a consensus statement from the renal disaster relief task force of the ERA. Nephrol. Dial. Transpl. 38, 56–65 (2023).
Eneanya, N. D. et al. Health inequities and the inappropriate use of race in nephrology. Nat. Rev. Nephrol. 18, 84–94 (2022).
Hounkpatin, H. O. et al. Ethnic minority disparities in progression and mortality of pre-dialysis chronic kidney disease: a systematic scoping review. BMC Nephrol. 21, 217 (2020).
Epstein, A. M. et al. Racial disparities in access to renal transplantation — clinically appropriate or due to underuse or overuse? N. Engl. J. Med. 343, 1537–1544 (2000).
Purnell, T. S. et al. Association of race and ethnicity with live donor kidney transplantation in the United States from 1995 to 2014. JAMA 319, 49–61 (2018).
Mehrotra, R. et al. Racial and ethnic disparities in use of and outcomes with home dialysis in the United States. J. Am. Soc. Nephrol. 27, 2123–2134 (2016).
Luyckx, V. A. & Brenner, B. M. Birth weight, malnutrition and kidney-associated outcomes-a global concern. Nat. Rev. Nephrol. 11, 135–149 (2015).
LaVeist, T. A. et al. The economic burden of racial, ethnic, and educational health inequities in the US. JAMA 329, 1682–1692 (2023).
Purnell, T. S., Hall, Y. N. & Boulware, L. E. Understanding and overcoming barriers to living kidney donation among racial and ethnic minorities in the United States. Adv. Chronic Kidney Dis. 19, 244–251 (2012).
Obermeyer, Z., Powers, B., Vogeli, C. & Mullainathan, S. Dissecting racial bias in an algorithm used to manage the health of populations. Science 366, 447–453 (2019).
Gichoya, J. W. et al. AI recognition of patient race in medical imaging: a modelling study. Lancet Digit. Health 4, e406–e414 (2022).
Williams, W. W., Hogan, J. W. & Ingelfinger, J. R. Time to eliminate health care disparities in the estimation of kidney function. N. Engl. J. Med. 385, 1804–1806 (2021).
Delanaye, P. et al. The « race » correction in estimating glomerular filtration rate: an European point of view. Curr. Opin. Nephrol. Hypertens. 30, 525–530 (2021).
Delgado, C. et al. A unifying approach for GFR estimation: recommendations of the NKF-ASN task force on reassessing the inclusion of race in diagnosing kidney disease. Am. J. Kidney Dis. 79, 268–88 e1 (2022).
Weiss B. D. Health Literacy and Patient Safety: Help Patients Understand: Manual for Clinicians, 2nd edn (American Medical Association Foundation and American Medical Association, 2022).
Vellar, L., Mastroianni, F. & Lambert, K. Embedding health literacy into health systems: a case study of a regional health service. Aust. Health Rev. 41, 621–625 (2017).
Levy, H. & Janke, A. Health literacy and access to care. J. Health Commun. 21, Suppl. 1 43–50 (2016).
Blumenthal, S. J. & Kagen, J. MSJAMA. The effects of socioeconomic status on health in rural and urban America. JAMA 287, 109 (2002).
Scholes-Robertson, N. et al. Perspectives of a proposed patient navigator programme for people with chronic kidney disease in rural communities: report from national workshops. Nephrology 27, 886–896 (2022).
Moist, L. M. et al. Travel time to dialysis as a predictor of health-related quality of life, adherence, and mortality: the dialysis outcomes and practice patterns study (DOPPS). Am. J. Kidney Dis. 51, 641–650 (2008).
Evans, R., Rudd, P., Hemmila, U., Dobbie, H. & Dreyer, G. Deficiencies in education and experience in the management of acute kidney injury among Malawian healthcare workers. Malawi Med. J. 27, 101–103 (2015).
Baelani, I. et al. Identifying resource needs for sepsis care and guideline implementation in the Democratic Republic of the Congo: a cluster survey of 66 hospitals in four eastern provinces. Middle East. J. Anaesthesiol. 21, 559–575 (2012).
Olowu, W. A. et al. Outcomes of acute kidney injury in children and adults in sub-Saharan Africa: a systematic review. Lancet Glob. Health 4, e242–e250 (2016).
Ramachandran, R. et al. Challenges in diagnosis and management of glomerular disease in resource-limited settings. Kidney Int. Rep. 7, 2141–2149 (2022).
Yeung, E. et al. Current status of health systems financing and oversight for end-stage kidney disease care: a cross-sectional global survey. BMJ Open 11, e047245 (2021).
Ludlow, M. J., Lauder, L. A., Mathew, T. H., Hawley, C. M. & Fortnum, D. Australian consumer perspectives on dialysis: first national census. Nephrology 17, 703–709 (2012).
Niang, A., Iyengar, A. & Luyckx, V. A. Hemodialysis versus peritoneal dialysis in resource-limited settings. Curr. Opin. Nephrol. Hypertens. 27, 463–471 (2018).
van der Tol, A., Lameire, N., Morton, R. L., Van Biesen, W. & Vanholder, R. An international analysis of dialysis services reimbursement. Clin. J. Am. Soc. Nephrol. 14, 84–93 (2019).
Okpechi, I. G. et al. The case for increased peritoneal dialysis utilization in low- and lower-middle-income countries. Nephrology 27, 391–403 (2022).
Brown, E. A. et al. Availability of assisted peritoneal dialysis in Europe: call for increased and equal access. Nephrol. Dial. Transpl. 37, 2080–2089 (2022).
Hamroun, A. et al. Barriers to conservative care from patients’ and nephrologists’ perspectives: the CKD-REIN Study. Nephrol. Dial. Transpl. 37, 2438–2448 (2022).
Wolfe, R. A. et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N. Engl. J. Med. 341, 1725–1730 (1999).
Giwa, S. et al. The promise of organ and tissue preservation to transform medicine. Nat. Biotechnol. 35, 530–542 (2017).
Bello, A. K. et al. Global kidney health atlas (GKHA): design and methods. Kidney Int. Suppl. 7, 145–153 (2012).
Wu, D. A. et al. Global trends and challenges in deceased donor kidney allocation. Kidney Int. 91, 1287–1299 (2017).
Vanholder, R. et al. Organ donation and transplantation: a multi-stakeholder call to action. Nat. Rev. Nephrol. 17, 554–568 (2021).
Tiong, M. K., Thomas, S., Fernandes, D. K. & Cherian, S. Examining barriers to timely waitlisting for kidney transplantation for Indigenous Australians in central Australia. Intern. Med. J. 52, 288–294 (2022).
Rota-Musoll, L. et al. An intersectional gender analysis in kidney transplantation: women who donate a kidney. BMC Nephrol. 22, 59 (2021).
Hecking, M. et al. Sex-specific differences in mortality and incident dialysis in the chronic kidney disease outcomes and practice patterns study. Kidney Int. Rep. 7, 410–423 (2022).
Sever, M. S. et al. Ethical and medical dilemmas in paid living kidney donor transplantation. Transpl. Rev. 36, 100726 (2022).
Steering Committee of the Istanbul S. Organ trafficking and transplant tourism and commercialism: the declaration of Istanbul. Lancet 372, 5–6 (2008).
Banerjee, S., Kamath, N., Antwi, S. & Bonilla-Felix, M. Paediatric nephrology in under-resourced areas. Pediatr. Nephrol. 37, 959–972 (2022).
Macedo, E. et al. Recognition and management of acute kidney injury in children: the ISN 0by25 Global Snapshot study. PLoS ONE 13, e0196586 (2018).
Kennedy, S. E., Bailey, R. & Kainer, G. Causes and outcome of late referral of children who develop end-stage kidney disease. J. Paediatr. Child. Health 48, 253–258 (2012).
Chesnaye, N. C. et al. Mortality risk in European children with end-stage renal disease on dialysis. Kidney Int. 89, 1355–1362 (2016).
Pais, P., Blydt-Hansen, T. D., Michael Raj, J. A., Dello Strologo, L. & Iyengar, A. Low renal transplantation rates in children with end-stage kidney disease: a study of barriers in a low-resource setting. Pediatr. Transpl. 25, e13867 (2021).
Sarnak, D. O., Squires, D., Kuzmak, G. & Bishop, S. Paying for prescription drugs around the world: why is the U.S. an outlier? Issue Brief. 2017, 1–14 (2017).
Vanholder, R., Van Biesen, W. & Lameire, N. Renal replacement therapy: how can we contain the costs? Lancet 383, 1783–1785 (2014).
Mohnen, S. M. et al. Healthcare costs of patients on different renal replacement modalities — analysis of Dutch health insurance claims data. PLoS ONE 14, e0220800 (2019).
de Vries, E. F., Los, J., de Wit, G. A. & Hakkaart-van, R. L. Patient, family and productivity costs of end-stage renal disease in the Netherlands; exposing non-healthcare related costs. BMC Nephrol. 22, 341 (2021).
Essue, B. M. et al. in Disease Control Priorities Improving Health and Reducing Poverty 3 edn (eds Jamison, D. T., Gelband H., Horton S. et al.) 121–143 (World Bank, 2018).
Luyckx, V. A. & Moosa, M. R. Priority setting as an ethical imperative in managing global dialysis access and improving kidney care. Semin. Nephrol. 41, 230–241 (2021).
Sculpher M., Revill P., Ochalek J. M., Claxton K. in What’s In, What’s Out? Designing Benefits for Universal Health Coverage (eds Glassman, A. et al.) 115–140 (Center for Global Development, USA).
Howell, M., Walker, R. C. & Howard, K. Cost effectiveness of dialysis modalities: a systematic review of economic evaluations. Appl. Health Econ. Health Policy 17, 315–330 (2019).
Johri, M. & Norheim, O. F. Can cost-effectiveness analysis integrate concerns for equity? Systematic review. Int. J. Technol. Assess. Health Care 28, 125–132 (2012).
Himmelfarb, J., Vanholder, R., Mehrotra, R. & Tonelli, M. The current and future landscape of dialysis. Nat. Rev. Nephrol. 16, 573–585 (2020).
van der Tol, A. et al. A call for harmonization of European kidney care: dialysis reimbursement and distribution of kidney replacement therapies. Nephrol. Dial. Transpl. 35, 979–986 (2020).
Van Biesen, W. et al. Considerations on equity in management of end-stage kidney disease in low- and middle-income countries. Kidney Int. Suppl. 10, e63–e71 (2020).
Ashu, J. T. et al. Challenges to the right to health in sub-Saharan Africa: reflections on inequities in access to dialysis for patients with end-stage kidney failure. Int. J. Equity Health 21, 126 (2022).
Crosby, L. et al. Dialysis in Africa: the need for evidence-informed decision making. Lancet Glob. Health 8, e476–e477 (2020).
Luyckx, V. A. et al. Sustainable Development Goals relevant to kidney health: an update on progress. Nat. Rev. Nephrol. 17, 15–32 (2021).
Sumaili, E. K. et al. High prevalence of undiagnosed chronic kidney disease among at-risk population in Kinshasa, the Democratic Republic of Congo. BMC Nephrol. 10, 18 (2009).
World Health Organization. Saving Lives, Spending Less: The Case for Investing In Noncommunicable Diseases. https://www.who.int/publications/i/item/9789240041059 (2021).
Ameh, O. I., Ekrikpo, U. E. & Kengne, A. P. Preventing CKD in low- and middle-income countries: a call for urgent action. Kidney Int. Rep. 5, 255–262 (2020).
Karpman, D. & Hoglund, P. Orphan drug policies and use in pediatric nephrology. Pediatr. Nephrol. 32, 1–6 (2017).
Zimmermann, B. M., Eichinger, J. & Baumgartner, M. R. A systematic review of moral reasons on orphan drug reimbursement. Orphanet J. Rare Dis. 16, 292 (2021).
Berdud, M., Drummond, M. & Towse, A. Establishing a reasonable price for an orphan drug. Cost. Eff. Resour. Alloc. 18, 31 (2020).
Onakpoya, I. J., Spencer, E. A., Thompson, M. J. & Heneghan, C. J. Effectiveness, safety and costs of orphan drugs: an evidence-based review. BMJ Open. 5, e007199 (2015).
Kesselheim, A. S. et al. The prevalence and cost of unapproved uses of top-selling orphan drugs. PLoS ONE 7, e31894 (2012).
Young, K. E., Soussi, I. & Toumi, M. The perverse impact of external reference pricing (ERP): a comparison of orphan drugs affordability in 12 European countries. A call for policy change. J. Mark. Access. Health Policy 5, 1369817 (2017).
Gammie, T., Lu, C. Y. & Babar, Z. U. Access to orphan drugs: a comprehensive review of legislations, regulations and policies in 35 countries. PLoS ONE 10, e0140002 (2015).
Marmot, M. Just societies, health equity, and dignified lives: the PAHO equity commission. Lancet 392, 2247–2250 (2018).
Garcia, G. G. et al. Sex and gender differences in chronic kidney disease and access to care around the globe. Semin. Nephrol. 42, 101–113 (2022).
Moosa, M. R. & Luyckx, V. A. The realities of rationing in health care. Nat. Rev. Nephrol. 17, 435–436 (2021).
Venkatapuram, S. Health Justice: An Argument from the Capabilities Approach (Polity Press, 2011).
Uberoi, D. & Forman, L. What role can the right to health play in advancing equity in kidney care? Semin. Nephrol. 41, 220–229 (2021).
Braveman, P. A. et al. Health disparities and health equity: the issue is justice. Am. J. Public. Health 101, Suppl. 1 S149–S155 (2011).
World Health Organization. Noncommunicable diseases. https://www.who.int/teams/surveillance-of-noncommunicable-diseases/about/ncds (accessed 31 July 2023).
Chin, M. H. et al. A roadmap and best practices for organizations to reduce racial and ethnic disparities in health care. J. Gen. Intern. Med. 27, 992–1000 (2012).
European Commission. Public Health. European Reference Networks. https://health.ec.europa.eu/european-reference-networks/overview_en (2023).
Plahte, J. Tiered pricing of vaccines: a win-win-win situation, not a subsidy. Lancet Infect. Dis. 5, 58–63 (2005).
Gopichandran, V. et al. Developing the ethics of implementation research in health. Implement. Sci. 11, 161 (2016).
Jager, K. J. et al. A snapshot of European registries on chronic kidney disease patients not on kidney replacement therapy. Nephrol. Dial. Transpl. 37, 8–13 (2021).
Qaseem, A., Hopkins, R. H. Jr., Sweet, D. E., Starkey, M. & Shekelle, P. Screening, monitoring, and treatment of stage 1 to 3 chronic kidney disease: a clinical practice guideline from the American College of Physicians. Ann. Intern. Med. 159, 835–847 (2013).
Greer, R. & Boulware, L. E. Reducing CKD risks among vulnerable populations in primary care. Adv. Chronic Kidney Dis. 22, 74–80 (2015).
Hull, S., Dreyer, G., Badrick, E., Chesser, A. & Yaqoob, M. M. The relationship of ethnicity to the prevalence and management of hypertension and associated chronic kidney disease. BMC Nephrol. 12, 41 (2011).
Tenkorang, E. Y. & Kuuire, V. Z. Noncommunicable diseases in Ghana: does the theory of social gradient in health hold? Health Educ. Behav. 43, 25S–36S (2016).
Wardle, J. & Steptoe, A. Socioeconomic differences in attitudes and beliefs about healthy lifestyles. J. Epidemiol. Community Health 57, 440–443 (2003).
United Nations. Department of Economic and Social Affairs. Sustainable Development Goal 3, https://sdgs.un.org/goals/goal3 (2022).
Chapman, A. R. Assessing the universal health coverage target in the sustainable development goals from a human rights perspective. BMC Int. Health Hum. Rights 16, 33 (2016).
Annemans, L. A proposal for value informed, affordable (“via”) prices for innovative medicines. J. Med. Econ. 22, 1235–1239 (2019).
Cookson, R. et al. Using cost-effectiveness analysis to address health equity concerns. Value Health 20, 206–212 (2017).
Bukhman, G. et al. From a Lancet commission to the NCDI poverty network: reaching the poorest billion through integration science. Lancet 398, 2217–2220 (2021).
Piaggio, D. et al. A framework for designing medical devices resilient to low-resource settings. Glob. Health 17, 64 (2021).
Karopadi, A. N., Mason, G., Rettore, E. & Ronco, C. Cost of peritoneal dialysis and haemodialysis across the world. Nephrol. Dial. Transpl. 28, 2553–2569 (2013).
Mendu, M. L. et al. Expanding utilization of home dialysis: an action agenda from the first international home dialysis roundtable. Kidney Med. 3, 635–643 (2021).
Good Medical Council. Good Medical Practice, https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/good-medical-practice (2019).
Vanholder, R., Conway, P. T., Gallego, D., Scheres, E. & Wieringa, F. The European Kidney Health Alliance (EKHA) and the Decade of the Kidney™. Nephrol. Dial. Transpl. 38, 1113–1122 (2023).
EUPATI. https://eupati.eu (2023).
Abdel-Kader, K., Greer, R. C., Boulware, L. E. & Unruh, M. L. Primary care physicians’ familiarity, beliefs, and perceived barriers to practice guidelines in non-diabetic CKD: a survey study. BMC Nephrol. 15, 64 (2014).
Lusignan, S. et al. Audit-based education lowers systolic blood pressure in chronic kidney disease: the Quality Improvement in CKD (QICKD) trial results. Kidney Int. 84, 609–620 (2013).
Bashshur, R. L. On the definition and evaluation of telemedicine. Telemed. J. 1, 19–30 (1995).
Parker, J. C. Cherry picking in ESRD: an ethical challenge in the era of pay for performance. Semin. Dialysis 24, 5–8 (2011).
Singer, P., McKie, J., Kuhse, H. & Richardson, J. Double jeopardy and the use of QALYs in health care allocation. J. Med. Ethics 21, 144–150 (1995).
Amaral, S. et al. Association between dialysis facility ownership and access to the waiting list and transplant in pediatric patients with end-stage kidney disease in the US. JAMA 328, 451–459 (2022).
Calderon, J. L. et al. Improving diabetes health literacy by animation. Diabetes Educ. 40, 361–372 (2014). 2014.
Koh, H. K., Brach, C., Harris, L. M. & Parchman, M. L. A proposed ‘health literate care model’ would constitute a systems approach to improving patients’ engagement in care. Health Aff. 32, 357–367 (2013).
Jukkala, A., Deupree, J. P. & Graham, S. Knowledge of limited health literacy at an academic health center. J. Contin. Educ. Nurs. 40, 298–302 (2009). quiz 3-4, 36.
Karuranga, S., Sorensen, K., Coleman, C. & Mahmud, A. J. Health literacy competencies for European health care personnel. Health Lit. Res. Pract. 1, e247–e256 (2017).
Elwyn, G. et al. Shared decision making: a model for clinical practice. J. Gen. Intern. Med. 27, 1361–1367 (2012).
Murgic, L., Hebert, P. C., Sovic, S. & Pavlekovic, G. Paternalism and autonomy: views of patients and providers in a transitional (post-communist) country. BMC Med. Ethics 16, 65 (2015).
Joosten, E. A. et al. Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychother. Psychosom. 77, 219–226 (2008).
Rosner, M. H., Husain-Syed, F., Reis, T., Ronco, C. & Vanholder, R. Uremic encephalopathy. Kidney Int. 101, 227–241 (2022).
Acknowledgements
This manuscript was coordinated by the European Kidney Health Alliance (EKHA), a non-governmental not-for-profit organization that advocates for kidney health at the level of the European Commission. The EKHA network has five full members (the European Renal Association, the International Society of Nephrology, the European Kidney Patients Federation, the European Dialysis and Transplant Nurses Association-European Renal Care Association and the Dutch Kidney Foundation), and 31 National or Regional Societies as affiliated members. The EKHA receives support from the European Union in the context of the Annual Work Program 2022 of EU4Health, relating to the prevention of non-communicable diseases, topic ID EU4H-2022-PJ02, project # 101101220 PREVENTCKD.
Author information
Authors and Affiliations
Contributions
R.V., L.A., E.A.B., P.P., S.S., N.S.-R., B.S., E.K.T. and V.A.L. researched data for the article. All authors contributed substantially to discussion of the content. R.V., E.A.B., P.P., S.S., N.S.-R., and V.A.L. wrote the article, and R.V., S.S. and V.A.L. reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
R.V. is an adviser to AstraZeneca, Glaxo Smith Kline, Fresenius Kabi, Novartis, Kibow, Baxter, Nipro, Fresenius Medical Care and Nextkidney. L.A. is an adviser to AstraZeneca and Baxter. E.A.B. is an adviser to Baxter, IiberDi and AWAK, and has received speaker fees from Baxter and Vifor. B.S. has received grant support from Glaxo Smith Kline, Fresenius Medical Care and Boehringer Ingelheim as part of the CKD-REIN study. V.A.L. receives royalties as a co-editor of “The Kidney” textbook. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Nephrology thanks Narayan Prasad, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vanholder, R., Annemans, L., Braks, M. et al. Inequities in kidney health and kidney care. Nat Rev Nephrol 19, 694–708 (2023). https://doi.org/10.1038/s41581-023-00745-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41581-023-00745-6