Abstract
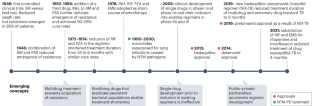
Tuberculosis (TB) drug discovery and development has undergone nothing short of a revolution over the past 20 years. Successful public–private partnerships and sustained funding have delivered a much-improved understanding of mycobacterial disease biology and pharmacology and a healthy pipeline that can tolerate inevitable attrition. Preclinical and clinical development has evolved from decade-old concepts to adaptive designs that permit rapid evaluation of regimens that might greatly shorten treatment duration over the next decade. But the past 20 years also saw the rise of a fatal and difficult-to-cure lung disease caused by nontuberculous mycobacteria (NTM), for which the drug development pipeline is nearly empty. Here, we discuss the similarities and differences between TB and NTM lung diseases, compare the preclinical and clinical advances, and identify major knowledge gaps and areas of cross-fertilization. We argue that applying paradigms and networks that have proved successful for TB, from basic research to clinical trials, will help to populate the pipeline and accelerate curative regimen development for NTM disease.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
WHO. Global Tuberculosis Report https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022 (Geneva, 2022).
Pai, M., Kasaeva, T. & Swaminathan, S. Covid-19’s devastating effect on tuberculosis care – a path to recovery. N. Engl. J. Med. 386, 1490–1493 (2022).
Marais, B. J., Hesseling, A. C. & Cotton, M. F. Poverty and tuberculosis: is it truly a simple inverse linear correlation? Eur. Respir. J. 33, 943–944 (2009).
Dartois, V. A. & Rubin, E. J. Anti-tuberculosis treatment strategies and drug development: challenges and priorities. Nat. Rev. Microbiol. 20, 685–701 (2022).
WHO. Global Tuberculosis Report https://www.who.int/publications/i/item/9789240037021 (Geneva, 2021).
WHO. WHO Consolidated Guidelines on Tuberculosis. Module 4: Drug-resistant Tuberculosis Treatment https://www.who.int/publications/i/item/9789240007048 (Geneva, 2020).
Motta, I. et al. Recent advances in the treatment of tuberculosis. Clin. Microbiol. Infect. https://doi.org/10.1016/j.cmi.2023.07.013 (2023).
Evangelopoulos, D. & McHugh, T. D. Improving the tuberculosis drug development pipeline. Chem. Biol. Drug Des. 86, 951–960 (2015).
Cowman, S., van Ingen, J., Griffith, D. E. & Loebinger, M. R. Non-tuberculous mycobacterial pulmonary disease. Eur. Respir. J. 54, 1900250 (2019).
Winthrop, K. L. et al. Incidence and prevalence of nontuberculous mycobacterial lung disease in a large U.S. managed care health plan, 2008–2015. Ann. Am. Thorac. Soc. 17, 178–185 (2020).
Prevots, D. R. & Marras, T. K. Epidemiology of human pulmonary infection with nontuberculous mycobacteria: a review. Clin. Chest Med. 36, 13–34 (2015).
Raju, R. M., Raju, S. M., Zhao, Y. & Rubin, E. J. Leveraging advances in tuberculosis diagnosis and treatment to address nontuberculous mycobacterial disease. Emerg. Infect. Dis. 22, 365–369 (2016).
Sawka, A. & Burke, A. Medications and monitoring in treatment of nontuberculous mycobacteria lung disease. Clin. Chest Med. 44, 815–828 (2023).
Daley, C. L. et al. Treatment of nontuberculous mycobacterial pulmonary disease: an official ATS/ERS/ESCMID/IDSA clinical practice guideline. Clin. Infect. Dis. 71, 905–913 (2020). A comprehensive review by US and European physicians of evidence-based recommendations for the treatment of NTM-PD.
Egorova, A., Jackson, M., Gavrilyuk, V. & Makarov, V. Pipeline of anti-Mycobacterium abscessus small molecules: repurposable drugs and promising novel chemical entities. Med. Res. Rev. 41, 2350–2387 (2021). A comprehensive review of the clinical and preclinical pipeline for MAB-PD, by mechanism of action and target.
Johansen, M. D., Herrmann, J. L. & Kremer, L. Non-tuberculous mycobacteria and the rise of Mycobacterium abscessus. Nat. Rev. Microbiol. 18, 392–407 (2020). A review covering the biology, virulence factors, host interactions and drug resistance mechanisms of M. abscessus, one of the most antibiotic-resistant mycobacteria.
Griffith, D. E. & Aksamit, T. R. Understanding nontuberculous mycobacterial lung disease: it’s been a long time coming. F1000Res 5, 2797 (2016).
Young, C., Walzl, G. & Du Plessis, N. Therapeutic host-directed strategies to improve outcome in tuberculosis. Mucosal Immunol. 13, 190–204 (2020).
Tiwari, D. & Martineau, A. R. Inflammation-mediated tissue damage in pulmonary tuberculosis and host-directed therapeutic strategies. Semin. Immunol. 65, 101672 (2022).
Lee, A., Xie, Y. L., Barry, C. E. & Chen, R. Y. Current and future treatments for tuberculosis. BMJ 368, m216 (2020).
Anidi, I. U. & Olivier, K. N. Host-directed therapy in nontuberculous mycobacterial pulmonary disease: preclinical and clinical data review. Clin. Chest Med. 44, 839–845 (2023).
Hatfull, G. F. Phage therapy for nontuberculous mycobacteria: challenges and opportunities. Pulm. Ther. 9, 91–107 (2022).
Sterling, T. R. et al. Guidelines for the treatment of latent tuberculosis infection: recommendations from the National Tuberculosis Controllers Association and CDC, 2020. MMWR Recomm. Rep. 69, 1–11 (2020).
Kumar, K. & Loebinger, M. R. Nontuberculous mycobacterial pulmonary disease: clinical epidemiologic features, risk factors, and diagnosis: the nontuberculous mycobacterial series. Chest 161, 637–646 (2022).
Sharma, S. K., Mohan, A. & Kohli, M. Extrapulmonary tuberculosis. Expert. Rev. Respir. Med. 15, 931–948 (2021).
Shih, D. C. et al. Extrapulmonary nontuberculous mycobacterial disease surveillance – Oregon, 2014–2016. MMWR Morb. Mortal. Wkly Rep. 67, 854–857 (2018).
Wilkinson, R. J. et al. Tuberculous meningitis. Nat. Rev. Neurol. 13, 581–598 (2017).
Ganchua, S. K. C., White, A. G., Klein, E. C. & Flynn, J. L. Lymph nodes — the neglected battlefield in tuberculosis. PLoS Pathog. 16, e1008632 (2020).
Lin, P. L. et al. Sterilization of granulomas is common in active and latent tuberculosis despite within-host variability in bacterial killing. Nat. Med. 20, 75–79 (2014).
Xie, Y. L. et al. Fourteen-day PET/CT imaging to monitor drug combination activity in treated individuals with tuberculosis. Sci. Transl. Med. 13, eabd7618 (2021).
Zhu, J., Liu, Y. J. & Fortune, S. M. Spatiotemporal perspectives on tuberculosis chemotherapy. Curr. Opin. Microbiol. 72, 102266 (2023).
Dorman, S. E. et al. Four-month rifapentine regimens with or without moxifloxacin for tuberculosis. N. Engl. J. Med. 384, 1705–1718 (2021). The first successful trial in more than four decades of treatment shortening in patients with DS-TB, reducing therapy duration from 6 to 4 months.
Conradie, F. et al. Treatment of highly drug-resistant pulmonary tuberculosis. N. Engl. J. Med. 382, 893–902 (2020). A landmark clinical trial that successfully reduced treatment duration from 18–24 months to 6 months for patients with drug-resistant TB, showing the power of novel mechanisms of action.
Dahl, V. N. et al. Global trends of pulmonary infections with nontuberculous mycobacteria: a systematic review. Int. J. Infect. Dis. 125, 120–131 (2022).
Honda, J. R., Bernhard, J. N. & Chan, E. D. Natural disasters and nontuberculous mycobacteria: a recipe for increased disease? Chest 147, 304–308 (2015).
Mirsaeidi, M. & Sadikot, R. T. Gender susceptibility to mycobacterial infections in patients with non-CF bronchiectasis. Int. J. Mycobacteriol. 4, 92–96 (2015).
Andrejak, C. et al. Chronic respiratory disease, inhaled corticosteroids and risk of non-tuberculous mycobacteriosis. Thorax 68, 256–262 (2013).
Chan, E. D. & Iseman, M. D. Underlying host risk factors for nontuberculous mycobacterial lung disease. Semin. Respir. Crit. Care Med. 34, 110–123 (2013).
Abidin, N. Z. et al. Trends in nontuberculous mycobacteria infection in children and young people with cystic fibrosis. J. Cyst. Fibros. 20, 737–741 (2021).
Brugha, R. & Spencer, H. Mycobacterium abscessus in cystic fibrosis. Science 372, 465–466 (2021).
Honda, J. R., Virdi, R. & Chan, E. D. Global environmental nontuberculous mycobacteria and their contemporaneous man-made and natural niches. Front. Microbiol. 9, 2029 (2018).
Kim, D. H. et al. In vitro activity and clinical outcomes of clofazimine for nontuberculous mycobacteria pulmonary disease. J. Clin. Med. 10, 4581 (2021).
Pfaeffle, H. O. I. et al. Clofazimine for treatment of multidrug-resistant non-tuberculous mycobacteria. Pulm. Pharmacol. Ther. 70, 102058 (2021).
Holt, M. R. & Baird, T. Treatment approaches to Mycobacterium abscessus pulmonary disease. Clin. Chest Med. 44, 785–798 (2023). A concise but complete review of treatment guidelines, side effects, novel and repurposed therapeutic options for MAB-PD.
van Ingen, J., Boeree, M. J., van Soolingen, D. & Mouton, J. W. Resistance mechanisms and drug susceptibility testing of nontuberculous mycobacteria. Drug Resist. Updat. 15, 149–161 (2012).
Falkinham, J. O. III Ecology of nontuberculous mycobacteria — where do human infections come from? Semin. Respir. Crit. Care Med. 34, 95–102 (2013).
Fennelly, K. P. et al. Biofilm formation by Mycobacterium abscessus in a lung cavity. Am. J. Respir. Crit. Care Med. 193, 692–693 (2016).
Henkle, E. & Winthrop, K. L. Nontuberculous mycobacteria infections in immunosuppressed hosts. Clin. Chest Med. 36, 91–99 (2015).
O’Connell, M. L. et al. Lung manifestations in an autopsy-based series of pulmonary or disseminated nontuberculous mycobacterial disease. Chest 141, 1203–1209 (2012).
Klein, J. L., Corbett, E. L., Slade, P. M., Miller, R. F. & Coker, R. J. Mycobacterium kansasii and human immunodeficiency virus co-infection in London. J. Infect. 37, 252–259 (1998).
Tomashefski, J. F. Jr, Stern, R. C., Demko, C. A. & Doershuk, C. F. Nontuberculous mycobacteria in cystic fibrosis. An autopsy study. Am. J. Respir. Crit. Care Med. 154, 523–528 (1996).
Swenson, C., Zerbe, C. S. & Fennelly, K. Host variability in NTM disease: implications for research needs. Front. Microbiol. 9, 2901 (2018).
Koh, W. J., Hong, G., Kim, K., Ahn, S. & Han, J. Pulmonary sequestration infected with nontuberculous mycobacteria: a report of two cases and literature review. Asian Pac. J. Trop. Med. 5, 917–919 (2012).
Merckx, J. J., Soule, E. H. & Karlson, A. G. The histopathology of lesions caused by infection with unclassified acid-fast bacteria in man. Report of 25 cases. Am. J. Clin. Pathol. 41, 244–255 (1964).
Yuan, M. K. et al. Comparative chest computed tomography findings of non-tuberculous mycobacterial lung diseases and pulmonary tuberculosis in patients with acid fast bacilli smear-positive sputum. BMC Pulm. Med. 14, 65 (2014).
Oshitani, Y. et al. Characteristic chest CT findings for progressive cavities in Mycobacterium avium complex pulmonary disease: a retrospective cohort study. Respir. Res. 21, 10 (2020).
Jeong, Y. J. et al. Nontuberculous mycobacterial pulmonary infection in immunocompetent patients: comparison of thin-section CT and histopathologic findings. Radiology 231, 880–886 (2004).
Kwon, Y. S. & Koh, W. J. Diagnosis of pulmonary tuberculosis and nontuberculous mycobacterial lung disease in Korea. Tuberc. Respir. Dis. 77, 1–5 (2014).
Jain, D., Ghosh, S., Teixeira, L. & Mukhopadhyay, S. Pathology of pulmonary tuberculosis and non-tuberculous mycobacterial lung disease: facts, misconceptions, and practical tips for pathologists. Semin. Diagn. Pathol. 34, 518–529 (2017). A review of the radiological and immunopathological similarities and differences between pulmonary tuberculosis and NTM lung disease.
Barry, C. E. III et al. The spectrum of latent tuberculosis: rethinking the biology and intervention strategies. Nat. Rev. Microbiol. 7, 845–855 (2009).
Griffith, D. E. et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am. J. Respir. Crit. Care Med. 175, 367–416 (2007).
Jo, K. W., Park, Y. E., Chong, Y. P. & Shim, T. S. Spontaneous sputum conversion and reversion in Mycobacterium abscessus complex lung disease. PLoS ONE 15, e0232161 (2020).
Kim, B., Yu, J. Y. & Jhun, B. W. Spontaneous cultural conversion rate of Mycobacterium avium complex pulmonary disease based on baces severity. J. Clin. Med. 12, 7125 (2023).
National Tuberculosis Institute. Tuberculosis in a rural population of South India: a five-year epidemiological study. Bull. World Health Organ. 51, 473–488 (1974).
Mehra, S. et al. The DosR regulon modulates adaptive immunity and is essential for Mycobacterium tuberculosis persistence. Am. J. Respir. Crit. Care Med. 191, 1185–1196 (2015).
Gerasimova, A., Kazakov, A. E., Arkin, A. P., Dubchak, I. & Gelfand, M. S. Comparative genomics of the dormancy regulons in mycobacteria. J. Bacteriol. 193, 3446–3452 (2011).
Belardinelli, J. M. et al. Therapeutic efficacy of antimalarial drugs targeting DosRS signaling in Mycobacterium abscessus. Sci. Transl. Med. 14, eabj3860 (2022).
Qvist, T. et al. Chronic pulmonary disease with Mycobacterium abscessus complex is a biofilm infection. Eur. Respir. J. 46, 1823–1826 (2015).
Mishra, R. et al. Mechanopathology of biofilm-like Mycobacterium tuberculosis cords. Cell 186, 5135–5150.e28 (2023).
Ankomah, P. & Levin, B. R. Exploring the collaboration between antibiotics and the immune response in the treatment of acute, self-limiting infections. Proc. Natl Acad. Sci. USA 111, 8331–8338 (2014).
Brown-Elliott, B. A. & Woods, G. L. Antimycobacterial susceptibility testing of nontuberculous mycobacteria. J. Clin. Microbiol. 57, e00834-19 (2019).
WHO. Rapid Communication: Key Changes to the Treatment of Drug-resistant Tuberculosis. https://www.who.int/publications/i/item/WHO-UCN-TB-2022-2 (2022).
Ji, B. et al. In vitro and in vivo activities of moxifloxacin and clinafloxacin against Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 42, 2066–2069 (1998).
Zurenko, G. E. et al. In vitro activities of U-100592 and U-100766, novel oxazolidinone antibacterial agents. Antimicrob. Agents Chemother. 40, 839–845 (1996).
Yun, H. Y. et al. Model-based efficacy and toxicity comparisons of moxifloxacin for multidrug-resistant tuberculosis. Open Forum Infect. Dis. 9, ofab660 (2022).
Alghamdi, W. A. et al. Population pharmacokinetics of linezolid in tuberculosis patients: dosing regimen simulation and target attainment analysis. Antimicrob. Agents Chemother. 64, e01174-20 (2020).
Leach, K. L., Brickner, S. J., Noe, M. C. & Miller, P. F. Linezolid, the first oxazolidinone antibacterial agent. Ann. N. Y. Acad. Sci. 1222, 49–54 (2011).
Ahmad, N. et al. Treatment correlates of successful outcomes in pulmonary multidrug-resistant tuberculosis: an individual patient data meta-analysis. Lancet 392, 821–834 (2018).
Falzon, D. et al. Resistance to fluoroquinolones and second-line injectable drugs: impact on multidrug-resistant TB outcomes. Eur. Respir. J. 42, 156–168 (2013).
Dheda, K. et al. The Lancet Respiratory Medicine Commission: 2019 update: epidemiology, pathogenesis, transmission, diagnosis, and management of multidrug-resistant and incurable tuberculosis. Lancet Respir. Med. 7, 820–826 (2019).
Dreyer, V. et al. High fluoroquinolone resistance proportions among multidrug-resistant tuberculosis driven by dominant L2 Mycobacterium tuberculosis clones in the Mumbai Metropolitan Region. Genome Med. 14, 95 (2022).
Agrawal, D., Udwadia, Z. F., Rodriguez, C. & Mehta, A. Increasing incidence of fluoroquinolone-resistant Mycobacterium tuberculosis in Mumbai, India. Int. J. Tuberc. Lung Dis. 13, 79–83 (2009).
Mbelele, P. M. et al. Whole genome sequencing-based drug resistance predictions of multidrug-resistant Mycobacterium tuberculosis isolates from Tanzania. JAC Antimicrob. Resist. 4, dlac042 (2022).
Ament, P. W., Jamshed, N. & Horne, J. P. Linezolid: its role in the treatment of Gram-positive, drug-resistant bacterial infections. Am. Fam. Physician 65, 663–670 (2002).
Thwaites, G. & Nguyen, N. V. Linezolid for drug-resistant tuberculosis. N. Engl. J. Med. 387, 842–843 (2022).
Tse-Chang, A., Kunimoto, D., Der, E. & Ahmed, R. Assessment of linezolid efficacy, safety and tolerability in the treatment of tuberculosis: a retrospective case review. Can. J. Infect. Dis. Med. Microbiol. 24, 535616 (2013).
Van Rie, A. et al. Balancing access to BPaLM regimens and risk of resistance. Lancet Infect. Dis. 22, 1411–1412 (2022).
Kim, J. S. et al. Early bactericidal activity of delpazolid (LCB01-0371) in patients with pulmonary tuberculosis. Antimicrob. Agents Chemother. 66, e0168421 (2022).
Wallis, R. S. et al. Mycobactericidal activity of sutezolid (PNU-100480) in sputum (EBA) and blood (WBA) of patients with pulmonary tuberculosis. PLoS ONE 9, e94462 (2014).
Conradie, F. et al. Bedaquiline–pretomanid–linezolid regimens for drug-resistant tuberculosis. N. Engl. J. Med. 387, 810–823 (2022).
Wallace, R. J. Jr et al. Initial clarithromycin monotherapy for Mycobacterium avium–intracellulare complex lung disease. Am. J. Respir. Crit. Care Med. 149, 1335–1341 (1994).
Li, G. et al. Antimicrobial susceptibility of standard strains of nontuberculous mycobacteria by microplate Alamar Blue assay. PLoS ONE 8, e84065 (2013).
Zheng, H. et al. In vitro activity of pretomanid against nontuberculous mycobacteria. Antimicrob. Agents Chemother. 66, e0181021 (2022).
Yu, X. et al. In vitro activities of bedaquiline and delamanid against nontuberculous mycobacteria isolated in Beijing, China. Antimicrob. Agents Chemother. 63, e00031-19 (2019).
Heifets, L., Higgins, M. & Simon, B. Pyrazinamide is not active against Mycobacterium tuberculosis residing in cultured human monocyte-derived macrophages. Int. J. Tuberc. Lung Dis. 4, 491–495 (2000).
Reingewertz, T. H. et al. Differential sensitivity of mycobacteria to isoniazid is related to differences in KatG-mediated enzymatic activation of the drug. Antimicrob. Agents Chemother. 64, e01899-19 (2020).
Cowman, S., Burns, K., Benson, S., Wilson, R. & Loebinger, M. R. The antimicrobial susceptibility of non-tuberculous mycobacteria. J. Infect. 72, 324–331 (2016).
Kim, D. H. et al. In vitro activity of bedaquiline and delamanid against nontuberculous mycobacteria, including macrolide-resistant clinical isolates. Antimicrob. Agents Chemother. 63, e00665-19 (2019).
Boorgula, G. D. et al. Isoniazid pharmacokinetics/pharmacodynamics as monotherapy and in combination regimen in the hollow fiber system model of Mycobacterium kansasii. Tuberculosis 138, 102289 (2022).
Mudde, S. E., Upton, A. M., Lenaerts, A., Bax, H. I. & De Steenwinkel, J. E. M. Delamanid or pretomanid? A Solomonic judgement! J. Antimicrob. Chemother. 77, 880–902 (2022).
Vilcheze, C. & Jacobs, W. R. Jr The isoniazid paradigm of killing, resistance, and persistence in Mycobacterium tuberculosis. J. Mol. Biol. 431, 3450–3461 (2019).
Gopal, P., Gruber, G., Dartois, V. & Dick, T. Pharmacological and molecular mechanisms behind the sterilizing activity of pyrazinamide. Trends Pharmacol. Sci. 40, 930–940 (2019).
Ushtanit, A. et al. Molecular determinants of ethionamide resistance in clinical isolates of Mycobacterium tuberculosis. Antibiotics 11, 133 (2022).
Guerrero, C. et al. Evaluation of the rpoB gene in rifampicin-susceptible and -resistant Mycobacterium avium and Mycobacterium intracellulare. J. Antimicrob. Chemother. 33, 661–663 (1994).
Moon, S. M. et al. Relationship between resistance to ethambutol and rifampin and clinical outcomes in Mycobacterium avium complex pulmonary disease. Antimicrob. Agents Chemother. 66, e0202721 (2022).
Hombach, M., Somoskovi, A., Homke, R., Ritter, C. & Bottger, E. C. Drug susceptibility distributions in slowly growing non-tuberculous mycobacteria using MGIT 960 TB eXiST. Int. J. Med. Microbiol. 303, 270–276 (2013).
Schon, T. et al. Evaluation of wild-type MIC distributions as a tool for determination of clinical breakpoints for Mycobacterium tuberculosis. J. Antimicrob. Chemother. 64, 786–793 (2009).
Schildkraut, J. A. et al. The role of rifampicin within the treatment of Mycobacterium avium pulmonary disease. Antimicrob. Agents Chemother. 67, e0087423 (2023).
Schon, T. & Chryssanthou, E. Minimum inhibitory concentration distributions for Mycobacterium avium complex — towards evidence-based susceptibility breakpoints. Int. J. Infect. Dis. 55, 122–124 (2017).
Andries, K. et al. A diarylquinoline drug active on the ATP synthase of Mycobacterium tuberculosis. Science 307, 223–227 (2005).
Lounis, N., Gevers, T., Van den Berg, J., Vranckx, L. & Andries, K. ATP synthase inhibition of Mycobacterium avium is not bactericidal. Antimicrob. Agents Chemother. 53, 4927–4929 (2009).
Ruth, M. M. et al. A bedaquiline/clofazimine combination regimen might add activity to the treatment of clinically relevant non-tuberculous mycobacteria. J. Antimicrob. Chemother. 74, 935–943 (2019).
Lindman, M. & Dick, T. Bedaquiline eliminates bactericidal activity of β-lactams against Mycobacterium abscessus. Antimicrob. Agents Chemother. 63, e00827-19 (2019).
Froberg, G. et al. Towards clinical breakpoints for non-tuberculous mycobacteria – determination of epidemiological cut off values for the Mycobacterium avium complex and Mycobacterium abscessus using broth microdilution. Clin. Microbiol. Infect. 29, 758–764 (2023).
Roemhild, R., Bollenbach, T. & Andersson, D. I. The physiology and genetics of bacterial responses to antibiotic combinations. Nat. Rev. Microbiol. 20, 478–490 (2022).
Gupta, R. et al. The Mycobacterium tuberculosis protein LdtMt2 is a nonclassical transpeptidase required for virulence and resistance to amoxicillin. Nat. Med. 16, 466–469 (2010).
Rifat, D., Chen, L., Kreiswirth, B. N. & Nuermberger, E. L. Genome-wide essentiality analysis of Mycobacterium abscessus by saturated transposon mutagenesis and deep sequencing. mBio 12, e0104921 (2021).
Nguyen, D. C. et al. “One-Two Punch”: synergistic ss-lactam combinations for Mycobacterium abscessus and target redundancy in the inhibition of peptidoglycan synthesis enzymes. Clin. Infect. Dis. 73, 1532–1536 (2021).
Negatu, D. A., Zimmerman, M., Dartois, V. A. & Dick, T. Strongly bactericidal all-oral β-lactam combinations for the treatment of Mycobacterium abscessus lung disease. Antimicrob. Agents Chemother. 66, e0079022 (2022).
Lee, M. et al. Linezolid for treatment of chronic extensively drug-resistant tuberculosis. N. Engl. J. Med. 367, 1508–1518 (2012).
Ignatius, E. H. & Dooley, K. E. New drugs for the treatment of tuberculosis. Clin. Chest Med. 40, 811–827 (2019).
Cho, Y. L. & Jang, J. Development of delpazolid for the treatment of tuberculosis. Appl. Sci. 10, 2211 (2020).
Negatu, D. A., Aragaw, W. W., Cangialosi, J., Dartois, V. & Dick, T. Side-by-side profiling of oxazolidinones to estimate the therapeutic window against mycobacterial infections. Antimicrob. Agents Chemother. 67, e0165522 (2023).
Mdluli, K. C. et al. TBI-223: a safer oxazolidinone in pre-clinical development for tuberculosis. In ASM Microbe 2017 (ASM, 2017).
McLeay, S. C., Vis, P., van Heeswijk, R. P. & Green, B. Population pharmacokinetics of bedaquiline (TMC207), a novel antituberculosis drug. Antimicrob. Agents Chemother. 58, 5315–5324 (2014).
Keutzer, L., Akhondipour Salehabad, Y., Davies Forsman, L. & Simonsson, U. S. H. A modeling-based proposal for safe and efficacious reintroduction of bedaquiline after dose interruption: a population pharmacokinetics study. CPT Pharmacomet. Syst. Pharmacol. 11, 628–639 (2022).
Mallick, J. S., Nair, P., Abbew, E. T., Van Deun, A. & Decroo, T. Acquired bedaquiline resistance during the treatment of drug-resistant tuberculosis: a systematic review. JAC Antimicrob. Resist. 4, dlac029 (2022).
Brown, T. S. et al. Genotype-phenotype characterization of serial Mycobacterium tuberculosis isolates in bedaquiline-resistant tuberculosis. Clin. Infect. Dis. https://doi.org/10.1093/cid/ciad596 (2023).
Sutherland, H. S. et al. Variations in the C-unit of bedaquiline provides analogues with improved biology and pharmacology. Bioorg. Med. Chem. 28, 115213 (2020).
Briffotaux, J., Huang, W., Wang, X. & Gicquel, B. MmpS5/MmpL5 as an efflux pump in Mycobacterium species. Tuberculosis 107, 13–19 (2017).
Xu, J. et al. Contribution of pretomanid to novel regimens containing bedaquiline with either linezolid or moxifloxacin and pyrazinamide in murine models of tuberculosis. Antimicrob. Agents Chemother. 63, e00021-19 (2019).
Almeida, D. et al. Comparative efficacy of the novel diarylquinoline TBAJ-876 and bedaquiline against a resistant Rv0678 mutant in a mouse model of tuberculosis. Antimicrob. Agents Chemother. 65, e0141221 (2021).
Yao, R. et al. Sudapyridine (WX-081), a novel compound against Mycobacterium tuberculosis. Microbiol. Spectr. 10, e0247721 (2022).
Huang, Z. et al. Discovery and preclinical profile of sudapyridine (WX-081), a novel anti-tuberculosis agent. Bioorg. Med. Chem. Lett. 71, 128824 (2022).
Sarathy, J. P. et al. TBAJ-876, a 3,5-dialkoxypyridine analogue of bedaquiline, is active against Mycobacterium abscessus. Antimicrob. Agents Chemother. 64, e02404-19 (2020).
Di Modugno, E. et al. In vitro activity of the tribactam GV104326 against Gram-positive, Gram-negative, and anaerobic bacteria. Antimicrob. Agents Chemother. 38, 2362–2368 (1994).
Lee, R. E. et al. Spectinamides: a new class of semisynthetic antituberculosis agents that overcome native drug efflux. Nat. Med. 20, 152–158 (2014).
Robertson, G. T. et al. Spectinamides are effective partner agents for the treatment of tuberculosis in multiple mouse infection models. J. Antimicrob. Chemother. 72, 770–777 (2017).
Rominski, A., Roditscheff, A., Selchow, P., Bottger, E. C. & Sander, P. Intrinsic rifamycin resistance of Mycobacterium abscessus is mediated by ADP-ribosyltransferase MAB_0591. J. Antimicrob. Chemother. 72, 376–384 (2017).
Kumar, K., Daley, C. L., Griffith, D. E. & Loebinger, M. R. Management of Mycobacterium avium complex and Mycobacterium abscessus pulmonary disease: therapeutic advances and emerging treatments. Eur. Respir. Rev. 31, 210212 (2022).
Baysarowich, J. et al. Rifamycin antibiotic resistance by ADP-ribosylation: structure and diversity of Arr. Proc. Natl Acad. Sci. USA 105, 4886–4891 (2008).
Ganapathy, U. S. et al. Blocking bacterial naphthohydroquinone oxidation and ADP-ribosylation improves activity of rifamycins against Mycobacterium abscessus. Antimicrob. Agents Chemother. 65, e0097821 (2021).
Prideaux, B. et al. The association between sterilizing activity and drug distribution into tuberculosis lesions. Nat. Med. 21, 1223–1227 (2015).
Sarathy, J. P. et al. Extreme drug tolerance of Mycobacterium tuberculosis in caseum. Antimicrob. Agents Chemother. 62, e02266–e02317 (2018).
Kolpen, M. et al. Biofilms of Mycobacterium abscessus complex can be sensitized to antibiotics by disaggregation and oxygenation. Antimicrob. Agents Chemother. 64, e01212-19 (2020).
Lan, T. et al. Redesign of rifamycin antibiotics to overcome ADP-ribosylation-mediated resistance. Angew. Chem. Int. Ed. Engl. 61, e202211498 (2022).
Paulowski, L. et al. C25-modified rifamycin derivatives with improved activity against Mycobacterium abscessus. PNAS Nexus 1, pgac130 (2022).
Payne, D. J., Gwynn, M. N., Holmes, D. J. & Pompliano, D. L. Drugs for bad bugs: confronting the challenges of antibacterial discovery. Nat. Rev. Drug. Discov. 6, 29–40 (2007).
Vincent, F. et al. Phenotypic drug discovery: recent successes, lessons learned and new directions. Nat. Rev. Drug. Discov. 21, 899–914 (2022). A review discussing the successes and challenges of modern phenotypic — as opposed to target-based — drug discovery, which combines original concepts with modern tools and strategies.
Working Group on New TB Drugs. Clinical Pipeline https://www.newtbdrugs.org/pipeline/clinical (2023).
Working Group on New TB Drugs. 2023 Global New TB Drug Discovery Pipeline https://www.newtbdrugs.org/pipeline/discovery (2023).
Fernandes, G. F. S., Thompson, A. M., Castagnolo, D., Denny, W. A. & Dos Santos, J. L. Tuberculosis drug discovery: challenges and new horizons. J. Med. Chem. 65, 7489–7531 (2022). A recent update of preclinical anti-TB compounds with in vivo efficacy against TB, and the global pipeline of drug candidates in clinical development, with a focus on mechanism of action.
Sethiya, J. P., Sowards, M. A., Jackson, M. & North, E. J. MmpL3 inhibition: a new approach to treat nontuberculous mycobacterial infections. Int. J. Mol. Sci. 21, 6202 (2020).
Sarathy, J. P., Zimmerman, M. D., Gengenbacher, M., Dartois, V. & Dick, T. Mycobacterium tuberculosis DprE1 inhibitor OPC-167832 is active against Mycobacterium abscessus in vitro. Antimicrob. Agents Chemother. 66, e0123722 (2022).
Li, W. et al. Direct inhibition of MmpL3 by novel antitubercular compounds. ACS Infect. Dis. 5, 1001–1012 (2019).
Rudraraju, R. S. et al. Mycobacterium tuberculosis KasA as a drug target: structure-based inhibitor design. Front. Cell Infect. Microbiol. 12, 1008213 (2022).
Fang, C. et al. Discovery of heterocyclic replacements for the coumarin core of anti-tubercular FadD32 inhibitors. Bioorg. Med. Chem. Lett. 28, 3529–3533 (2018).
Aggarwal, A. et al. Development of a novel lead that targets M. tuberculosis polyketide synthase 13. Cell 170, 249–259 e225 (2017).
Hugonnet, J. E., Tremblay, L. W., Boshoff, H. I., Barry, C. E. III & Blanchard, J. S. Meropenem–clavulanate is effective against extensively drug-resistant Mycobacterium tuberculosis. Science 323, 1215–1218 (2009).
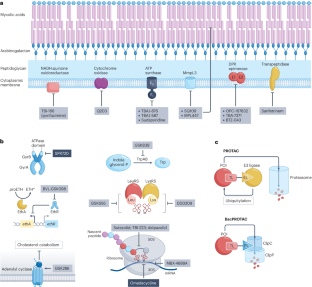
Vilchèze, C. Mycobacterial cell wall: a source of successful targets for old and new drugs. Appl. Sci. 10, 2278 (2020).
Li, S. et al. CRISPRi chemical genetics and comparative genomics identify genes mediating drug potency in Mycobacterium tuberculosis. Nat. Microbiol. 7, 766–779 (2022). A research article that describes the application of CRISPR interference to bacterial gene silencing to discover mechanisms of intrinsic and acquired resistance and targets for synergistic drug combinations.
Beites, T. et al. Plasticity of the Mycobacterium tuberculosis respiratory chain and its impact on tuberculosis drug development. Nat. Commun. 10, 4970 (2019).
Jeffreys, L. N. et al. Identification of 2-aryl-quinolone inhibitors of cytochrome bd and chemical validation of combination strategies for respiratory inhibitors against Mycobacterium tuberculosis. ACS Infect. Dis. 9, 221–238 (2023).
Lee, B. S. et al. Dual inhibition of the terminal oxidases eradicates antibiotic-tolerant Mycobacterium tuberculosis. EMBO Mol. Med. 13, e13207 (2021).
Singh, R. et al. PA-824 kills nonreplicating Mycobacterium tuberculosis by intracellular NO release. Science 322, 1392–1395 (2008).
Kwon, N. H., Fox, P. L. & Kim, S. Aminoacyl-tRNA synthetases as therapeutic targets. Nat. Rev. Drug. Discov. 18, 629–650 (2019).
Li, X. et al. Discovery of a potent and specific M. tuberculosis leucyl-tRNA synthetase inhibitor: (S)-3-(aminomethyl)-4-chloro-7-(2-hydroxyethoxy)benzo[c][1,2]oxaborol-1(3H)-ol (GSK656). J. Med. Chem. 60, 8011–8026 (2017).
Green, S. R. et al. Lysyl-tRNA synthetase, a target for urgently needed M. tuberculosis drugs. Nat. Commun. 13, 5992 (2022).
Abrahams, K. A. et al. Inhibiting mycobacterial tryptophan synthase by targeting the inter-subunit interface. Sci. Rep. 7, 9430 (2017).
Brown, K. L. et al. Cyclic AMP-mediated inhibition of cholesterol catabolism in Mycobacterium tuberculosis by the novel drug candidate GSK2556286. Antimicrob. Agents Chemother. 67, e0129422 (2023).
Kim, M. J. et al. Caseation of human tuberculosis granulomas correlates with elevated host lipid metabolism. EMBO Mol. Med. 2, 258–274 (2010).
Guerrini, V. et al. Storage lipid studies in tuberculosis reveal that foam cell biogenesis is disease-specific. PLoS Pathog. 14, e1007223 (2018).
Nuermberger, E. L. et al. GSK2556286 is a novel antitubercular drug candidate effective in vivo with the potential to shorten tuberculosis treatment. Antimicrob. Agents Chemother. 66, e0013222 (2022).
Lupoli, T. J., Vaubourgeix, J., Burns-Huang, K. & Gold, B. Targeting the proteostasis network for mycobacterial drug discovery. ACS Infect. Dis. 4, 478–498 (2018).
Bhandari, V. et al. The role of ClpP protease in bacterial pathogenesis and human diseases. ACS Chem. Biol. 13, 1413–1425 (2018).
Hawkins, P. M. E. et al. Potent bactericidal antimycobacterials targeting the chaperone ClpC1 based on the depsipeptide natural products ecumicin and ohmyungsamycin A. J. Med. Chem. 65, 4893–4908 (2022).
Maitre, T., Baulard, A., Aubry, A. & Veziris, N. Optimizing the use of current antituberculosis drugs to overcome drug resistance in Mycobacterium tuberculosis. Infect. Dis. Now. 54, 104807 (2023).
Blondiaux, N. et al. Reversion of antibiotic resistance in Mycobacterium tuberculosis by spiroisoxazoline SMARt-420. Science 355, 1206–1211 (2017).
Flipo, M. et al. The small-molecule SMARt751 reverses Mycobacterium tuberculosis resistance to ethionamide in acute and chronic mouse models of tuberculosis. Sci. Transl. Med. 14, eaaz6280 (2022).
Rubin, E. J. Reviving a drug for tuberculosis? N. Engl. J. Med. 376, 2292–2294 (2017).
Ganapathy, U. S. & Dick, T. Why matter matters: fast-tracking Mycobacterium abscessus drug discovery. Molecules 27, 6948 (2022). A survey of anti-TB agents that have shown in vivo efficacy in MAB mouse models, showing the value of screening advanced TB chemical matter as a means of fast-tracking MAB drug discovery and highlighting the dire state of the pipeline.
Chong, S. L., Tan, J. L. & Ngeow, Y. F. The resistomes of Mycobacteroides abscessus complex and their possible acquisition from horizontal gene transfer. BMC Genomics 23, 715 (2022).
Bekes, M., Langley, D. R. & Crews, C. M. PROTAC targeted protein degraders: the past is prologue. Nat. Rev. Drug. Discov. 21, 181–200 (2022).
Morreale, F. E. et al. BacPROTACs mediate targeted protein degradation in bacteria. Cell 185, 2338–2353 e2318 (2022).
Hoi, D. M. et al. Clp-targeting BacPROTACs impair mycobacterial proteostasis and survival. Cell 186, 2176–2192.e22 (2023).
Nuermberger, E. L. Preclinical efficacy testing of new drug candidates. Microbiol. Spectr. 5, https://doi.org/10.1128/microbiolspec.TBTB2-0034-2017 (2017).
Tasneen, R. et al. Novel regimens of bedaquiline-pyrazinamide combined with moxifloxacin, rifabutin, delamanid and/or OPC-167832 in murine tuberculosis models. Antimicrob. Agents Chemother. 66, e0239821 (2022).
Irwin, S. M. et al. Presence of multiple lesion types with vastly different microenvironments in C3HeB/FeJ mice following aerosol infection with Mycobacterium tuberculosis. Dis. Model. Mech. 8, 591–602 (2015).
Ernest, J. P. et al. Development of new tuberculosis drugs: translation to regimen composition for drug-sensitive and multidrug-resistant tuberculosis. Annu. Rev. Pharmacol. Toxicol. 61, 495–516 (2021).
Via, L. E. et al. A sterilizing tuberculosis treatment regimen is associated with faster clearance of bacteria in cavitary lesions in marmosets. Antimicrob. Agents Chemother. 59, 4181–4189 (2015).
Lin, P. L. et al. Radiologic responses in cynomolgous macaques for assessing tuberculosis chemotherapy regimens. Antimicrob. Agents Chemother. 57, 4237–4244 (2013).
Obregon-Henao, A. et al. Susceptibility of Mycobacterium abscessus to antimycobacterial drugs in preclinical models. Antimicrob. Agents Chemother. 59, 6904–6912 (2015).
Nicola, F., Cirillo, D. M. & Lore, N. I. Preclinical murine models to study lung infection with Mycobacterium abscessus complex. Tuberculosis 138, 102301 (2023).
De Groote, M. A. et al. GM-CSF knockout mice for preclinical testing of agents with antimicrobial activity against Mycobacterium abscessus. J. Antimicrob. Chemother. 69, 1057–1064 (2014).
Libardo, J., Boshoff, H. I. & Barry, C. E. III The present state of the tuberculosis drug development pipeline. Curr. Opin. Pharmacol. 42, 81–94 (2018).
Berg, A. et al. Model-based meta-analysis of relapsing mouse model studies from the critical path to tuberculosis drug regimens initiative database. Antimicrob. Agents Chemother. 66, e0179321 (2022).
Bartelink, I. H. et al. New paradigm for translational modeling to predict long-term tuberculosis treatment response. Clin. Transl. Sci. 10, 366–379 (2017).
Larkins-Ford, J., Degefu, Y. N., Van, N., Sokolov, A. & Aldridge, B. B. Design principles to assemble drug combinations for effective tuberculosis therapy using interpretable pairwise drug response measurements. Cell Rep. Med. 3, 100737 (2022).
Mudde, S. E. et al. Predictive modeling to study the treatment-shortening potential of novel tuberculosis drug regimens, towards bundling of preclinical data. J. Infect. Dis. 225, 1876–1885 (2021).
Pienaar, E. et al. A computational tool integrating host immunity with antibiotic dynamics to study tuberculosis treatment. J. Theor. Biol. 367, 166–179 (2015).
Dooley, K. E., Hanna, D., Mave, V., Eisenach, K. & Savic, R. M. Advancing the development of new tuberculosis treatment regimens: the essential role of translational and clinical pharmacology and microbiology. PLoS Med. 16, e1002842 (2019).
Davies, G. R. & Wallis, R. S. Methods for selecting regimen duration to prevent relapse in drug-susceptible and drug-resistant TB. Int. J. Tuberc. Lung Dis. 20, 13–17 (2016).
Imperial, M. Z., Phillips, P. P. J., Nahid, P. & Savic, R. M. Precision-enhancing risk stratification tools for selecting optimal treatment durations in tuberculosis clinical trials. Am. J. Respir. Crit. Care Med. 204, 1086–1096 (2021). A retrospective analyses of large TB clinical trials to develop a risk stratification tool for the selection of patient-specific optimal treatment durations.
Chen, R. Y. et al. Using biomarkers to predict TB treatment duration (Predict TB): a prospective, randomized, noninferiority, treatment shortening clinical trial. Gates Open Res. 1, 9 (2017).
Nyang’wa, B. T. et al. A 24-week, all-oral regimen for rifampin-resistant tuberculosis. N. Engl. J. Med. 387, 2331–2343 (2022).
Mok, J. et al. 9 months of delamanid, linezolid, levofloxacin, and pyrazinamide versus conventional therapy for treatment of fluoroquinolone-sensitive multidrug-resistant tuberculosis (MDR-END): a multicentre, randomised, open-label phase 2/3 non-inferiority trial in South Korea. Lancet 400, 1522–1530 (2022).
Paton, N. I. et al. Treatment strategy for rifampin-susceptible tuberculosis. N. Engl. J. Med. 388, 873–887 (2023).
The CRyPTIC Consortium.Genome-wide association studies of global Mycobacterium tuberculosis resistance to 13 antimicrobials in 10,228 genomes identify new resistance mechanisms. PLoS Biol. 20, e3001755 (2022).
Fors, J., Strydom, N., Fox, W. S., Keizer, R. J. & Savic, R. M. Mathematical model and tool to explore shorter multi-drug therapy options for active pulmonary tuberculosis. PLoS Comput. Biol. 16, e1008107 (2020).
Dheda, K. et al. Drug-penetration gradients associated with acquired drug resistance in patients with tuberculosis. Am. J. Respir. Crit. Care Med. 198, 1208–1219 (2018).
Strydom, N. et al. Tuberculosis drugs’ distribution and emergence of resistance in patient’s lung lesions: a mechanistic model and tool for regimen and dose optimization. PLoS Med. 16, e1002773 (2019).
Diacon, A. H. Two steps forward, one step back. N. Engl. J. Med. 387, 2380–2381 (2022).
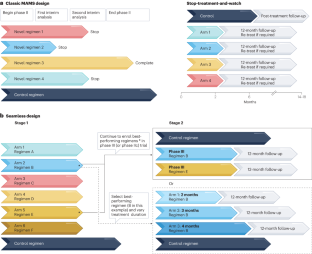
Lienhardt, C. et al. Advances in clinical trial design: weaving tomorrow’s TB treatments. PLoS Med. 17, e1003059 (2020). A review and opinion of present and future advances in clinical trial design to harmonize and accelerate the development of novel TB regimens.
Davies, G., Boeree, M., Hermann, D. & Hoelscher, M. Accelerating the transition of new tuberculosis drug combinations from phase II to phase III trials: new technologies and innovative designs. PLoS Med. 16, e1002851 (2019).
Biomarkers Development Working Group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin. Pharmacol. Ther. 69, 89–95 (2001).
Boeree, M. J. et al. A dose-ranging trial to optimize the dose of rifampin in the treatment of tuberculosis. Am. J. Respir. Crit. Care Med. 191, 1058–1065 (2015).
Wallis, R. S., Wang, C., Meyer, D. & Thomas, N. Month 2 culture status and treatment duration as predictors of tuberculosis relapse risk in a meta-regression model. PLoS ONE 8, e71116 (2013).
Phillips, P. P. et al. Limited role of culture conversion for decision-making in individual patient care and for advancing novel regimens to confirmatory clinical trials. BMC Med. 14, 19 (2016).
Davies, G. R. Early clinical development of anti-tuberculosis drugs: science, statistics and sterilizing activity. Tuberculosis 90, 171–176 (2010).
Bouton, T. C. et al. An optimized background regimen design to evaluate the contribution of levofloxacin to multidrug-resistant tuberculosis treatment regimens: study protocol for a randomized controlled trial. Trials 18, 563 (2017).
Aguilar Diaz, J. M. et al. New and repurposed drugs for the treatment of active tuberculosis: an update for clinicians. Respiration 102, 83–100 (2022).
Esmail, A. et al. An all-oral 6-month regimen for multidrug-resistant tuberculosis: a multicenter, randomized controlled clinical trial (the NExT Study). Am. J. Respir. Crit. Care Med. 205, 1214–1227 (2022).
Chang, V., Phillips, P. P. J., Imperial, M. Z., Nahid, P. & Savic, R. M. A comparison of clinical development pathways to advance tuberculosis regimen development. BMC Infect. Dis. 22, 920 (2022).
Paton, N. I. et al. A treatment strategy for rifampicin-susceptible tuberculosis. N. Engl. J. Med. 388, 873–887 (2023). A landmark clinical trial based on the pioneering paradigm of ‘stop-treatment-and-watch’ to discover treatment-shortening TB drug regimens.
Nogueira, B. M. F. et al. Diagnostic biomarkers for active tuberculosis: progress and challenges. EMBO Mol. Med. 14, e14088 (2022).
CDC. Virtual Meeting of the Advisory Council for the Elimination of Tuberculosis https://www.cdc.gov/faca/committees/pdfs/acet/acet-minutes-20211214-15-508.pdf (2022).
Vinnard, C. et al. Assessing response to therapy for nontuberculous mycobacterial lung disease: quo vadis? Front. Microbiol. 9, 2813 (2018).
Henkle, E. et al. Patient-reported symptom and health-related quality-of-life validation and responsiveness during the first 6 months of treatment for Mycobacterium avium complex pulmonary disease. Chest 164, 53–64 (2023).
Cella, D. et al. Patient-Reported Outcomes in Performance Measurement (RTI Press, 2015).
Waglechner, N. et al. Genomic epidemiology of Mycobacterium abscessus in a Canadian cystic fibrosis centre. Sci. Rep. 12, 16116 (2022).
Zumla, A., Nahid, P. & Cole, S. T. Advances in the development of new tuberculosis drugs and treatment regimens. Nat. Rev. Drug. Discov. 12, 388–404 (2013). The predecessor of the present Review, showing the progress achieved and road travelled over the past 10 years.
Houben, R., Esmail, H., Cobelens, F., Williams, C. M. L. & Coussens, A. K. Tuberculosis prevalence: beyond the tip of the iceberg. Lancet Respir. Med. 10, 537–539 (2022).
van Ingen, J. et al. Nontuberculous mycobacterial lung disease caused by Mycobacterium avium complex – disease burden, unmet needs, and advances in treatment developments. Expert Rev. Respir. Med. 15, 1387–1401 (2021). An overview of treatment guidelines and numerous unmet needs for MAC-PD.
Adjemian, J., Olivier, K. N. & Prevots, D. R. Nontuberculous mycobacteria among patients with cystic fibrosis in the United States: screening practices and environmental risk. Am. J. Respir. Crit. Care Med. 190, 581–586 (2014).
Diel, R., Lipman, M. & Hoefsloot, W. High mortality in patients with Mycobacterium avium complex lung disease: a systematic review. BMC Infect. Dis. 18, 206 (2018).
Jhun, B. W. et al. Prognostic factors associated with long-term mortality in 1445 patients with nontuberculous mycobacterial pulmonary disease: a 15-year follow-up study. Eur. Respir. J. 55, 1900798 (2020).
Griffith, D. E. & Daley, C. L. Treatment of Mycobacterium abscessus pulmonary disease. Chest 161, 64–75 (2022).
Borisov, S. E. et al. Effectiveness and safety of bedaquiline-containing regimens in the treatment of MDR- and XDR-TB: a multicentre study. Eur. Respir. J. 49, 1700387 (2017).
Ndjeka, N. et al. High treatment success rate for multidrug-resistant and extensively drug-resistant tuberculosis using a bedaquiline-containing treatment regimen. Eur. Respir. J. 52, 1801528 (2018).
Xu, H. B., Jiang, R. H. & Li, L. Treatment outcomes for Mycobacterium avium complex: a systematic review and meta-analysis. Eur. J. Clin. Microbiol. Infect. Dis. 33, 347–358 (2014).
Nasiri, M. J. et al. Antibiotic therapy success rate in pulmonary Mycobacterium avium complex: a systematic review and meta-analysis. Expert Rev. Anti Infect. Ther. 18, 263–273 (2020).
Kwak, N. et al. Treatment outcomes of Mycobacterium avium complex lung disease: a systematic review and meta-analysis. Clin. Infect. Dis. 65, 1077–1084 (2017).
Kwak, N. et al. Mycobacterium abscessus pulmonary disease: individual patient data meta-analysis. Eur. Respir. J. 54, 1801991 (2019).
Yano, T. et al. Reduction of clofazimine by mycobacterial type 2 NADH:quinone oxidoreductase: a pathway for the generation of bactericidal levels of reactive oxygen species. J. Biol. Chem. 286, 10276–10287 (2011).
Borisov, S. E. et al. Efficiency and safety of chemotherapy regimen with SQ109 in those suffering from multiple drug resistant tuberculosis [Russian]. Tuberculosis Lung Dis. 96, 6–18 (2018).
Kim, J. et al. Safety, tolerability, pharmacokinetics, and metabolism of telacebec (Q203) for the treatment of tuberculosis: a randomized, placebo-controlled, multiple ascending dose phase 1B trial. Antimicrob. Agents Chemother. 67, e0112322 (2022).
Cevik, M. Abstr. 109. SimpliciTB Results and hepatic safety of pretomanid regimens +/− pyrazinamide. CROI 2023 https://www.croiconference.org/abstract/simplicitb-results-and-hepatic-safety-of-pretomanid-regimens-pyrazinamide/ (2023).
Dierig, A. et al. A phase IIb, open-label, randomized controlled dose ranging multi-centre trial to evaluate the safety, tolerability, pharmacokinetics and exposure-response relationship of different doses of delpazolid in combination with bedaquiline delamanid moxifloxacin in adult subjects with newly diagnosed, uncomplicated, smear-positive, drug-sensitive pulmonary tuberculosis. Trials 24, 382 (2023).
Jindani, A. et al. Four-month high-dose rifampicin regimens for pulmonary tuberculosis. N. Engl. J. Med. 384, 1705–1718 (2023).
Guglielmetti, L. et al. Evaluating newly approved drugs for multidrug-resistant tuberculosis (endTB): study protocol for an adaptive, multi-country randomized controlled trial. Trials 22, 651 (2021).
Boeree, M. J. et al. High-dose rifampicin, moxifloxacin, and SQ109 for treating tuberculosis: a multi-arm, multi-stage randomised controlled trial. Lancet Infect. Dis. 17, 39–49 (2017).
Fox, W., Ellard, G. A. & Mitchison, D. A. Studies on the treatment of tuberculosis undertaken by the British Medical Research Council tuberculosis units, 1946–1986, with relevant subsequent publications. Int. J. Tuberc. Lung Dis. 3, S231–279 (1999).
Dorman, S. E. et al. Substitution of rifapentine for rifampin during intensive phase treatment of pulmonary tuberculosis: study 29 of the tuberculosis trials consortium. J. Infect. Dis. 206, 1030–1040 (2012).
Gillespie, S. H. et al. Four-month moxifloxacin-based regimens for drug-sensitive tuberculosis. N. Engl. J. Med. 371, 1577–1587 (2014).
WHO. Global Tuberculosis Report 2020. Report No. ISBN 978-92-4-001313-1 (WHO, 2020).
Aldridge, B. B. et al. The tuberculosis drug accelerator at year 10: what have we learned? Nat. Med. 27, 1333–1337 (2021). A review of achievements of the Tuberculosis Drug Accelerator, an experiment designed to facilitate collaboration in TB drug discovery by breaking down barriers between competing labs and institutions.
Mekota, A. M. et al. Building sustainable clinical trial sites in sub-Saharan Africa through networking, infrastructure improvement, training and conducting clinical studies: the PanACEA approach. Acta Trop. 238, 106776 (2022).
Koele, S. E. et al. Early bactericidal activity studies for pulmonary tuberculosis: a systematic review of methodological aspects. Int. J. Antimicrob. Agents 61, 106775 (2023).
Ntinginya, N. E. et al. Tuberculosis molecular bacterial load assay reveals early delayed bacterial killing in relapse patients. Clin. Infect. Dis. 76, e990–e994 (2022).
Jones, A. et al. Sputum lipoarabinomannan (LAM) as a biomarker to determine sputum mycobacterial load: exploratory and model-based analyses of integrated data from four cohorts. BMC Infect. Dis. 22, 327 (2022).
Kawasaki, M. et al. Lipoarabinomannan in sputum to detect bacterial load and treatment response in patients with pulmonary tuberculosis: analytic validation and evaluation in two cohorts. PLoS Med. 16, e1002780 (2019).
le Roux, S. P. et al. Resistance-conferring mycobacterial mutations and quantification of early bactericidal activity. Am. J. Respir. Crit. Care Med. 203, 635–637 (2021).
Mukamolova, G. V., Turapov, O., Malkin, J., Woltmann, G. & Barer, M. R. Resuscitation-promoting factors reveal an occult population of tubercle bacilli in sputum. Am. J. Respir. Crit. Care Med. 181, 174–180 (2010).
Chengalroyen, M. D. et al. Detection and quantification of differentially culturable tubercle bacteria in sputum from patients with tuberculosis. Am. J. Respir. Crit. Care Med. 194, 1532–1540 (2016).
Walter, N. D. et al. Mycobacterium tuberculosis precursor rRNA as a measure of treatment-shortening activity of drugs and regimens. Nat. Commun. 12, 2899 (2021).
Acknowledgements
The authors thank A. Diacon for stimulating discussions on present and future biomarkers of TB drug response. T.D. and V.D. receive support from the National Institute of Allergy and Infectious Diseases of the NIH, Award Numbers R01AI132374 and U19 AI142731, and from the Bill & Melinda Gates Foundation, award number INV-004704, respectively. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
V.D. researched data for the article. Both authors contributed substantially to discussion of the content, wrote the article, and edited and reviewed the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Drug Discovery thanks Payam Nahid, Robert Wilkinson and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
ClinicalTrials.gov: https://clinicaltrials.gov
MARK-TB: https://www.mark-tb.org/
Risk Stratification Tool for Tuberculosis Clinical Trial Design: http://saviclab.org/tb-risk/
STOP-TB partnership: https://www.stoptb.org/
The Critical Path to TB Drug Regimen: https://c-path.org/programs/cptr/
The European Accelerator of Tuberculosis Regime Project: https://era4tb.org/
The Project to Accelerate New Treatments for Tuberculosis: https://fnih.org/our-programs/project-accelerate-new-treatments-tuberculosis-pan-tb
The TB Drug Accelerator: https://www.tbdrugaccelerator.org/
Working Group on New Drugs: https://www.newtbdrugs.org/
Glossary
- Clinical breakpoint
-
The minimum inhibitory concentration above which an antimicrobial agent is considered to have a low probability of treatment success in the clinic.
- Minimum inhibitory concentration (MIC)
-
The lowest concentration that inhibits bacterial growth in vitro.
- Non-inferiority trials
-
Designed to show that the effect of a new treatment is not worse than that of an active control by more than a specified margin.
- Pharmacokinetic–pharmacodynamic (PK–PD)
-
The relationship between concentrations achieved in the body or in the tissue of interest (PK) and the concentrations required to exert antibacterial effect (PD).
- Probability of target attainment (PTA)
-
PTA analysis evaluates the plasma exposure of an antibiotic in a patient population (pharmacokinetics) against a target exposure required for efficacy and calculates the likelihood of achieving a specific pharmacokinetic–pharmacodynamic criterion (‘target′) expressed relative to the minimum inhibitory concentration for a pathogen in that patient population.
- Sputum culture conversion
-
Conversion of sputum from which Mycobacterium tuberculosis 9MTB0 can be grown under standardized condition to sputum from which no M. tuberculosis can be cultured. This conversion from positive to negative is the best way to determine whether a patient is responding to treatment. Spontaneous conversion was seen in a fraction of patients during the pre-antibiotic era.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dartois, V., Dick, T. Therapeutic developments for tuberculosis and nontuberculous mycobacterial lung disease. Nat Rev Drug Discov (2024). https://doi.org/10.1038/s41573-024-00897-5
Accepted:
Published:
DOI: https://doi.org/10.1038/s41573-024-00897-5



