Abstract
Neuroblastomas are tumours of sympathetic origin, with a heterogeneous clinical course ranging from localized or spontaneously regressing to widely metastatic disease. Neuroblastomas recapitulate many of the features of sympathoadrenal development, which have been directly targeted to improve the survival outcomes in patients with high-risk disease. Over the past few decades, improvements in the 5-year survival of patients with metastatic neuroblastomas, from <20% to >50%, have resulted from clinical trials incorporating high-dose chemotherapy with autologous stem cell transplantation, differentiating agents and immunotherapy with anti-GD2 monoclonal antibodies. The next generation of trials are designed to improve the initial response rates in patients with high-risk neuroblastomas via the addition of immunotherapies, targeted therapies (such as ALK inhibitors) and radiopharmaceuticals to standard induction regimens. Other trials are focused on testing precision medicine strategies for patients with relapsed and/or refractory disease, enhancing the antitumour immune response and improving the effectiveness of maintenance regimens, in order to prolong disease remission. In this Review, we describe advances in delineating the pathogenesis of neuroblastoma and in identifying the drivers of high-risk disease. We then discuss how this knowledge has informed improvements in risk stratification, risk-adapted therapy and the development of novel therapies.
Key points
-
Neuroblastomas are a biologically and clinically heterogeneous group of tumours; this diversity has implications for pathogenesis, prognosis and treatment.
-
Neuroblastomas emerge from cells of the developing sympathetic nervous system and maintain several of the key features of sympathoadrenal tissues, leading to the development of targeted small molecules, radiopharmaceuticals and immunotherapies.
-
Prospective studies of risk stratification and risk-adapted therapy have sustained the excellent outcomes in patients with low-risk and intermediate-risk neuroblastoma while also reducing the incidence of adverse events; improved outcomes have also been achieved in those with high-risk disease.
-
Rational combination strategies will be necessary to further advance therapies for patients with high-risk neuroblastoma, including efforts to increase the response rates to first-line therapies, develop effective salvage therapies for relapsed and/or refractory disease, and sustain disease remissions.
-
High-risk neuroblastomas are able to suppress antitumour immunity via several mechanisms; chimeric antigen receptor engineering and combination strategies designed to enhance antitumour immune function might ultimately overcome these effects.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
D’Angio, G. J., Evans, A. E. & Koop, C. E. Special pattern of widespread neuroblastoma with a favourable prognosis. Lancet 1, 1046–1049 (1971).
Hero, B. et al. Localized infant neuroblastomas often show spontaneous regression: results of the prospective trials NB95-S and NB97. J. Clin. Oncol. 26, 1504–1510 (2008).
Matthay, K. K. et al. Neuroblastoma. Nat. Rev. Dis. Prim. 2, 16078 (2016).
DuBois, S. G. et al. Metastatic sites in stage IV and IVS neuroblastoma correlate with age, tumor biology, and survival. J. Pediatr. Hematol. Oncol. 21, 181–189 (1999).
Antunes, N. L. et al. Antineuronal antibodies in patients with neuroblastoma and paraneoplastic opsoclonus-myoclonus. J. Pediatr. Hematol. Oncol. 22, 315–320 (2000).
Pugh, T. J. et al. The genetic landscape of high-risk neuroblastoma. Nat. Genet. 45, 279–284 (2013).
Janoueix-Lerosey, I. et al. Overall genomic pattern is a predictor of outcome in neuroblastoma. J. Clin. Oncol. 27, 1026–1033 (2009).
Mosse, Y. P. et al. Identification of ALK as a major familial neuroblastoma predisposition gene. Nature 455, 930–935 (2008).
Amiel, J. et al. Polyalanine expansion and frameshift mutations of the paired-like homeobox gene PHOX2B in congenital central hypoventilation syndrome. Nat. Genet. 33, 459–461 (2003).
Trochet, D. et al. Germline mutations of the paired-like homeobox 2B (PHOX2B) gene in neuroblastoma. Am. J. Hum. Genet. 74, 761–764 (2004).
Bosse, K. R. & Maris, J. M. Advances in the translational genomics of neuroblastoma: from improving risk stratification and revealing novel biology to identifying actionable genomic alterations. Cancer 122, 20–33 (2016).
Diskin, S. J. et al. Common variation at 6q16 within HACE1 and LIN28B influences susceptibility to neuroblastoma. Nat. Genet. 44, 1126–1130 (2012).
Oldridge, D. A. et al. Genetic predisposition to neuroblastoma mediated by a LMO1 super-enhancer polymorphism. Nature 528, 418–421 (2015).
Kratz, C. P. et al. Cancer spectrum and frequency among children with Noonan, Costello, and cardio-facio-cutaneous syndromes. Br. J. Cancer 112, 1392–1397 (2015).
Emery, L. G., Shields, M., Shah, N. R. & Garbes, A. Neuroblastoma associated with Beckwith-Wiedemann syndrome. Cancer 52, 176–179 (1983).
Kamihara, J. et al. Retinoblastoma and neuroblastoma predisposition and surveillance. Clin. Cancer Res. 23, e98–e106 (2017).
Sznewajs, A., Pon, E. & Matthay, K. K. Congenital malformation syndromes associated with peripheral neuroblastic tumors: a systematic review. Pediatr. Blood Cancer 66, e27901 (2019).
George, R. E. et al. Hyperdiploidy plus nonamplified MYCN confers a favorable prognosis in children 12 to 18 months old with disseminated neuroblastoma: a Pediatric Oncology Group study. J. Clin. Oncol. 23, 6466–6473 (2005).
Egolf, L. E. et al. Germline 16p11.2 microdeletion predisposes to neuroblastoma. Am. J. Hum. Genet. 105, 658–668 (2019).
Biegel, J. A. et al. Constitutional 1p36 deletion in a child with neuroblastoma. Am. J. Hum. Genet. 52, 176–182 (1993).
Depuydt, P. et al. Genomic amplifications and distal 6q loss: novel markers for poor survival in high-risk neuroblastoma patients. J. Natl Cancer Inst. 110, 1084–1093 (2018).
Shi, H. et al. ARID1A loss in neuroblastoma promotes the adrenergic-to-mesenchymal transition by regulating enhancer-mediated gene expression. Sci. Adv. 6, eaaz3440 (2020).
Sausen, M. et al. Integrated genomic analyses identify ARID1A and ARID1B alterations in the childhood cancer neuroblastoma. Nat. Genet. 45, 12–17 (2013).
Brodeur, G. M., Seeger, R. C., Schwab, M., Varmus, H. E. & Bishop, J. M. Amplification of N-myc in untreated human neuroblastomas correlates with advanced disease stage. Science 224, 1121–1124 (1984).
Seeger, R. C. et al. Association of multiple copies of the N-myc oncogene with rapid progression of neuroblastomas. N. Engl. J. Med. 313, 1111–1116 (1985).
Liu, Y. et al. The genomic landscape of pediatric and young adult T-lineage acute lymphoblastic leukemia. Nat. Genet. 49, 1211–1218 (2017).
Zimmerman, M. W. et al. MYC drives a subset of high-risk pediatric neuroblastomas and is activated through mechanisms including enhancer hijacking and focal enhancer amplification. Cancer Discov. 8, 320–335 (2018).
Ackermann, S. et al. A mechanistic classification of clinical phenotypes in neuroblastoma. Science 362, 1165–1170 (2018).
Koneru, B. et al. Telomere maintenance mechanisms define clinical outcome in high-risk neuroblastoma. Cancer Res. 80, 2663–2675 (2020).
Peifer, M. et al. Telomerase activation by genomic rearrangements in high-risk neuroblastoma. Nature 526, 700–704 (2015).
Roderwieser, A. et al. Telomerase is a prognostic marker of poor outcome and a therapeutic target in neuroblastoma. JCO Precis. Oncol. https://doi.org/10.1200/po.19.00072 (2019).
Valentijn, L. J. et al. TERT rearrangements are frequent in neuroblastoma and identify aggressive tumors. Nat. Genet. 47, 1411–1414 (2015).
Qadeer, Z. A. et al. ATRX in-frame fusion neuroblastoma is sensitive to EZH2 inhibition via modulation of neuronal gene signatures. Cancer Cell 36, 512–527.e9 (2019).
Brady, S. W. et al. Pan-neuroblastoma analysis reveals age- and signature-associated driver alterations. Nat. Commun. 11, 5183 (2020).
Cheung, N. K. et al. Association of age at diagnosis and genetic mutations in patients with neuroblastoma. JAMA 307, 1062–1071 (2012).
Eleveld, T. F. et al. Relapsed neuroblastomas show frequent RAS-MAPK pathway mutations. Nat. Genet. 47, 864–871 (2015).
Schramm, A. et al. Mutational dynamics between primary and relapse neuroblastomas. Nat. Genet. 47, 872–877 (2015).
Carr-Wilkinson, J. et al. High frequency of p53/MDM2/p14ARF pathway abnormalities in relapsed neuroblastoma. Clin. Cancer Res. 16, 1108–1118 (2010).
Bellini, A. et al. Frequency and prognostic impact of ALK amplifications and mutations in the European Neuroblastoma Study Group (SIOPEN) high-risk neuroblastoma trial (HR-NBL1). J. Clin. Oncol. https://doi.org/10.1200/JCO.21.00086 (2021).
O’Donohue, T. et al. Differential impact of ALK mutations in neuroblastoma. JCO Precis. Oncol. https://doi.org/10.1200/PO.20.00181 (2021).
Zhu, S. et al. Activated ALK collaborates with MYCN in neuroblastoma pathogenesis. Cancer Cell 21, 362–373 (2012).
Berry, T. et al. The ALK(F1174L) mutation potentiates the oncogenic activity of MYCN in neuroblastoma. Cancer Cell 22, 117–130 (2012).
Heukamp, L. C. et al. Targeted expression of mutated ALK induces neuroblastoma in transgenic mice. Sci. Transl. Med. 4, 141ra191 (2012).
Schleiermacher, G. et al. Emergence of new ALK mutations at relapse of neuroblastoma. J. Clin. Oncol. 32, 2727–2734 (2014).
Padovan-Merhar, O. M. et al. Enrichment of targetable mutations in the relapsed neuroblastoma genome. PLoS Genet. 12, e1006501 (2016).
Combaret, V. et al. Detection of tumor ALK status in neuroblastoma patients using peripheral blood. Cancer Med. 4, 540–550 (2015).
Cimmino, F., Lasorsa, V. A., Vetrella, S., Iolascon, A. & Capasso, M. A targeted gene panel for circulating tumor DNA sequencing in neuroblastoma. Front. Oncol. 10, 596191 (2020).
Cheung, N. K. et al. Monoclonal antibodies to a glycolipid antigen on human neuroblastoma cells. Cancer Res. 45, 2642–2649 (1985).
Dubois, S. G. et al. Evaluation of norepinephrine transporter expression and metaiodobenzylguanidine avidity in neuroblastoma: a report from the Children’s Oncology Group. Int. J. Mol. Imaging 2012, 250834 (2012).
Boeva, V. et al. Heterogeneity of neuroblastoma cell identity defined by transcriptional circuitries. Nat. Genet. 49, 1408–1413 (2017).
van Groningen, T. et al. Neuroblastoma is composed of two super-enhancer-associated differentiation states. Nat. Genet. 49, 1261–1266 (2017).
Decaesteker, B. et al. TBX2 is a neuroblastoma core regulatory circuitry component enhancing MYCN/FOXM1 reactivation of DREAM targets. Nat. Commun. 9, 4866 (2018).
Durbin, A. D. et al. Selective gene dependencies in MYCN-amplified neuroblastoma include the core transcriptional regulatory circuitry. Nat. Genet. 50, 1240–1246 (2018).
van Groningen, T. et al. A NOTCH feed-forward loop drives reprogramming from adrenergic to mesenchymal state in neuroblastoma. Nat. Commun. 10, 1530 (2019).
Jansky, S. et al. Single-cell transcriptomic analyses provide insights into the developmental origins of neuroblastoma. Nat. Genet. https://doi.org/10.1038/s41588-021-00806-1 (2021).
Dong, R. et al. Single-cell characterization of malignant phenotypes and developmental trajectories of adrenal neuroblastoma. Cancer Cell 38, 716–733.e6 (2020).
Kildisiute, G. et al. Tumor to normal single-cell mRNA comparisons reveal a pan-neuroblastoma cancer cell. Sci. Adv. https://doi.org/10.1126/sciadv.abd3311 (2021).
Kameneva, P. et al. Single-cell transcriptomics of human embryos identifies multiple sympathoblast lineages with potential implications for neuroblastoma origin. Nat. Genet. 53, 694–706 (2021).
Melaiu, O. et al. PD-L1 is a therapeutic target of the bromodomain inhibitor JQ1 and, combined with HLA class I, a promising prognostic biomarker in neuroblastoma. Clin. Cancer Res. 23, 4462–4472 (2017).
Wolfl, M. et al. Expression of MHC class I, MHC class II, and cancer germline antigens in neuroblastoma. Cancer Immunol. Immunother. 54, 400–406 (2005).
Mina, M. et al. Tumor-infiltrating T lymphocytes improve clinical outcome of therapy-resistant neuroblastoma. Oncoimmunology 4, e1019981 (2015).
Davis, K. L. et al. Nivolumab in children and young adults with relapsed or refractory solid tumours or lymphoma (ADVL1412): a multicentre, open-label, single-arm, phase 1-2 trial. Lancet Oncol. 21, 541–550 (2020).
Merchant, M. S. et al. Phase I clinical trial of ipilimumab in pediatric patients with advanced solid tumors. Clin. Cancer Res. 22, 1364–1370 (2016).
Bernards, R., Dessain, S. K. & Weinberg, R. A. N-myc amplification causes down-modulation of MHC class I antigen expression in neuroblastoma. Cell 47, 667–674 (1986).
Spel, L. et al. Nedd4-binding protein 1 and TNFAIP3-interacting protein 1 control MHC-1 display in neuroblastoma. Cancer Res. 78, 6621–6631 (2018).
Bottino, C. et al. Natural killer cells and neuroblastoma: tumor recognition, escape mechanisms, and possible novel immunotherapeutic approaches. Front. Immunol. 5, 56 (2014).
Raffaghello, L. et al. Downregulation and/or release of NKG2D ligands as immune evasion strategy of human neuroblastoma. Neoplasia 6, 558–568 (2004).
Mao, Y. et al. Targeting suppressive myeloid cells potentiates checkpoint inhibitors to control spontaneous neuroblastoma. Clin. Cancer Res. 22, 3849–3859 (2016).
Asgharzadeh, S. et al. Clinical significance of tumor-associated inflammatory cells in metastatic neuroblastoma. J. Clin. Oncol. 30, 3525–3532 (2012).
Theruvath, J. et al. Anti-GD2 synergizes with CD47 blockade to mediate tumor eradication. Nat. Med. 28, 333–344 (2022).
Morgenstern, D. A. et al. Risk stratification of high-risk metastatic neuroblastoma: a report from the HR-NBL-1/SIOPEN study. Pediatr. Blood Cancer 65, e27363 (2018).
Moreno, L. et al. A nomogram of clinical and biologic factors to predict survival in children newly diagnosed with high-risk neuroblastoma: an International Neuroblastoma Risk Group project. Pediatr. Blood Cancer 68, e28794 (2021).
Strenger, V. et al. Diagnostic and prognostic impact of urinary catecholamines in neuroblastoma patients. Pediatr. Blood Cancer 48, 504–509 (2007).
Matthay, K. K. et al. Criteria for evaluation of disease extent by (123)I-metaiodobenzylguanidine scans in neuroblastoma: a report for the International Neuroblastoma Risk Group (INRG) task force. Br. J. Cancer 102, 1319–1326 (2010).
Lumbroso, J. D. et al. Meta-iodobenzylguanidine (mIBG) scans in neuroblastoma: sensitivity and specificity, a review of 115 scans. Prog. Clin. Biol. Res. 271, 689–705 (1988).
Aboian, M. S. et al. (124)I-MIBG PET/CT to monitor metastatic disease in children with relapsed neuroblastoma. J. Nucl. Med. 62, 43–47 (2021).
Pandit-Taskar, N. et al. Biodistribution and dosimetry of (18)F-meta-fluorobenzylguanidine: a first-in-human PET/CT imaging study of patients with neuroendocrine malignancies. J. Nucl. Med. 59, 147–153 (2018).
Nuchtern, J. G. et al. A prospective study of expectant observation as primary therapy for neuroblastoma in young infants: a Children’s Oncology Group study. Ann. Surg. 256, 573–580 (2012).
Twist, C. J. et al. Defining risk factors for chemotherapeutic intervention in infants with stage 4S neuroblastoma: a report from Children’s Oncology Group study ANBL0531. J. Clin. Oncol. 37, 115–124 (2019).
Peuchmaur, M. et al. Revision of the international neuroblastoma pathology classification: confirmation of favorable and unfavorable prognostic subsets in ganglioneuroblastoma, nodular. Cancer 98, 2274–2281 (2003).
Shimada, H. et al. The international neuroblastoma pathology classification (the Shimada system). Cancer 86, 364–372 (1999).
Brodeur, G. M. et al. Revisions of the international criteria for neuroblastoma diagnosis, staging, and response to treatment. J. Clin. Oncol. 11, 1466–1477 (1993).
Monclair, T. et al. The International Neuroblastoma Risk Group (INRG) staging system: an INRG task force report. J. Clin. Oncol. 27, 298–303 (2009).
Irwin, M. S. et al. Revised neuroblastoma risk classification system: a report from the Children’s Oncology Group. J. Clin. Oncol. https://doi.org/10.1200/JCO.21.00278 (2021).
Meany, H. J. et al. Significance of clinical and biologic features in stage 3 neuroblastoma: a report from the International Neuroblastoma Risk Group project. Pediatr. Blood Cancer 61, 1932–1939 (2014).
Schmidt, M. L. et al. Favorable prognosis for patients 12 to 18 months of age with stage 4 nonamplified MYCN neuroblastoma: a Children’s Cancer Group Study. J. Clin. Oncol. 23, 6474–6480 (2005).
London, W. B. et al. Evidence for an age cutoff greater than 365 days for neuroblastoma risk group stratification in the Children’s Oncology Group. J. Clin. Oncol. 23, 6459–6465 (2005).
Twist, C. J. et al. Maintaining outstanding outcomes using response- and biology-based therapy for intermediate-risk neuroblastoma: a report from the Children’s Oncology Group study ANBL0531. J. Clin. Oncol. 37, 3243–3255 (2019).
Iehara, T. et al. Successful treatment of infants with localized neuroblastoma based on their MYCN status. Int. J. Clin. Oncol. 18, 389–395 (2013).
Strother, D. R. et al. Outcome after surgery alone or with restricted use of chemotherapy for patients with low-risk neuroblastoma: results of Children’s Oncology Group study P9641. J. Clin. Oncol. 30, 1842–1848 (2012).
Matthay, K. K. et al. Successful treatment of stage III neuroblastoma based on prospective biologic staging: a Children’s Cancer Group study. J. Clin. Oncol. 16, 1256–1264 (1998).
Rubie, H. et al. Excellent outcome with reduced treatment in infants with nonmetastatic and unresectable neuroblastoma without MYCN amplification: results of the prospective INES 99.1. J. Clin. Oncol. 29, 449–455 (2011).
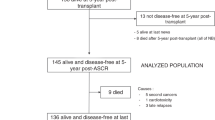
Park, J. R. et al. Effect of tandem autologous stem cell transplant vs single transplant on event-free survival in patients with high-risk neuroblastoma: a randomized clinical trial. JAMA 322, 746–755 (2019).
Ladenstein, R. et al. Busulfan and melphalan versus carboplatin, etoposide, and melphalan as high-dose chemotherapy for high-risk neuroblastoma (HR-NBL1/SIOPEN): an international, randomised, multi-arm, open-label, phase 3 trial. Lancet Oncol. 18, 500–514 (2017).
Applebaum, M. A. et al. Second malignancies in patients with neuroblastoma: the effects of risk-based therapy. Pediatr. Blood Cancer 62, 128–133 (2015).
Cohen, L. E. et al. Late effects in children treated with intensive multimodal therapy for high-risk neuroblastoma: high incidence of endocrine and growth problems. Bone Marrow Transpl. 49, 502–508 (2014).
Friedman, D. N. & Henderson, T. O. Late effects and survivorship issues in patients with neuroblastoma. Children https://doi.org/10.3390/children5080107 (2018).
Geurten, C., Geurten, M., Hoyoux, C. & Lebrethon, M. C. Endocrine consequences of neuroblastoma treatment in children: 20 years’ experience of a single center. J. Pediatr. Endocrinol. Metab. 32, 347–354 (2019).
Gurney, J. G. et al. Hearing loss, quality of life, and academic problems in long-term neuroblastoma survivors: a report from the Children’s Oncology Group. Pediatrics 120, e1229–e1236 (2007).
Laverdiere, C. et al. Long-term outcomes in survivors of neuroblastoma: a report from the Childhood Cancer Survivor study. J. Natl Cancer Inst. 101, 1131–1140 (2009).
Norsker, F. N. et al. Neurologic disorders in long-term survivors of neuroblastoma–a population-based cohort study within the adult life after childhood cancer in Scandinavia (ALiCCS) research program. Acta Oncol. 59, 134–140 (2020).
Zheng, D. J. et al. Long-term psychological and educational outcomes for survivors of neuroblastoma: a report from the Childhood Cancer Survivor study. Cancer 124, 3220–3230 (2018).
Park, J. R. et al. Revisions to the International Neuroblastoma Response Criteria: a consensus statement from the National Cancer Institute clinical trials planning meeting. J. Clin. Oncol. 35, 2580–2587 (2017).
Garaventa, A. et al. Randomized trial of two induction therapy regimens for high-risk neuroblastoma: HR-NBL1.5 International Society of Pediatric Oncology European Neuroblastoma Group study. J. Clin. Oncol. 39, 2552–2563 (2021).
Pinto, N. et al. Predictors of differential response to induction therapy in high-risk neuroblastoma: a report from the Children’s Oncology Group (COG). Eur. J. Cancer 112, 66–79 (2019).
Pearson, A. D. et al. High-dose rapid and standard induction chemotherapy for patients aged over 1 year with stage 4 neuroblastoma: a randomised trial. Lancet Oncol. 9, 247–256 (2008).
Berthold, F. et al. Extended induction chemotherapy does not improve the outcome for high-risk neuroblastoma patients: results of the randomized open-label GPOH trial NB2004-HR. Ann. Oncol. 31, 422–429 (2020).
Holmes, K. et al. Influence of surgical excision on the survival of patients with stage 4 high-risk neuroblastoma: a report from the HR-NBL1/SIOPEN study. J. Clin. Oncol. 38, 2902–2915 (2020).
von Allmen, D. et al. Impact of extent of resection on local control and survival in patients from the COG A3973 study with high-risk neuroblastoma. J. Clin. Oncol. 35, 208–216 (2017).
Temple, W. C. et al. Association of image-defined risk factors with clinical features, histopathology, and outcomes in neuroblastoma. Cancer Med. 10, 2232–2241 (2021).
Brisse, H. J. et al. Radiogenomics of neuroblastomas: Relationships between imaging phenotypes, tumor genomic profile and survival. PLoS ONE 12, e0185190 (2017).
Wolden, S. L. et al. Local control with multimodality therapy for stage 4 neuroblastoma. Int. J. Radiat. Oncol. Biol. Phys. 46, 969–974 (2000).
Haas-Kogan, D. A. et al. Impact of radiotherapy for high-risk neuroblastoma: a children’s cancer group study. Int. J. Radiat. Oncol. Biol. Phys. 56, 28–39 (2003).
Liu, K. X. et al. Prospective evaluation of radiation dose escalation in patients with high-risk neuroblastoma and gross residual disease after surgery: a report from the Children’s Oncology Group ANBL0532 study. J. Clin. Oncol. 38, 2741–2752 (2020).
Berthold, F. et al. Myeloablative megatherapy with autologous stem-cell rescue versus oral maintenance chemotherapy as consolidation treatment in patients with high-risk neuroblastoma: a randomised controlled trial. Lancet Oncol. 6, 649–658 (2005).
Matthay, K. K. et al. Treatment of high-risk neuroblastoma with intensive chemotherapy, radiotherapy, autologous bone marrow transplantation, and 13-cis-retinoic acid. Children’s Cancer Group. N. Engl. J. Med. 341, 1165–1173 (1999).
Higham, C. S. et al. Transplant-associated thrombotic microangiopathy in pediatric patients: pre-HSCT risk stratification and prophylaxis. Blood Adv. 5, 2106–2114 (2021).
Jodele, S. et al. High-dose carboplatin/etoposide/melphalan increases risk of thrombotic microangiopathy and organ injury after autologous stem cell transplantation in patients with neuroblastoma. Bone Marrow Transpl. 53, 1311–1318 (2018).
Tolbert, V. P. et al. Risk factors for transplant-associated thrombotic microangiopathy after autologous hematopoietic cell transplant in high-risk neuroblastoma. Biol. Blood Marrow Transpl. 25, 2031–2039 (2019).
Elzembely, M. M. et al. Acute complications after high-dose chemotherapy and stem-cell rescue in pediatric patients with high-risk neuroblastoma treated in countries with different resources. J. Glob. Oncol. 4, 1–12 (2018).
Matthay, K. K. et al. Long-term results for children with high-risk neuroblastoma treated on a randomized trial of myeloablative therapy followed by 13-cis-retinoic acid: a Children’s Oncology Group study. J. Clin. Oncol. 27, 1007–1013 (2009).
Yu, A. L. et al. Anti-GD2 antibody with GM-CSF, interleukin-2, and isotretinoin for neuroblastoma. N. Engl. J. Med. 363, 1324–1334 (2010).
Yu, A. L. et al. Long-term follow-up of a phase III study of ch14.18 (dinutuximab) + cytokine immunotherapy in children with high-risk neuroblastoma: COG study ANBL0032. Clin. Cancer Res. 27, 2179–2189 (2021).
Ladenstein, R. et al. Interleukin 2 with anti-GD2 antibody ch14.18/CHO (dinutuximab beta) in patients with high-risk neuroblastoma (HR-NBL1/SIOPEN): a multicentre, randomised, phase 3 trial. Lancet Oncol. 19, 1617–1629 (2018).
Park, J. A. & Cheung, N. V. Targets and antibody formats for immunotherapy of neuroblastoma. J. Clin. Oncol. 38, 1836–1848 (2020).
Navid, F. et al. Phase I trial of a novel anti-GD2 monoclonal antibody, Hu14.18K322A, designed to decrease toxicity in children with refractory or recurrent neuroblastoma. J. Clin. Oncol. 32, 1445–1452 (2014).
Federico, S. M. et al. A pilot trial of humanized anti-GD2 monoclonal antibody (hu14.18K322A) with chemotherapy and natural killer cells in children with recurrent/refractory neuroblastoma. Clin. Cancer Res. 23, 6441–6449 (2017).
Matthay, K. K. et al. Global Neuroblastoma Network: an international multidisciplinary neuroblastoma tumor board for resource-limited countries. Pediatr. Blood Cancer 69, e29568 (2022).
London, W. B. et al. Historical time to disease progression and progression-free survival in patients with recurrent/refractory neuroblastoma treated in the modern era on Children’s Oncology Group early-phase trials. Cancer 123, 4914–4923 (2017).
Di Giannatale, A. et al. Phase II study of temozolomide in combination with topotecan (TOTEM) in relapsed or refractory neuroblastoma: a European Innovative Ttherapies for Children with Cancer-SIOP-European Neuroblastoma study. Eur. J. Cancer 50, 170–177 (2014).
Bagatell, R. et al. Phase II study of irinotecan and temozolomide in children with relapsed or refractory neuroblastoma: a Children’s Oncology Group study. J. Clin. Oncol. 29, 208–213 (2011).
Kushner, B. H., Kramer, K., Modak, S. & Cheung, N. K. Irinotecan plus temozolomide for relapsed or refractory neuroblastoma. J. Clin. Oncol. 24, 5271–5276 (2006).
London, W. B. et al. Phase II randomized comparison of topotecan plus cyclophosphamide versus topotecan alone in children with recurrent or refractory neuroblastoma: a Children’s Oncology Group study. J. Clin. Oncol. 28, 3808–3815 (2010).
Su, Y. et al. Increased plasma concentration of cell-free DNA precedes disease recurrence in children with high-risk neuroblastoma. BMC Cancer 20, 102 (2020).
Wang, X. et al. Plasma cell-free DNA quantification is highly correlated to tumor burden in children with neuroblastoma. Cancer Med. https://doi.org/10.1002/cam4.1586 (2018).
Mody, R. et al. Irinotecan-temozolomide with temsirolimus or dinutuximab in children with refractory or relapsed neuroblastoma (COG ANBL1221): an open-label, randomised, phase 2 trial. Lancet Oncol. 18, 946–957 (2017).
Mody, R. et al. Irinotecan, temozolomide, and dinutuximab with GM-CSF in children with refractory or relapsed neuroblastoma: a report from the Children’s Oncology Group. J. Clin. Oncol. 38, 2160–2169 (2020).
Granger, M. M. et al. Myeloablative busulfan/melphalan consolidation following induction chemotherapy for patients with newly diagnosed high-risk neuroblastoma: Children’s Oncology Group trial ANBL12P1. Transpl. Cell Ther. 27, 490.e1–490.e8 (2021).
Furman, W. L. et al. Improved outcome in children with newly diagnosed high-risk neuroblastoma treated with chemoimmunotherapy: updated results of a phase II study using hu14.18K322A. J. Clin. Oncol. 40, 335–344 (2022).
Illhardt, T. et al. Haploidentical stem cell transplantation for refractory/relapsed neuroblastoma. Biol. Blood Marrow Transpl. 24, 1005–1012 (2018).
Kantarjian, H. et al. Blinatumomab versus chemotherapy for advanced acute lymphoblastic leukemia. N. Engl. J. Med. 376, 836–847 (2017).
Straathof, K. et al. Antitumor activity without on-target off-tumor toxicity of GD2-chimeric antigen receptor T cells in patients with neuroblastoma. Sci. Transl. Med. https://doi.org/10.1126/scitranslmed.abd6169 (2020).
Godfrey, D. I., MacDonald, H. R., Kronenberg, M., Smyth, M. J. & Van Kaer, L. NKT cells: what’s in a name? Nat. Rev. Immunol. 4, 231–237 (2004).
Heczey, A. et al. Anti-GD2 CAR-NKT cells in patients with relapsed or refractory neuroblastoma: an interim analysis. Nat. Med. 26, 1686–1690 (2020).
Bosse, K. R. et al. Identification of GPC2 as an oncoprotein and candidate immunotherapeutic target in high-risk neuroblastoma. Cancer Cell 32, 295–309.e12 (2017).
Li, N. et al. CAR T cells targeting tumor-associated exons of glypican 2 regress neuroblastoma in mice. Cell Rep. Med. 2, 100297 (2021).
Kramer, K. et al. Compartmental intrathecal radioimmunotherapy: results for treatment for metastatic CNS neuroblastoma. J. Neurooncol 97, 409–418 (2010).
Moghimi, B. et al. Preclinical assessment of the efficacy and specificity of GD2-B7H3 SynNotch CAR-T in metastatic neuroblastoma. Nat. Commun. 12, 511 (2021).
Cheung, I. Y. et al. Survival impact of anti-GD2 antibody response in a phase II ganglioside vaccine trial among patients with high-risk neuroblastoma with prior disease progression. J. Clin. Oncol. 39, 215–226 (2021).
Geller, J. I. et al. ADVL1522: a phase 2 study of IMGN901 (lorvotuzumab mertansine; IND# 126953, NSC# 783609) in children with relapsed or refractory Wilms tumor, rhabdomyosarcoma, neuroblastoma, pleuropulmonary blastoma, malignant peripheral nerve sheath tumor (MPNST), and synovial sarcoma: a Children’s Oncology Group study [abstract]. J. Clin. Oncol. 35 (Suppl. 15), 10537 (2017).
Sano, R. et al. An antibody-drug conjugate directed to the ALK receptor demonstrates efficacy in preclinical models of neuroblastoma. Sci. Transl. Med. https://doi.org/10.1126/scitranslmed.aau9732 (2019).
Onda, M., Wang, Q. C., Guo, H. F., Cheung, N. K. & Pastan, I. In vitro and in vivo cytotoxic activities of recombinant immunotoxin 8H9(Fv)-PE38 against breast cancer, osteosarcoma, and neuroblastoma. Cancer Res. 64, 1419–1424 (2004).
Matthay, K. K. et al. Phase II study on the effect of disease sites, age, and prior therapy on response to iodine-131-metaiodobenzylguanidine therapy in refractory neuroblastoma. J. Clin. Oncol. 25, 1054–1060 (2007).
Zhou, M. J. et al. Different outcomes for relapsed versus refractory neuroblastoma after therapy with (131)I-metaiodobenzylguanidine ((131)I-MIBG). Eur. J. Cancer 51, 2465–2472 (2015).
Wilson, J. S., Gains, J. E., Moroz, V., Wheatley, K. & Gaze, M. N. A systematic review of 131I-meta iodobenzylguanidine molecular radiotherapy for neuroblastoma. Eur. J. Cancer 50, 801–815 (2014).
Huibregtse, K. E. et al. Incidence and risk factors for secondary malignancy in patients with neuroblastoma after treatment with (131)I-metaiodobenzylguanidine. Eur. J. Cancer 66, 144–152 (2016).
Quach, A. et al. Thyroid and hepatic function after high-dose 131 I-metaiodobenzylguanidine (131 I-MIBG) therapy for neuroblastoma. Pediatr. Blood Cancer 56, 191–201 (2011).
Matthay, K. K. et al. Dose escalation study of no-carrier-added 131I-metaiodobenzylguanidine for relapsed or refractory neuroblastoma: new approaches to neuroblastoma therapy consortium trial. J. Nucl. Med. 53, 1155–1163 (2012).
Weiss, B. D. et al. A safety and feasibility trial of (131)I-MIBG in newly diagnosed high-risk neuroblastoma: a Children’s Oncology Group study. Pediatr. Blood Cancer 68, e29117 (2021).
More, S. S. et al. Vorinostat increases expression of functional norepinephrine transporter in neuroblastoma in vitro and in vivo model systems. Clin. Cancer Res. 17, 2339–2349 (2011).
Simon, R. M. et al. Clinical trial designs for the early clinical development of therapeutic cancer vaccines. J. Clin. Oncol. 19, 1848–1854 (2001).
DuBois, S. G. et al. Randomized phase II trial of MIBG versus MIBG, vincristine, and irinotecan versus MIBG and vorinostat for patients with relapsed or refractory neuroblastoma: a report from NANT consortium. J. Clin. Oncol. https://doi.org/10.1200/JCO.21.00703 (2021).
Kroesen, M. et al. Anti-GD2 mAb and vorinostat synergize in the treatment of neuroblastoma. Oncoimmunology 5, e1164919 (2016).
Qiu, B., Kline, C. & Mueller, S. Radiation in combination with targeted agents and immunotherapies for pediatric central nervous system tumors–progress, opportunities, and challenges. Front. Oncol. 11, 674596 (2021).
Voeller, J. et al. Combined innate and adaptive immunotherapy overcomes resistance of immunologically cold syngeneic murine neuroblastoma to checkpoint inhibition. J. Immunother. Cancer 7, 344 (2019).
Strosberg, J. et al. Phase 3 trial of (177)Lu-Dotatate for midgut neuroendocrine tumors. N. Engl. J. Med. 376, 125–135 (2017).
Gains, J. E. et al. 177Lu-DOTATATE molecular radiotherapy for childhood neuroblastoma. J. Nucl. Med. 52, 1041–1047 (2011).
Gains, J. E. et al. A phase IIa trial of molecular radiotherapy with 177-lutetium DOTATATE in children with primary refractory or relapsed high-risk neuroblastoma. Eur. J. Nucl. Med. Mol. Imaging 47, 2348–2357 (2020).
Foster, J. H. et al. Activity of crizotinib in patients with ALK-aberrant relapsed/refractory neuroblastoma: a Children’s Oncology Group study (ADVL0912). Clin. Cancer Res. 27, 3543–3548 (2021).
Bresler, S. C. et al. Differential inhibitor sensitivity of anaplastic lymphoma kinase variants found in neuroblastoma. Sci. Transl. Med. 3, 108ra114 (2011).
Infarinato, N. R. et al. The ALK/ROS1 inhibitor PF-06463922 overcomes primary resistance to crizotinib in ALK-driven neuroblastoma. Cancer Discov. 6, 96–107 (2016).
Schulte, J. H. et al. Final analysis of phase I study of ceritinib in pediatric patients with malignancies harboring activated anaplastic lymphoma kinase (ALK) [abstract]. J. Clin. Oncol. 38 (Suppl. 15), 10505 (2020).
Eleveld, T. F. et al. RAS-MAPK pathway-driven tumor progression is associated with loss of CIC and other genomic aberrations in neuroblastoma. Cancer Res. 78, 6297–6307 (2018).
Brockmann, M. et al. Small molecule inhibitors of Aurora-A induce proteasomal degradation of N-myc in childhood neuroblastoma. Cancer Cell 24, 75–89 (2013).
Gustafson, W. C. et al. Drugging MYCN through an allosteric transition in Aurora kinase A. Cancer Cell 26, 414–427 (2014).
DuBois, S. G. et al. Phase II trial of alisertib in combination with irinotecan and temozolomide for patients with relapsed or refractory neuroblastoma. Clin. Cancer Res. 24, 6142–6149 (2018).
Du, J. et al. Aurora A-selective inhibitor LY3295668 leads to dominant mitotic arrest, apoptosis in cancer cells, and shows potent preclinical antitumor efficacy. Mol. Cancer Ther. 18, 2207–2219 (2019).
Buchel, G. et al. Association with Aurora-A controls N-MYC-dependent promoter escape and pause release of RNA polymerase II during the cell cycle. Cell Rep. 21, 3483–3497 (2017).
Adhikari, B. et al. PROTAC-mediated degradation reveals a non-catalytic function of AURORA-A kinase. Nat. Chem. Biol. 16, 1179–1188 (2020).
Wolpaw, A. J. et al. Drugging the “undruggable” MYCN oncogenic transcription factor: overcoming previous obstacles to impact childhood cancers. Cancer Res. 81, 1627–1632 (2021).
Puissant, A. et al. Targeting MYCN in neuroblastoma by BET bromodomain inhibition. Cancer Discov. 3, 308–323 (2013).
Hogarty, M. D. et al. ODC1 is a critical determinant of MYCN oncogenesis and a therapeutic target in neuroblastoma. Cancer Res. 68, 9735–9745 (2008).
Sholler, G. L. S. et al. Maintenance DFMO increases survival in high risk neuroblastoma. Sci. Rep. 8, 14445 (2018).
Cole, K. A. et al. Phase I clinical trial of the Wee1 inhibitor adavosertib (AZD1775) with irinotecan in children with relapsed solid tumors: a COG Phase I Consortium report (ADVL1312). Clin. Cancer Res. 26, 1213–1219 (2020).
Chen, L. et al. CRISPR-Cas9 screen reveals a MYCN-amplified neuroblastoma dependency on EZH2. J. Clin. Invest. 128, 446–462 (2018).
Durbin, A. D. et al. EP300 selectively controls the enhancer landscape of MYCN-amplified neuroblastoma. Cancer Discov. https://doi.org/10.1158/2159-8290.Cd-21-0385 (2021).
Chen, J. et al. Targeted therapy of TERT-rearranged neuroblastoma with BET bromodomain inhibitor and proteasome inhibitor combination therapy. Clin. Cancer Res. 27, 1438–1451 (2021).
Koneru, B. et al. ALT neuroblastoma chemoresistance due to telomere dysfunction-induced ATM activation is reversible with ATM inhibitor AZD0156. Sci. Transl. Med. 13, eabd (2021).
Geoerger, B. et al. A phase I study of the CDK4/6 inhibitor ribociclib (LEE011) in pediatric patients with malignant rhabdoid tumors, neuroblastoma, and other solid tumors. Clin. Cancer Res. 23, 2433–2441 (2017).
Barbieri, E. et al. MDM2 inhibition sensitizes neuroblastoma to chemotherapy-induced apoptotic cell death. Mol. Cancer Ther. 5, 2358–2365 (2006).
Wang, H. Q. et al. Combined ALK and MDM2 inhibition increases antitumor activity and overcomes resistance in human ALK mutant neuroblastoma cell lines and xenograft models. Elife https://doi.org/10.7554/eLife.17137 (2017).
Chen, L. et al. Preclinical evaluation of the first intravenous small molecule MDM2 antagonist alone and in combination with temozolomide in neuroblastoma. Int. J. Cancer 144, 3146–3159 (2019).
Van Goethem, A. et al. Dual targeting of MDM2 and BCL2 as a therapeutic strategy in neuroblastoma. Oncotarget 8, 57047–57057 (2017).
Kohler, J. A. et al. Treatment of children over the age of one year with unresectable localised neuroblastoma without MYCN amplification: results of the SIOPEN study. Eur. J. Cancer 49, 3671–3679 (2013).
Howell, C. R. et al. Cohort profile: the St. Jude Lifetime Cohort study (SJLIFE) for paediatric cancer survivors. Int. J. Epidemiol. 50, 39–49 (2021).
Author information
Authors and Affiliations
Contributions
Both authors made a substantial contribution to all aspects of the preparation of this manuscript.
Corresponding authors
Ethics declarations
Competing interests
K.K.M. is a consultant for Illumina Radiopharmaceuticals. B.Q. declares no competing interests.
Peer review
Peer review information
Nature Reviews Clinical Oncology thanks B. Decarolis, M. Fischer, M. Hogarty, A. Nakagawara and the other, anonymous reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Qiu, B., Matthay, K.K. Advancing therapy for neuroblastoma. Nat Rev Clin Oncol 19, 515–533 (2022). https://doi.org/10.1038/s41571-022-00643-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41571-022-00643-z
This article is cited by
-
Visual conservation treatment dilemmas in neuroblastoma with bilateral blindness
Discover Oncology (2024)
-
Identifying Protein Phosphorylation Site-Disease Associations Based on Multi-Similarity Fusion and Negative Sample Selection by Convolutional Neural Network
Interdisciplinary Sciences: Computational Life Sciences (2024)
-
Comprehensive exploration of the involvement of cuproptosis in tumorigenesis and progression of neuroblastoma
BMC Genomics (2023)
-
Prevention of STAT3-related pathway in SK-N-SH cells by natural product astaxanthin
BMC Complementary Medicine and Therapies (2023)
-
LncRNA AC142119.1 facilitates the progression of neuroblastoma by epigenetically initiating the transcription of MYCN
Journal of Translational Medicine (2023)