Abstract
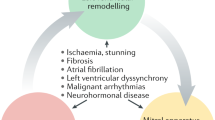
Cardiomyopathies and valvular heart diseases are typically considered distinct diagnostic categories with dedicated guidelines for their management. However, the interplay between these conditions is increasingly being recognized and they frequently coexist, as in the paradigmatic examples of dilated cardiomyopathy and hypertrophic cardiomyopathy, which are often complicated by the occurrence of mitral regurgitation. Moreover, cardiomyopathies and valvular heart diseases can have a shared aetiology because several genetic or acquired diseases can affect both the cardiac valves and the myocardium. In addition, the association between cardiomyopathies and valvular heart diseases has important prognostic and therapeutic implications. Therefore, a better understanding of their shared pathophysiological mechanisms, as well as of the prevalence and predisposing factors to their association, might lead to a different approach in the risk stratification and management of these diseases. In this Review, we discuss the different scenarios in which valvular heart diseases and cardiomyopathies coexist, highlighting the need for an improved classification and clustering of these diseases with potential repercussions in the clinical management and, particularly, personalized therapeutic approaches.
Key points
-
Cardiomyopathies and valvular heart diseases are traditionally considered to be distinct diagnostic categories, but their coexistence is increasingly being recognized in several clinical settings.
-
Dilated cardiomyopathy and hypertrophic cardiomyopathy are the paradigmatic examples of the coexistence of valvular heart disease and cardiomyopathy, given that these cardiomyopathies are often associated with mitral regurgitation, which further complicates their management.
-
Cardiomyopathies and valvular heart disease can also share specific pathophysiological mechanisms, given that various genetic or acquired diseases can affect both the valves and the myocardium, including storage or immune-mediated disorders and radiation-induced cardiac damage.
-
The association between cardiomyopathies and valvular heart diseases can have prognostic implications and can affect clinical decision-making; therefore, a personalized medicine approach is advocated for patients in whom these conditions coexist.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Vahanian, A. et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur. Heart J. 43, 561–632 (2022).
Elliott, P. et al. Classification of the cardiomyopathies: a position statement from the European Society of Cardiology working group on myocardial and pericardial diseases. Eur. Heart J. 29, 270–276 (2008).
McKenna, W. J., Maron, B. J. & Thiene, G. Classification, epidemiology, and global burden of cardiomyopathies. Circ. Res. 121, 722–730 (2017).
Lancellotti, P., Zamorano, J. L. & Vannan, M. A. Imaging challenges in secondary mitral regurgitation: unsolved issues and perspectives. Circ. Cardiovasc. Imaging 7, 735–746 (2014).
Wigle, E. D. Cardiomyopathy: the diagnosis of hypertrophic cardiomyopathy. Heart 86, 709–714 (2001).
Milleron, O. et al. Eclipsed mitral regurgitation: an unusual cause of acute heart failure. Eur. Heart J. Cardiovasc. Imaging 18, 1163–1169 (2017).
Agricola, E. et al. Non-ischemic dilated cardiopathy: prognostic value of functional mitral regurgitation. Int. J. Cardiol. 146, 426–428 (2010).
He, S., Fontaine, A. A., Schwammenthal, E., Yoganathan, A. P. & Levine, R. A. Integrated mechanism for functional mitral regurgitation: leaflet restriction versus coapting force: in vitro studies. Circulation 96, 1826–1834 (1997).
Levack, M. M. et al. Three-dimensional echocardiographic analysis of mitral annular dynamics: implication for annuloplasty selection. Circulation 126, S183–S188 (2012).
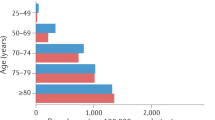
Rossi, A. et al. Independent prognostic value of functional mitral regurgitation in patients with heart failure. A quantitative analysis of 1256 patients with ischaemic and non-ischaemic dilated cardiomyopathy. Heart 97, 1675–1680 (2011).
Mack, M. & Grayburn, P. Guideline-directed medical therapy for secondary mitral regurgitation: more questions than answers! JACC Heart Fail. 5, 660–662 (2017).
El Sabbagh, A., Reddy, Y. N. V. & Nishimura, R. A. Mitral valve regurgitation in the contemporary era: insights into diagnosis, management, and future directions. JACC Cardiovasc. Imaging 11, 628–643 (2018).
Kajimoto, K., Minami, Y., Otsubo, S. & Sato, N. Ischemic or nonischemic functional mitral regurgitation and outcomes in patients with acute decompensated heart failure with preserved or reduced ejection fraction. Am. J. Cardiol. 120, 809–816 (2017).
Trichon, B. H., Felker, G. M., Shaw, L. K., Cabell, C. H. & O’Connor, C. M. Relation of frequency and severity of mitral regurgitation to survival among patients with left ventricular systolic dysfunction and heart failure. Am. J. Cardiol. 91, 538–543 (2003).
Goliasch, G. et al. Refining the prognostic impact of functional mitral regurgitation in chronic heart failure. Eur. Heart J. 39, 39–46 (2018).
Seneviratne, B., Moore, G. A. & West, P. D. Effect of captopril on functional mitral regurgitation in dilated heart failure: a randomised double blind placebo controlled trial. Br. Heart J. 72, 63–68 (1994).
Nasser, R. et al. Evolution of functional mitral regurgitation and prognosis in medically managed heart failure patients with reduced ejection fraction. JACC Heart Fail. 5, 652–659 (2017).
Pagnesi, M. et al. Clinical impact of changes in mitral regurgitation severity after medical therapy optimization in heart failure. Clin. Res. Cardiol. 111, 912–923 (2022).
Kang, D. H. et al. Angiotensin receptor neprilysin inhibitor for functional mitral regurgitation. Circulation 139, 1354–1365 (2019).
Cabrera-Bueno, F. et al. Persistence of secondary mitral regurgitation and response to cardiac resynchronization therapy. Eur. J. Echocardiogr. 11, 131–137 (2010).
Verhaert, D. et al. Impact of mitral regurgitation on reverse remodeling and outcome in patients undergoing cardiac resynchronization therapy. Circ. Cardiovasc. Imaging 5, 21–26 (2012).
Van Bommel, R. J. et al. Cardiac resynchronization therapy as a therapeutic option in patients with moderate–severe functional mitral regurgitation and high operative risk. Circulation 124, 912–919 (2011).
Spartera, M. et al. Role of cardiac dyssynchrony and resynchronization therapy in functional mitral regurgitation. Eur. Heart J. Cardiovasc. Imaging 17, 471–480 (2016).
Acker, M. A. et al. Mitral-valve repair versus replacement for severe ischemic mitral regurgitation. N. Engl. J. Med. 370, 23–32 (2014).
Smith, P. K. et al. Cardiothoracic Surgical Trials Network Investigators. Surgical treatment of moderate ischemic mitral regurgitation. N. Engl. J. Med. 371, 2178–2188 (2014).
Obadia, J. F. et al. Percutaneous repair or medical treatment for secondary mitral regurgitation. N. Engl. J. Med. 379, 2297–2306 (2018).
Stone, G. W. et al. Transcatheter mitral-valve repair in patients with heart failure. N. Engl. J. Med. 379, 2307–2318 (2018).
Chiarito, M. et al. Edge-to-edge percutaneous mitral repair for functional ischaemic and non-ischaemic mitral regurgitation: a systematic review and meta-analysis. Esc. Heart Fail. 9, 3177–3187 (2022).
Grayburn, P. A., Sannino, A. & Packer, M. Proportionate and disproportionate functional mitral regurgitation: a new conceptual framework that reconciles the results of the MITRA-FR and COAPT trials. JACC Cardiovasc. Imaging 12, 353–362 (2019).
Lindenfeld, J. et al. Association of effective regurgitation orifice area to left ventricular end-diastolic volume ratio with transcatheter mitral valve repair outcomes: a secondary analysis of the COAPT trial. JAMA Cardiol. 6, 427–443 (2021).
Ooms, J. F. et al. Transcatheter edge-to-edge repair in proportionate versus disproportionate functional mitral regurgitation. J. Am. Soc. Echocardiogr. 35, 105–115e8 (2022).
Orban, M. et al. Impact of proportionality of secondary mitral regurgitation on outcome after transcatheter mitral valve repair. JACC Cardiovasc. Imaging 14, 715–725 (2021).
Adamo, M. et al. COAPT-like profile predicts long-term outcomes in patients with secondary mitral regurgitation undergoing mitraclip implantation. JACC Cardiovasc. Interv. 14, 15–25 (2021).
Brener, M. I. et al. Right ventricular–pulmonary arterial coupling in patients with HF secondary MR: analysis from the COAPT trial. JACC Cardiovasc. Interv. 14, 2231–2242 (2021).
Otto, C. M. et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 143, e72–e227 (2021).
Rose, E. A. et al. Long-term use of a left ventricular assist device for end-stage heart failure. N. Engl. J. Med. 345, 1435–1443 (2001).
Maron, B. J. et al. Diagnosis and evaluation of hypertrophic cardiomyopathy: JACC state-of-the-art review. J. Am. Coll. Cardiol. 79, 372–389 (2022).
Ommen, S. R. et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: executive summary: a report of The American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 76, 3022–3055 (2020).
Woo, A. & Jedrzkiewicz, S. The mitral valve in hypertrophic cardiomyopathy: it’s a long story. Circulation 124, 9–12 (2011).
Maron, M. S. et al. Mitral valve abnormalities identified by cardiovascular magnetic resonance represent a primary phenotypic expression of hypertrophic cardiomyopathy. Circulation 124, 40–47 (2011).
Levine, R. A. et al. Papillary muscle displacement causes systolic anterior motion of the mitral valve. Experimental validation and insights into the mechanism of subaortic obstruction. Circulation 91, 1189–1195 (1995).
Klues, H. G., Roberts, W. C. & Maron, B. J. Anomalous insertion of papillary muscle directly into anterior mitral leaflet in hypertrophic cardiomyopathy. Significance in producing left ventricular outflow obstruction. Circulation 84, 1188–1197 (1991).
Groarke, J. D. et al. Intrinsic mitral valve alterations in hypertrophic cardiomyopathy sarcomere mutation carriers. Eur. Heart J. Cardiovasc. Imaging 19, 1109–1116 (2018).
Ferrazzi, P. et al. Congenital muscular mitral-aortic discontinuity identified in patients with obstructive hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 76, 2238–2247 (2020).
Olivotto, I., Cecchi, F., Poggesi, C. & Yacoub, M. H. Developmental origins of hypertrophic cardiomyopathy phenotypes: a unifying hypothesis. Nat. Rev. Cardiol. 6, 317–321 (2009).
Djenoune, L., Berg, K., Brueckner, M. & Yuan, S. A change of heart: new roles for cilia in cardiac development and disease. Nat. Rev. Cardiol. 19, 211–227 (2022).
Wigle, E. D., Adelman, A., Auger, P. & Marquis, Y. Mitral regurgitation in muscular subaortic stenosis. Am. J. Cardiol. 24, 698–706 (1969).
Rowin, E. J., Maron, B. J., Olivotto, I. & Maron, M. S. Role of exercise testing in hypertrophic cardiomyopathy. JACC Cardiovasc. Imaging 10, 1374–1386 (2017).
Maron, M. S. et al. Effect of left ventricular outflow tract obstruction on clinical outcome in hypertrophic cardiomyopathy. N. Engl. J. Med. 348, 295–303 (2003).
Maron, B. J., Rowin, E. J., Udelson, J. E. & Maron, M. S. Clinical spectrum and management of heart failure in hypertrophic cardiomyopathy. JACC Heart Fail. 6, 353–363 (2018).
Elliott, P. M. et al. 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy: the task force for the diagnosis and management of hypertrophic cardiomyopathy of the European Society of Cardiology (ESC). Eur. Heart J. 35, 2733–2779 (2014).
Maron, B. J. et al. Left atrial remodeling in hypertrophic cardiomyopathy and susceptibility markers for atrial fibrillation identified by cardiovascular magnetic resonance. Am. J. Cardiol. 113, 1394–1400 (2014).
Feneon, D. et al. Impact of exercise-induced mitral regurgitation on hypertrophic cardiomyopathy outcomes. Eur. Heart J. Cardiovasc. Imaging 17, 1110–1117 (2016).
Olivotto, I., Cecchi, F., Poggesi, C. & Yacoub, M. H. Patterns of disease progression in hypertrophic cardiomyopathy: an individualized approach to clinical staging. Circ. Heart Fail. 5, 535–546 (2012).
Hong, J. H. et al. Mitral regurgitation in patients with hypertrophic obstructive cardiomyopathy: implications for concomitant valve procedures. J. Am. Coll. Cardiol. 68, 1497–1504 (2016).
Iacovoni, A. et al. A contemporary European experience with surgical septal myectomy in hypertrophic cardiomyopathy. Eur. Heart J. 33, 2080–2087 (2012).
Pelliccia, F. et al. Multidisciplinary evaluation and management of obstructive hypertrophic cardiomyopathy in 2020: towards the HCM Heart Team. Int. J. Cardiol. 304, 86–92 (2020).
Maron, B. J. et al. The case for surgery in obstructive hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 44, 2044–2053 (2004).
Ferrazzi, P. et al. Transaortic chordal cutting: mitral valve repair for obstructive hypertrophic cardiomyopathy with mild septal hypertrophy. J. Am. Coll. Cardiol. 66, 1687–1696 (2015).
Morcos, M., Strobel, A., Messenger, J. & Gill, E. Treatment of severe left ventricular outflow tract obstruction and mitral regurgitation with alcohol septal ablation. CASE 6, 387–391 (2022).
Nielsen, C. D., Fernandes, V. & Spencer, W. H. III Alcohol septal ablation for obstructive hypertrophic cardiomyopathy. Am. Heart Hosp. J. 1, 83–90 (2003).
Krajcer, Z., Leachman, R. D., Cooley, D. A. & Coronado, R. Septal myotomy-myomectomy versus mitral valve replacement in hypertrophic cardiomyopathy. Ten-year follow-up in 185 patients. Circulation 80, I57–I64 (1989).
Sherrid, M. V., Balaram, S., Kim, B., Axel, L. & Swistel, D. G. The mitral valve in obstructive hypertrophic cardiomyopathy: a test in context. J. Am. Coll. Cardiol. 67, 1846–1858 (2016).
Afanasyev, A. V. et al. Edge-to-Edge repair versus secondary cord cutting during septal myectomy in patients with hypertrophic obstructive cardiomyopathy: a pilot randomised study. Heart Lung Circ. 30, 438–445 (2021).
Thomas, F., Rader, F. & Siegel, R. J. The use of mitraclip for symptomatic patients with hypertrophic obstructive cardiomyopathy. Cardiology 137, 58–61 (2017).
van der Lee, C., Kofflard, M. J. & van Herwerden, L. A. Sustained improvement after combined anterior mitral leaflet extension and myectomy in hypertrophic obstructive cardiomyopathy. Circulation 108, 2088–2092 (2003).
Rankin, J. S. et al. A new mitral valve repair strategy for hypertrophic obstructive cardiomyopathy. J. Heart Valve Dis. 17, 642–647 (2008).
Delmo Walter, E. M., Siniawski, H. & Hetzer, R. Sustained improvement after combined anterior mitral valve leaflet retention plasty and septal myectomy in preventing systolic anterior motion in hypertrophic obstructive cardiomyopathy in children. Eur. J. Cardiothorac. Surg. 36, 546–552 (2009).
Nasseri, B. A. et al. Combined anterior mitral valve leaflet retention plasty and septal myectomy in patients with hypertrophic obstructive cardiomyopathy. Eur. J. Cardiothorac. Surg. 40, 1515–1520 (2011).
Nistri, S. et al. β-Blockers for prevention of exercise-induced left ventricular outflow tract obstruction in patients with hypertrophic cardiomyopathy. Am. J. Cardiol. 110, 715–719 (2012).
Cohen, L. S. & Braunwald, E. Amelioration of angina pectoris in idiopathic hypertrophic subaortic stenosis with beta-adrenergic blockade. Circulation 35, 847–851 (1967).
Dybro, A. M. et al. Randomized trial of metoprolol in patients with obstructive hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 78, 2505–2517 (2021).
Maron, B. J. Clinical course and management of hypertrophic cardiomyopathy. N. Engl. J. Med. 379, 655–668 (2018).
Olivotto, I. et al. EXPLORER-HCM_Study Investigators. Mavacamten for treatment of symptomatic obstructive hypertrophic cardiomyopathy (EXPLORER-HCM): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 396, 759–769 (2020).
Maron, M. S. & Ommen, S. R. Exploring new and old therapies for obstructive hypertrophic cardiomyopathy: mavacamten in perspective. Circulation 143, 1181–1183 (2021).
Schönbeck, M. H. et al. Long-term follow-up in hypertrophic obstructive cardiomyopathy after septal myectomy. Ann. Thorac. Surg. 65, 1207–1214 (1998).
Sun, D. et al. Posterior wall thickness associates with survival following septal myectomy for obstructive hypertrophic cardiomyopathy. JACC Heart Fail. 10, 831–837 (2022).
Woo, A. et al. Clinical and echocardiographic determinants of long-term survival after surgical myectomy in obstructive hypertrophic cardiomyopathy. Circulation 111, 2033–2041 (2005).
Gigli, M. et al. Genetic risk of arrhythmic phenotypes in patients with dilated cardiomyopathy. J. Am. Coll. Cardiol. 74, 1480–1490 (2019).
De Frutos, F. et al. Natural history of MYH7-related dilated cardiomyopathy. J. Am. Coll. Cardiol. 80, 1447–1461 (2022).
Paldino, A. et al. Prognostic prediction of genotype vs phenotype in genetic cardiomyopathies. J. Am. Coll. Cardiol. 80, 1981–1994 (2022).
Ho, C. Y. et al. Genotype and lifetime burden of disease in hypertrophic cardiomyopathy: insights from the Sarcomeric Human Cardiomyopathy Registry (SHaRe). Circulation 138, 1387–1398 (2018).
Arends, M. et al. Characterization of classical and nonclassical fabry disease: a multicenter study. J. Am. Soc. Nephrol. 28, 1631–1641 (2017).
LaHaye, S., Lincoln, J. & Garg, V. Genetics of valvular heart disease. Curr. Cardiol. Rep. 16, 487 (2014).
Durst, R. et al. Mutations in DCHS1 cause mitral valve prolapse. Nature 525, 109–113 (2015).
Ta-Shma, A. et al. Congenital valvular defects associated with deleterious mutations in the PLD1 gene. J. Med. Genet. 54, 278–286 (2017).
Wünnemann, F. et al. Loss of ADAMTS19 causes progressive non-syndromic heart valve disease. Nat. Genet. 52, 40–47 (2020).
Hiemstra, Y. L. et al. Familial occurrence of mitral regurgitation in patients with mitral valve prolapse undergoing mitral valve surgery. Eur. J. Prev. Cardiol. 27, 272–280 (2020).
Lillo, R. et al. Echocardiography in Anderson–Fabry disease. Rev. Cardiovasc. Med. 23, 201 (2022).
Prasad, M. et al. Cardiorheumatology: cardiac involvement in systemic rheumatic disease. Nat. Rev. Cardiol. 12, 168–176 (2015).
Shammas, R. L. & Movahed, A. Sarcoidosis of the heart. Clin. Cardiol. 16, 462–472 (1993).
Remenyi, B. et al. Valvular aspects of rheumatic heart disease. Lancet 387, 1335–1346 (2016).
Desai, M. Y., Jellis, C. L., Kotecha, R., Johnston, D. R. & Griffin, B. P. Radiation-associated cardiac disease: a practical approach to diagnosis and management. JACC Cardiovasc. Imaging 11, 1132–1149 (2018).
Freed, L. A. et al. Mitral valve prolapse in the general population: the benign nature of echocardiographic features in the Framingham Heart Study. J. Am. Coll. Cardiol. 40, 1298–1304 (2002).
Van Wijngaarden, A. L., Kruithof, B. P. T., Vinella, T., Barge-Schaapveld, D. Q. C. M. & Ajmone Marsan, N. Characterization of degenerative mitral valve disease: differences between fibroelastic deficiency and Barlow’s disease. J. Cardiovasc. Dev. Dis. 8, 23 (2021).
Nascimento, R. et al. Is mitral valve prolapse a congenital or acquired disease? Am. J. Cardiol. 79, 226–227 (1997).
Kruithof, B. P. T. et al. Stress-induced remodelling of the mitral valve: a model for leaflet thickening and superimposed tissue formation in mitral valve disease. Cardiovasc. Res. 5, 931–943 (2020).
Van Wijngaarden, A. L. et al. Identification of known and unknown genes associated with mitral valve prolapse using an exome slice methodology. J. Med. Genet. 57, 843–850 (2020).
Delwarde, C. et al. Genetics and pathophysiology of mitral valve prolapse. Front. Cardiovasc. Med. 10, 1077788 (2023).
Gulotta, S. J., Gulco, L., Padmanabhan, V. & Miller, S. The syndrome of systolic click, murmur, and mitral valve prolapse — a cardiomyopathy? Circulation 49, 717–728 (1974).
Yang, L. T. et al. Mitral valve prolapse patients with less than moderate mitral regurgitation exhibit early cardiac chamber remodeling. J. Am. Soc. Echocardiogr. 33, 815–825 (2020).
Romero Daza, A. et al. Mitral valve prolapse morphofunctional features by cardiovascular magnetic resonance: more than just a valvular disease. J. Cardiovasc. Magn. Reson. 23, 107 (2021).
Kitkungvan, D. et al. Myocardial fibrosis in patients with primary mitral regurgitation with and without prolapse. J. Cardiovasc. Magn. Reson. 72, 823–834 (2018).
Han, Y. et al. Cardiovascular magnetic resonance characterization of mitral valve prolapse. JACC Cardiovasc. Imaging 1, 294–303 (2008).
Bui, A. H. et al. Diffuse myocardial fibrosis in patients with mitral valve prolapse and ventricular arrhythmia. Heart 103, 204–209 (2017).
Constant Dit Beaufils, A. L. et al. Replacement myocardial fibrosis in patients with mitral valve prolapse: relation to mitral regurgitation, ventricular remodeling, and arrhythmia. Circulation 143, 1763–1774 (2021).
Sabbag, A. et al. EHRA expert consensus statement on arrhythmic mitral valve prolapse and mitral annular disjunction complex in collaboration with the ESC Council on Valvular Heart Disease and the European Association of Cardiovascular Imaging endorsed by the Heart Rhythm Society, by the Asia Pacific Heart Rhythm Society, and by the Latin American Heart Rhythm Society. Europace 24, 1981–2003 (2022).
Perazzolo Marra, M. et al. Morphofunctional abnormalities of mitral annulus and arrhythmic mitral valve prolapse. Circ. Cardiovasc. Imaging 9, e005030 (2016).
Basso, C. et al. Arrhythmic mitral valve prolapse and sudden cardiac death. Circulation 132, 556–566 (2015).
Van Wijngaarden, A. L. et al. Parameters associated with ventricular arrhythmias in mitral valve prolapse with significant regurgitation. Heart 107, 411–418 (2021).
Dejgaard, L. A. et al. The mitral annulus disjunction arrhythmic syndrome. J. Am. Coll. Cardiol. 72, 1600–1609 (2018).
Toh, H. et al. Prevalence and extent of mitral annular disjunction in structurally normal hearts: comprehensive 3D analysis using cardiac computed tomography. Eur. Heart J. Cardiovasc. Imaging 22, 614–622 (2021).
Faletra, F. F. et al. Morphology of mitral annular disjunction in mitral valve prolapse. J. Am. Soc. Echocardiogr. 35, 176–186 (2022).
Basso, C. et al. An echocardiographic survey of primary school children for bicuspid aortic valve. Am. J. Cardiol. 93, 661–663 (2004).
Siu, S. C. & Silversides, C. K. Bicuspid aortic valve disease. J. Am. Coll. Cardiol. 55, 2789–2800 (2010).
Roberts, W. C. & Ko, J. M. Frequency by decades of unicuspid, bicuspid, and tricuspid aortic valves in adults having isolated aortic valve replacement for aortic stenosis, with or without associated aortic regurgitation. Circulation 111, 920–925 (2005).
Padang, R., Bagnall, R. D. & Semsarian, C. Genetic basis of familial valvular heart disease. Circ. Cardiovasc. Genet. 5, 569–580 (2012).
Glick, B. N. & Roberts, W. C. Congenitally bicuspid aortic valve in multiple family members. Am. J. Cardiol. 73, 400–404 (1994).
Martin, L. J. et al. Evidence in favor of linkage to human chromosomal regions 18q, 5q and 13q for bicuspid aortic valve and associated cardiovascular malformations. Hum. Genet. 121, 275–284 (2007).
Fedak, P. W. et al. Clinical and pathophysiological implications of a bicuspid aortic valve. Circulation 106, 900–904 (2002).
Yassine, N. M., Shahram, J. T. & Body, S. C. Pathogenic mechanisms of bicuspid aortic valve aortopathy. Front. Physiol. 8, 687 (2017).
Owens, G. K., Kumar, M. S. & Wamhoff, B. R. Molecular regulation of vascular smooth muscle cell differentiation in development and disease. Physiol. Rev. 84, 767–801 (2004).
Feizi, O., Farrer Brown, G. & Emanuel, R. Familial study of hypertrophic cardiomyopathy and congenital aortic valve disease. Am. J. Cardiol. 41, 956–964 (1978).
Brown, P. S. Jr, Roberts, C. S., McIntosh, C. L., Roberts, W. C. & Clark, R. E. Combined obstructive hypertrophic cardiomyopathy and stenotic congenitally bicuspid aortic valve. Am. J. Cardiol. 66, 1273–1275 (1990).
Agarwal, A. et al. Left ventricular noncompaction in patients with bicuspid aortic valve. J. Am. Soc. Echocardiogr. 26, 1306–1313 (2013).
Jeong, H. et al. Prevalence, characteristics, and clinical significance of concomitant cardiomyopathies in subjects with bicuspid aortic valves. Yonsei Med. J. 60, 816–823 (2019).
Galat, A. et al. Aortic stenosis and transthyretin cardiac amyloidosis: the chicken or the egg? Eur. Heart J. 37, 3525–3531 (2016).
Tanskanen, M. et al. Senile systemic amyloidosis affects 25% of the very aged and associates with genetic variation in alpha2-macroglobulin and tau: a population based autopsy study. Ann. Med. 40, 232–239 (2008).
Osnabrugge, R. L. et al. Aortic stenosis in the elderly: disease prevalence and number of candidates for transcatheter aortic valve replacement: a meta-analysis and modeling study. J. Am. Coll. Cardiol. 62, 1002–1012 (2013).
Cooper, J. H. Localized dystrophic amyloidosis of heart valves. Hum. Pathol. 14, 649–653 (1983).
Conte, M. et al. Isolated valve amyloidosis in aortic stenosis: a new clinical scenario? J. Am. Coll. Cardiol. 79, 3476 (2022).
Kristen, A. V. et al. High prevalence of amyloid in 150 surgically removed heart valves — a comparison of histological and clinical data reveals a correlation to atheroinflammatory conditions. Cardiovasc. Pathol. 19, 228–235 (2010).
Fujimoto, T. et al. Case with transthyretin amyloid cardiomyopathy complicated with rapidly progressive aortic stenosis possibly caused by amyloid deposition in the aortic valve. Circ. Cardiovasc. Imaging 14, e013357 (2021).
Singal, A. K. et al. Concomitant transthyretin amyloidosis and severe aortic stenosis in elderly Indian population: a pilot study. JACC CardioOncol 3, 565–576 (2021).
Merlini, G. & Bellotti, V. Molecular mechanisms of amyloidosis. N. Engl. J. Med. 349, 583–596 (2003).
Henderson, B. C. et al. Oxidative remodeling in pressure overload induced chronic heart failure. Eur. J. Heart Fail. 9, 450–457 (2007).
Park, J. Y. et al. Association of inflammation, myocardial fibrosis and cardiac remodelling in patients with mild aortic stenosis as assessed by biomarkers and echocardiography. Clin. Exp. Pharmacol. Physiol. 41, 185–191 (2014).
Rosenblum, H. et al. Unveiling outcomes in coexisting severe aortic stenosis and transthyretin cardiac amyloidosis. Eur. J. Heart Fail. 23, 250–258 (2021).
Chacko, L. et al. Echocardiographic phenotype and prognosis in transthyretin cardiac amyloidosis. Eur. Heart J. 41, 1439–1447 (2020).
Ricci, F. et al. Prognostic significance of cardiac amyloidosis in patients with aortic stenosis: a systematic review and meta-analysis. JACC Cardiovasc. Imaging 14, 293–295 (2021).
Myasoedova, V. A. et al. Red flags, prognostic impact, and management of patients with cardiac amyloidosis and aortic valve stenosis: a systematic review and meta-analysis. Front. Med. 9, 858281 (2022).
Ternacle, J. et al. Aortic stenosis and cardiac amyloidosis: JACC review topic of the week. J. Am. Coll. Cardiol. 74, 2638–2651 (2019).
Dahl Pedersen, A. L. et al. Prevalence and prognostic implications of increased apical-to-basal strain ratio in patients with aortic stenosis undergoing transcatheter aortic valve replacement. J. Am. Soc. Echocardiogr. 33, 1465–1473 (2020).
Cannata, F. et al. Transcatheter aortic valve replacement in aortic stenosis and cardiac amyloidosis: a systematic review and meta-analysis. ESC Heart Fail. 9, 3188–3197 (2022).
Nitsche, C. et al. Prevalence and outcomes of concomitant aortic stenosis and cardiac amyloidosis. J. Am. Coll. Cardiol. 77, 128–139 (2021).
Scully, P. R. et al. Prevalence and outcome of dual aortic stenosis and cardiac amyloid pathology in patients referred for transcatheter aortic valve implantation. Eur. Heart J. 41, 2759–2767 (2020).
Burzotta, F. et al. Clinical impact of heart team decisions for patients with complex valvular heart disease: a large, single-center experience. J. Am. Heart Assoc. 11, e024404 (2022).
Ammar, K. A. et al. Cardiac amyloidosis presenting as severe mitral regurgitation. JACC Cardiovasc. Imaging 9, 1003–1006 (2016).
Krishnaswamy, A., Hanna, M., Goodman, A. & Kapadia, S. R. First reported case of mitraclip placement due to mitral valve flail in the setting of cardiac amyloidosis. Circ. Heart Fail. 9, e003069 (2016).
Donà, C. et al. Unveiling cardiac amyloidosis, its characteristics, and outcomes among patients with MR undergoing transcatheter edge-to-edge MV repair. JACC Cardiovasc. Interv. 15, 1748–1758 (2022).
Braunlin, E. A. et al. Cardiac disease in patients with mucopolysaccharidosis: presentation, diagnosis and management. J. Inherit. Metab. Dis. 34, 1183–1197 (2011).
Rosser, B. A., Chan, C. & Hoschtitzky, A. Surgical management of valvular heart disease in mucopolysaccharidoses: a review of literature. Biomedicines 10, 375 (2022).
Mori, N. et al. Transcatheter aortic valve implantation for severe aortic stenosis in a patient with mucopolysaccharidosis type II (Hunter syndrome) accompanied by severe airway obstruction. J. Cardiol. Cases 25, 49–51 (2021).
Lillo, R., Ingrasciotta, G., Locorotondo, G., Lombardo, A. & Graziani, F. An unusual case of mitral valve chordal rupture. Echocardiography 38, 2109–2111 (2021).
Calcagni, G. et al. Cardiac defects, morbidity and mortality in patients affected by RASopathies. CARNET study results. Int. J. Cardiol. 245, 92–98 (2017).
Sade, L. E. & Akdogan, A. Imaging for screening cardiovascular involvement in patients with systemic rheumatologic diseases: more questions than answers. Eur. Heart J. Cardiovasc. Imaging 20, 967–978 (2019).
Donnellan, E. et al. Outcomes of patients with mediastinal radiation-associated severe aortic stenosis undergoing transcatheter aortic valve replacement. Circulation 138, 1752–1754 (2018).
Donnellan, E. et al. Longterm outcomes of patients with mediastinal radiation-associated severe aortic stenosis and subsequent surgical aortic valve replacement: a matched cohort study. J. Am. Heart Assoc. 6, e005396 (2017).
Donnellan, E. et al. Outcomes of patients with mediastinal radiation-associated mitral valve disease undergoing cardiac surgery. Circulation 140, 1288–1290 (2019).
Wilde, A. A. M. et al. Expert consensus statement on the state of genetic testing for cardiac diseases. Europace 24, 1307–1367 (2022).
Rapezzi, C. et al. Diagnostic work-up in cardiomyopathies: bridging the gap between clinical phenotypes and final diagnosis. A position statement from the ESC working group on myocardial and pericardial diseases. Eur. Heart J. 34, 1448–1458 (2013).
Author information
Authors and Affiliations
Contributions
N.A.M., F.G., M.C.M., H.W.W. and R.L. researched data for the article. N.A.M., F.G., M.C.M. and R.L. provided substantial contribution to the discussion of content. All the authors wrote the manuscript and reviewed and/or edited it before submission.
Corresponding author
Ethics declarations
Competing interests
N.A.M. received speaker fees from Abbott Vascular, GE Healthcare and Philips Ultrasound and a research grant from Alnylam and Pfizer. F.G. received honoraria for board meetings; speaker fees from Sanofi-Genzyme, Shire, Takeda and Pfizer and research grants from Takeda and Pfizer. R.L. received honoraria for board meetings from Sanofi-Genzyme and Shire. J.J.B. received speaker fees from Abbott Vascular. F.B. received speaker fees from Abiomed, Abbott, Medtronic and Terumo. J.W.J. and his department received research grants from and/or was a speaker (with or without lecture fees) at meetings sponsored or supported by Abbott, Amarin, Amgen, Athera, Biotronik, Boston Scientific, Dalcor, Daiichi Sankyo, Edwards Lifesciences, GE Healthcare, Johnson and Johnson, Lilly, Medtronic, Merck-Schering-Plough, Novartis, Novo Nordisk, Pfizer, Roche, Sanofi Aventis, the Netherlands Heart Foundation, CardioVascular Research the Netherlands, the Netherlands Heart Institute and the European Community Framework KP7 Programme. F.C. received personal fees from Amgen, Astra Zeneca, BMS, GlyCardial Diagnostics and Servier. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Cardiology thanks Christopher Semsarian and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ajmone Marsan, N., Graziani, F., Meucci, M.C. et al. Valvular heart disease and cardiomyopathy: reappraisal of their interplay. Nat Rev Cardiol 21, 37–50 (2024). https://doi.org/10.1038/s41569-023-00911-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-023-00911-0