Abstract
Approximately 65 million adults globally have heart failure, and the prevalence is expected to increase substantially with ageing populations. Despite advances in pharmacological and device therapy of heart failure, long-term morbidity and mortality remain high. Many patients progress to advanced heart failure and develop persistently severe symptoms. Heart transplantation remains the gold-standard therapy to improve the quality of life, functional status and survival of these patients. However, there is a large imbalance between the supply of organs and the demand for heart transplants. Therefore, expanding the donor pool is essential to reduce mortality while on the waiting list and improve clinical outcomes in this patient population. A shift has occurred to consider the use of organs from donors with hepatitis C virus, HIV or SARS-CoV-2 infection. Other advances in this field have also expanded the donor pool, including opt-out donation policies, organ donation after circulatory death and xenotransplantation. We provide a comprehensive overview of these various novel strategies, provide objective data on their safety and efficacy, and discuss some of the unresolved issues and controversies of each approach.
Key points
-
Heart transplantation is a crucial therapy for patients with advanced heart failure, but the availability of organs is limited, necessitating strategies to expand the pool of organ donors.
-
Interest is growing in heart transplantation from donors with hepatitis C virus (HCV) viraemia to recipients negative for HCV, with the initial experience of these transplantations producing excellent outcomes, and from donors positive for HIV to recipients positive for HIV.
-
Multiple case series of heart transplantation from donors with positive nucleic acid testing for SARS-CoV-2 infection have reported no significant difference in outcomes compared with heart transplantation from donors without SARS-CoV-2, although a trend towards increased early mortality in recipients from donors with active SARS-CoV-2 infection was reported in one study.
-
An opt-out organ donation policy, in which individuals are presumed to be willing deceased organ donors unless they opt out, is a governmental strategy adopted by various countries to increase the donor pool.
-
Donation after circulatory (rather than brain) death, with either direct procurement and perfusion or normothermic regional perfusion, could initiate the largest expansion in heart transplantation in recent years.
-
Heart xenotransplantation is still largely in the investigational phase but the experience of heart transplantation from gene-edited pigs into humans is promising.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392, 1789–1858 (2018).
Virani, S. S. et al. Heart disease and stroke statistics — 2021 update: a report from the American Heart Association. Circulation 143, e254–e743 (2021).
Heidenreich, P. A. et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ. Heart Fail. 6, 606–619 (2013).
Fang, J. C. et al. Advanced (stage D) heart failure: a statement from the Heart Failure Society of America Guidelines Committee. J. Card. Fail. 21, 519–534 (2015).
Fang, N., Jiang, M. & Fan, Y. Ideal cardiovascular health metrics and risk of cardiovascular disease or mortality: a meta-analysis. Int. J. Cardiol. 214, 279–283 (2016).
Crespo-leiro, M. G. et al. Advanced heart failure: a position statement of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 20, 1505–1535 (2018).
Heidenreich, P. et al. 2022 AHA/ACC/HFSA Guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 145, e895–e1032 (2022).
Kalogeropoulos, A. P. et al. Progression to stage D heart failure among outpatients with stage C heart failure and reduced ejection fraction. JACC Heart Fail. 5, 528–537 (2017).
Colvin, M. et al. OPTN/SRTR 2020 annual data report: heart. Am. J. Transplant. 22, 350–437 (2022).
Khush, K. K. et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: thirty-eighth adult heart transplantation report — 2021; focus on recipient characteristics. J. Heart Lung Transplant. 40, 1035–1049 (2021).
Khush, K. K. et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: thirty-sixth adult heart transplantation report — 2019; focus theme: donor and recipient size match. J. Heart Lung Transplant. 38, 1056–1066 (2019).
NHS Blood and Transplant. How Long is the Wait for a Heart? https://www.nhsbt.nhs.uk/organ-transplantation/heart/receiving-a-heart/how-long-is-the-wait-for-a-heart (2022).
Truby, L. & Rogers, J. Advanced heart failure: epidemiology, diagnosis, and therapeutic approaches. JACC Heart Fail. 8, 523–536 (2020).
US Department of Health and Human Services. Organ Procurement and Transplantation Network https://optn.transplant.hrsa.gov/data/view-data-reports/national-data (2022).
Roest, S. et al. Waiting list mortality and the potential of donation after circulatory death heart transplantations in the Netherlands. Neth. Heart J. 29, 88–97 (2021).
Sun, Y. F. et al. Current status of and opinions on heart transplantation in China. Curr. Med. Sci. 41, 841–846 (2021).
Bakhtiyar, S. S. et al. Survival on the heart transplant waiting list. JAMA Cardiol. 5, 1227–1235 (2020).
Kittleson, M. M. & Kobashigawa, J. A. Cardiac transplantation: current outcomes and contemporary controversies. JACC Heart Fail. 5, 857–868 (2017).
Tong, C. K. W. & Khush, K. K. New approaches to donor selection and preparation in heart transplantation. Curr. Treat. Options Cardiovasc. Med. 23, 28 (2021).
Sathianathan, S. & Bhat, G. Heart transplant donor selection guidelines: review and recommendations. Curr. Cardiol. Rep. 24, 119–130 (2022).
DeFilippis, E. M. et al. Evolving characteristics of heart transplantation donors and recipients: JACC focus seminar. J. Am. Coll. Cardiol. 79, 1108–1123 (2022).
Haji, S. A. et al. Donor hepatitis-C seropositivity is an independent risk factor for the development of accelerated coronary vasculopathy and predicts outcome after cardiac transplantation. J. Heart Lung Transplant. 23, 277–283 (2004).
Gasink, L. B. et al. Hepatitis C virus seropositivity in organ donors and survival in heart transplant recipients. J. Am. Med. Assoc. 296, 1843–1850 (2006).
British Viral Hepatitis Group. UK Position Statement on the Use of Organs from Hepatitis C Viraemic Donors and Increased Infectious Risk Donors in Hepatitis C https://go.nature.com/46Mb1LM (2021).
Levitsky, J. et al. The American Society of Transplantation consensus conference on the use of hepatitis C viremic donors in solid organ transplantation. Am. J. Transplant. 17, 2790–2802 (2017).
Mehra, M. et al. The drug-intoxication epidemic and solid-organ transplantation. N. Engl. J. Med. 378, 1943–1945 (2018).
Durand, C. et al. The drug overdose epidemic and deceased-donor transplantation in the United States. Ann. Intern. Med. 168, 702–711 (2018).
Huckaby, L. V. et al. Center-level utilization of hepatitis C virus-positive donors for orthotopic heart transplantation. Transplantation 105, 2639–2645 (2021).
Aslam, S. et al. Utilization of hepatitis C virus-infected organ donors in cardiothoracic transplantation: an ISHLT expert consensus statement. J. Heart Lung Transplant. 39, 418–432 (2020).
Bruno, S. et al. Heart transplantation from hepatitis C-positive donors in the era of direct acting antiviral therapy: a comprehensive literature review. Transplant. Direct 5, e486 (2019).
Aslam, S., Yumul, I., Mariski, M., Pretorius, V. & Adler, E. Outcomes of heart transplantation from hepatitis C virus–positive donors. J. Heart Lung Transplant. 38, 1259–1267 (2019).
Schlendorf, K. H. et al. Expanding heart transplant in the era of direct-acting antiviral therapy for hepatitis C. JAMA Cardiol. 5, 167–174 (2020).
Lewis, T. C. et al. Management and tolerability of glecaprevir-pibrentasvir pharmacotherapy in hepatitis C viremic heart and lung transplant recipients. Clin. Transplant. 34, e14030 (2020).
Moayedi, Y. et al. Current use of hearts from hepatitis C viremic donors. Circ. Heart Fail. 11, e005276 (2018).
Gernhofer, Y. K. et al. The impact of using hepatitis c virus nucleic acid test–positive donor hearts on heart transplant waitlist time and transplant rate. J. Heart Lung Transplant. 38, 1178–1188 (2019).
Reyentovich, A. et al. Outcomes of the treatment with glecaprevir/pibrentasvir following heart transplantation utilizing hepatitis C viremic donors. Clin. Transplant. 34, e13989 (2020).
Smith, D. E. et al. Impact of early initiation of direct-acting antiviral therapy in thoracic organ transplantation from hepatitis C virus positive donors. Semin. Thorac. Cardiovasc. Surg. 33, 407–415 (2021).
Stachel, M. W. et al. Long-term follow-up of acute and chronic rejection in heart transplant recipients from hepatitis C viremic (NAT+) donors. Am. J. Transplant. 22, 2951–2960 (2022).
Villegas-Galaviz, J., Anderson, E. & Guglin, M. Clinical outcomes of heart transplantation using hepatitis C-viremic donors: a systematic review with meta-analysis. J. Heart Lung Transplant. 41, 538–549 (2022).
Kilic, A. et al. Outcomes of adult heart transplantation using hepatitis C-positive donors. J. Am. Heart Assoc. 9, e014495 (2020).
Gidea, C. G. et al. Increased early acute cellular rejection events in hepatitis C-positive heart transplantation. J. Heart Lung Transplant. 39, 1199–1207 (2020).
Stewart, Z. A. et al. Clinical and financial implications of 2 treatment strategies for donor-derived hepatitis C infections. Transplant. Direct 7, e762 (2021).
Woolley, A. E. et al. The cost-effectiveness of transplanting hearts from hepatitis C-infected donors into uninfected recipients. Transplantation 107, 961–969 (2023).
Rochlani, Y., Diab, K. & Jorde, U. P. Hepatitis C-positive donors in cardiac transplantation: problems and opportunities. Curr. Heart Fail. Rep. 17, 106–115 (2020).
Siddiqi, H. K. & Schlendorf, K. H. Hepatitis C positive organ donation in heart transplantation. Curr. Transplant. Rep. 8, 359–367 (2021).
Ingelfinger, J. R. & Rubin, E. J. The HIV-positive transplant donor — change born of necessity. N. Engl. J. Med. 372, 663–665 (2015).
Muller, E., Barday, Z., Mendelson, M. & Kahn, D. HIV-positive-to-HIV-positive kidney transplantation —results at 3 to 5 years. N. Engl. J. Med. 372, 613–620 (2015).
Woods, C. et al. Efficacy of hope: analysis of organ quality and availability among deceased HIV-positive donors. Transpl. Infect. Dis. 24, e13916 (2022).
Mehta, S. & Locke, J. E. Human immunodeficiency virus from life taking to life giving: expanding the donor pool by using HIV-positive donors. Curr. Opin. Organ Transplant. 25, 626–630 (2020).
Uriel, N. et al. Heart transplantation in human immunodeficiency virus-positive patients. J. Heart Lung Transplant. 28, 667–669 (2009).
Doberne, J. W. et al. Heart transplantation survival outcomes of HIV positive and negative recipients. Ann. Thorac. Surg. 111, 1465–1471 (2021).
Organ Procurement and Transplantation Network. HOPE Act https://optn.transplant.hrsa.gov/learn/professional-education/hope-act (2022).
Bonny, T. et al. Outcomes of donor-derived superinfection screening in HIV-positive to HIV-positive kidney and liver transplantation a multicentre, prospective, observational study. Lancet HIV 7, e611–e619 (2020).
Montefiore. World’s First HIV-Positive to HIV-Positive Heart Transplant Performed at Montefiore Health System https://www.montefiore.org/body.cfm?id=1738&action=detail&ref=2194 (2022).
ABC7 NY. Recipient in 1st HIV-positive Heart Transplant Meets Donor’s Family After Groundbreaking Surgery https://abc7ny.com/hiv-positive-heart-transplant-montefiore-donor-recipient/12481563/ (2022).
Madan, S. et al. Outcomes of heart transplantation in patients with human immunodeficiency virus. Am. J. Transplant. 19, 1529–1535 (2019).
Ison, M. G. et al. Transmission of human immunodeficiency virus and hepatitis C virus from an organ donor to four transplant recipients. Am. J. Transplant. 11, 1218–1225 (2011).
Simonds, R. J. HIV transmission by organ and tissue transplantation. AIDS 7S35, S35–S38 (1993).
Aslam, S. et al. Guidance from the International Society of Heart and Lung Transplantation Regarding the SARS CoV-2 Pandemic. ISHLT https://ishlt.org/ishlt/media/documents/SARS-CoV-2_-Guidance-for-Cardiothoracic-Transplant-and-VAD-centers.pdf (2020).
Eichenberger, E. M. et al. Transplanting thoracic COVID-19 positive donors: an institutional protocol and report of the first 14 cases. J. Heart Lung Transplant. 41, 1376–1381 (2022).
Bock, M. J. et al. Organ transplantation using COVID-19-positive deceased donors. Am. J. Transplant. 22, 2203–2216 (2022).
Neidlinger, N. A. et al. Organ recovery from deceased donors with prior COVID-19: a case series. Transpl. Infect. Dis. 23, e13503 (2021).
Schold, J. D., Koval, C. E., Wee, A., Eltemamy, M. & Poggio, E. D. Utilization and outcomes of deceased donor SARS-CoV-2-positive organs for solid organ transplantation in the United States. Am. J. Transplant. 22, 2217–2227 (2022).
Martinez-Reviejo, R. et al. Solid organ transplantation from donors with recent or current SARS-CoV-2 infection: a systematic review. Anaesth. Crit. Care Pain. Med. 41, 101098 (2022).
Ushiro-Lumb, I. et al. Transplantation of organs from SARS-CoV-2 RNA positive deceased donors: the UK experience so far. Transplantation 106, e418–e419 (2022).
Madgula, A. S. et al. Tackling the paradox of orthotropic heart transplantation from SARS-CoV-2 positive donors: a single center experience. J. Heart Lung Transplant. 41, 1650–1653 (2022).
Dhand, A., Okumura, K., Nabors, C. & Nishida, S. Solid organ transplantation from COVID positive donors in the United States: analysis of United Network for organ sharing database. Transpl. Infect. Dis. 25, e13925 (2023).
Madan, S. et al. Early outcomes of adult heart transplantation from COVID-19 infected donors. J. Am. Coll. Cardiol. https://doi.org/10.1016/j.jacc.2023.04.022 (2023).
Etheredge, H. R. Assessing global organ donation policies: opt-in vs opt-out. Risk Manag. Healthc. Policy 14, 1985–1998 (2021).
Kaushik, J. Organ transplant and presumed consent: towards an ‘opting out’ system. Indian J. Med. Ethics 6, 149–152 (2009).
Shepherd, L., O’Carroll, R. E. & Ferguson, E. An international comparison of deceased and living organ donation/transplant rates in opt-in and opt-out systems: a panel study. BMC Med. 12, 131 (2014).
Wu, Y. et al. Cadaveric organ donation in China: a crossroads for ethics and sociocultural factors. Medicine 97, e9951 (2018).
Arshad, A., Anderson, B. & Sharif, A. Comparison of organ donation and transplantation rates between opt-out and opt-in systems. Kidney Int. 95, 1453–1460 (2019).
Golsteyn, B. H. H. & Verhagen, A. M. C. Deceased by default: consent systems and organ-patient mortality. PLoS ONE 16, e0247719 (2021).
Jansen, N. E., Williment, C., Haase-Kromwijk, B. J. J. M. & Gardiner, D. Changing to an opt out system for organ donation-reflections from England and Netherlands. Transpl. Int. 35, 10466 (2022).
Watson, M. B. Presumed consent for organ transplantation: a better system. Curr. Surg. 60, 156–157 (2003).
Davidai, S., Gilovich, T. & Ross, L. D. The meaning of default options for potential organ donors. Proc. Natl Acad. Sci. USA 109, 15201–15205 (2012).
Ahmad, M. U. et al. A systematic review of opt-out versus opt-in consent on deceased organ donation and transplantation (2006-2016). World J. Surg. 43, 3161–3171 (2019).
Rithalia, A. et al. A systematic review of presumed consent systems for deceased organ donation. Health Technol. Assess. 13, 1–95 (2009).
Appadurai, A. Presumed consent to organ donation: 10 years’ experience in Belgium. J. R. Soc. Med. 89, 663–666 (1996).
Domínguez, J. & Rojas, J. L. Presumed consent legislation failed to improve organ donation in Chile. Transplant. Proc. 45, 1316–1317 (2013).
Ezaz, G. & Lai, M. How the ‘opt-in’ option optimizes organ donation rates. Dig. Dis. Sci. 64, 1067–1069 (2019).
Matesanz, R. & Domínguez-Gil, B. Opt-out legislations: the mysterious viability of the false. Kidney Int. 95, 1301–1303 (2019).
Fabre, J., Murphy, P. & Matesanz, R. Presumed consent: a distraction in the quest for increasing rates of organ donation. BMJ 341, c4973 (2010).
Glazier, A. & Mone, T. Success of opt-in organ donation policy in the United States. J. Am. Med. Assoc. 322, 719–720 (2019).
Zúñiga-Fajuri, A. Increasing organ donation by presumed consent and allocation priority: Chile. Bull. World Health Organ. 93, 199–202 (2015).
Cronin, A. J. Points mean prizes: priority points, preferential status and directed organ donation in Israel. Isr. J. Health Policy Res. 3, 8 (2014).
Kootstra, G., Daemen, J. & Oomen, A. P. Categories of non-heart-beating donors. Transpl. Proc. 27, 2893–2894 (1995).
Thuong, M. et al. New classification of donation after circulatory death donors definitions and terminology. Transpl. Int. 29, 749–759 (2016).
Reich, D. J. et al. ASTS recommended practice guidelines for controlled donation after cardiac death organ procurement and transplantation. Am. J. Transplant. 9, 2004–2011 (2009).
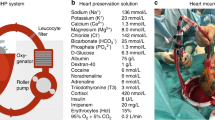
Scheuer, S. E., Jansz, P. C. & Macdonald, P. S. Heart transplantation following donation after circulatory death: expanding the donor pool. J. Heart Lung Transplant. 40, 882–889 (2021).
Page, A., Messer, S. & Large, S. R. Heart transplantation from donation after circulatory determined death. Ann. Cardiothorac. Surg. 7, 75–81 (2018).
Niederberger, P. et al. Heart transplantation with donation after circulatory death. Circ. Heart Fail. 12, e005517 (2019).
Truby, L. K. et al. Donation after circulatory death in heart transplantation: history, outcomes, clinical challenges, and opportunities to expand the donor pool. J. Card. Fail. 28, 1456–1463 (2022).
Ardehali, A. et al. Ex-vivo perfusion of donor hearts for human heart transplantation (PROCEED II): a prospective, open-label, multicentre, randomised non-inferiority trial. Lancet 385, 2577–2584 (2015).
Schroder, J. et al. Successful utilization of extended criteria donor (ECD) hearts for transplantation — results of the OCSTM heart EXPAND trial to evaluate the effectiveness and safety of the OCS heart system to preserve and assess ECD hearts for transplantation. J. Heart Lung Transplant. 38, S42 (2019).
Dhital, K. K. et al. Adult heart transplantation with distant procurement and ex-vivo preservation of donor hearts after circulatory death: a case series. Lancet 385, 2585–2591 (2015).
Messer, S. J. et al. Functional assessment and transplantation of the donor heart after circulatory death. J. Heart Lung Transplant. 35, 1443–1452 (2016).
Messer, S. et al. Outcome after heart transplantation from donation after circulatory-determined death donors. J. Heart Lung Transplant. 36, 1311–1318 (2017).
Chew, H. et al. Outcomes of donation after circulatory death heart transplantation in Australia. J. Am. Coll. Cardiol. 73, 1447–1459 (2019).
Dhital, K., Ludhani, P., Scheuer, S., Connellan, M. & Macdonald, P. DCD donations and outcomes of heart transplantation: the Australian experience. Indian J. Thorac. Cardiovasc. Surg. 36, 224–232 (2020).
Iyer, A. & Dhital, K. Cardiac donation after circulatory death. Curr. Opin. Organ Transplant. 25, 241–247 (2020).
Messer, S. et al. A 5-year single-center early experience of heart transplantation from donation after circulatory-determined death donors. J. Heart Lung Transplant. 39, 1463–1475 (2020).
Abbasi, J. “Donation after circulatory death” heart transplant is a US first. J. Am. Med. Assoc. 323, 111 (2020).
Hoffman, J. R. H. et al. Early US experience with cardiac donation after circulatory death (DCD) using normothermic regional perfusion. J. Heart Lung Transplant. 40, 1408–1418 (2021).
Jawitz, O. K., Bryner, B. S., Schroder, J. N. & DeVore, A. D. Donation after circulatory death heart transplantation in the United States: an early report of donor characteristics. JTCVS Tech. 12, 104–107 (2022).
Suarez-Pierre, A. et al. Appraisal of donation after circulatory death: how far could we expand the heart donor pool? Ann. Thorac. Surg. 114, 676–682 (2022).
Madan, S. et al. Feasibility and potential impact of heart transplantation from adult donors after circulatory death. J. Am. Coll. Cardiol. 79, 148–162 (2022).
Smith, D. E. et al. Early experience with donation after circulatory death heart transplantation using normothermic regional perfusion in the United States. J. Thorac. Cardiovasc. Surg. 164, 557–568.e1 (2022).
Louca, J. et al. The international experience of in-situ recovery of the DCD heart: a multicentre retrospective observational study. eClinicalMedicine 58, 101887 (2023).
D’Alessandro, D. A. et al. Hemodynamic and clinical performance of hearts donated after circulatory death. J. Am. Coll. Cardiol. 80, 1314–1326 (2022).
Schroder, J. et al. Expanding heart transplants from donors after circulatory death (DCD) — results of the first randomized controlled trial using the Organ Care System (OCSTM) heart — (OCS DCD heart trial). J. Heart Lung Transplant. 41, S72 (2022).
Farr, M. et al. Potential for donation after circulatory death heart transplantation in the United States: retrospective analysis of a limited UNOS dataset. Am. J. Transplant. 20, 525–529 (2020).
Pagani, F. D. Heart transplantation using organs from donors following circulatory death: the journey continues. J. Am. Coll. Cardiol. 79, 163–165 (2022).
Parent, B. et al. Ethical and logistical concerns for establishing NRP-cDCD heart transplantation in the United States. Am. J. Transplant. 20, 1508–1512 (2020).
Rajab, T. K. & Singh, S. K. Donation after cardiac death heart transplantation in America is clinically necessary and ethically justified. Circ. Heart Fail. 11, e004884 (2018).
Ave, A. L. D., Sulmasy, D. P. & Bernat, J. L. The ethical obligation of the dead donor rule. Med. Health Care Philos. 23, 43–50 (2020).
American College of Physicians. Ethics, Determination of Death, and Organ Transplantation in Normothermic Regional Perfusion (NRP) with Controlled Donation After Circulatory Determination of Death (cDCD): American College of Physicians Statement of Concern https://www.acponline.org/acp_policy/policies/ethics_determination_of_death_and_organ_transplantation_in_nrp_2021.pdf (2021).
Vanholder, R. et al. Organ donation and transplantation: a multi-stakeholder call to action. Nat. Rev. Nephrol. 17, 554–568 (2021).
Parent, B., Caplan, A., Moazami, N. & Montgomery, R. A. Response to American College of Physician’s statement on the ethics of transplant after normothermic regional perfusion. Am. J. Transplant. 22, 1307–1310 (2022).
Smith, D. & Moazami, N. Commentary: normothermic regional perfusion: ethical issues in thoracic organ donation: an important discussion, but stop the press! J. Thorac. Cardiovasc. Surg. 164, 155–156 (2022).
Kon, Z. N., Smith, D. E., Carillo, J. A. & Moazami, N. Commentary: the future is now — heart donation after circulatory death. J. Thorac. Cardiovasc. Surg. 161, 1342–1343 (2021).
Moazami, N., Smith, D. & Galloway, A. Logistics for expanding heart transplantation from donation after circulatory death using normothermic regional perfusion. JTCVS Tech. 12, 110–112 (2022).
Hardy, J. D. et al. Heart transplantation in man. Developmental studies and report of a case. J. Am. Med. Assoc. 188, 1132–1140 (1964).
Shu, S., Ren, J. & Song, J. Cardiac xenotransplantation: a promising way to treat advanced heart failure. Heart Fail. Rev. 27, 71–91 (2022).
Yang, B. Q., Park, A. C. & Schilling, J. D. Cardiac xenotransplantation: 5 things every cardiologist should know. JACC Basic Transl. Sci. 7, 518–521 (2022).
Montgomery, R. A., Mehta, S. A., Parent, B. & Griesemer, A. Next steps for the xenotransplantation of pig organs into humans. Nat. Med. 28, 1533–1536 (2022).
Vadori, M. & Cozzi, E. The immunological barriers to xenotransplantation. Tissue Antigens 86, 239–253 (2015).
Pierson, R. N. 3rd Progress toward pig-to-human xenotransplantation. N. Engl. J. Med. 386, 1871–1873 (2022).
Boulet, J., Cunningham, J. W. & Mehra, M. R. Cardiac xenotransplantation: challenges, evolution, and advances. JACC Basic Transl. Sci. 7, 716–729 (2022).
Sykes, M. & Sachs, D. H. Transplanting organs from pigs to humans. Sci. Immunol. 4, eaau6298 (2019).
Phimister, E. G. Genetic modification in pig-to-human transplantation. N. Engl. J. Med. 387, 79–82 (2022).
Hamadeh, R. M., Galili, U., Zhou, P. & Griffiss, J. M. Anti-alpha-galactosyl immunoglobulin A (IgA), IgG, and IgM in human secretions. Clin. Diagn. Lab. Immunol. 2, 125–131 (1995).
Zappe, A., Rosenlöcher, J., Kohla, G., Hinderlich, S. & Parr, M. K. Purification and characterization of antibodies directed against the α-Gal epitope. BioChem 1, 81–97 (2021).
Sandrin, M. S. & McKenzie, I. F. Galα(1,3)Gal, the major xenoantigen(s) recognised in pigs by human natural antibodies. Immunol. Rev. 141, 169–190 (1994).
Candinas, D. & Adams, D. H. Xenotransplantation: postponed by a millennium? Q. J. Med. 93, 63–66 (2000).
Dai, Y. et al. Targeted disruption of the alpha1,3-galactosyltransferase gene in cloned pigs. Nat. Biotechnol. 20, 251–255 (2002).
Dolgin, E. First GM pigs for allergies. Could xenotransplants be next? Nat. Biotechnol. 39, 397–400 (2021).
US Food & Drug Administration. FDA Approves First-of-its-Kind Intentional Genomic Alteration in Line of Domestic Pigs for Both Human Food, Potential Therapeutic Uses https://www.fda.gov/news-events/press-announcements/fda-approves-first-its-kind-intentional-genomic-alteration-line-domestic-pigs-both-human-food (2020).
Montgomery, R. A. et al. Results of two cases of pig-to-human kidney xenotransplantation. N. Engl. J. Med. 386, 1889–1898 (2022).
Mehra, M. R. Cardiac xenotransplantation: rebirth amidst an uncertain future. J. Card. Fail. 28, 873–874 (2022).
Miyagawa, S. et al. Aspects of the complement system in new era of xenotransplantation. Front. Immunol. 13, 860165 (2022).
Porrett, P. M. et al. First clinical-grade porcine kidney xenotransplant using a human decedent model. Am. J. Transplant. 22, 1037–1053 (2022).
Boksa, M., Zeyland, J., Słomski, R. & Lipiński, D. Immune modulation in xenotransplantation. Arch. Immunol. Ther. Exp. 63, 181–192 (2015).
Yamamoto, T. et al. Life-supporting kidney xenotransplantation from genetically engineered pigs in baboons: a comparison of two immunosuppressive regimens. Transplantation 103, 2090–2104 (2019).
Adams, A. B. et al. Anti-C5 antibody tesidolumab reduces early antibody-mediated rejection and prolongs survival in renal xenotransplantation. Ann. Surg. 274, 473–480 (2021).
Eiras, G. et al. Species differences in sensitivity of T lymphocytes to immunosuppressive effects of FK 506. Transplantation 49, 1170–1172 (1990).
Cooper, D. K. C. et al. Report of the Xenotransplantation Advisory Committee of the International Society for Heart and Lung Transplantation: the present status of xenotransplantation and its potential role in the treatment of end-stage cardiac and pulmonary diseases. J. Heart Lung Transplant. 19, 1125–1165 (2000).
Platt, J., DiSesa, V., Gail, D. & Massicot-Fisher, J. Recommendations of the National Heart, Lung, and Blood Institute Heart and Lung Xenotransplantation Working Group. Circulation 106, 1043–1047 (2002).
Niu, D. et al. Inactivation of porcine endogenous retrovirus in pigs using CRISPR-Cas9. Science 357, 1303–1307 (2017).
Griffith, B. P. et al. Genetically modified porcine-to-human cardiac xenotransplantation. N. Engl. J. Med. 387, 35–44 (2022).
Denner, J. et al. Impact of porcine cytomegalovirus on long-term orthotopic cardiac xenotransplant survival. Sci. Rep. 10, 17531 (2020).
NYU Langone Health. Successful Heart Xenotransplant Experiments at NYU Langone Set Protocol for Pig-to-Human Organ Transplants https://nyulangone.org/news/successful-heart-xenotransplant-experiments-nyu-langone-set-protocol-pig-human-organ-transplants (2022).
Schoenrath, F., Falk, V. & Emmert, M. Y. Xenotransplantation in the era of a zoonotic pandemic. Eur. Heart J. 42, 1283–1285 (2021).
Pig-to-human transplants take a leap toward reality. Nat. Med. 28, 423 (2022).
Mann, D. L. When pigs fly what will the future of heart failure therapeutics look like? JACC Basic. Transl. Sci. 7, 745–746 (2022).
Kuehn, B. M. First pig-to-human heart transplant marks a milestone in xenotransplantation. Circulation 145, 1870–1871 (2022).
Pierson, R. N. 3rd et al. Progress toward cardiac xenotransplantation. Circulation 142, 1389–1398 (2020).
Chaban, R., Cooper, D. K. C. & Pierson, R. N. 3rd Pig heart and lung xenotransplantation: present status. J. Heart Lung Transplant. 41, 1014–1022 (2022).
Reichart, B. et al. Pig-to-non-human primate heart transplantation: the final step toward clinical xenotransplantation? J. Heart Lung Transplant. 39, 751–757 (2020).
Farr, M. & Stehlik, J. Heart xenotransplant: a door that is finally opening. Circulation 145, 871–873 (2022).
Author information
Authors and Affiliations
Contributions
S.J., S.M., J.F. and L.M. researched data for the article. All the authors contributed to the discussion of content. S.J., S.M., J.F., L.M. and M.M. wrote the manuscript. All the authors reviewed/edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Cardiology thanks Axel Haverich, Bruno Reichart and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jou, S., Mendez, S.R., Feinman, J. et al. Heart transplantation: advances in expanding the donor pool and xenotransplantation. Nat Rev Cardiol 21, 25–36 (2024). https://doi.org/10.1038/s41569-023-00902-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-023-00902-1
This article is cited by
-
Levothyroxine supplementation does not improve heart transplantation from brain-dead donors
Nature Reviews Cardiology (2024)