Abstract
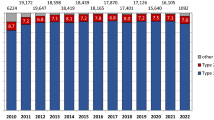
This Review provides an epidemiological overview of global mortality from acute coronary syndromes (ACS). Across the regions of the world where data are available, mortality from ACS — including premature (age <70 years) mortality from ACS — was higher in men than in women. In both sexes, age-standardized mortality rates (ASMRs) for ACS in 2020 were highest in lower-income global regions. However, 20 years earlier, ASMRs for ACS were highest in higher-income global regions, including Europe, Northern America and Oceania. These higher-income regions have seen progressive reductions in mortality from ACS during the past 20 years, which is in contrast to the more stable levels of mortality from ACS in Asia and in Latin America and the Caribbean. In the seven African countries with data available, a small upwards trend in ASMRs for ACS was observed, reflecting an epidemiological transition that is already well advanced in these regions. Consistent with these changes during the past 20 years were >50% reductions in ASMRs for ACS in the high-income countries of the world compared with <15% reductions in lower-middle-income countries. Policymakers need more complete epidemiological data across and within global regions to identify those countries in which the burden of death from ACS is greatest and the need to implement preventive strategies is most pressing.
Key points
-
The availability of data on mortality from acute coronary syndromes (ACS) is heterogeneous between global regions and is particularly sparse across sub-Saharan Africa and large parts of Asia.
-
In all regions of the world with available data, age-standardized mortality rates (ASMRs) for ACS were higher in men than in women.
-
In 2020, ASMRs for ACS in both sexes were higher in lower-income regions (Africa, Asia, and Latin America and the Caribbean) than in higher-income regions (Europe, Northern America and Oceania).
-
In Europe, Northern America and Oceania, steep declines in ASMRs for ACS have occurred in both men and women in the past 20 years, but ASMRs for ACS have increased in several Latin American, Caribbean and Asian countries.
-
Consistent with these regional changes are marked reductions in ASMRs for ACS in high-income countries during the past 20 years, whereas ASMRs for ACS have increased in lower-middle-income countries in both men and women.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
World Health Organization. Cardiovascular Diseases https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1 (2023).
Sanchis-Gomar, F., Perez-Quilis, C., Leischik, R. & Lucia, A. Epidemiology of coronary heart disease and acute coronary syndrome. Ann. Transl. Med. 4, 256 (2016).
Shah, R. et al. Epidemiology report: trends in sex-specific cerebrovascular disease mortality in Europe based on WHO mortality data. Eur. Heart J. 40, 755–764 (2019).
Townsend, N. et al. Cardiovascular disease in Europe: epidemiological update 2016. Eur. Heart J. 37, 3232–3245 (2016).
Mok, A. et al. Physical activity trajectories and mortality: population based cohort study. Br. Med. J. 365, l2323 (2019).
Li, C. et al. Long-term physical activity participation trajectories were associated with subsequent cognitive decline, risk of dementia and all-cause mortality among adults aged ≥50 years: a population-based cohort study. Age Ageing 51, afac071 (2022).
Roffi, M. et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur. Heart J. 37, 267–315 (2016).
National Institute for Health and Care Excellence. Acute Coronary Syndromes: NICE Guideline [NG185] https://www.nice.org.uk/guidance/ng185 (2020).
Thygesen, K. et al. Fourth universal definition of myocardial infarction. Eur. Heart J. 40, 237–269 (2018).
Sandoval, Y. et al. High-sensitivity cardiac troponin and the 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guidelines for the evaluation and diagnosis of acute chest pain. Circulation 146, 569–581 (2022).
Braunwald, E. & Morrow, D. A. Unstable angina: is it time for a requiem? Circulation 127, 2452–2457 (2013).
Eggers, K. M., Jernberg, T. & Lindahl, B. Unstable angina in the era of cardiac troponin assays with improved sensitivity — a clinical dilemma. Am. J. Med. 130, 1423–1430 (2017).
Yusuf, S. et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 364, 937–952 (2004).
World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases https://apps.who.int/iris/bitstream/handle/10665/94384/?sequence=1 (2013).
Ahmad, O. B. et al. Age Standardization of Rates: A New WHO Standard https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/gpe_discussion_paper_series_paper31_2001_age_standardization_rates.pdf (2001).
Hamdeh, N., van Rompaey, C. & Metreau, E. New World Bank Country Classifications by Income Level: 2021–2022 https://blogs.worldbank.org/opendata/new-world-bank-country-classifications-income-level-2021-2022 (2021).
Habibzadeh, F. Statistical data editing in scientific articles. J. Korean Med. Sci. 32, 1072–1076 (2017).
Cleveland, W. S. Robust locally weighted regression and smoothing scatter-plots. J. Am. Stat. Assoc. 74, 829–836 (1979).
Ralapanawa, U. & Sivakanesan, R. Epidemiology and the magnitude of coronary artery disease and acute coronary syndrome: a narrative review. J. Epidemiol. Glob. Health 11, 169–177 (2021).
Cao, B. et al. WHO Methods and Data Sources for Country-level Causes of Death 2000–2019 https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/ghe2019_cod_methods.pdf (2020).
Abouzahr, C., Mikkelsen, L., Rampatige, R. & Lopez, A. Mortality statistics: a tool to enchance understanding and improve quality. Pac. Health Dialog. 18, 247–270 (2012).
Bhalla, K., Harrison, J. E., Shahraz, S. & Fingerhut, L. A. Availability and quality of cause-of-death data for estimating the global burden of injuries. Bull. World Health Organ. 88, 831–838C (2010).
Yeh, S. T., Ng, Y. Y. & Wu, S. C. Hospital and patient characteristics regarding the place of death of hospitalized impending death patients: a multilevel analysis. Int. J. Environ. Res. Public Health 16, 4609 (2019).
Cárdenas-Turanzas, M., Torres-Vigil, I., Tovalín-Ahumada, H. & Nates, J. L. Hospital versus home death: results from the Mexican Health and Aging Study. J. Pain. Symptom Manag. 41, 880–892 (2011).
Iburg, K. M., Mikkelsen, L., Adair, T. & Lopez, A. D. Are cause of death data fit for purpose? Evidence from 20 countries at different levels of socio-economic development. PLoS One 15, e0237539 (2020).
Mikkelsen, L. et al. A global assessment of civil registration and vital statistics systems: monitoring data quality and progress. Lancet 386, 1395–1406 (2015).
Tsao, C. W. et al. Heart disease and stroke statistics — 2023 update: a report from the American Heart Association. Circulation 147, e93–e621 (2023).
Timmis, A. et al. European Society of Cardiology: cardiovascular disease statistics 2021. Eur. Heart J. 43, 716–799 (2022).
Gouda, H. N. et al. Burden of non-communicable diseases in sub-Saharan Africa, 1990-2017: results from the Global Burden of Disease Study 2017. Lancet Glob. Health 7, e1375–e1387 (2019).
Statista. Distribution of the Leading Causes of Death in Africa in 2019 https://www.statista.com/statistics/1029337/top-causes-of-death-africa/ (2023).
Nichols, M., Townsend, N., Scarborough, P. & Rayner, M. Trends in age-specific coronary heart disease mortality in the European Union over three decades: 1980-2009. Eur. Heart J. 34, 3017–3027 (2013).
Shah, R. et al. Trends in sex-specific cerebrovascular disease mortality in Europe based on WHO mortality data. Eur. Heart J. 40, 755–764 (2019).
Kopp, W. How western diet and lifestyle drive the pandemic of obesity and civilization diseases. Diabetes Metab. Syndr. Obes. 12, 2221–2236 (2019).
Smolina, K. et al. Determinants of the decline in mortality from acute myocardial infarction in England between 2002 and 2010: linked national database study. Br. Med. J. 344, d8059 (2012).
O’Flaherty, M., Buchan, I. & Capewell, S. Contributions of treatment and lifestyle to declining CVD mortality: why have CVD mortality rates declined so much since the 1960s? Heart 99, 159–162 (2013).
Dai, H. et al. Global, regional, and national burden of ischaemic heart disease and its attributable risk factors, 1990-2017: results from the Global Burden of Disease Study 2017. Eur. Heart J. Qual. Care Clin. Outcomes 8, 50–60 (2022).
Mackay, D. F., Irfan, M. O., Haw, S. & Pell, J. P. Meta-analysis of the effect of comprehensive smoke-free legislation on acute coronary events. Heart 96, 1525–1530 (2010).
World Health Organization. WHO Global Report on Trends in Prevalence of Tobacco Use 2000–2025, Fourth Edition https://www.who.int/publications/i/item/9789240039322 (2021).
Xie, J. et al. Global burden of type 2 diabetes in adolescents and young adults, 1990-2019: systematic analysis of the Global Burden of Disease Study 2019. Br. Med. J. 379, e072385 (2022).
World Health Organization. Global Action Plan for the Prevention and Control of NCDs 2013–2020 https://www.who.int/publications/i/item/9789241506236 (2013).
Mensah, G. A. Ischaemic heart disease in Africa. Heart 94, 836–843 (2008).
Fuster, V. & Kelly, B. B. Institute of Medicine (US) Committee on Preventing the Global Epidemic of Cardiovascular Disease: Meeting the Challenges in Developing Countries. Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health (National Academies Press, 2010).
Uthman, O. A. et al. Multiple risk factor interventions for primary prevention of cardiovascular disease in low- and middle-income countries. Cochrane Database Syst. Rev. 8, CD011163 (2015).
Park, J. & Oremus, M. Review of cardiovascular disease primary prevention interventions in low- and middle-income countries [abstract]. J. Epidemiol. Commun. Health 69, A003 (2015).
Aminde, L. N. et al. Primary and secondary prevention interventions for cardiovascular disease in low-income and middle-income countries: a systematic review of economic evaluations. Cost. Eff. Resour. Alloc. 16, 22 (2018).
Oliver, K. A. et al. Identifying public health policymakers’ sources of information: comparing survey and network analyses. Eur. J. Public Health 27, 118–123 (2017).
Townsend, N. et al. Epidemiology of cardiovascular disease in Europe. Nat. Rev. Cardiol. 19, 133–143 (2022).
Finegold, J. A., Asaria, P. & Francis, D. P. Mortality from ischaemic heart disease by country, region, and age: statistics from World Health Organisation and United Nations. Int. J. Cardiol. 168, 934–945 (2013).
Khan, M. A. et al. Global epidemiology of ischemic heart disease: results from the Global Burden of Disease Study. Cureus 12, e9349 (2020).
Safiri, S. et al. Burden of ischemic heart disease and its attributable risk factors in 204 countries and territories, 1990-2019. Eur. J. Prev. Cardiol. 29, 420–431 (2022).
Crea, F. & Liuzzo, G. Pathogenesis of acute coronary syndromes. J. Am. Coll. Cardiol. 61, 1–11 (2013).
Tamis-Holland, J. E. et al. Contemporary diagnosis and management of patients with myocardial infarction in the absence of obstructive coronary artery disease: a scientific statement from the American Heart Association. Circulation 139, 891–908 (2019).
Khan, A. et al. Myocardial Infarction with non-obstructive coronary arteries: an updated overview of pathophysiology, diagnosis, and management. Cureus 14, e23602 (2022).
British Heart Foundation. UK Factsheet April 2023 https://www.bhf.org.uk/-/media/files/for-professionals/research/heart-statistics/bhf-cvd-statistics-uk-factsheet.pdf (2023).
Public Health England. Cardiovascular Disease Profiles: May 2020 Update https://www.gov.uk/government/statistics/cardiovascular-disease-profiles-may-2020-update (2020).
Author information
Authors and Affiliations
Contributions
All the authors researched data for the article. A.T., D.K., N.T., R.H. and P.V. contributed substantially to discussion of the content. A.T., N.T. and P.V. wrote the article. All the authors reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Cardiology thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Institute for Health Metrics and Evaluation: https://www.healthdata.org/results/gbd_summaries/2019/ischaemic-heart-disease-level-3-cause
R Statistical Software: https://www.r-project.org
The World Bank. The World by Income and Region: https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html
UN grouping of countries by geographical regions: https://population.un.org/wpp/Download/Documentation/Documentation/
UN World Population Prospects: https://population.un.org/wpp/
WHO Global Health Observatory: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/3411
WHO International Classification of Diseases: https://www.who.int/standards/classifications/classification-of-diseases
WHO Mortality Database: https://www.who.int/data/data-collection-tools/who-mortality-database
WHO World Standard Population (2000–2025): https://seer.cancer.gov/stdpopulations/world.who.html
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Timmis, A., Kazakiewicz, D., Townsend, N. et al. Global epidemiology of acute coronary syndromes. Nat Rev Cardiol 20, 778–788 (2023). https://doi.org/10.1038/s41569-023-00884-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-023-00884-0
This article is cited by
-
Cost–utility analysis of using high-intensity statin among post-hospitalized acute coronary syndrome patients
The Egyptian Heart Journal (2024)