Abstract
Sodium–glucose cotransporter 2 (SGLT2) inhibitors reduce heart failure events by direct action on the failing heart that is independent of changes in renal tubular function. In the failing heart, nutrient transport into cardiomyocytes is increased, but nutrient utilization is impaired, leading to deficient ATP production and the cytosolic accumulation of deleterious glucose and lipid by-products. These by-products trigger downregulation of cytoprotective nutrient-deprivation pathways, thereby promoting cellular stress and undermining cellular survival. SGLT2 inhibitors restore cellular homeostasis through three complementary mechanisms: they might bind directly to nutrient-deprivation and nutrient-surplus sensors to promote their cytoprotective actions; they can increase the synthesis of ATP by promoting mitochondrial health (mediated by increasing autophagic flux) and potentially by alleviating the cytosolic deficiency in ferrous iron; and they might directly inhibit glucose transporter type 1, thereby diminishing the cytosolic accumulation of toxic metabolic by-products and promoting the oxidation of long-chain fatty acids. The increase in autophagic flux mediated by SGLT2 inhibitors also promotes the clearance of harmful glucose and lipid by-products and the disposal of dysfunctional mitochondria, allowing for mitochondrial renewal through mitochondrial biogenesis. This Review describes the orchestrated interplay between nutrient transport and metabolism and nutrient-deprivation and nutrient-surplus signalling, to explain how SGLT2 inhibitors reverse the profound nutrient, metabolic and cellular abnormalities observed in heart failure, thereby restoring the myocardium to a healthy molecular and cellular phenotype.
Key points
-
Sodium–glucose cotransporter 2 (SGLT2) inhibitors have a direct cytoprotective effect on the failing heart that is mediated by SGLT2-independent actions to increase nutrient-deprivation signalling and autophagic flux, thereby reducing cellular stress, promoting mitochondrial health and renewal, and decreasing pro-inflammatory signalling and apoptosis.
-
The failing heart is characterized by upregulation of glucose transporter type 1 (GLUT1) levels, increased glycolysis and impaired glucose oxidation, which lead to cytosolic accumulation of deleterious glucose intermediates that can activate mechanistic target of rapamycin (mTOR) and suppress nutrient-deprivation signalling.
-
The failing heart has increased uptake but decreased oxidation of long-chain fatty acids, which impairs ATP production and leads to cytosolic accumulation of deleterious lipid intermediates that result from impaired mitochondrial function and nutrient-deprivation signalling; the cytosolic accumulation of amino acids can promote the activation of mTOR.
-
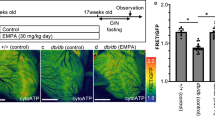
SGLT2 inhibitors reverse heart failure-related abnormalities in glucose, long-chain fatty acid and amino acid uptake and metabolism by inhibiting GLUT1 (potentially) and by promoting nutrient-deprivation signalling and restoring mitochondrial health and renewal, which increases nutrient oxidation and oxidative phosphorylation and reduces the cytosolic accumulation of deleterious glucose and lipid by-products.
-
The ketonaemia that accompanies SGLT2 inhibition does not act as an energy substrate for ATP production but might promote nutrient-deprivation signalling, reduce the activation of pro-inflammatory pathways and increase autophagic flux.
-
SGLT2 inhibitors might facilitate ATP and haemoglobin production by increasing the pool of bioreactive cytosolic Fe2+ as a result of the SGLT2 inhibitor-induced decrease in hepcidin and ferritin levels, thereby alleviating the state of inflammation-mediated functional iron deficiency that is observed in heart failure.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Giugliano, D. et al. SGLT-2 inhibitors and cardiorenal outcomes in patients with or without type 2 diabetes: a meta-analysis of 11 CVOTs. Cardiovasc. Diabetol. 20, 236 (2021).
Mordi, N. A. et al. Renal and cardiovascular effects of SGLT2 inhibition in combination with loop diuretics in patients with type 2 diabetes and chronic heart failure: the RECEDE-CHF trial. Circulation 142, 1713–1724 (2020).
Scholtes, R. A. et al. The adaptive renal response for volume homeostasis during 2 weeks of dapagliflozin treatment in people with type 2 diabetes and preserved renal function on a sodium-controlled diet. Kidney Int. Rep. 7, 1084–1092 (2022).
Zannad, F. et al. Effect of empagliflozin on circulating proteomics in heart failure: mechanistic insights from the EMPEROR program. Eur. Heart J. 10.1093eurheartj/ehac495 (2022).
Januzzi, J. L. Jr. et al. EMPEROR-reduced trial committees and investigators. Prognostic importance of NT-proBNP and effect of empagliflozin in the EMPEROR-reduced trial. J. Am. Coll. Cardiol. 78, 1321–1332 (2021).
Nassif, M. E. et al. Empagliflozin effects on pulmonary artery pressure in patients with heart failure: results from the EMBRACE-HF trial. Circulation 143, 1673–1686 (2021).
Omar, M. et al. Effect of empagliflozin on blood volume redistribution in patients with chronic heart failure and reduced ejection fraction: an analysis from the Empire HF randomized clinical trial. Circ. Heart Fail. 15, e009156 (2022).
Ferrannini, E. et al. Shift to fatty substrate utilization in response to sodium-glucose cotransporter 2 inhibition in subjects without diabetes and patients with type 2 diabetes. Diabetes 65, 1190–1195 (2016).
Petrie, M. C. et al. Effect of dapagliflozin on worsening heart failure and cardiovascular death in patients with heart failure with and without diabetes. JAMA 323, 1353–1368 (2020).
Sayour, A. A. et al. Characterization of left ventricular myocardial sodium-glucose cotransporter 1 expression in patients with end-stage heart failure. Cardiovasc. Diabetol. 19, 159 (2020).
Marfella, R. et al. Sodium-glucose cotransporter-2 (SGLT2) expression in diabetic and non-diabetic failing human cardiomyocytes. Pharmacol. Res. 184, 106448 (2022).
Packer, M. Critical reanalysis of the mechanisms underlying the cardiorenal benefits of SGLT2 inhibitors and reaffirmation of the nutrient deprivation signaling/autophagy hypothesis. Circulation 146, 1383–1405 (2022).
Packer, M. Cardioprotective effects of sirtuin-1 and its downstream effectors: potential role in mediating the heart failure benefits of SGLT2 (sodium-glucose cotransporter 2) inhibitors. Circ. Heart Fail. 13, e007197 (2020).
Vallon, V. & Nakagawa, T. Renal tubular handling of glucose and fructose in health and disease. Compr. Physiol. 12, 2995–3044 (2021).
Pessoa, T. D., Campos, L. C., Carraro-Lacroix, L., Girardi, A. C. & Malnic, G. Functional role of glucose metabolism, osmotic stress, and sodium-glucose cotransporter isoform-mediated transport on Na+/H+ exchanger isoform 3 activity in the renal proximal tubule. J. Am. Soc. Nephrol. 25, 2028–2039 (2014).
Li, X. et al. Direct cardiac actions of the sodium glucose co-transporter 2 inhibitor empagliflozin improve myocardial oxidative phosphorylation and attenuate pressure-overload heart failure. J. Am. Heart Assoc. 10, e018298 (2021).
Borges-Júnior, F. A. et al. Empagliflozin inhibits proximal tubule NHE3 activity, preserves GFR, and restores euvolemia in nondiabetic rats with induced heart failure. J. Am. Soc. Nephrol. 32, 1616–1629 (2021).
Baartscheer, A. et al. Empagliflozin decreases myocardial cytoplasmic Na+ through inhibition of the cardiac Na+/H+ exchanger in rats and rabbits. Diabetologia 60, 568–573 (2017).
Philippaert, K. et al. Cardiac late sodium channel current is a molecular target for the sodium/glucose cotransporter 2 inhibitor empagliflozin. Circulation 143, 2188–2204 (2021).
Mustroph, J. et al. Empagliflozin inhibits cardiac late sodium current by Ca/calmodulin-dependent kinase II. Circulation 146, 1259–1261 (2022).
Vila-Petroff, M. et al. Ca2+/calmodulin-dependent protein kinase II contributes to intracellular pH recovery from acidosis via Na+/H+ exchanger activation. J. Mol. Cell. Cardiol. 49, 106–112 (2010).
Wagner, S. et al. Reactive oxygen species-activated Ca/calmodulin kinase IIδ is required for late I(Na) augmentation leading to cellular Na and Ca overload. Circ. Res. 108, 555–565 (2011).
Chung, Y. J. et al. Off-target effects of sodium-glucose co-transporter 2 blockers: empagliflozin does not inhibit Na+/H+ exchanger-1 or lower [Na+]i in the heart. Cardiovasc. Res. 117, 2794–2806 (2021).
Baker, H. E. et al. Acute SGLT-2i treatment improves cardiac efficiency during myocardial ischemia independent of Na+/H+ exchanger-1. Int. J. Cardiol. 363, 138–148 (2022).
Moopanar, T. R. et al. AICAR inhibits the Na+/H+ exchanger in rat hearts–possible contribution to cardioprotection. Pflug. Arch. 453, 147–156 (2006).
Liao, W., Rao, Z., Wu, L., Chen, Y. & Li, C. Cariporide attenuates doxorubicin-induced cardiotoxicity in rats by inhibiting oxidative stress, inflammation and apoptosis partly through regulation of Akt/GSK-3β and Sirt1 signaling pathway. Front. Pharmacol. 13, 850053 (2022).
Gupta, A. et al. Creatine kinase-mediated improvement of function in failing mouse hearts provides causal evidence the failing heart is energy starved. J. Clin. Invest. 122, 291–302 (2012).
Gupta, A. & Houston, B. A comprehensive review of the bioenergetics of fatty acid and glucose metabolism in the healthy and failing heart in nondiabetic condition. Heart Fail. Rev. 22, 825–842 (2017).
Carley, A. N. et al. Short-chain fatty acids outpace ketone oxidation in the failing heart. Circulation 143, 1797–1808 (2021).
Murashige, D. et al. Comprehensive quantification of fuel use by the failing and nonfailing human heart. Science 370, 364–368 (2020).
Bedi, K. C. Jr et al. Evidence for intramyocardial disruption of lipid metabolism and increased myocardial ketone utilization in advanced human heart failure. Circulation 133, 706–716 (2016).
Ferrannini, E., Mark, M. & Mayoux, E. C. V. protection in the EMPA-REG OUTCOME trial: a “thrifty substrate” hypothesis. Diabetes Care 39, 1108–1114 (2016).
Klip, I. T. et al. Iron deficiency in chronic heart failure: an international pooled analysis. Am. Heart J. 165, 575–582 (2013).
Hoes, M. F. et al. Iron deficiency impairs contractility of human cardiomyocytes through decreased mitochondrial function. Eur. J. Heart Fail. 20, 910–919 (2018).
Docherty, K. F. et al. Iron deficiency in heart failure and effect of dapagliflozin: findings from DAPA-HF. Circulation 146, 980–994 (2022).
Sharma, S. et al. Intramyocardial lipid accumulation in the failing human heart resembles the lipotoxic rat heart. FASEB J. 18, 1692–1700 (2004).
Akkafa, F. et al. Reduced SIRT1 expression correlates with enhanced oxidative stress in compensated and decompensated heart failure. Redox Biol. 6, 169–173 (2015).
Wang, B. et al. AMPKα2 protects against the development of heart failure by enhancing mitophagy via PINK1 phosphorylation. Circ. Res. 122, 712–729 (2018).
Faerber, G. et al. Induction of heart failure by minimally invasive aortic constriction in mice: reduced peroxisome proliferator-activated receptor γ coactivator levels and mitochondrial dysfunction. J. Thorac. Cardiovasc. Surg. 141, 492–500 (2011).
Castillo, E. C. et al. Mitochondrial hyperacetylation in the failing hearts of obese patients mediated partly by a reduction in SIRT3: The involvement of the mitochondrial permeability transition pore. Cell Physiol. Biochem. 53, 465–479 (2019).
Yano, T. et al. Clinical impact of myocardial mTORC1 activation in nonischemic dilated cardiomyopathy. J. Mol. Cell Cardiol. 91, 6–9 (2016).
Zhang, D. et al. mTORC1 regulates cardiac function and myocyte survival through 4E-BP1 inhibition in mice. J. Clin. Invest. 120, 2805–2816 (2010).
Matsushima, S. & Sadoshima, J. The role of sirtuins in cardiac disease. Am. J. Physiol. Heart Circ. Physiol. 309, H1375–H1389 (2015).
Chen, L. et al. PGC-1α-mediated mitochondrial quality control: molecular mechanisms and implications for heart failure. Front. Cell Dev. Biol. 10, 871357 (2022).
Herzig, S. & Shaw, R. J. AMPK: guardian of metabolism and mitochondrial homeostasis. Nat. Rev. Mol. Cell Biol. 19, 121–135 (2018).
Gao, G. et al. Rapamycin regulates the balance between cardiomyocyte apoptosis and autophagy in chronic heart failure by inhibiting mTOR signaling. Int. J. Mol. Med. 45, 195–209 (2020).
Tomczyk, M. M. et al. Mitochondrial sirtuin-3 (SIRT3) prevents doxorubicin-induced dilated cardiomyopathy by modulating protein acetylation and oxidative stress. Circ. Heart Fail. 15, e008547 (2022).
Li, Y. et al. AMPK inhibits cardiac hypertrophy by promoting autophagy via mTORC1. Arch. Biochem. Biophys. 558, 79–86 (2014).
Pires Da Silva, J. et al. SIRT1 protects the heart from ER stress-induced injury by promoting eEF2K/eEF2-dependent autophagy. Cells 9, 426 (2020).
Zhang, T., Liu, C. F., Zhang, T. N., Wen, R. & Song, W. L. Overexpression of peroxisome proliferator-activated receptor γ coactivator 1-α protects cardiomyocytes from lipopolysaccharide-induced mitochondrial damage and apoptosis. Inflammation 43, 1806–1820 (2020).
Mizushima, N. & Levine, B. Autophagy in human diseases. N. Engl. J. Med. 383, 1564–1576 (2020).
Levine, B. & Kroemer, G. Biological functions of autophagy genes: a disease perspective. Cell 176, 11–42 (2019).
Lin, B. et al. Sirt1 improves heart failure through modulating the NF-κB p65/microRNA-155/BNDF signaling cascade. Aging 13, 14482–14498 (2020).
Han, Y. et al. SIRT1 agonism modulates cardiac NLRP3 inflammasome through pyruvate dehydrogenase during ischemia and reperfusion. Redox Biol. 34, 101538 (2020).
Chen, Y., He, T., Zhang, Z. & Zhang, J. Activation of SIRT1 by resveratrol alleviates pressure overload-induced cardiac hypertrophy via suppression of TGF-β1 signaling. Pharmacology 106, 667–681 (2021).
Packer, M. Role of deranged energy deprivation signaling in the pathogenesis of cardiac and renal disease in states of perceived nutrient overabundance. Circulation 141, 2095–2105 (2020).
Packer, M. SGLT2 inhibitors produce cardiorenal benefits by promoting adaptive cellular reprogramming to induce a state of fasting mimicry: a paradigm shift in understanding their mechanism of action. Diabetes Care 43, 508–511 (2020).
Ying, Y. et al. Phloretin protects against cardiac damage and remodeling via restoring SIRT1 and anti-inflammatory effects in the streptozotocin-induced diabetic mouse model. Aging 11, 2822–2835 (2019).
Koyani, C. N. et al. Empagliflozin protects heart from inflammation and energy depletion via AMPK activation. Pharmacol. Res. 158, 104870 (2020).
Lu, Q. et al. Empagliflozin attenuates ischemia and reperfusion injury through LKB1/AMPK signaling pathway. Mol. Cell Endocrinol. 501, 110642 (2020).
Wang, C. Y. et al. TLR9 binding to Beclin 1 and mitochondrial SIRT3 by a sodium-glucose co-transporter 2 inhibitor protects the heart from doxorubicin toxicity. Biology 9, 369 (2020).
Kondo, H. et al. Effects of canagliflozin on human myocardial redox signalling: clinical implications. Eur. Heart J. 42, 4947–4960 (2021).
Lee, C. C., Chen, W. T., Chen, S. Y. & Lee, T. M. Dapagliflozin attenuates arrhythmic vulnerabilities by regulating connexin43 expression via the AMPK pathway in post-infarcted rat hearts. Biochem. Pharmacol. 192, 114674 (2021).
Ren, F. F. et al. Dapagliflozin attenuates pressure overload-induced myocardial remodeling in mice via activating SIRT1 and inhibiting endoplasmic reticulum stress. Acta Pharmacol. Sin. 43, 1721–1732 (2022).
Ren, C. et al. Sodium-glucose cotransporter-2 inhibitor empagliflozin ameliorates sunitinib-induced cardiac dysfunction via regulation of AMPK-mTOR signaling pathway-mediated autophagy. Front. Pharmacol. 12, 664181 (2021).
Sun, P. et al. Canagliflozin attenuates lipotoxicity in cardiomyocytes and protects diabetic mouse hearts by inhibiting the mTOR/HIF-1α pathway. iScience 24, 102521 (2021).
Tian, G. et al. Empagliflozin alleviates ethanol-induced cardiomyocyte injury through inhibition of mitochondrial apoptosis via a SIRT1/PTEN/Akt pathway. Clin. Exp. Pharmacol. Physiol. 48, 837–845 (2021).
Yu, Y. W. et al. Sodium-glucose co-transporter-2 inhibitor of dapagliflozin attenuates myocardial ischemia/reperfusion injury by limiting NLRP3 inflammasome activation and modulating autophagy. Front. Cardiovasc. Med. 8, 768214 (2022).
He, L. et al. An effective sodium-dependent glucose transporter 2 inhibition, canagliflozin, prevents development of hypertensive heart failure in Dahl salt-sensitive rats. Front. Pharmacol. 13, 856386 (2022).
Aragón-Herrera, A. et al. Empagliflozin reduces the levels of CD36 and cardiotoxic lipids while improving autophagy in the hearts of Zucker diabetic fatty rats. Biochem. Pharmacol. 170, 113677 (2019).
Li, X. et al. Direct cardiac actions of sodium-glucose cotransporter 2 inhibition improve mitochondrial function and attenuate oxidative stress in pressure overload-induced heart failure. Front. Cardiovasc. Med. 9, 859253 (2022).
Packer, M. Mutual antagonism of hypoxia-inducible factor isoforms in cardiac, vascular, and renal disorders. JACC Basic Transl. Sci. 5, 961–968 (2020).
Chen, R. et al. The acetylase/deacetylase couple CREB-binding protein/sirtuin 1 controls hypoxia-inducible factor 2 signaling. J. Biol. Chem. 287, 30800–30811 (2012).
He, X. et al. Endothelial specific SIRT3 deletion impairs glycolysis and angiogenesis and causes diastolic dysfunction. J. Mol. Cell Cardiol. 112, 104–113 (2017).
Yang, Z. et al. SGLT2 inhibitor dapagliflozin attenuates cardiac fibrosis and inflammation by reverting the HIF-2α signaling pathway in arrhythmogenic cardiomyopathy. FASEB J. 36, e22410 (2022).
Fitchett, D. et al. Mediators of the improvement in heart failure outcomes with empagliflozin in the EMPA-REG OUTCOME trial. ESC. Heart Fail. 8, 4517–4527 (2021).
Umino, H. et al. High basolateral glucose increases sodium-glucose cotransporter 2 and reduces sirtuin-1 in renal tubules through glucose transporter-2 detection. Sci. Rep. 8, 6791 (2018).
Wicik, Z. et al. Characterization of the SGLT2 interaction network and its regulation by SGLT2 inhibitors: a bioinformatic analysis. Front. Pharmacol. 13, 901340 (2022).
Lopaschuk, G. D., Karwi, Q. G., Tian, R., Wende, A. R. & Abel, E. D. Cardiac energy metabolism in heart failure. Circ. Res. 128, 1487–1513 (2021).
Mohamed, T. M. A., Abouleisa, R. & Hill, B. G. Metabolic determinants of cardiomyocyte proliferation. Stem Cell 40, 458–467 (2022).
Shin, A. N. et al. SIRT1 increases cardiomyocyte binucleation in the heart development. Oncotarget 9, 7996–8010 (2018).
Garbern, J. C. et al. Inhibition of mTOR signaling enhances maturation of cardiomyocytes derived from human-induced pluripotent stem cells via p53-induced quiescence. Circulation 141, 285–300 (2020).
Zhang, P., Shan, T., Liang, X., Deng, C. & Kuang, S. Mammalian target of rapamycin is essential for cardiomyocyte survival and heart development in mice. Biochem. Biophys. Res. Commun. 452, 53–59 (2014).
Sánchez-Díaz, M., Nicolás-Ávila, J. Á., Cordero, M. D. & Hidalgo, A. Mitochondrial adaptations in the growing heart. Trends Endocrinol. Metab. 31, 308–319 (2020).
Lehman, J. J. & Kelly, D. P. Transcriptional activation of energy metabolic switches in the developing and hypertrophied heart. Clin. Exp. Pharmacol. Physiol. 29, 339–345 (2002).
Gong, G. et al. Parkin-mediated mitophagy directs perinatal cardiac metabolic maturation in mice. Science 350, aad2459 (2015).
Kantor, P. F., Robertson, M. A., Coe, J. Y. & Lopaschuk, G. D. Volume overload hypertrophy of the newborn heart slows the maturation of enzymes involved in the regulation of fatty acid metabolism. J. Am. Coll. Cardiol. 33, 1724–1734 (1999).
Bertrand, L. et al. Glucose transporters in cardiovascular system in health and disease. Pflug. Arch. 472, 1385–1399 (2020).
Heilig, C. W. et al. Glucose transporter-1-deficient mice exhibit impaired development and deformities that are similar to diabetic embryopathy. Proc. Natl Acad. Sci. USA 100, 15613–15618 (2003).
Nisr, R. B. & Affouritit, C. Insulin acutely improves mitochondrial function of rat and human skeletal muscle by increasing coupling efficiency of oxidative phosphorylation. Biochim. Biophys. Acta 1837, 270–276 (2014).
Kato, T. et al. Analysis of metabolic remodeling in compensated left ventricular hypertrophy and heart failure. Circ. Heart Fail. 3, 420–430 (2010).
Pereira, R. O. et al. Inducible overexpression of GLUT1 prevents mitochondrial dysfunction and attenuates structural remodeling in pressure overload but does not prevent left ventricular dysfunction. J. Am. Heart Assoc. 2, e000301 (2013).
Fillmore, N. et al. Uncoupling of glycolysis from glucose oxidation accompanies the development of heart failure with preserved ejection fraction. Mol. Med. 24, 3 (2018).
Zhabyeyev, P. et al. Pressure-overload-induced heart failure induces a selective reduction in glucose oxidation at physiological afterload. Cardiovasc. Res. 97, 676–685 (2013).
Kutsche, H. S. et al. Alterations in glucose metabolism during the transition to heart failure: the contribution of UCP-2. Cells 9, 552 (2020).
Diakos, N. A. et al. Evidence of glycolysis up‐regulation and pyruvate mitochondrial oxidation mismatch during mechanical unloading of the failing human heart: implications for cardiac reloading and conditioning. JACC Basic Transl. Sci. 1, 432–444 (2016).
Bhaskar, P. T. et al. mTORC1 hyperactivity inhibits serum deprivation-induced apoptosis via increased hexokinase II and GLUT1 expression, sustained Mcl-1 expression, and glycogen synthase kinase 3beta inhibition. Mol. Cell Biol. 29, 5136–5147 (2009).
Sokolovska, J. et al. Influence of metformin on GLUT1 gene and protein expression in rat streptozotocin diabetes mellitus model. Arch. Physiol. Biochem. 116, 137–145 (2010).
Hölscher, M. et al. Unfavourable consequences of chronic cardiac HIF-1α stabilization. Cardiovasc. Res. 94, 77–86 (2012).
Yang, J. & Holman, G. D. Long-term metformin treatment stimulates cardiomyocyte glucose transport through an AMP-activated protein kinase-dependent reduction in GLUT4 endocytosis. Endocrinology 147, 2728–2736 (2006).
Li, X. et al. Enhancement of glucose metabolism via PGC-1α participates in the cardioprotection of chronic intermittent hypobaric hypoxia. Front. Physiol. 7, 219 (2016).
Murugasamy, K., Munjal, A. & Sundaresan, N. R. Emerging roles of SIRT3 in cardiac metabolism. Front. Cardiovasc. Med. 9, 850340 (2022).
Bersin, R. M. et al. Improved hemodynamic function and mechanical efficiency in congestive heart failure with sodium dichloroacetate. J. Am. Coll. Cardiol. 23, 1617–1624 (1994).
Clanachan, A. S. Contribution of protons to post-ischemic Na+ and Ca2+ overload and left ventricular mechanical dysfunction. J. Cardiovasc. Electrophysiol. 17, S141–S148 (2006).
Chen, Z. T. et al. Glycolysis inhibition alleviates cardiac fibrosis after myocardial infarction by suppressing cardiac fibroblast activation. Front. Cardiovasc. Med. 8, 701745 (2021).
Zheng, Z. et al. Enhanced glycolytic metabolism contributes to cardiac dysfunction in polymicrobial sepsis. J. Infect. Dis. 215, 1396–1406 (2017).
Sen, S. et al. Glucose regulation of load-induced mTOR signaling and ER stress in mammalian heart. J. Am. Heart Assoc. 2, e004796 (2013).
Roberts, D. J. & Miyamoto, S. Hexokinase II integrates energy metabolism and cellular protection: Akting on mitochondria and TORCing to autophagy. Cell Death Differ. 22, 248–257 (2015).
Tran, D. H. et al. Chronic activation of hexosamine biosynthesis in the heart triggers pathological cardiac remodeling. Nat. Commun. 11, 1771 (2020).
Marsh, S. A., Powell, P. C., Dell’italia, L. J. & Chatham, J. C. Cardiac O-GlcNAcylation blunts autophagic signaling in the diabetic heart. Life Sci. 92, 648–656 (2013).
Gelinas, R. et al. AMPK activation counteracts cardiac hypertrophy by reducing O-GlcNAcylation. Nat. Commun. 9, 374 (2018).
Chai, Q. et al. Knockdown of SGLT1 prevents the apoptosis of cardiomyocytes induced by glucose fluctuation via relieving oxidative stress and mitochondrial dysfunction. Biochem. Cell Biol. 99, 356–363 (2021).
Ferté, L. et al. New insight in understanding the contribution of SGLT1 in cardiac glucose uptake: evidence for a truncated form in mice and humans. Am. J. Physiol. Heart Circ. Physiol. 320, H838–H853 (2021).
Bhatt, D. L. et al. SOLOIST-WHF trial investigators. Sotagliflozin in patients with diabetes and recent worsening heart failure. N. Engl. J. Med. 384, 117–128 (2021).
Santos-Gallego, C. G. et al. Empagliflozin ameliorates adverse left ventricular remodeling in nondiabetic heart failure by enhancing myocardial energetics. J. Am. Coll. Cardiol. 73, 1931–1944 (2019).
Lauritsen, K. M. et al. SGLT2 inhibition does not affect myocardial fatty acid oxidation or uptake, but reduces myocardial glucose uptake and blood flow in individuals with type 2 diabetes: a randomized double-blind, placebo-controlled crossover trial. Diabetes 70, 800–808 (2021).
Asrih, M., Lerch, R., Papageorgiou, I., Pellieux, C. & Montessuit, C. Differential regulation of stimulated glucose transport by free fatty acids and PPARα or -δ agonists in cardiac myocytes. Am. J. Physiol. Endocrinol. Metab. 302, E872–E884 (2012).
Yurista, S. R. et al. Sodium-glucose co-transporter 2 inhibition with empagliflozin improves cardiac function in non-diabetic rats with left ventricular dysfunction after myocardial infarction. Eur. J. Heart Fail. 21, 862–873 (2019).
Zhang, H. et al. Empagliflozin decreases lactate generation in an NHE-1 dependent fashion and increases α-ketoglutarate synthesis from palmitate in type ii diabetic mouse hearts. Front. Cardiovasc. Med. 7, 592233 (2020).
Verma, S. et al. Empagliflozin increases cardiac energy production in diabetes: novel translational insights into the heart failure benefits of SGLT2 inhibitors. JACC Basic Transl. Sci. 3, 575–587 (2018).
Xie, B. et al. Empagliflozin restores cardiac metabolic flexibility in diet-induced obese C57BL6/J mice. Curr. Res. Physiol. 5, 232–239 (2022).
Uthman, L. et al. Novel anti-inflammatory effects of canagliflozin involving hexokinase II in lipopolysaccharide-stimulated human coronary artery endothelial cells. Cardiovasc. Drugs Ther. 35, 1083–1094 (2021).
Joubert, M. et al. The sodium-glucose cotransporter 2 inhibitor dapagliflozin prevents cardiomyopathy in a diabetic lipodystrophic mouse model. Diabetes 66, 1030–1040 (2017).
Ducheix, S., Magré, J., Cariou, B. & Prieur, X. Chronic O-GlcNAcylation and diabetic cardiomyopathy: the bitterness of glucose. Front. Endocrinol. 9, 642 (2018).
Hawley, S. A. et al. The Na+/glucose cotransporter inhibitor canagliflozin activates AMPK by inhibiting mitochondrial function and increasing cellular AMP levels. Diabetes 65, 2784–2794 (2016).
Karlstaedt, A., Khanna, R., Thangam, M. & Taegtmeyer, H. Glucose 6-phosphate accumulates via phosphoglucose isomerase inhibition in heart muscle. Circ. Res. 126, 60–74 (2020).
Davogustto, G. E. et al. Metabolic remodeling precedes mTORC1-mediated cardiac hypertrophy. Mol. Cell Cardiol. 158, 115–127 (2021).
Roberts, D. J., Tan-Sah, V. P., Ding, E. Y., Smith, J. M. & Miyamoto, S. Hexokinase-II positively regulates glucose starvation-induced autophagy through TORC1 inhibition. Mol. Cell 53, 521–533 (2014).
Brainard, R. E. & Facundo, H. T. Cardiac hypertrophy drives PGC-1α suppression associated with enhanced O-glycosylation. Biochim. Biophys. Acta Mol. Basis Dis. 1867, 166080 (2021).
Bullen, J. W. et al. Cross-talk between two essential nutrient-sensitive enzymes: O-GlcNAc transferase (OGT) and AMP-activated protein kinase (AMPK). J. Biol. Chem. 289, 10592–10606 (2014).
Luiken, J. J. F. P., Nabben, M., Neumann, D. & Glatz, J. F. C. Understanding the distinct subcellular trafficking of CD36 and GLUT4 during the development of myocardial insulin resistance. Biochim. Biophys. Acta Mol. Basis Dis. 1866, 165775 (2020).
van der Vusse, G. J., van Bilsen, M., Glatz, J. F., Hasselbaink, D. M. & Luiken, J. J. Critical steps in cellular fatty acid uptake and utilization. Mol. Cell Biochem. 239, 9–15 (2002).
Sorokina, N. et al. Recruitment of compensatory pathways to sustain oxidative flux with reduced carnitine palmitoyltransferase I activity characterizes inefficiency in energy metabolism in hypertrophied hearts. Circulation 115, 2033–2041 (2007).
Warren, J. S. et al. Histone methyltransferase Smyd1 regulates mitochondrial energetics in the heart. Proc. Natl Acad. Sci. USA 115, E7871–E7880 (2018).
Fukushima, A. & Lopaschuk, G. D. Cardiac fatty acid oxidation in heart failure associated with obesity and diabetes. Biochim. Biophys. Acta 1861, 1525–1534 (2016).
Osorio, J. C. et al. Impaired myocardial fatty acid oxidation and reduced protein expression of retinoid x receptor-alpha in pacing-induced heart failure. Circulation 106, 606–612 (2002).
Doenst, T. et al. Decreased rates of substrate oxidation ex vivo predict the onset of heart failure and contractile dysfunction in rats with pressure overload. Cardiovasc. Res. 86, 461–470 (2010).
Choi, Y. S. et al. Preservation of myocardial fatty acid oxidation prevents diastolic dysfunction in mice subjected to angiotensin II infusion. J. Mol. Cell Cardiol. 100, 64–71 (2016).
Law, B. A. et al. Lipotoxic very-long-chain ceramides cause mitochondrial dysfunction, oxidative stress, and cell death in cardiomyocytes. FASEB J. 32, 1403–1416 (2018).
Hunter, W. G. et al. Metabolomic profiling identifies novel circulating biomarkers of mitochondrial dysfunction differentially elevated in heart failure with preserved versus reduced ejection fraction: evidence for shared metabolic impairments in clinical heart failure. J. Am. Heart Assoc. 5, e003190 (2016).
Gupte, A. A. et al. Mechanical unloading promotes myocardial energy recovery in human heart failure. Circ. Cardiovasc. Genet. 7, 266–276 (2014).
Previs, M. J. et al. Defects in the proteome and metabolome in human hypertrophic cardiomyopathy. Circ. Heart Fail. 15, e009521 (2022).
Dávila-Román, V. G. et al. Altered myocardial fatty acid and glucose metabolism in idiopathic dilated cardiomyopathy. J. Am. Coll. Cardiol. 40, 271–277 (2002).
Yan, J. et al. Increased glucose uptake and oxidation in mouse hearts prevent high fatty acid oxidation but cause cardiac dysfunction in diet-induced obesity. Circulation 119, 2818–2828 (2009).
Heather, L. C. et al. Fatty acid transporter levels and palmitate oxidation rate correlate with ejection fraction in the infarcted rat heart. Cardiovasc. Res. 72, 430–437 (2006).
Sihag, S., Cresci, S., Li, A. Y., Sucharov, C. C. & Lehman, J. J. PGC-1alpha and ERRalpha target gene downregulation is a signature of the failing human heart. J. Mol. Cell Cardiol. 46, 201–212 (2009).
Knuuti, J. & Opie, L. H. The adrenergic-fatty acid load in heart failure. J. Am. Coll. Cardiol. 54, 1637–1646 (2009).
Pohl, J. et al. Fatty acid transporters in plasma membranes of cardiomyocytes in patients with dilated cardiomyopathy. Eur. J. Med. Res. 5, 438–442 (2000).
Goldberg, I. J., Trent, C. M. & Schulze, C. Lipid metabolism and toxicity in the heart. Cell Metab. 15, 805–812 (2012).
Wu, Y., Song, P., Xu, J., Zhang, M. & Zou, M. H. Activation of protein phosphatase 2A by palmitate inhibits AMP-activated protein kinase. J. Biol. Chem. 282, 9777–9788 (2007).
Smolka, C. et al. Cardiomyocyte-specific miR-100 overexpression preserves heart function under pressure overload in mice and diminishes fatty acid uptake as well as ROS production by direct suppression of Nox4 and CD36. FASEB J. 35, e21956 (2021).
He, L. et al. Carnitine palmitoyltransferase-1b deficiency aggravates pressure overload-induced cardiac hypertrophy caused by lipotoxicity. Circulation 126, 1705–1716 (2012).
Kolwicz, S. C. Jr. et al. Cardiac-specific deletion of acetyl CoA carboxylase 2 prevents metabolic remodeling during pressure-overload hypertrophy. Circ. Res. 111, 728–738 (2012).
Shao, D. et al. Increasing fatty acid oxidation prevents high-fat diet-induced cardiomyopathy through regulating Parkin-mediated mitophagy. Circulation 142, 983–997 (2020).
Huang, W. P. et al. Fenofibrate attenuates doxorubicin-induced cardiac dysfunction in mice via activating the eNOS/EPC pathway. Sci. Rep. 11, 1159 (2021).
Brigadeau, F. et al. The PPARalpha activator fenofibrate slows down the progression of the left ventricular dysfunction in porcine tachycardia-induced cardiomyopathy. J. Cardiovasc. Pharmacol. 49, 408–415 (2007).
Zhang, J. et al. Fenofibrate increases cardiac autophagy via FGF21/SIRT1 and prevents fibrosis and inflammation in the hearts of type 1 diabetic mice. Clin. Sci. 130, 625–641 (2016).
Ferreira, J. P. et al. Fenofibrate and heart failure outcomes in patients with type 2 diabetes: analysis from ACCORD. Diabetes Care 45, 1584–1591 (2022).
Supruniuk, E., Mikłosz, A. & Chabowski, A. The implication of PGC-1α on fatty acid transport across plasma and mitochondrial membranes in the insulin sensitive tissues. Front. Physiol. 8, 923 (2017).
Wang, S. Y. et al. Exercise enhances cardiac function by improving mitochondrial dysfunction and maintaining energy homoeostasis in the development of diabetic cardiomyopathy. J. Mol. Med. 98, 245–261 (2020).
Hirschey, M. D. et al. SIRT3 regulates mitochondrial fatty-acid oxidation by reversible enzyme deacetylation. Nature 464, 121–125 (2010).
Wen, D. T. et al. Endurance exercise resistance to lipotoxic cardiomyopathy is associated with cardiac NAD+/dSIR2/PGC-1α pathway activation in old Drosophila. Biol. Open. 8, bio044719 (2019).
Chen, T. et al. Mouse SIRT3 attenuates hypertrophy-related lipid accumulation in the heart through the deacetylation of LCAD. PLoS One 10, e0118909 (2015).
Turdi, S. et al. Deficiency in AMP-activated protein kinase exaggerates high fat diet-induced cardiac hypertrophy and contractile dysfunction. J. Mol. Cell Cardiol. 50, 712–722 (2011).
Sambandam, N. et al. Malonyl-CoA decarboxylase (MCD) is differentially regulated in subcellular compartments by 5’AMP-activated protein kinase (AMPK). Studies using H9c2 cells overexpressing MCD and AMPK by adenoviral gene transfer technique. Eur. J. Biochem. 271, 2831–2840 (2004).
Bai, F. et al. Metformin regulates lipid metabolism in a canine model of atrial fibrillation through AMPK/PPAR-α/VLCAD pathway. Lipids Health Dis. 18, 109 (2019).
Viglino, C., Foglia, B. & Montessuit, C. Chronic AICAR treatment prevents metabolic changes in cardiomyocytes exposed to free fatty acids. Pflug. Arch. 471, 1219–1234 (2019).
Adrian, L. et al. AMPK prevents palmitic acid-induced apoptosis and lipid accumulation in cardiomyocytes. Lipids 52, 737–750 (2017).
Pettersen, I. K. N. et al. Upregulated PDK4 expression is a sensitive marker of increased fatty acid oxidation. Mitochondrion 49, 97–110 (2019).
Zhu, Y. et al. Regulation of fatty acid metabolism by mTOR in adult murine hearts occurs independently of changes in PGC-1α. Am. J. Physiol. Heart Circ. Physiol. 305, H41–H51 (2013).
Moellmann, J. et al. The sodium-glucose co-transporter-2 inhibitor ertugliflozin modifies the signature of cardiac substrate metabolism and reduces cardiac mTOR signalling, endoplasmic reticulum stress and apoptosis. Diabetes Obes. Metab. 24, 2263–2272 (2022).
Wei, D. et al. Canagliflozin ameliorates obesity by improving mitochondrial function and fatty acid oxidation via PPARα in vivo and in vitro. Life Sci. 247, 117414 (2020).
Ferrannini, E. et al. Mechanisms of sodium-glucose cotransporter 2 inhibition: insights from large-scale proteomics. Diabetes Care 43, 2183–2189 (2020).
Furuhashi, M. et al. Possible increase in serum FABP4 level despite adiposity reduction by canagliflozin, an SGLT2 inhibitor. PLoS ONE 11, e0154482 (2016).
Grevengoed, T. J., Cooper, D. E., Young, P. A., Ellis, J. M. & Coleman, R. A. Loss of long-chain acyl-CoA synthetase isoform 1 impairs cardiac autophagy and mitochondrial structure through mechanistic target of rapamycin complex 1 activation. FASEB J. 29, 4641–4653 (2015).
Crozier, S. J., Bolster, D. R., Reiter, A. K., Kimball, S. R. & Jefferson, L. S. Beta -oxidation of free fatty acids is required to maintain translational control of protein synthesis in heart. Am. J. Physiol. Endocrinol. Metab. 283, E1144–E1150 (2002).
Essop, M. F. et al. Reduced heart size and increased myocardial fuel substrate oxidation in ACC2 mutant mice. Am. J. Physiol. Heart Circ. Physiol. 295, H256–H265 (2008).
Xiao, X. et al. Peroxisome proliferator-activated receptors gamma and alpha agonists stimulate cardiac glucose uptake via activation of AMP-activated protein kinase. J. Nutr. Biochem. 21, 621–626 (2010).
Liu, G. Z. et al. Fenofibrate inhibits atrial metabolic remodelling in atrial fibrillation through PPAR-α/sirtuin 1/PGC-1α pathway. Br. J. Pharmacol. 173, 1095–1109 (2016).
Witham, W. G., Yester, K. A. & McGaffin, K. R. A high leucine diet mitigates cardiac injury and improves survival after acute myocardial infarction. Metabolism 62, 290–302 (2013).
Kaye, D. M., Parnell, M. M. & Ahlers, B. A. Reduced myocardial and systemic L-arginine uptake in heart failure. Circ. Res. 91, 1198–1203 (2002).
Kimura, Y. et al. Usefulness of plasma branched-chain amino acid analysis in predicting outcomes of patients with nonischemic dilated cardiomyopathy. Int. Heart J. 61, 739–747 (2020).
Sansbury, B. E. et al. Metabolomic analysis of pressure-overloaded and infarcted mouse hearts. Circ. Heart Fail. 7, 634–642 (2014).
Uddin, G. M. et al. Impaired branched chain amino acid oxidation contributes to cardiac insulin resistance in heart failure. Cardiovasc. Diabetol. 18, 86 (2019).
Sun, H. et al. Catabolic defect of branched-chain amino acids promotes heart failure. Circulation 133, 2038–2049 (2016).
Caragnano, A. et al. Autophagy and inflammasome activation in dilated cardiomyopathy. J. Clin. Med. 8, 1519 (2019).
Shao, D. et al. Glucose promotes cell growth by suppressing branched-chain amino acid degradation. Nat. Commun. 9, 2935 (2018).
Wang, W. et al. Defective branched chain amino acid catabolism contributes to cardiac dysfunction and remodeling following myocardial infarction. Am. J. Physiol. Heart Circ. Physiol. 311, H1160–H1169 (2016).
Renguet, E. et al. Metabolism and acetylation contribute to leucine-mediated inhibition of cardiac glucose uptake. Am. J. Physiol. Heart Circ. Physiol. 313, H432–H445 (2017).
Gong, Q. et al. SGLT2 inhibitor-empagliflozin treatment ameliorates diabetic retinopathy manifestations and exerts protective effects associated with augmenting branched chain amino acids catabolism and transportation in db/db mice. Biomed. Pharmacother. 152, 113222 (2022).
Kappel, B. A. et al. Effect of empagliflozin on the metabolic signature of patients with type 2 diabetes mellitus and cardiovascular disease. Circulation 136, 969–972 (2017).
Palm, C. L., Nijholt, K. T., Bakker, B. M. & Westenbrink, B. D. Short-chain fatty acids in the metabolism of heart failure - rethinking the fat stigma. Front. Cardiovasc. Med. 9, 915102 (2022).
Sun, W. et al. Alterations of the gut microbiota in patients with severe chronic heart failure. Front. Microbiol. 12, 813289 (2022).
Jóhannsson, E. et al. Upregulation of the cardiac monocarboxylate transporter MCT1 in a rat model of congestive heart failure. Circulation 104, 729–734 (2001).
Zhang, L. et al. Sodium butyrate attenuates angiotensin II-induced cardiac hypertrophy by inhibiting COX2/PGE2 pathway via a HDAC5/HDAC6-dependent mechanism. J. Cell Mol. Med. 23, 8139–8150 (2019).
Hallows, W. C., Lee, S. & Denu, J. M. Sirtuins deacetylate and activate mammalian acetyl-CoA synthetases. Proc. Natl Acad. Sci. USA 103, 10230–10235 (2006).
Zhu, Y., Wu, J. & Yuan, S. Y. MCT1 and MCT4 expression during myocardial ischemic-reperfusion injury in the isolated rat heart. Cell Physiol. Biochem. 32, 663–674 (2013).
Zeng, Z. et al. Effects of short-chain acyl-CoA dehydrogenase on cardiomyocyte apoptosis. J. Cell Mol. Med. 20, 1381–1391 (2016).
Saucedo-Orozco, H., Voorrips, S. N., Yurista, S. R., de Boer, R. A. & Westenbrink, B. D. SGLT2 inhibitors and ketone metabolism in heart failure. J. Lipid Atheroscler. 11, 1–19 (2022).
Lommi, J. et al. Blood ketone bodies in congestive heart failure. J. Am. Coll. Cardiol. 28, 665–672 (1996).
Nagao, M. et al. β-Hydroxybutyrate elevation as a compensatory response against oxidative stress in cardiomyocytes. Biochem. Biophys. Res. Commun. 475, 322–328 (2016).
Nielsen, R. et al. Cardiovascular effects of treatment with the ketone body 3-hydroxybutyrate in chronic heart failure patients. Circulation 139, 2129–2141 (2019).
Yurista, S. R. et al. Ketone ester treatment improves cardiac function and reduces pathologic remodeling in preclinical models of heart failure. Circ. Heart Fail. 14, e007684 (2021).
Horton, J. L. et al. The failing heart utilizes 3-hydroxybutyrate as a metabolic stress defense. JCI Insight 4, e124079 (2019).
Ho, K. L. et al. Increased ketone body oxidation provides additional energy for the failing heart without improving cardiac efficiency. Cardiovasc. Res. 115, 1606–1616 (2019).
Uchihashi, M. et al. Cardiac-specific Bdh1 overexpression ameliorates oxidative stress and cardiac remodeling in pressure overload-induced heart failure. Circ. Heart Fail. 10, e004417 (2017).
Byrne, N. J. et al. Chronically elevating circulating ketones can reduce cardiac inflammation and blunt the development of heart failure. Circ. Heart Fail. 13, e006573 (2020).
Deng, Y. et al. Targeting mitochondria-inflammation circuit by β-hydroxybutyrate mitigates HFpEF. Circ. Res. 128, 232–245 (2021).
Liu, Y. et al. Cardioprotective roles of β-hydroxybutyrate against doxorubicin induced cardiotoxicity. Front. Pharmacol. 11, 603596 (2021).
Nakamura, M. et al. Dietary carbohydrates restriction inhibits the development of cardiac hypertrophy and heart failure. Cardiovasc. Res. 117, 2365–2376 (2021).
Oka, S. I. et al. β-Hydroxybutyrate, a ketone body, potentiates the antioxidant defense via thioredoxin 1 upregulation in cardiomyocytes. Antioxid 10, 1153 (2021).
Kawakami, R. et al. Ketone body and FGF21 coordinately regulate fasting-induced oxidative stress response in the heart. Sci. Rep. 12, 7338 (2022).
Xu, M. et al. Choline ameliorates cardiac hypertrophy by regulating metabolic remodelling and UPRmt through SIRT3-AMPK pathway. Cardiovasc. Res. 115, 530–545 (2019).
Thai, P. N. et al. Ketone ester D-β-hydroxybutyrate-(R)-1,3 butanediol prevents decline in cardiac function in type 2 diabetic mice. J. Am. Heart Assoc. 10, e020729 (2021).
Nilsson, M. I. et al. Nutritional co-therapy with 1,3-butanediol and multi-ingredient antioxidants enhances autophagic clearance in Pompe disease. Mol. Genet Metab. 137, 228–240 (2022).
Wallenius, K. et al. The SGLT2 inhibitor dapagliflozin promotes systemic FFA mobilization, enhances hepatic β-oxidation, and induces ketosis. J. Lipid Res. 63, 100176 (2022).
Wolf, P. et al. Gluconeogenesis, but not glycogenolysis, contributes to the increase in endogenous glucose production by SGLT-2 inhibition. Diabetes Care 44, 541–548 (2021).
Yang, X. et al. The diabetes medication canagliflozin promotes mitochondrial remodelling of adipocyte via the AMPK-Sirt1-Pgc-1α signalling pathway. Adipocyte 9, 484–494 (2020).
Swe, M. T. et al. Dapagliflozin not only improves hepatic injury and pancreatic endoplasmic reticulum stress, but also induces hepatic gluconeogenic enzymes expression in obese rats. Clin. Sci. 133, 2415–2430 (2019).
Erion, D. M. et al. SirT1 knockdown in liver decreases basal hepatic glucose production and increases hepatic insulin responsiveness in diabetic rats. Proc. Natl Acad. Sci. USA 106, 11288–11293 (2009).
Hirschey, M. D., Shimazu, T., Capra, J. A., Pollard, K. S. & Verdin, E. SIRT1 and SIRT3 deacetylate homologous substrates: AceCS1,2 and HMGCS1,2. Aging 3, 635–642 (2011).
Velasco, G., Geelen, M. J. H. & Guzmán, M. Control of hepatic fatty acid oxidation by 5′-AMP-activated protein kinase involves a malonyl-CoA-dependent and a malonyl-CoA-independent mechanism. Arch. Biochem. Biophys. 337, 169–175 (1997).
Sengupta, S., Peterson, T. R., Laplante, M., Oh, S. & Sabatini, D. M. mTORC1 controls fasting-induced ketogenesis and its modulation by ageing. Nature 468, 1100–1104 (2010).
McCarthy, C. G. et al. Ketone body β-hydroxybutyrate is an autophagy-dependent vasodilator. JCI Insight 6, e149037 (2021).
Ferrannini, E. et al. Renal handling of ketones in response to sodium-glucose cotransporter 2 inhibition in patients with type 2 diabetes. Diabetes Care 40, 771–776 (2017).
Heerspink, H. J. L. et al. DAPA-CKD trial committees and investigators. Dapagliflozin in patients with chronic kidney disease. N. Engl. J. Med. 383, 1436–1446 (2020).
Sahasrabudhe, V. et al. The effect of renal impairment on the pharmacokinetics and pharmacodynamics of ertugliflozin in subjects with type 2 diabetes mellitus. J. Clin. Pharmacol. 57, 1432–1443 (2017).
Pietschner, R. et al. Effect of empagliflozin on ketone bodies in patients with stable chronic heart failure. Cardiovasc. Diabetol. 20, 219 (2021).
Selvaraj, S. et al. Metabolomic profiling of the effects of dapagliflozin in heart failure with reduced ejection fraction: DEFINE-HF. Circulation 146, 808–818 (2022).
Marilly, E. et al. SGLT2 inhibitors in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials balancing their risks and benefits. Diabetologia 65, 2000–2010 (2022).
Packer, M. et al. EMPEROR-reduced trial investigators. Cardiovascular and renal outcomes with empagliflozin in heart failure. N. Engl. J. Med. 383, 1413–1424 (2020).
Oh, C. M. et al. Cardioprotective potential of an SGLT2 inhibitor against doxorubicin-induced heart failure. Korean Circ. J. 49, 1183–1195 (2019).
Byrne, N. J. et al. Empagliflozin prevents worsening of cardiac function in an experimental model of pressure overload-induced heart failure. JACC Basic Transl. Sci. 2, 347–354 (2017).
Abdurrachim, D. et al. Empagliflozin reduces myocardial ketone utilization while preserving glucose utilization in diabetic hypertensive heart disease: a hyperpolarized 13C magnetic resonance spectroscopy study. Diabetes Obes. Metab. 21, 357–365 (2019).
Kimura, T. et al. Inhibitory effects of tofogliflozin on cardiac hypertrophy in Dahl salt-sensitive and salt-resistant rats fed a high-fat diet. Int. Heart J. 60, 728–735 (2019).
Gaborit, B. et al. Effect of empagliflozin on ectopic fat stores and myocardial energetics in type 2 diabetes: the EMPACEF study. Cardiovasc. Diabetol. 20, 57 (2021).
Tomita, I. et al. SGLT2 inhibition mediates protection from diabetic kidney disease by promoting ketone body-induced mTORC1 inhibition. Cell Metab. 32, 404–419.e6 (2020).
Papalia, F. et al. Cardiac energetics in patients with chronic heart failure and iron deficiency: an in-vivo 31P magnetic resonance spectroscopy study. Eur. J. Heart Fail. 24, 716–723 (2022).
Charles-Edwards, G. et al. Effect of iron isomaltoside on skeletal muscle energetics in patients with chronic heart failure and iron deficiency. Circulation 139, 2386–2398 (2019).
Haddad, S. et al. Iron-regulatory proteins secure iron availability in cardiomyocytes to prevent heart failure. Eur. Heart J. 38, 362–372 (2017).
Long, M. et al. DGAT1 activity synchronises with mitophagy to protect cells from metabolic rewiring by iron depletion. EMBO J. 41, e109390 (2022).
Jang, S. et al. Elucidating the contribution of mitochondrial glutathione to ferroptosis in cardiomyocytes. Redox Biol. 45, 102021 (2021).
Tadokoro, T. et al. Mitochondria-dependent ferroptosis plays a pivotal role in doxorubicin cardiotoxicity. JCI Insight 5, e132747 (2020).
Fang, X. et al. Ferroptosis as a target for protection against cardiomyopathy. Proc. Natl Acad. Sci. USA 116, 2672–2680 (2019).
Komai, K., Kawasaki, N. K., Higa, J. K. & Matsui, T. The role of ferroptosis in adverse left ventricular remodeling following acute myocardial infarction. Cells 11, 1399 (2022).
Fang, X. et al. Loss of cardiac ferritin H facilitates cardiomyopathy via Slc7a11-mediated ferroptosis. Circ. Res. 127, 486–501 (2020).
Nemeth, E. & Ganz, T. The role of hepcidin in iron metabolism. Acta Haematol. 122, 78–86 (2009).
Kralova, B. et al. Developmental changes in iron metabolism and erythropoiesis in mice with human gain-of-function erythropoietin receptor. Am. J. Hematol. 97, 1286–1299 (2022).
Fang, X., Ardehali, H., Min, J. & Wang, F. The molecular and metabolic landscape of iron and ferroptosis in cardiovascular disease. Nat. Rev. Cardiol. https://doi.org/10.1038/s41569-022-00735-4 (2022).
Ito, J. et al. Iron derived from autophagy-mediated ferritin degradation induces cardiomyocyte death and heart failure in mice. eLife 10, e62174 (2021).
Martínez-Ruiz, A. et al. Soluble TNFα receptor type I and hepcidin as determinants of development of anemia in the long-term follow-up of heart failure patients. Clin. Biochem. 45, 1455–1458 (2012).
Masini, G. et al. Criteria for iron deficiency in patients with heart failure. J. Am. Coll. Cardiol. 79, 341–351 (2022).
Ghanim, H. et al. Dapagliflozin suppresses hepcidin and increases erythropoiesis. J. Clin. Endocrinol. Metab. 105, dgaa057 (2020).
Thiele, K. et al. Effects of empagliflozin on erythropoiesis in patients with type 2 diabetes: data from a randomized, placebo-controlled study. Diabetes Obes. Metab. 23, 2814–2818 (2021).
Xin, H. et al. Hydrogen sulfide attenuates inflammatory hepcidin by reducing IL-6 secretion and promoting SIRT1-mediated STAT3 deacetylation. Antioxid. Redox Signal. 24, 70–83 (2016).
Salazar, G. et al. SQSTM1/p62 and PPARGC1A/PGC-1alpha at the interface of autophagy and vascular senescence. Autophagy 16, 1092–1110 (2020).
Crane, F. L., Navas, P., Low, H., Sun, I. L. & de Cabo, R. Sirtuin activation: a role for plasma membrane in the cell growth puzzle. J. Gerontol. A Biol. Sci. Med. Sci. 68, 368–370 (2013).
Xu, W. et al. Lethal cardiomyopathy in mice lacking transferrin receptor in the heart. Cell Rep. 13, 533–545 (2015).
Lin, J. et al. Mitochondrial dynamics and mitophagy in cardiometabolic disease. Front. Cardiovasc. Med. 9, 917135 (2022).
Cui, L. et al. Erythropoietin activates SIRT1 to protect human cardiomyocytes against doxorubicin-induced mitochondrial dysfunction and toxicity. Toxicol. Lett. 275, 28–38 (2017).
Li, X. et al. NCOA4 is regulated by HIF and mediates mobilization of murine hepatic iron stores after blood loss. Blood 136, 2691–2702 (2020).
Berezovsky, B. et al. Effect of erythropoietin on the expression of murine transferrin receptor 2. Int. J. Mol. Sci. 22, 8209 (2021).
Honda, H. et al. Associations among erythroferrone and biomarkers of erythropoiesis and iron metabolism, and treatment with long-term erythropoiesis-stimulating agents in patients on hemodialysis. PLoS ONE 11, e0151601 (2016).
Waldman, M. et al. The role of heme oxygenase 1 in the protective effect of caloric restriction against diabetic cardiomyopathy. Int. J. Mol. Sci. 20, 2427 (2019).
Li, D. et al. Fisetin attenuates doxorubicin-induced cardiomyopathy in vivo and in vitro by inhibiting ferroptosis through SIRT1/Nrf2 signaling pathway activation. Front. Pharmacol. 12, 808480 (2022).
Docherty, K. F. et al. Effect of dapagliflozin on anaemia in DAPA-HF. Eur. J. Heart Fail. 23, 617–628 (2021).
Yamada, T. et al. Analysis of time-dependent alterations of parameters related to erythrocytes after ipragliflozin initiation. Diabetol. Int. 12, 197–206 (2020).
Kanamori, H. et al. Impact of autophagy on prognosis of patients with dilated cardiomyopathy. J. Am. Coll. Cardiol. 79, 789–801 (2022).
Hahn, V. S. et al. Myocardial gene expression signatures in human heart failure with preserved ejection fraction. Circulation 143, 120–134 (2021).
Saito, T. et al. Autophagic vacuoles in cardiomyocytes of dilated cardiomyopathy with initially decompensated heart failure predict improved prognosis. Autophagy 12, 579–587 (2016).
Saito, T. et al. Long-term prognostic value of ultrastructural features in dilated cardiomyopathy: comparison with cardiac magnetic resonance. Esc. Heart Fail. 7, 682–691 (2020).
Watanabe, T. et al. Restriction of food intake prevents postinfarction heart failure by enhancing autophagy in the surviving cardiomyocytes. Am. J. Pathol. 184, 1384–1394 (2014).
Zhu, H. et al. Cardiac autophagy is a maladaptive response to hemodynamic stress. J. Clin. Invest. 117, 1782–1793 (2007).
Nah, J. et al. Ulk1-dependent alternative mitophagy plays a protective role during pressure overload in the heart. Cardiovasc. Res. 118, 2638–2651 (2022).
Ghosh, R. et al. Chaperone mediated autophagy protects cardiomyocytes against hypoxic-cell death. Am. J. Physiol. Cell Physiol. 323, C1555–C1575 (2022).
Russo, M., Bono, E. & Ghigo, A. The interplay between autophagy and senescence in anthracycline cardiotoxicity. Curr. Heart Fail. Rep. 18, 180–190 (2021).
Wang, K. et al. Cardioprotection of Klotho against myocardial infarction-induced heart failure through inducing autophagy. Mech. Ageing Dev. 207, 111714 (2022).
Li, Q. et al. Hypoxia acclimation protects against heart failure postacute myocardial infarction via Fundc1-mediated mitophagy. Oxid. Med. Cell Longev. 2022, 8192552 (2022).
Li, L. et al. ATP6AP2 knockdown in cardiomyocyte deteriorates heart function via compromising autophagic flux and NLRP3 inflammasome activation. Cell Death Discov. 8, 161 (2022).
Deng, Z. et al. DNA methyltransferase 1 (DNMT1) suppresses mitophagy and aggravates heart failure via the microRNA-152-3p/ETS1/RhoH axis. Lab. Invest. 102, 782–793 (2022).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
During the past 3 years, M.P. has received consulting fees from AbbVie, Actavis, Amarin, Amgen, AstraZeneca, Boehringer Ingelheim, Caladrius, Casana, CSL Behring, Cytokinetics, Imara, Lilly, Moderna, Novartis, Reata, Relypsa and Salamandra, entirely related to the design and execution of clinical trials.
Peer review
Peer review information
Nature Reviews Cardiology thanks Gary Lopaschuk, Christoph Maack and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Packer, M. SGLT2 inhibitors: role in protective reprogramming of cardiac nutrient transport and metabolism. Nat Rev Cardiol 20, 443–462 (2023). https://doi.org/10.1038/s41569-022-00824-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-022-00824-4
This article is cited by
-
Advances in secondary prevention mechanisms of macrovascular complications in type 2 diabetes mellitus patients: a comprehensive review
European Journal of Medical Research (2024)
-
SGLT inhibitors: a serendipitous glycaemic tale
Nature Reviews Endocrinology (2024)
-
Association of sodium-glucose cotransporter 2 inhibitors with post-discharge outcomes in patients with acute heart failure with type 2 diabetes: a cohort study
Cardiovascular Diabetology (2023)
-
Multi-omics analysis reveals attenuation of cellular stress by empagliflozin in high glucose-treated human cardiomyocytes
Journal of Translational Medicine (2023)
-
Empagliflozin induces the transcriptional program for nutrient homeostasis in skeletal muscle in normal mice
Scientific Reports (2023)