Virtual reality is a fast-evolving technology that already has several promising applications in medicine. In this Clinical Outlook, we discuss the current evidence and the future challenges for virtual reality applications in cardiac interventions. The incorporation of virtual reality in daily practice will inevitably make clinical care more robust, patient-centred and safe.
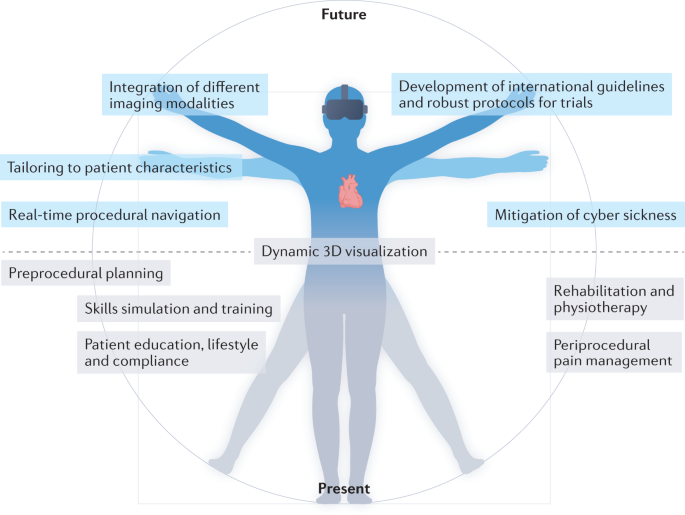
Right from its conception in studies of Ibn Sina (also known as Avicenna) and his contemporaries1, modern medicine has been and will always be subject to scientific and technological evolution. In the cyber era, the influences of extended reality modalities such as augmented reality and virtual reality (VR) are growing. VR platforms provide the user with the possibility of submerging into an alternative 3D environment and interacting with the surroundings in a real-time manner. A growing number of publications have described the potential applications of VR in medicine. However, randomized controlled trials involving VR in medicine are scarce, and robust evidence for the broad implementation of VR platforms in the clinic is limited. Several methodological and practical challenges need to be addressed in the near future before this highly promising technique can be fully implemented in the field of cardiac interventions (Fig. 1).
Several 3D virtual reality (VR) modules are in use in the field of cardiac interventions. The applications include skills simulation and training, periprocedural guidance and planning, enhanced 3D imaging visualization, patient education, pain management and rehabilitation. Although the use of VR applications is growing, many technological and methodological challenges remain. These challenges include addressing technical flaws such as the lack of haptic feedback, cyber sickness and the need for integration of multimodality imaging and real-time procedural visualization, as well as the need to tailor the module to the patient. Finally, international guidelines and protocols for the use of VR technology in scientific research and in the clinic are also needed.
Contemporary cardiac care includes increasingly complex percutaneous interventions and technical skills that require iterative practice and many working hours to acquire the necessary dexterity and clinical competency. Interventional cardiology is a continually evolving field associated with numerous technological advances over the past decades. Cardiac interventions are associated with a risk of major complications, which require adequate technical performance and effective team communication under stress to achieve positive outcomes. In this context, lifelong training and sufficient exposure to these cases are imperative, and VR technologies can have an important role in this process.
VR technologies can revolutionize the practice of clinical and technical skills training in the field of cardiac interventions2. Many VR-based skills simulators have been described and implemented in practice, including ones for vascular catheter cannulation and angiography, rhythm device and percutaneous valve implantation procedures, procedural anatomy teaching, and patient education and involvement in decision-making. Our group is developing several VR-based simulators for extracorporeal circulation and cardiopulmonary resuscitation after cardiac surgery3. These simulations have the potential to boost individual as well as team skills in the setting of complex clinical multidisciplinary situations.
“VR technologies can revolutionize the practice of clinical and technical skills training in the field of cardiac interventions”
VR technology provides digital, online, remotely accessible and blended simulation and live modules. Such a platform can alleviate many of the restrictions imposed by inability to travel (whether owing to travel restrictions, such as during the COVID-19 pandemic, or financial limitations) and provides training support, as well as expert and technical external periprocedural support.
In the preprocedural period, VR technology can provide a diagnostic and planning tool that is both dynamic and interactive. VR simulators facilitate the visualization of complex anatomy and allow the clinician to select the optimal intervention strategy (either percutaneous or surgical), tools and team4,5. This utility is of particular importance in the field of structural and congenital heart disease, for which interactive 3D visualization of the complex and often unique anatomy is imperative for procedural success6,7. The first feasibility studies evaluating the integration of CT, MRI and cardiac ultrasonography with VR technology are ongoing. Such technology will allow the incorporation of real-time haemodynamic data in high-spatial-resolution 3D structures. The introduction of these VR modules is expected to change the utilization of diagnostic imaging tools and will enhance our understanding of complex pathoanatomy.
“VR simulators facilitate the visualization of complex anatomy”
The role of VR technology in periprocedural pain management and rehabilitation has also been studied8. VR has been shown to reduce patient-perceived pain levels and periprocedural anxiety, as well as contribute to faster post-procedural functional recovery in patients undergoing cardiovascular interventions9. Furthermore, VR applications might also be of use as an adjunct strategy in cardiac rehabilitation. However, methodologically robust studies are needed to tailor the technology to the patient group (to take into account factors such as sex, age and technical literacy). Given the growing evidence on the potential of VR modules in both in-hospital and home-based pain management, it is tempting to think that VR technology might indeed become a part of regular treatment plans in the near future10. Of note, VR technology incorporates the features of meditation, cognitive behavioural therapy and mindfulness, highlighting how these often underappreciated ‘soft’ concepts of modern medicine can contribute to ‘hard’ clinical outcomes. VR technology can also be incorporated into outpatient clinics to improve patient education and thereby enhance the shared decision-making process and increase patient compliance. Meticulous patient selection and evaluation of cost/benefit ratios require further investigation before VR modules can be successfully implemented in insurance-based health care systems.
The outlook on the use of VR technology for cardiac interventions and patient care is promising. However, several challenges need to be addressed before this technology can be successfully implemented in daily clinical care. Aside from the technical challenges, such as the development of haptic feedback, prevention of cyber sickness, integration of multimodality imaging and implementation of real-time procedural visualization, two drawbacks related to methodology require specific attention. First, the majority of the studies on VR technology have been observational in nature, mostly describing the pioneering work and feasibility of the concept. These studies have low case numbers, single-centre experiences, divergent study protocols and differences in techniques used. The lack of overall methodological standardization makes the comparison of results from these studies challenging and impedes the generation of solid conclusions. Second, no recommendations or a formal consensus is available to guide the incorporation of VR technology in cardiac interventions. The successful implementation of VR in clinical care requires a formalized and, at least to some degree, a standardized approach. To address these challenges, we propose an expert taskforce among international scientific communities (including the AHA, ESC and EACTS) to identify the most important gaps in evidence on the implementation of VR technology in the field of cardiac interventions, as well as to set priorities, standardize research protocols and formulate recommendations and guidelines.
To conclude, the application of VR technology in cardiac interventions is developing apace and is here to stay. These modalities are expected to improve clinical practice and make patient care more robust, patient-centred and safe. However, several technological and methodological challenges need to be addressed before VR platforms can be implemented in the clinic. International cardiovascular communities can have a key role in this process through a dedicated expert taskforce.
References
UNESCO. Avicenna and the ethics of science and technology today. https://unesdoc.unesco.org/ark:/48223/pf0000134475 (2004).
Pezel, T. et al. Simulation-based training in cardiology: state-of-the-art review from the French Commission of Simulation Teaching (Commission d’enseignement par simulation-COMSI) of the French Society of Cardiology. Arch. Cardiovasc. Dis. 114, 73–84 (2021).
Sadeghi, A. H. et al. Virtual reality simulation training for cardiopulmonary resuscitation after cardiac surgery: face and content validity study. JMIR Serious Games 10, e30456 (2022).
Jung, C. et al. Virtual and augmented reality in cardiovascular care: state-of-the-art and future perspectives. JACC Cardiovasc. Imaging 15, 519–532 (2022).
Sadeghi, A. H. et al. Current and future applications of virtual, augmented, and mixed reality in cardiothoracic surgery. Ann. Thorac. Surg. 113, 681–691 (2022).
Zablah, J. E. & Morgan, G. J. Innovations in congenital interventional cardiology. Pediatr. Clin. North Am. 67, 973–993 (2020).
Deng, S. et al. A virtual reality system for improved image-based planning of complex cardiac procedures. J. Imaging 7, 151 (2021).
Birckhead, B. et al. Recommendations for methodology of virtual reality clinical trials in health care by an international working group: iterative study. JMIR Ment. Health 6, e11973 (2019).
García-Bravo, S. et al. Virtual reality and video games in cardiac rehabilitation programs. A systematic review. Disabil. Rehabil. 43, 448–457 (2021).
Spiegel, B. et al. Virtual reality for management of pain in hospitalized patients: a randomized comparative effectiveness trial. PLoS One 14, e0219115 (2019).
Acknowledgements
We thank Amir H. Sadeghi for help with preparing this manuscript and Jette J. Peek for help with preparing the figure.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
E.A.F.M. is a co-developer of several virtual reality modules in the field of cardiothoracic surgery. A.D.E. declares no competing interests.
Rights and permissions
About this article
Cite this article
Mahtab, E.A.F., Egorova, A.D. Current and future applications of virtual reality technology for cardiac interventions. Nat Rev Cardiol 19, 779–780 (2022). https://doi.org/10.1038/s41569-022-00789-4
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-022-00789-4