Abstract
The epidemiology of congenital heart disease (CHD) has changed in the past 50 years as a result of an increase in the prevalence and survival rate of CHD. In particular, mortality in patients with CHD has changed dramatically since the latter half of the twentieth century as a result of more timely diagnosis and the development of interventions for CHD that have prolonged life. As patients with CHD age, the disease burden shifts away from the heart and towards acquired cardiovascular and systemic complications. The societal costs of CHD are high, not just in terms of health-care utilization but also with regards to quality of life. Lifespan disease trajectories for populations with a high disease burden that is measured over prolonged time periods are becoming increasingly important to define long-term outcomes that can be improved. Quality improvement initiatives, including advanced physician training for adult CHD in the past 10 years, have begun to improve disease outcomes. As we seek to transform lifespan into healthspan, research efforts need to incorporate big data to allow high-value, patient-centred and artificial intelligence-enabled delivery of care. Such efforts will facilitate improved access to health care in remote areas and inform the horizontal integration of services needed to manage CHD for the prolonged duration of survival among adult patients.
Key points
-
Measurable changes in the prevalence of congenital heart disease (CHD) in the past decades are the result of evolving trends in birth prevalence and survival of patients over time.
-
Changes in birth prevalence over time and by region are, at least in part, attributable to variations in the availability of diagnostic tools and ascertainment.
-
Despite regional variations, the survival rates of patients with CHD have improved globally as evidenced by an increasing median age of CHD populations.
-
With prolonged survival among patients with CHD, the disease burden is shifting away from the heart and towards acquired cardiovascular and systemic complications throughout the lifespan.
-
Lifespan disease trajectories for CHD populations with a high disease burden measured over prolonged time windows are becoming increasingly important to define long-term outcomes that can be improved.
-
Strategically deployed, high-quality care will facilitate the integration of services that are needed to manage CHD and related comorbidities for the duration of the patient’s life.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Khairy, P. et al. Changing mortality in congenital heart disease. J. Am. Coll. Cardiol. 56, 1149–1157 (2010).
Marelli, A. The future of adult congenital heart disease care symposium: changing demographics of congenital heart disease. Prog. Pediatr. Cardiol. 34, 85–90 (2012). The paper provides the basic concepts of epidemiology of CHD and its determinants.
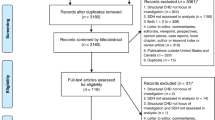
Liu, Y. et al. Global birth prevalence of congenital heart defects 1970–2017: updated systematic review and meta-analysis of 260 studies. Int. J. Epidemiol. 48, 455–463 (2019). The study is a systematic review and meta-analysis of the birth prevalence of CHD.
Dadvand, P., Rankin, J., Shirley, M. D., Rushton, S. & Pless-Mulloli, T. Descriptive epidemiology of congenital heart disease in Northern England. Paediatr. Perinat. Epidemiol. 23, 58–65 (2009).
Rodriguez Dehli, C. et al. [The epidemiology of congenital heart disease in Asturias (Spain) during the period 1990-2004]. An. Pediatr. 71, 502–509 (2009).
Riehle-Colarusso, T. et al. Congenital heart defects and receipt of special education services. Pediatrics 136, 496–504 (2015).
Wilson, P. D., Correa-Villasenor, A., Loffredo, C. A. & Ferencz, C. Temporal trends in prevalence of cardiovascular malformations in Maryland and the district of Columbia, 1981–1988. The Baltimore-Washington Infant Study Group. Epidemiology 4, 259–265 (1993).
Oyen, N. et al. National time trends in congenital heart defects, Denmark, 1977-2005. Am. Heart J. 157, 467–473 e461 (2009).
van der Linde, D. et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J. Am. Coll. Cardiol. 58, 2241–2247 (2011).
Malcic, I. & Dilber, D. [Distribution of congenital heart disease in Croatia and outcome analysis. a Croatian epidemiological study (2002–2007)]. Lijec. Vjesn. 133, 81–88 (2011).
Yu, M. et al. The survey of birth defects rate based on birth registration system. Chin. Med. J. 128, 7–14 (2015).
Xie, D., Yang, T., Liu, Z. & Wang, H. Epidemiology of birth defects based on a birth defect surveillance system from 2005 to 2014 in Hunan Province, China. PLoS One 11, e0147280 (2016).
Liu, S. et al. Association between maternal chronic conditions and congenital heart defects: a population-based cohort study. Circulation 128, 583–589 (2013).
Kolo, P. M., Adeoye, P. O., Omotosho, A. B. & Afolabi, J. K. Pattern of congenital heart disease in Ilorin, Nigeria. Niger. Postgrad. Med. J. 19, 230–234 (2012).
Robida, A., Folger, G. M. & Hajar, H. A. Incidence of congenital heart disease in Qatari children. Int. J. Cardiol. 60, 19–22 (1997).
Subramanyan, R., Joy, J., Venugopalan, P., Sapru, A. & al Khusaiby, S. M. Incidence and spectrum of congenital heart disease in Oman. Ann. Trop. Paediatr. 20, 337–341 (2000).
Egbe, A. et al. Temporal variation of birth prevalence of congenital heart disease in the United States. Congenit. Heart Dis. 10, 43–50 (2015).
Botto, L. D., Correa, A. & Erickson, J. D. Racial and temporal variations in the prevalence of heart defects. Pediatrics 107, E32 (2001).
Jung, S. C., Kim, S. S., Yoon, K. S. & Lee, J. S. Prevalence of congenital malformations and genetic diseases in Korea. J. Hum. Genet. 44, 30–34 (1999).
Lamichhane, D. K. et al. Increased prevalence of some birth defects in Korea, 2009–2010. BMC Pregnancy Childbirth 16, 61 (2016).
Yeh, S. J. et al. Prevalence, mortality, and the disease burden of pediatric congenital heart disease in Taiwan. Pediatr. Neonatol. 54, 113–118 (2013).
Plana, M. N. et al. Pulse oximetry screening for critical congenital heart defects. Cochrane Database Syst. Rev. 3, CD011912 (2018).
Mahle, W. T. et al. Endorsement of health and human services recommendation for pulse oximetry screening for critical congenital heart disease. Pediatrics 129, 190–192 (2012).
Wong, K. K. et al. Canadian Cardiovascular Society/Canadian Pediatric Cardiology Association position statement on pulse oximetry screening in newborns to enhance detection of critical congenital heart disease. Can. J. Cardiol. 33, 199–208 (2017).
Manzoni, P. et al. Pulse oximetry screening for critical congenital heart defects: a European consensus statement. Lancet Child. Adolesc. Health 1, 88–90 (2017).
Zhao, Q. M. et al. Pulse oximetry with clinical assessment to screen for congenital heart disease in neonates in China: a prospective study. Lancet 384, 747–754 (2014).
Hom, L. A. & Martin, G. R. Newborn critical congenital heart disease screening using pulse oximetry: value and unique challenges in developing regions. Int. J. Neonatal Screen. 6, 74 (2020).
Martin, G. R. et al. Updated strategies for pulse oximetry screening for critical congenital heart disease. Pediatrics https://doi.org/10.1542/peds.2019-1650 (2020).
Warnes, C. A. et al. Task force 1: the changing profile of congenital heart disease in adult life. J. Am. Coll. Cardiol. 37, 1170–1175 (2001).
Oster, M. E. et al. Temporal trends in survival among infants with critical congenital heart defects. Pediatrics 131, e1502–e1508 (2013).
Boneva, R. S. et al. Mortality associated with congenital heart defects in the United States: trends and racial disparities, 1979-1997. Circulation 103, 2376–2381 (2001).
Pillutla, P., Shetty, K. D. & Foster, E. Mortality associated with adult congenital heart disease: trends in the US population from 1979 to 2005. Am. Heart J. 158, 874–879 (2009).
Raissadati, A., Nieminen, H., Haukka, J., Sairanen, H. & Jokinen, E. Late causes of death after pediatric cardiac surgery: a 60-year population-based study. J. Am. Coll. Cardiol. 68, 487–498 (2016).
Moons, P., Bovijn, L., Budts, W., Belmans, A. & Gewillig, M. Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation 122, 2264–2272 (2010).
Mandalenakis, Z. et al. Survivorship in children and young adults with congenital heart disease in Sweden. JAMA Intern. Med. 177, 224–230 (2017). The study assessed survival in children and young adults with CHD compared with matched controls from the general population.
van der Bom, T. et al. Contemporary survival of adults with congenital heart disease. Heart 101, 1989–1995 (2015).
GBD 2017 Congenital Heart Disease Collaborators. Global, regional, and national burden of congenital heart disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Child. Adolesc. Health 4, 185–200 (2020). The study provides a systematic analysis of the global prevalence of CHD in 1990 and 2017.
Marelli, A. J. et al. Lifetime prevalence of congenital heart disease in the general population from 2000 to 2010. Circulation 130, 749–756 (2014). The study provides an empirical analysis of the lifetime prevalence of CHD during the first decade of the twenty-first century.
Benziger, C. P., Stout, K., Zaragoza-Macias, E., Bertozzi-Villa, A. & Flaxman, A. D. Projected growth of the adult congenital heart disease population in the United States to 2050: an integrative systems modeling approach. Popul. Health Metr. 13, 29 (2015).
van der Bom, T., Bouma, B. J., Meijboom, F. J., Zwinderman, A. H. & Mulder, B. J. The prevalence of adult congenital heart disease, results from a systematic review and evidence based calculation. Am. Heart J. 164, 568–575 (2012).
Wu, M. H., Lu, C. W., Chen, H. C., Kao, F. Y. & Huang, S. K. Adult congenital heart disease in a nationwide population 2000-2014: epidemiological trends, arrhythmia, and standardized mortality ratio. J. Am. Heart Assoc. https://doi.org/10.1161/JAHA.117.007907 (2018).
Bouchardy, J. et al. Atrial arrhythmias in adults with congenital heart disease. Circulation 120, 1679–1686 (2009).
Cohen, S. et al. Risk prediction models for heart failure admissions in adults with congenital heart disease. Int. J. Cardiol. https://doi.org/10.1016/j.ijcard.2020.08.039 (2020).
van Riel, A. C. et al. Contemporary prevalence of pulmonary arterial hypertension in adult congenital heart disease following the updated clinical classification. Int. J. Cardiol. 174, 299–305 (2014).
Lin, Y. S. et al. Major adverse cardiovascular events in adult congenital heart disease: a population-based follow-up study from Taiwan. BMC Cardiovasc. Disord. 14, 38 (2014).
Kuijpers, J. M. et al. Risk of coronary artery disease in adults with congenital heart disease: a comparison with the general population. Int. J. Cardiol. 304, 39–42 (2020).
Bouma, B. J. & Mulder, B. J. Changing landscape of congenital heart disease. Circ. Res. 120, 908–922 (2017).
Kwiatek-Wrzosek, A., Kowalik, E., Kowalski, M. & Hoffman, P. The burden of cardiovascular risk factors among seniors with congenital heart disease: a single tertiary center experience. Kardiol. Pol. 79, 1251–1255 (2021).
Goldstein, S. A. et al. Causes of death and cardiovascular comorbidities in adults with congenital heart disease. J. Am. Heart Assoc. 9, e016400 (2020).
Lanz, J. et al. Stroke in adults with congenital heart disease: incidence, cumulative risk, and predictors. Circulation 132, 2385–2394 (2015).
International Cardiac Collaborative on Neurodevelopment Investigators. Impact of operative and postoperative factors on neurodevelopmental outcomes after cardiac operations. Ann. Thorac. Surg. 102, 843–849 (2016).
Sterling, L. H. et al. Neurocognitive disorders amongst patients with congenital heart disease undergoing procedures in childhood. Int. J. Cardiol. 336, 47–53 (2021).
Cohen, S. et al. Exposure to low-dose ionizing radiation from cardiac procedures and malignancy risk in adults with congenital heart disease. Circulation 137, 1334–1345 (2018).
Chong, L. S. H. et al. Children’s experiences of congenital heart disease: a systematic review of qualitative studies. Eur. J. Pediatr. 177, 319–336 (2018).
Delaney, A. E. et al. Parents’ perceptions of emerging adults with congenital heart disease: an integrative review of qualitative studies. J. Pediatr. Health Care 35, 362–376 (2021).
Svensson, M. K., Wahlberg, A. & Gislason, G. H. Chronic paradoxes: a systematic review of qualitative family perspectives on living with congenital heart defects. Qual. Health Res. 30, 119–132 (2020).
Deng, L. X. et al. Prevalence and correlates of post-traumatic stress disorder in adults with congenital heart disease. Am. J. Cardiol. 117, 853–857 (2016).
Westhoff-Bleck, M. et al. Mental disorders in adults with congenital heart disease: unmet needs and impact on quality of life. J. Affect. Disord. 204, 180–186 (2016).
Eslami, B. Correlates of posttraumatic stress disorder in adults with congenital heart disease. Congenit. Heart Dis. 12, 357–363 (2017).
Kasmi, L. et al. Neurocognitive and psychological outcomes in adults with dextro-transposition of the great arteries corrected by the arterial switch operation. Ann. Thorac. Surg. 105, 830–836 (2018).
Moreland, P. & Santacroce, S. J. Illness uncertainty and posttraumatic stress in young adults with congenital heart disease. J. Cardiovasc. Nurs. 33, 356–362 (2018).
Carazo, M. R. et al. Prevalence and prognostic association of a clinical diagnosis of depression in adult congenital heart disease: results of the boston adult congenital heart disease biobank. J. Am. Heart Assoc. 9, e014820 (2020).
Simeone, R. M. et al. Post-traumatic stress disorder, anxiety, and depression among adults with congenital heart defects. Birth Defects Res. 114, 124–135 (2022).
Apers, S. et al. Sense of coherence and perceived physical health explain the better quality of life in adolescents with congenital heart disease. Eur. J. Cardiovasc. Nurs. 12, 475–483 (2013).
Moons, P. et al. Sense of coherence in adults with congenital heart disease in 15 countries: patient characteristics, cultural dimensions and quality of life. Eur. J. Cardiovasc. Nurs. 20, 48–55 (2021).
Apers, S. et al. Quality of life of adults with congenital heart disease in 15 countries: evaluating country-specific characteristics. J. Am. Coll. Cardiol. 67, 2237–2245 (2016).
Schroder, M., Boisen, K. A., Reimers, J., Teilmann, G. & Brok, J. Quality of life in adolescents and young adults with CHD is not reduced: a systematic review and meta-analysis. Cardiol. Young 26, 415–425 (2016).
Kahr, P. C., Radke, R. M., Orwat, S., Baumgartner, H. & Diller, G. P. Analysis of associations between congenital heart defect complexity and health-related quality of life using a meta-analytic strategy. Int. J. Cardiol. 199, 197–203 (2015).
Willems, R., Werbrouck, A., De Backer, J. & Annemans, L. Real-world healthcare utilization in adult congenital heart disease: a systematic review of trends and ratios. Cardiol. Young 29, 553–563 (2019).
Cedars, A. et al. Contemporary hospitalization rate among adults with complex congenital heart disease. World J. Pediatr. Congenit. Heart Surg. 7, 334–343 (2016).
Ombelet, F. et al. Creating the BELgian COngenital heart disease database combining administrative and clinical data (BELCODAC): rationale, design and methodology. Int. J. Cardiol. 316, 72–78 (2020).
Farr, S. L., Downing, K. F., Riehle-Colarusso, T. & Abarbanell, G. Functional limitations and educational needs among children and adolescents with heart disease. Congenit. Heart Dis. 13, 633–639 (2018).
Agom, D. A., Onyeka, T. C., Iheanacho, P. N. & Ominyi, J. Barriers to the provision and utilization of palliative care in Africa: a rapid scoping review. Indian J. Palliat. Care 27, 3–17 (2021).
Downing, K. F. et al. Disability among young adults with congenital heart defects: congenital heart survey to recognize outcomes, needs, and well-being 2016–2019. J. Am. Heart Assoc. 10, e022440 (2021).
Sluman, M. A. et al. Education as important predictor for successful employment in adults with congenital heart disease worldwide. Congenit. Heart Dis. 14, 362–371 (2019).
Mackie, A. S., Tran, D. T., Marelli, A. J. & Kaul, P. Cost of congenital heart disease hospitalizations in Canada: a population-based study. Can. J. Cardiol. 33, 792–798 (2017).
Briston, D. A., Bradley, E. A., Sabanayagam, A. & Zaidi, A. N. Health care costs for adults with congenital heart disease in the United States 2002 to 2012. Am. J. Cardiol. 118, 590–596 (2016).
Lonsdale, H., Jalali, A., Ahumada, L. & Matava, C. Machine learning and artificial intelligence in pediatric research: current state, future prospects, and examples in perioperative and critical care. J. Pediatr. 221, S3–S10 (2020).
Baumgartner, H. et al. 2020 ESC guidelines for the management of adult congenital heart disease. Eur. Heart J. 42, 563–645 (2021).
Lu, X. H. et al. Recurrent disease progression networks for modelling risk trajectory of heart failure. PLoS One 16, e0245177 (2021).
Diller, G. P. et al. Lifespan perspective on congenital heart disease research: JACC state-of-the-art review. J. Am. Coll. Cardiol. 77, 2219–2235 (2021). The paper suggested a paradigm shift in CHD research towards a lifespan perspective and proactive approach to CHD care.
Mei, H. & Eisner, J. M. The neural Hawkes process: a neurally self-modulating multivariate point process. in Adv. Neural Inf. Process. Syst. 6754–6764 (2017).
Choi, E., Du, N., Chen, R., Song, L. & Sun, J. in 2015 IEEE International Conference on Data Mining (ICDM). 721–726 (IEEE, 2015).
Bertsimas, D. et al. Adverse outcomes prediction for congenital heart surgery: a machine learning approach. World J. Pediatr. Congenit. Heart Surg. 12, 453–460 (2021).
Christodoulou, E. et al. A systematic review shows no performance benefit of machine learning over logistic regression for clinical prediction models. J. Clin. Epidemiol. 110, 12–22 (2019).
Van den Eynde, J. et al. Medicine-based evidence in congenital heart disease: how artificial intelligence can guide treatment decisions for individual patients. Front. Cardiovasc. Med. 8, 798215 (2021).
Diller, G. P. et al. Machine learning algorithms estimating prognosis and guiding therapy in adult congenital heart disease: data from a single tertiary centre including 10 019 patients. Eur. Heart J. 40, 1069–1077 (2019).
Diller, G. P. et al. Prediction of prognosis in patients with tetralogy of Fallot based on deep learning imaging analysis. Heart 106, 1007–1014 (2020).
Cohen, S. & Marelli, A. Increasing survival in patients with congenital heart disease-a glass half full or half empty? JAMA Intern. Med. 177, 1690–1691 (2017).
Webb, G. D. & Williams, R. G. Care of the adult with congenital heart disease: introduction. J. Am. Coll. Cardiol. 37, 1166 (2001).
Stout, K. K. et al. 2018 AHA/ACC guideline for the management of adults with congenital heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 73, 1494–1563 (2019).
ABIM. Adult Congenital Heart Disease Policies https://www.abim.org/certification/policies/internal-medicine-subspecialty-policies/adult-congenital-heart-disease.aspx (2022).
Kaemmerer, H. et al. Recommendations for improving the quality of the interdisciplinary medical care of grown-ups with congenital heart disease (GUCH). Int. J. Cardiol. 150, 59–64 (2011).
Neidenbach, R. et al. Systematic assessment of health care perception in adults with congenital heart disease in Germany. Cardiovasc. Diagn. Ther. 11, 481–491 (2021).
CachNet. Canadian Adult Congenital Heart Disease Network http://www.cachnet.org.
ACHA. The Adult Congenital Heart Association Program Accreditation https://www.achaheart.org/your-heart/programs/accreditation/.
Mylotte, D. et al. Specialized adult congenital heart disease care: the impact of policy on mortality. Circulation 129, 1804–1812 (2014). The study demonstrated the effect of specialized adult CHD care in reducing mortality.
Nguyen, V. P. et al. Improved outcomes of heart transplantation in adults with congenital heart disease receiving regionalized care. J. Am. Coll. Cardiol. 74, 2908–2918 (2019).
Cordina, R. et al. Management errors in adults with congenital heart disease: prevalence, sources, and consequences. Eur. Heart J. 39, 982–989 (2018).
Fernandes, S. M., Marelli, A., Hile, D. M. & Daniels, C. J. Access and delivery of adult congenital heart disease care in the United States: quality-driven team-based care. Cardiol. Clin. 38, 295–304 (2020).
Marelli, A. J., Therrien, J., Mackie, A. S., Ionescu-Ittu, R. & Pilote, L. Planning the specialized care of adult congenital heart disease patients: from numbers to guidelines; an epidemiologic approach. Am. Heart J. 157, 1–8 (2009).
Kwan, G. F. et al. Endemic cardiovascular diseases of the poorest billion. Circulation 133, 2561–2575 (2016).
Mattos Sda, S. et al. A telemedicine network for remote paediatric cardiology services in north-east Brazil. Bull. World Health Organ. 93, 881–887 (2015).
Joury, A. et al. Leadless and wireless cardiac devices: the next frontier in remote patient monitoring. Curr. Probl. Cardiol. 46, 100800 (2021).
United States Government Accountability Office. Artificial Intelligence in Health Care: Benefits and Challenges of Technologies to Augment Patient Care (Publication GAO-21-7SP, 2020).
Hummel, K. et al. Development of an international standard set of clinical and patient-reported outcomes for children and adults with congenital heart disease: a report from the International Consortium for Health Outcomes Measurement Congenital Heart Disease Working Group. Eur. Heart J. Qual. Care Clin. Outcomes 7, 354–365 (2021). The paper reported the first international development of a stakeholder-informed standard set of outcome measures for CHD.
Harahsheh, A. S. et al. American College of Cardiology body mass index counseling quality improvement initiative. Pediatr. Cardiol. 42, 1190–1199 (2021).
Author information
Authors and Affiliations
Contributions
The authors contributed substantially to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Cardiology thanks Peter Ewert, who co-reviewed with Michael Huntgeburth; Yves d’Udekem and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
International Consortium for Health Outcomes Measurement: http://www.ichom.org/
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, A., Diller, GP., Moons, P. et al. Changing epidemiology of congenital heart disease: effect on outcomes and quality of care in adults. Nat Rev Cardiol 20, 126–137 (2023). https://doi.org/10.1038/s41569-022-00749-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-022-00749-y