Abstract
Variants in >12 genes encoding sarcomeric proteins can cause various cardiomyopathies. The two most common are hypertrophic cardiomyopathy (HCM) and dilated cardiomyopathy (DCM). Current therapeutics do not target the root causes of these diseases, but attempt to prevent disease progression and/or to manage symptoms. Accordingly, novel approaches are being developed to treat the cardiac muscle dysfunction directly. Challenges to developing therapeutics for these diseases include the diverse mechanisms of pathogenesis, some of which are still being debated and defined. Four small molecules that modulate the myosin motor protein in the cardiac sarcomere have shown great promise in the settings of HCM and DCM, regardless of the underlying genetic pathogenesis, and similar approaches are being developed to target other components of the sarcomere. In the setting of HCM, mavacamten and aficamten bind to the myosin motor and decrease the ATPase activity of myosin. In the setting of DCM, omecamtiv mecarbil and danicamtiv increase myosin activity in cardiac muscle (but omecamtiv mecarbil decreases myosin activity in vitro). In this Review, we discuss the therapeutic strategies to alter sarcomere contractile activity and summarize the data indicating that targeting one protein in the sarcomere can be effective in treating patients with genetic variants in other sarcomeric proteins, as well as in patients with non-sarcomere-based disease.
Key points
-
Variants in genes encoding sarcomeric proteins are a leading cause of cardiomyopathies that are characterized by protein-specific molecular mechanisms of disease.
-
Sarcomeric proteins can be targeted by small molecules to directly modulate contractile function in cardiac muscle.
-
Small molecules that are targeted to the myosin heavy chain modulate enzymatic activity and/or availability of the myosin motor, leading to an increase or decrease in force production.
-
Small molecules that target the myosin heavy chain, such as mavacamten and aficamten, can act via distinct molecular mechanisms that lead to altered myosin function.
-
Sarcomere pharmacology suggests that small molecules targeting a specific sarcomeric protein will be effective even in patients with a causal variant in a gene encoding another sarcomeric protein.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Geisterfer-Lowrance, A. A. et al. A molecular basis for familial hypertrophic cardiomyopathy: a β cardiac myosin heavy chain gene missense mutation. Cell 62, 999–1006 (1990).
Kamisago, M. et al. Mutations in sarcomere protein genes as a cause of dilated cardiomyopathy. N. Engl. J. Med. 343, 1688–1696 (2000).
Herman, D. et al. Truncations of titin causing dilated cardiomyopathy. N. Engl. J. Med. 366, 619–628 (2012).
McNally, E. & Mestroni, L. Dilated cardiomyopathy: genetic determinants and mechanisms. Circ. Res. 121, 731–748 (2017).
Spudich, J. Three perspectives on the molecular basis of hypercontractility caused by hypertrophic cardiomyopathy mutations. Pflug. Arch. 471, 701–717 (2019).
Ho, C. et al. Genotype and lifetime burden of disease in hypertrophic cardiomyopathy: insights from the sarcomeric human cardiomyopathy registry (SHaRe). Circulation 138, 1387–1398 (2018).
Repetti, G., Toepfer, C., Seidman, J. & Seidman, C. Novel therapies for prevention and early treatment of cardiomyopathies. Circ. Res. 124, 1536–1550 (2019).
Said, S., Dearani, J., Ommen, S. & Schaff, H. Surgical treatment of hypertrophic cardiomyopathy. Expert Rev. Cardiovasc. Ther. 11, 617–627 (2013).
Mateo, J. & Gimeno, J. Alcohol septal ablation in hypertrophic cardiomyopathy. Glob. Cardiol. Sci. Pract. 2018, 30 (2018).
Verlinden, N. & Coons, J. Disopyramide for hypertrophic cardiomyopathy: a pragmatic reappraisal of an old drug. Pharmacotherapy 35, 1164–1172 (2015).
Cardoso, R. et al. SGLT2 inhibitors decrease cardiovascular death and heart failure hospitalizations in patients with heart failure: a systematic review and meta-analysis. EClinicalMedicine 36, 100933 (2021).
Alsulami, K. & Marston, S. Small molecules acting on myofilaments as treatments for heart and skeletal muscle diseases. Int. J. Mol. Sci. 21, 9599 (2020).
Malik, F. I. et al. Cardiac myosin activation: a potential therapeutic approach for systolic heart failure. Science 331, 1439–1443 (2011).
Green, E. M. et al. A small-molecule inhibitor of sarcomere contractility suppresses hypertrophic cardiomyopathy in mice. Science 351, 617–621 (2016).
Price, H. The skeletal muscle fiber in the light of electron microscope studies: a review. Am. J. Med. 35, 589–605 (1963).
Gordon, A., Homsher, E. & Regnier, M. Regulation of contraction in striated muscle. Physiol. Rev. 80, 853–924 (2000).
Woodhead, J. L. et al. Atomic model of a myosin filament in the relaxed state. Nature 436, 1195–1199 (2005).
Jung, H., Komatsu, S., Ikebe, M. & Craig, R. Head-head and head-tail interaction: a general mechanism for switching off myosin II activity in cells. Mol. Biol. Cell 19, 3234–3242 (2008).
Zoghbi, M., Woodhead, J., Moss, R. & Craig, R. Three-dimensional structure of vertebrate cardiac muscle myosin filaments. Proc. Natl Acad. Sci. USA 105, 2386–2390 (2008).
Stewart, M., Franks-Skiba, K., Chen, S. & Cooke, R. Myosin ATP turnover rate is a mechanism involved in thermogenesis in resting skeletal muscle fibers. Proc. Natl Acad. Sci. USA 107, 430–435 (2010).
Hooijman, P., Stewart, M. & Cooke, R. A new state of cardiac myosin with very slow ATP turnover: a potential cardioprotective mechanism in the heart. Biophys. J. 100, 1969–1976 (2011).
Toepfer, C. et al. Myosin sequestration regulates sarcomere function, cardiomyocyte energetics, and metabolism, informing the pathogenesis of hypertrophic cardiomyopathy. Circulation 141, 828–842 (2020).
Alamo, L. et al. Conserved intramolecular interactions maintain myosin interacting-heads motifs explaining tarantula muscle super-relaxed state structural basis. J. Mol. Biol. 428, 1142–1164 (2016).
Ma, W., Gong, H. & Irving, T. Myosin head configurations in resting and contracting murine skeletal muscle. Int. J. Mol. Sci. 19, 2643 (2018).
Robert-Paganin, J., Auguin, D. & Houdusse, A. Hypertrophic cardiomyopathy disease results from disparate impairments of cardiac myosin function and auto-inhibition. Nat. Commun. 9, 4019 (2018).
Chu, S., Muretta, J. & Thomas, D. Direct detection of the myosin super-relaxed state and interacting-heads motif in solution. J. Biol. Chem. 297, 101157 (2021).
Knupp, C., Morris, E. & Squire, J. The interacting head motif structure does not explain the X-ray diffraction patterns in relaxed vertebrate (bony fish) skeletal muscle and insect (Lethocerus) flight muscle. Biology 8, 67 (2019).
Brunello, E. et al. Myosin filament-based regulation of the dynamics of contraction in heart muscle. Proc. Natl Acad. Sci. USA 117, 8177–8186 (2020).
Crocini, C. & Gotthardt, M. Cardiac sarcomere mechanics in health and disease. Biophys. Rev. 13, 637–652 (2021).
Rahmanseresht, S. et al. The N terminus of myosin-binding protein C extends toward actin filaments in intact cardiac muscle. J. Gen. Physiol. 153, e202012726 (2021).
Inchingolo, A., Previs, S., Previs, M., Warshaw, D. & Kad, N. Revealing the mechanism of how cardiac myosin-binding protein C N-terminal fragments sensitize thin filaments for myosin binding. Proc. Natl Acad. Sci. USA 116, 6828–6835 (2019).
Li, A. et al. Skeletal MyBP-C isoforms tune the molecular contractility of divergent skeletal muscle systems. Proc. Natl Acad. Sci. USA 116, 21882–21892 (2019).
Moss, R., Fitzsimons, D. & Ralphe, J. Cardiac MyBP-C regulates the rate and force of contraction in mammalian myocardium. Circ. Res. 116, 183–192 (2015).
McNamara, J. et al. Ablation of cardiac myosin binding protein-C disrupts the super-relaxed state of myosin in murine cardiomyocytes. J. Mol. Cell Cardiol. 94, 65–71 (2016).
Nelson, S., Li, A., Beck-Previs, S., Kennedy, G. & Warshaw, D. Imaging ATP consumption in resting skeletal muscle: one molecule at a time. Biophys. J. 119, 1050–1055 (2020).
Kensler, R., Craig, R. & Moss, R. Phosphorylation of cardiac myosin binding protein C releases myosin heads from the surface of cardiac thick filaments. Proc. Natl Acad. Sci. USA 114, E1355–E1364 (2017).
Sarkar, S. et al. The hypertrophic cardiomyopathy mutations R403Q and R663H increase the number of myosin heads available to interact with actin. Sci. Adv. 6, eaax0069 (2021).
McNamara, J., Singh, R. & Sadayappan, S. Cardiac myosin binding protein-C phosphorylation regulates the super-relaxed state of myosin. Proc. Natl Acad. Sci. USA 116, 11731–11736 (2019).
Walsh, R., Offerhaus, J., Tadros, R. & Bezzina, C. Minor hypertrophic cardiomyopathy genes, major insights into the genetics of cardiomyopathies. Nat. Rev. Cardiol. 19, 151–167 (2022).
Marian, A. & Braunwald, E. Hypertrophic cardiomyopathy: genetics, pathogenesis, clinical manifestations, diagnosis, and therapy. Circ. Res. 121, 749–770 (2017).
Glazier, A., Thompson, A. & Day, S. Allelic imbalance and haploinsufficiency in MYBPC3-linked hypertrophic cardiomyopathy. Pflug. Arch. 471, 781–793 (2019).
Yang, Q. et al. A mouse model of myosin binding protein C human familial hypertrophic cardiomyopathy. J. Clin. Invest. 102, 1292–1300 (1998).
Helms, A. et al. Effects of MYBPC3 loss-of-function mutations preceding hypertrophic cardiomyopathy. JCI Insight 5, e133782 (2020).
Schmid, M. & Toepfer, C. Cardiac myosin super relaxation (SRX): a perspective on fundamental biology, human disease and therapeutics. Biol. Open 10, bio.057646 (2021).
McNamara, J. et al. MYBPC3 mutations are associated with a reduced super-relaxed state in patients with hypertrophic cardiomyopathy. PLoS ONE 12, e0180064 (2017).
Anderson, R. et al. Deciphering the super relaxed state of human β-cardiac myosin and the mode of action of mavacamten from myosin molecules to muscle fibers. Proc. Natl Acad. Sci. USA 115, E8143–E8152 (2018).
Rohde, J., Roopnarine, O., Thomas, D. & Muretta, J. Mavacamten stabilizes an autoinhibited state of two-headed cardiac myosin. Proc. Natl Acad. Sci. USA 115, E7486–E7494 (2018).
Adhikari, A. et al. β-Cardiac myosin hypertrophic cardiomyopathy mutations release sequestered heads and increase enzymatic activity. Nat. Commun. 10, 2685 (2019).
Gollapudi, S., Yu, M., Gan, Q. & Nag, S. Synthetic thick filaments: a new avenue for better understanding the myosin super-relaxed state in healthy, diseased, and mavacamten-treated cardiac systems. J. Biol. Chem. 296, 100114 (2021).
Alamo, L. et al. Effects of myosin variants on interacting-heads motif explain distinct hypertrophic and dilated cardiomyopathy phenotypes. eLife 6, e24634 (2017).
Dellefave, L. & McNally, E. The genetics of dilated cardiomyopathy. Curr. Opin. Cardiol. 25, 198–204 (2010).
Ceco, E. et al. Targeting latent TGFβ release in muscular dystrophy. Sci. Transl Med. 6, 259ra144 (2014).
Roncarati, R. et al. Doubly heterozygous LMNA and TTN mutations revealed by exome sequencing in a severe form of dilated cardiomyopathy. Eur. J. Hum. Genet. 21, 1105–1111 (2013).
Gerull, B. et al. Mutations of TTN, encoding the giant muscle filament titin, cause familial dilated cardiomyopathy. Nat. Genet. 30, 201–204 (2002).
Ware, J. & Cook, S. Role of titin in cardiomyopathy: from DNA variants to patient stratification. Nat. Rev. Cardiol. 15, 241–252 (2017).
McAfee, Q. et al. Truncated titin proteins in dilated cardiomyopathy. Sci. Transl Med. 13, eabd7287 (2021).
Nagy, L., Pollesello, P. & Papp, Z. Inotropes and inodilators for acute heart failure: sarcomere active drugs in focus. J. Cardiovasc. Pharmacol. 64, 199–208 (2014).
Herzig, J. W., Feile, K. & Ruegg, J. C. Activating effects of AR-L 115 BS on the Ca2+ sensitive force, stiffness and unloaded shortening velocity (Vmax) in isolated contractile structures from mammalian heart muscle. Arzneimittelforschung 31, 188–191 (1981).
Solaro, R. J. & Ruegg, J. C. Stimulation of Ca++ binding and ATPase activity of dog cardiac myofibrils by AR-L 115BS, a novel cardiotonic agent. Circ. Res. 51, 290–294 (1982).
Raasmaja, A. et al. Biochemical properties of OR-1259 – a positive inotropic and vasodilatory compound with an antiarrhythmic effect. Adv. Exp. Med. Biol. 311, 423 (1992).
Haikala, H. et al. Cardiac troponin C as a target protein for a novel calcium sensitizing drug, levosimendan. J. Mol. Cell Cardiol. 27, 1859–1866 (1995).
Pollesello, P. et al. Binding of a new Ca2+ sensitizer, levosimendan, to recombinant human cardiac troponin C. A molecular modelling, fluorescence probe, and proton nuclear magnetic resonance study. J. Biol. Chem. 269, 28584–28590 (1994).
Sorsa, T., Pollesello, P. & Solaro, R. The contractile apparatus as a target for drugs against heart failure: interaction of levosimendan, a calcium sensitiser, with cardiac troponin c. Mol. Cell Biochem. 266, 87–107 (2004).
Sorsa, T. et al. Binding of levosimendan, a calcium sensitizer, to cardiac troponin C. J. Biol. Chem. 276, 9337–9343 (2001).
Haikala, H. & Linden, I. Mechanisms of action of calcium-sensitizing drugs. J. Cardiovasc. Pharmacol. 26 (Suppl. 1), 10–19 (1995).
Boknik, P. et al. Mechanisms of the contractile effects of levosimendan in the mammalian heart. J. Pharmacol. Exp. Ther. 280, 277–283 (1997).
Szilagyi, S. et al. The effects of levosimendan and OR-1896 on isolated hearts, myocyte-sized preparations and phosphodiesterase enzymes of the guinea pig. Eur. J. Pharmacol. 486, 67–74 (2004).
Orstavik, O. et al. The inotropic effect of the active metabolite of levosimendan, OR-1896, is mediated through inhibition of PDE3 in rat ventricular myocardium. PLoS ONE 10, e0115547 (2015).
Follath, F. et al. Efficacy and safety of intravenous levosimendan compared with dobutamine in severe low-output heart failure (the LIDO study): a randomised double-blind trial. Lancet 360, 196–202 (2002).
Mebazaa, A. et al. Levosimendan vs dobutamine for patients with acute decompensated heart failure: the SURVIVE randomized trial. JAMA 297, 1883–1891 (2007).
Landoni, G. et al. Levosimendan for hemodynamic support after cardiac surgery. N. Engl. J. Med. 376, 2021–2031 (2017).
Mehta, R. H. et al. Levosimendan in patients with left ventricular dysfunction undergoing cardiac surgery. N. Engl. J. Med. 376, 2032–2042 (2017).
Cholley, B. et al. Effect of levosimendan on low cardiac output syndrome in patients with low ejection fraction undergoing coronary artery bypass grafting with cardiopulmonary bypass: the LICORN randomized clinical trial. JAMA 318, 548–556 (2017).
Packer, M. et al. Effect of levosimendan on the short-term clinical course of patients with acutely decompensated heart failure. JACC Heart Fail. 1, 103–111 (2013).
Harjola, V. et al. Organ dysfunction, injury and failure in acute heart failure: from pathophysiology to diagnosis and management. A review on behalf of the Acute Heart Failure Committee of the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur. J. Heart Fail. 19, 821–836 (2017).
Reagan, J. D. et al. The novel myotrope, AMG 594, is a small-molecule cardiac troponin activator that increases cardiac contractility in vitro and in vivo. Presented at the Keystone Symposium on Charting a New Course for Heart Failure: From Discovery to Data (Amgen and Cytokinetics, 2020).
He, H. et al. A novel small molecule troponin activator increases cardiac contractile function without negative impact on energetics or diastolic function. Circ. Heart Fail. 144, A9199 (2021).
Morgan, B. P. et al. Discovery of omecamtiv mecarbil the first, selective, small molecule activator of cardiac myosin. ACS Med. Chem. Lett. 1, 472–477 (2010).
Liu, Y., White, H. D., Belknap, B., Winkelmann, D. A. & Forgacs, E. Omecamtiv mecarbil modulates the kinetic and motile properties of porcine β-cardiac myosin. Biochemistry 54, 1963–1975 (2015).
Rohde, J., Thomas, D. & Muretta, J. Heart failure drug changes the mechanoenzymology of the cardiac myosin powerstroke. Proc. Natl Acad. Sci. USA 114, E1796–E1804 (2017).
Swenson, A. M. et al. Omecamtiv mecarbil enhances the duty ratio of human β-cardiac myosin resulting in increased calcium sensitivity and slowed force development in cardiac muscle. J. Biol. Chem. 292, 3768–3778 (2017).
Woody, M. S. et al. Positive cardiac inotrope omecamtiv mecarbil activates muscle despite suppressing the myosin working stroke. Nat. Commun. 9, 3838 (2018).
Gollapudi, S. et al. Two classes of myosin inhibitors, blebbistatin, and mavacamten, stabilize β-cardiac myosin in different structural and functional states. J. Mol. Biol. 433, 167295 (2021).
Planelles-Herrero, V., Hartman, J., Robert-Paganin, J., Malik, F. & Houdusse, A. Mechanistic and structural basis for activation of cardiac myosin force production by omecamtiv mecarbil. Nat. Commun. 8, 190 (2017).
McKillop, D. F. & Geeves, M. A. Regulation of the interaction between actin and myosin subfragment 1: evidence for three states of the thin filament. Biophys. J. 65, 693–701 (1993).
Bakkehaug, J. P. et al. Myosin activator omecamtiv mecarbil increases myocardial oxygen consumption and impairs cardiac efficiency mediated by resting myosin atpase activity. Circ. Heart Fail. 8, 766–775 (2015).
Shen, Y. T. et al. Improvement of cardiac function by a cardiac myosin activator in conscious dogs with systolic heart failure. Circ. Heart Fail. 3, 522–527 (2010).
Teerlink, J. R. et al. Dose-dependent augmentation of cardiac systolic function with the selective cardiac myosin activator, omecamtiv mecarbil: a first-in-man study. Lancet 378, 667–675 (2011).
Teerlink, J. et al. Chronic oral study of myosin activation to increase contractility in heart failure (COSMIC-HF): a phase 2, pharmacokinetic, randomised, placebo-controlled trial. Lancet 388, 2895–2903 (2016).
Biering-Sørensen, T. et al. The effect of the cardiac myosin activator, omecamtiv mecarbil, on right ventricular structure and function in chronic systolic heart failure (COSMIC-HF). Eur. J. Heart Fail. 23, 1052–1056 (2021).
Guazzi, M., Bandera, F., Ozemek, C., Systrom, D. & Arena, R. Cardiopulmonary exercise testing: what is its value? J. Am. Coll. Cardiol. 70, 1618–1636 (2017).
Teerlink, J. R. et al. Effect of ejection fraction on clinical outcomes in patients treated with omecamtiv mecarbil in GALACTIC-HF. J. Am. Coll. Cardiol. 78, 97–108 (2021).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03759392 (2022).
Teerlink, J. R. et al. Cardiac myosin activation with omecamtiv mecarbil in systolic heart failure. N. Engl. J. Med. 384, 105–116 (2021).
Felker, G. et al. Assessment of omecamtiv mecarbil for the treatment of patients with severe heart failure. a post hoc analysis of data from the GALACTIC-HF randomized clinical trial. JAMA Cardiol. 7, 26–34 (2021).
Fernandes, S. et al. MYK-491, a novel small-molecule cardiac myosin activator increases cardiac systolic function and preserves mechanical efficiency: pre-clinical in vivo and in vitro evidence [abstract]. Circulation 140, A15707 (2019).
Bell, K., Anto, A. R., Anderson, R. L., Del Rio, C. L. & Henze, M. Cardiac muscle activation: the role of length dependent activation and the novel myosin activator danicamtiv. Eur. Heart J. 41 (Suppl. 2), ehaa946.3681 (2020).
Shen, S., Sewanan, L. R., Jacoby, D. L. & Campbell, S. G. Danicamtiv enhances systolic function and Frank-Starling behavior at minimal diastolic cost in engineered human myocardium. J. Am. Heart Assoc. 10, e020860 (2021).
Voors, A. et al. Effects of danicamtiv, a novel cardiac myosin activator, in heart failure with reduced ejection fraction: experimental data and clinical results from a phase 2a trial. Eur. J. Heart Fail. 22, 1649–1658 (2020).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT04572893 (2021).
Zhang, R., Zhao, J. & Potter, J. D. Phosphorylation of both serine residues in cardiac troponin I is required to decrease the Ca2+ affinity of cardiac troponin C. J. Biol. Chem. 270, 30773–30780 (1995).
Kentish, J. C. et al. Phosphorylation of troponin I by protein kinase A accelerates relaxation and crossbridge cycle kinetics in mouse ventricular muscle. Circ. Res. 88, 1059–1065 (2001).
Ommen, S. et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation 142, e558–e631 (2020).
Hidaka, H. et al. Calcium-regulated modulator protein interacting agents inhibit smooth muscle calcium-stimulated protein kinase and ATPase. Mol. Pharmacol. 17, 66–72 (1980).
Silver, P. J., Pinto, P. B. & Dachiw, J. Modulation of vascular and cardiac contractile protein regulatory mechanisms by calmodulin inhibitors and related compounds. Biochem. Pharmacol. 35, 2545–2551 (1986).
Osawa, M. et al. Solution structure of calmodulin-W-7 complex: the basis of diversity in molecular recognition. J. Mol. Biol. 276, 165–176 (1998).
Thompson, B. R., Martindale, J. & Metzger, J. M. Sarcomere neutralization in inherited cardiomyopathy: small-molecule proof-of-concept to correct hyper-Ca2+-sensitive myofilaments. Am. J. Physiol. Heart Circ. Physiol. 311, H36–H43 (2016).
Kawas, R. F. et al. A small-molecule modulator of cardiac myosin acts on multiple stages of the myosin chemomechanical cycle. J. Biol. Chem. 292, 16571–16577 (2017).
del Rio, C. L. et al. In vivo cardiac effects of mavacamten (MYK-461): evidence for negative inotropy and improved compliance [abstract]. Circulation 136, A20593 (2017).
Stern, J. et al. A small molecule inhibitor of sarcomere contractility acutely relieves left ventricular outflow tract obstruction in feline hypertrophic cardiomyopathy. PLoS ONE 11, e0168407 (2016).
Sewanan, L., Shen, S. & Campbell, S. Mavacamten preserves length-dependent contractility and improves diastolic function in human engineered heart tissue. Am. J. Physiol. Heart Circ. Physiol. 320, H1112–H1123 (2021).
Awinda, P. et al. Effects of mavacamten on Ca2+ sensitivity of contraction as sarcomere length varied in human myocardium. Br. J. Pharmacol. 177, 5609–5621 (2020).
Awinda, P. et al. Mavacamten decreases maximal force and Ca2+ sensitivity in the N47K-myosin regulatory light chain mouse model of hypertrophic cardiomyopathy. Am. J. Physiol. Heart Circ. Physiol. 320, H881–H890 (2021).
Toepfer, C. et al. Hypertrophic cardiomyopathy mutations in MYBPC3 dysregulate myosin. Sci. Transl Med. 11, eaat1199 (2019).
Sparrow, A., Watkins, H., Daniels, M., Redwood, C. & Robinson, P. Mavacamten rescues increased myofilament calcium sensitivity and dysregulation of Ca2+ flux caused by thin filament hypertrophic cardiomyopathy mutations. Am. J. Physiol. Heart Circ. Physiol. 318, H715–H722 (2020).
Ho, C. et al. Evaluation of mavacamten in symptomatic patients with nonobstructive hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 75, 2649–2660 (2020).
Heitner, S. et al. Mavacamten treatment for obstructive hypertrophic cardiomyopathy: a clinical trial. Ann. Intern. Med. 170, 741–748 (2019).
Ho, C. et al. Study design and rationale of EXPLORER-HCM: evaluation of mavacamten in adults with symptomatic obstructive hypertrophic cardiomyopathy. Circ. Heart Fail. 13, e006853 (2020).
Olivotto, I. et al. Mavacamten for treatment of symptomatic obstructive hypertrophic cardiomyopathy (EXPLORER-HCM): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 396, 759–769 (2020).
Saberi, S. et al. Mavacamten favorably impacts cardiac structure in obstructive hypertrophic cardiomyopathy: EXPLORER-HCM cardiac magnetic resonance substudy analysis. Circulation 143, 606–608 (2021).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03723655 (2021).
Owens, A. et al. Long-term efficacy and safety of mavacamten in patients with non-obstructive hypertrophic cardiomyopathy: interim results from the MAVERICK-LTE cohort of the MAVA-LTE study [abstract]. Circulation 144, A9685 (2021).
Grillo, M. P. et al. In vitro and in vivo pharmacokinetic characterization of mavacamten, a first-in-class small molecule allosteric modulator of beta cardiac myosin. Xenobiotica 49, 718–733 (2019).
del Rio, C. L. et al. Chronic treatment with a mavacamten-like myosin-modulator (MYK-581) blunts disease progression in a mini-pig genetic model of non-obstructed hypertrophic cardiomyopathy: in vivo evidence for improved relaxation and functional reserve [abstract]. Circulation 140, A14585 (2019).
Ferguson, B. S. et al. Acute effects of a mavacamten-like myosin-inhibitor MYK-581 in a feline model of obstructed hypertrophic cardiomyopathy: evidence of improved ventricular filling (beyond obstruction reprieve). Eur. Heart J. 41 (Suppl. 2), ehaa946.3713 (2020).
Australian New Zealand Clinical Trials Registry. ANZCTR https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=378908 (2021).
Allingham, J., Smith, R. & Rayment, I. The structural basis of blebbistatin inhibition and specificity for myosin II. Nat. Struct. Mol. Biol. 12, 378–379 (2005).
Wilson, C., Naber, N., Pate, E. & Cooke, R. The myosin inhibitor blebbistatin stabilizes the super-relaxed state in skeletal muscle. Biophys. J. 107, 1637–1646 (2014).
Chuang, C. et al. Discovery of aficamten (CK-274), a next-generation cardiac myosin inhibitor for the treatment of hypertrophic cardiomyopathy. J. Med. Chem. 64, 14142–14152 (2021).
Hwee, D. et al. Pharmacologic characterization of the cardiac myosin inhibitor, CK-3773274: a potential therapeutic approach for hypertrophic cardiomyopathy [abstract]. Circ. Res. 125, A332 (2019).
Hartman, J. et al. Characterization of the cardiac myosin inhibitor CK-3773274: a potential therapeutic approach for hypertrophic cardiomyopathy. Biophys. J. 118, 596a (2020).
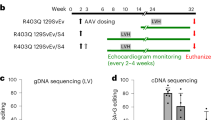
Hwee, D. et al. The cardiac myosin inhibitor, CK-3773274, reduces contractility in the R403q mouse model of hypertrophic cardiomyopathy [abstract]. Circ. Res. 125, A615 (2019).
Cremin, P. et al. In vivo pharmacokinetic characterization of CK-3773274, a novel cardiac myosin inhibitor. AAPS 304702, 887215 (2020).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT04219826 (2021).
BioSpace. Cytokinetics announces positive topline results from cohort 3 of REDWOOD-HCM. BioSpace https://www.biospace.com/article/releases/cytokinetics-announces-positive-topline-results-from-cohort-3-of-redwood-hcm (2022).
Cytokinetics. Cytokinetics announces positive topline results of REDWOOD-HCM. Cytokinetics https://ir.cytokinetics.com/news-releases/news-release-details/cytokinetics-announces-positive-topline-results-redwood-hcm (2021).
Fordyce, C. et al. Cardiovascular drug development: is it dead or just hibernating? J. Am. Coll. Cardiol. 65, 1567–1582 (2015).
Tucholski, T. et al. Distinct hypertrophic cardiomyopathy genotypes result in convergent sarcomeric proteoform profiles revealed by top-down proteomics. Proc. Natl Acad. Sci. USA 117, 24691–24700 (2020).
Bunch, T. et al. Cardiac myosin-binding protein C interaction with actin is inhibited by compounds identified in a high-throughput fluorescence lifetime screen. J. Biol. Chem. 297, 100840 (2021).
Nag, S. & Trivedi, D. To lie or not to lie: super-relaxing with myosins. eLife 10, e63703 (2021).
Author information
Authors and Affiliations
Contributions
The authors contributed substantially to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
S.J.L. is currently a part-time employee of Edgewise Therapeutics. L.A.L. is on the scientific advisory board and has a sponsored research agreement with Bristol Myers Squibb/MyoKardia. C.C. declares no competing interests.
Peer review
Peer review information
Nature Reviews Cardiology thanks Sharlene Day, Ahmad Masri and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lehman, S.J., Crocini, C. & Leinwand, L.A. Targeting the sarcomere in inherited cardiomyopathies. Nat Rev Cardiol 19, 353–363 (2022). https://doi.org/10.1038/s41569-022-00682-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-022-00682-0
This article is cited by
-
Danicamtiv affected isometric force and cross-bridge kinetics similarly in skinned myocardial strips from male and female rats
Journal of Muscle Research and Cell Motility (2024)
-
Multi-parametric non-contrast cardiac magnetic resonance for the differentiation between cardiac amyloidosis and hypertrophic cardiomyopathy
Clinical Research in Cardiology (2024)
-
Discovery of novel cardiac troponin activators using fluorescence polarization-based high throughput screening assays
Scientific Reports (2023)
-
α-myosin heavy chain lactylation maintains sarcomeric structure and function and alleviates the development of heart failure
Cell Research (2023)
-
Detection of subclinical hypertrophic cardiomyopathy
Nature Reviews Cardiology (2023)