Abstract
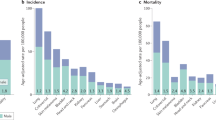
Sex differences are present across multiple non-reproductive organ cancers, with male individuals generally experiencing higher incidence of cancer with poorer outcomes. Although some mechanisms underlying these differences are emerging, the immunological basis is not well understood. Observations from clinical trials also suggest a sex bias in conventional immunotherapies with male individuals experiencing a more favourable response and female individuals experiencing more severe adverse events to immune checkpoint blockade. In this Perspective article, we summarize the major biological hallmarks underlying sex bias in immuno-oncology. We focus on signalling from sex hormones and chromosome-encoded gene products, along with sex hormone-independent and chromosome-independent epigenetic mechanisms in tumour and immune cells such as myeloid cells and T cells. Finally, we highlight opportunities for future studies on sex differences that integrate sex hormones and chromosomes and other emerging cancer hallmarks such as ageing and the microbiome to provide a more comprehensive view of how sex differences underlie the response in cancer that can be leveraged for more effective immuno-oncology approaches.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Haupt, S., Caramia, F., Klein, S. L., Rubin, J. B. & Haupt, Y. Sex disparities matter in cancer development and therapy. Nat. Rev. Cancer 21, 393–407 (2021).
Clocchiatti, A., Cora, E., Zhang, Y. & Dotto, G. P. Sexual dimorphism in cancer. Nat. Rev. Cancer 16, 330–339 (2016).
Schafer, J. M. et al. Sex-biased adaptive immune regulation in cancer development and therapy. iScience 25, 104717 (2022).
Yang, C. et al. Androgen receptor-mediated CD8+ T cell stemness programs drive sex differences in antitumor immunity. Immunity 55, 1268–1283.e9 (2022).
Bayik, D. et al. Myeloid-derived suppressor cell subsets drive glioblastoma growth in a sex-specific manner. Cancer Discov. 10, 1210–1225 (2020).
Klein, S. L. & Flanagan, K. L. Sex differences in immune responses. Nat. Rev. Immunol. 16, 626–638 (2016).
Lee, J. et al. Sex-biased T-cell exhaustion drives differential immune responses in glioblastoma. Cancer Discov. 13, 2090–2105 (2023).
Kwon, H. et al. Androgen conspires with the CD8+ T cell exhaustion program and contributes to sex bias in cancer. Sci. Immunol. 7, eabq2630 (2022).
Guan, X. et al. Androgen receptor activity in T cells limits checkpoint blockade efficacy. Nature 606, 791–796 (2022).
Al-Attar, A., Presnell, S. R., Peterson, C. A., Thomas, D. T. & Lutz, C. T. The effect of sex on immune cells in healthy aging: elderly women have more robust natural killer lymphocytes than do elderly men. Mech. Ageing Dev. 156, 25–33 (2016).
Huang, Z. et al. Effects of sex and aging on the immune cell landscape as assessed by single-cell transcriptomic analysis. Proc. Natl Acad. Sci. USA 118, e2023216116 (2021).
Ozdemir, B. C. & Dotto, G. P. Sex hormones and anticancer immunity. Clin. Cancer Res. 25, 4603–4610 (2019).
Edwards, M., Dai, R. & Ahmed, S. A. Our environment shapes us: the importance of environment and sex differences in regulation of autoantibody production. Front. Immunol. 9, 478 (2018).
Tiniakou, E., Costenbader, K. H. & Kriegel, M. A. Sex-specific environmental influences on the development of autoimmune diseases. Clin. Immunol. 149, 182–191 (2013).
Tan, M. H., Li, J., Xu, H. E., Melcher, K. & Yong, E. L. Androgen receptor: structure, role in prostate cancer and drug discovery. Acta Pharmacol. Sin. 36, 3–23 (2015).
Benten, W. P. et al. Functional testosterone receptors in plasma membranes of T cells. FASEB J. 13, 123–133 (1999).
Benten, W. P., Becker, A., Schmitt-Wrede, H. P. & Wunderlich, F. Developmental regulation of intracellular and surface androgen receptors in T cells. Steroids 67, 925–931 (2002).
Viselli, S. M., Reese, K. R., Fan, J., Kovacs, W. J. & Olsen, N. J. Androgens alter B cell development in normal male mice. Cell. Immunol. 182, 99–104 (1997).
Lai, J. J. et al. Monocyte/macrophage androgen receptor suppresses cutaneous wound healing in mice by enhancing local TNF-α expression. J. Clin. Invest. 119, 3739–3751 (2009).
Abu, E. O., Horner, A., Kusec, V., Triffitt, J. T. & Compston, J. E. The localization of androgen receptors in human bone. J. Clin. Endocrinol. Metab. 82, 3493–3497 (1997).
Chuang, K. H. et al. Neutropenia with impaired host defense against microbial infection in mice lacking androgen receptor. J. Exp. Med. 206, 1181–1199 (2009).
Khetawat, G. et al. Human megakaryocytes and platelets contain the estrogen receptor β and androgen receptor (AR): testosterone regulates AR expression. Blood 95, 2289–2296 (2000).
Zhang, X. et al. Androgen signaling contributes to sex differences in cancer by inhibiting NF-κB activation in T cells and suppressing antitumor immunity. Cancer Res. 83, 906–921 (2023).
Lefebvre, C. et al. A human B-cell interactome identifies MYB and FOXM1 as master regulators of proliferation in germinal centers. Mol. Syst. Biol. 6, 377 (2010).
Alvarez, M. J. et al. Functional characterization of somatic mutations in cancer using network-based inference of protein activity. Nat. Genet. 48, 838–847 (2016).
Heemers, H. V. & Tindall, D. J. Androgen receptor (AR) coregulators: a diversity of functions converging on and regulating the AR transcriptional complex. Endocr. Rev. 28, 778–808 (2007).
Kissick, H. T. et al. Androgens alter T-cell immunity by inhibiting T-helper 1 differentiation. Proc. Natl Acad. Sci. USA 111, 9887–9892 (2014).
Liva, S. M. & Voskuhl, R. R. Testosterone acts directly on CD4+ T lymphocytes to increase IL-10 production. J. Immunol. 167, 2060–2067 (2001).
Fijak, M. et al. Testosterone replacement effectively inhibits the development of experimental autoimmune orchitis in rats: evidence for a direct role of testosterone on regulatory T cell expansion. J. Immunol. 186, 5162–5172 (2011).
Walecki, M. et al. Androgen receptor modulates Foxp3 expression in CD4+CD25+Foxp3+ regulatory T-cells. Mol. Biol. Cell 26, 2845–2857 (2015).
Obradovic, A. Z. et al. T-cell infiltration and adaptive Treg resistance in response to androgen deprivation with or without vaccination in localized prostate cancer. Clin. Cancer Res. 26, 3182–3192 (2020).
Tang, S., Moore, M. L., Grayson, J. M. & Dubey, P. Increased CD8+ T-cell function following castration and immunization is countered by parallel expansion of regulatory T cells. Cancer Res. 72, 1975–1985 (2012).
Liu, Q. et al. Targeting the androgen receptor to enhance NK cell killing efficacy in bladder cancer by modulating ADAR2/circ_0001005/PD-L1 signaling. Cancer Gene Ther. 29, 1988–2000 (2022).
Tang, M. et al. High dose androgen suppresses natural killer cytotoxicity of castration-resistant prostate cancer cells via altering AR/circFKBP5/miRNA-513a-5p/PD-L1 signals. Cell Death Dis. 13, 746 (2022).
Shi, L. et al. Targeting androgen receptor (AR)–>IL12A signal enhances efficacy of sorafenib plus NK cells immunotherapy to better suppress HCC progression. Mol. Cancer Ther. 15, 731–742 (2016).
Izumi, K. et al. Targeting the androgen receptor with siRNA promotes prostate cancer metastasis through enhanced macrophage recruitment via CCL2/CCR2-induced STAT3 activation. EMBO Mol. Med. 5, 1383–1401 (2013).
Fang, L. Y. et al. Infiltrating macrophages promote prostate tumorigenesis via modulating androgen receptor-mediated CCL4-STAT3 signaling. Cancer Res. 73, 5633–5646 (2013).
Alsamraae, M. et al. Androgen receptor inhibition suppresses anti-tumor neutrophil response against bone metastatic prostate cancer via regulation of TβRI expression. Cancer Lett. https://doi.org/10.1016/j.canlet.2023.216468 (2023).
Markman, J. L. et al. Loss of testosterone impairs anti-tumor neutrophil function. Nat. Commun. 11, 1613 (2020).
Cioni, B. et al. Androgen receptor signalling in macrophages promotes TREM-1-mediated prostate cancer cell line migration and invasion. Nat. Commun. 11, 4498 (2020).
Koh, Y. T., Gray, A., Higgins, S. A., Hubby, B. & Kast, W. M. Androgen ablation augments prostate cancer vaccine immunogenicity only when applied after immunization. Prostate 69, 571–584 (2009).
Corrales, J. J. et al. Enhanced immunological response by dendritic cells in male hypogonadism. Eur. J. Clin. Invest. 42, 1205–1212 (2012).
Hepworth, M. R., Hardman, M. J. & Grencis, R. K. The role of sex hormones in the development of Th2 immunity in a gender-biased model of Trichuris muris infection. Eur. J. Immunol. 40, 406–416 (2010).
Marino, M., Galluzzo, P. & Ascenzi, P. Estrogen signaling multiple pathways to impact gene transcription. Curr. Genomics 7, 497–508 (2006).
O’Malley, B. W. A life-long search for the molecular pathways of steroid hormone action. Mol. Endocrinol. 19, 1402–1411 (2005).
Le Dily, F. & Beato, M. Signaling by steroid hormones in the 3D nuclear space. Int. J. Mol. Sci. 19, 306 (2018).
Klinge, C. M. Estrogen receptor interaction with estrogen response elements. Nucleic Acids Res. 29, 2905–2919 (2001).
Filardo, E. et al. Activation of the novel estrogen receptor G protein-coupled receptor 30 (GPR30) at the plasma membrane. Endocrinology 148, 3236–3245 (2007).
Filardo, E. J. & Thomas, P. Minireview: G protein-coupled estrogen receptor-1, GPER-1: its mechanism of action and role in female reproductive cancer, renal and vascular physiology. Endocrinology 153, 2953–2962 (2012).
Molina, L., Figueroa, C. D., Bhoola, K. D. & Ehrenfeld, P. GPER-1/GPR30 a novel estrogen receptor sited in the cell membrane: therapeutic coupling to breast cancer. Expert Opin. Ther. Targets 21, 755–766 (2017).
Losel, R. & Wehling, M. Nongenomic actions of steroid hormones. Nat. Rev. Mol. Cell Biol. 4, 46–56 (2003).
Barton, M. et al. Twenty years of the G protein-coupled estrogen receptor GPER: historical and personal perspectives. J. Steroid Biochem. Mol. Biol. 176, 4–15 (2018).
Majumdar, S. et al. Differential actions of estrogen receptor α and β via nongenomic signaling in human prostate stem and progenitor cells. Endocrinology 160, 2692–2708 (2019).
Laffont, S. et al. X-chromosome complement and estrogen receptor signaling independently contribute to the enhanced TLR7-mediated IFN-α production of plasmacytoid dendritic cells from women. J. Immunol. 193, 5444–5452 (2014).
Phiel, K. L., Henderson, R. A., Adelman, S. J. & Elloso, M. M. Differential estrogen receptor gene expression in human peripheral blood mononuclear cell populations. Immunol. Lett. 97, 107–113 (2005).
Grimaldi, C. M., Cleary, J., Dagtas, A. S., Moussai, D. & Diamond, B. Estrogen alters thresholds for B cell apoptosis and activation. J. Clin. Invest. 109, 1625–1633 (2002).
Curran, E. M. et al. Natural killer cells express estrogen receptor-α and estrogen receptor-β and can respond to estrogen via a non-estrogen receptor-α-mediated pathway. Cell. Immunol. 214, 12–20 (2001).
Lambert, K. C., Curran, E. M., Judy, B. M., Lubahn, D. B. & Estes, D. M. Estrogen receptor-α deficiency promotes increased TNF-α secretion and bacterial killing by murine macrophages in response to microbial stimuli in vitro. J. Leukoc. Biol. 75, 1166–1172 (2004).
Ribas, V. et al. Myeloid-specific estrogen receptor α deficiency impairs metabolic homeostasis and accelerates atherosclerotic lesion development. Proc. Natl Acad. Sci. USA 108, 16457–16462 (2011).
Calippe, B. et al. 17β-Estradiol promotes TLR4-triggered proinflammatory mediator production through direct estrogen receptor α signaling in macrophages in vivo. J. Immunol. 185, 1169–1176 (2010).
Kovats, S. & Carreras, E. Regulation of dendritic cell differentiation and function by estrogen receptor ligands. Cell. Immunol. 252, 81–90 (2008).
Paharkova-Vatchkova, V., Maldonado, R. & Kovats, S. Estrogen preferentially promotes the differentiation of CD11c+ CD11bintermediate dendritic cells from bone marrow precursors. J. Immunol. 172, 1426–1436 (2004).
Mao, A., Paharkova-Vatchkova, V., Hardy, J., Miller, M. M. & Kovats, S. Estrogen selectively promotes the differentiation of dendritic cells with characteristics of Langerhans cells. J. Immunol. 175, 5146–5151 (2005).
Lelu, K. et al. Estrogen receptor α signaling in T lymphocytes is required for estradiol-mediated inhibition of Th1 and Th17 cell differentiation and protection against experimental autoimmune encephalomyelitis. J. Immunol. 187, 2386–2393 (2011).
Karpuzoglu, E., Phillips, R. A., Gogal, R. M. Jr & Ansar Ahmed, S. IFN-γ-inducing transcription factor, T-bet is upregulated by estrogen in murine splenocytes: role of IL-27 but not IL-12. Mol. Immunol. 44, 1808–1814 (2007).
Maret, A. et al. Estradiol enhances primary antigen-specific CD4 T cell responses and Th1 development in vivo. Essential role of estrogen receptor α expression in hematopoietic cells. Eur. J. Immunol. 33, 512–521 (2003).
Fox, H. S., Bond, B. L. & Parslow, T. G. Estrogen regulates the IFN-γ promoter. J. Immunol. 146, 4362–4367 (1991).
Polanczyk, M. J. et al. Cutting edge: estrogen drives expansion of the CD4+CD25+ regulatory T cell compartment. J. Immunol. 173, 2227–2230 (2004).
Prieto, G. A. & Rosenstein, Y. Oestradiol potentiates the suppressive function of human CD4 CD25 regulatory T cells by promoting their proliferation. Immunology 118, 58–65 (2006).
Fuseini, H. et al. ERα signaling increased IL-17A production in Th17 cells by upregulating IL-23R expression, mitochondrial respiration, and proliferation. Front. Immunol. 10, 2740 (2019).
Chen, R. Y. et al. Estradiol inhibits Th17 cell differentiation through inhibition of RORγT transcription by recruiting the ERα/REA complex to estrogen response elements of the RORγT promoter. J. Immunol. 194, 4019–4028 (2015).
Tyagi, A. M. et al. Estrogen deficiency induces the differentiation of IL-17 secreting Th17 cells: a new candidate in the pathogenesis of osteoporosis. PLoS ONE 7, e44552 (2012).
Newcomb, D. C. et al. Estrogen and progesterone decrease let-7f microRNA expression and increase IL-23/IL-23 receptor signaling and IL-17A production in patients with severe asthma. J. Allergy Clin. Immunol. 136, 1025–1034.e11 (2015).
Chakir, J. et al. Airway remodeling-associated mediators in moderate to severe asthma: effect of steroids on TGF-β, IL-11, IL-17, and type I and type III collagen expression. J. Allergy Clin. Immunol. 111, 1293–1298 (2003).
Molet, S. et al. IL-17 is increased in asthmatic airways and induces human bronchial fibroblasts to produce cytokines. J. Allergy Clin. Immunol. 108, 430–438 (2001).
Al-Ramli, W. et al. TH17-associated cytokines (IL-17A and IL-17F) in severe asthma. J. Allergy Clin. Immunol. 123, 1185–1187 (2009).
Kim, D. H. et al. Estrogen receptor α in T cells suppresses follicular helper T cell responses and prevents autoimmunity. Exp. Mol. Med. 51, 1–9 (2019).
Mohammad, I. et al. Estrogen receptor α contributes to T cell-mediated autoimmune inflammation by promoting T cell activation and proliferation. Sci. Signal. 11, eaap9415 (2018).
Yuan, B. et al. Estrogen receptor β signaling in CD8+ T cells boosts T cell receptor activation and antitumor immunity through a phosphotyrosine switch. J. Immunother. Cancer 9, e001932 (2021).
Hill, L., Jeganathan, V., Chinnasamy, P., Grimaldi, C. & Diamond, B. Differential roles of estrogen receptors α and β in control of B-cell maturation and selection. Mol. Med. 17, 211–220 (2011).
Chung, H. H. et al. Estrogen reprograms the activity of neutrophils to foster protumoral microenvironment during mammary involution. Sci. Rep. 7, 46485 (2017).
Lyons, T. R. et al. Postpartum mammary gland involution drives progression of ductal carcinoma in situ through collagen and COX-2. Nat. Med. 17, 1109–1115 (2011).
Lyons, T. R. et al. Cyclooxygenase-2-dependent lymphangiogenesis promotes nodal metastasis of postpartum breast cancer. J. Clin. Invest. 124, 3901–3912 (2014).
Svoronos, N. et al. Tumor cell-independent estrogen signaling drives disease progression through mobilization of myeloid-derived suppressor cells. Cancer Discov. 7, 72–85 (2017).
Milette, S. et al. Sexual dimorphism and the role of estrogen in the immune microenvironment of liver metastases. Nat. Commun. 10, 5745 (2019).
Ham, B. et al. TNF receptor-2 facilitates an immunosuppressive microenvironment in the liver to promote the colonization and growth of hepatic metastases. Cancer Res. 75, 5235–5247 (2015).
Kozasa, K. et al. Estrogen stimulates female cancer progression by inducing myeloid-derived suppressive cells: investigations on pregnant and non-pregnant experimental models. Oncotarget 10, 1887–1902 (2019).
Ouyang, L. et al. Estrogen-induced SDF-1α production promotes the progression of ER-negative breast cancer via the accumulation of MDSCs in the tumor microenvironment. Sci. Rep. 6, 39541 (2016).
Chakraborty, B. et al. Inhibition of estrogen signaling in myeloid cells increases tumor immunity in melanoma. J. Clin. Invest. 131, e151347 (2021).
Hao, S., Li, P., Zhao, J., Hu, Y. & Hou, Y. 17β-Estradiol suppresses cytotoxicity and proliferative capacity of murine splenic NK1.1+ cells. Cell Mol. Immunol. 5, 357–364 (2008).
Diefenbach, A., Jensen, E. R., Jamieson, A. M. & Raulet, D. H. Rae1 and H60 ligands of the NKG2D receptor stimulate tumour immunity. Nature 413, 165–171 (2001).
Cerwenka, A., Baron, J. L. & Lanier, L. L. Ectopic expression of retinoic acid early inducible-1 gene (RAE-1) permits natural killer cell-mediated rejection of a MHC class I-bearing tumor in vivo. Proc. Natl Acad. Sci. USA 98, 11521–11526 (2001).
Karre, K., Ljunggren, H. G., Piontek, G. & Kiessling, R. Selective rejection of H-2-deficient lymphoma variants suggests alternative immune defence strategy. Nature 319, 675–678 (1986).
Seaman, W. E., Sleisenger, M., Eriksson, E. & Koo, G. C. Depletion of natural killer cells in mice by monoclonal antibody to NK-1.1. Reduction in host defense against malignancy without loss of cellular or humoral immunity. J. Immunol. 138, 4539–4544 (1987).
Siiteri, P. K. et al. Progesterone and maintenance of pregnancy: is progesterone nature’s immunosuppressant? Ann. N. Y. Acad. Sci. 286, 384–397 (1977).
Piccinni, M. P. et al. Progesterone favors the development of human T helper cells producing Th2-type cytokines and promotes both IL-4 production and membrane CD30 expression in established Th1 cell clones. J. Immunol. 155, 128–133 (1995).
Hellberg, S. et al. Progesterone dampens immune responses in in vitro activated CD4+ T cells and affects genes associated with autoimmune diseases that improve during pregnancy. Front. Immunol. 12, 672168 (2021).
Yao, Y., Li, H., Ding, J., Xia, Y. & Wang, L. Progesterone impairs antigen-non-specific immune protection by CD8 T memory cells via interferon-γ gene hypermethylation. PLoS Pathog. 13, e1006736 (2017).
Lee, J. H., Ulrich, B., Cho, J., Park, J. & Kim, C. H. Progesterone promotes differentiation of human cord blood fetal T cells into T regulatory cells but suppresses their differentiation into Th17 cells. J. Immunol. 187, 1778–1787 (2011).
Monin, L. et al. γδ T cells compose a developmentally regulated intrauterine population and protect against vaginal candidiasis. Mucosal Immunol. 13, 969–981 (2020).
Werner, L. R. et al. Progesterone promotes immunomodulation and tumor development in the murine mammary gland. J. Immunother. Cancer 9, e001710 (2021).
Zhang, L., Chang, K. K., Li, M. Q., Li, D. J. & Yao, X. Y. Mouse endometrial stromal cells and progesterone inhibit the activation and regulate the differentiation and antibody secretion of mouse B cells. Int. J. Clin. Exp. Pathol. 7, 123–133 (2014).
Canellada, A., Blois, S., Gentile, T. & Margni Idehu, R. A. In vitro modulation of protective antibody responses by estrogen, progesterone and interleukin-6. Am. J. Reprod. Immunol. 48, 334–343 (2002).
Pauklin, S. & Petersen-Mahrt, S. K. Progesterone inhibits activation-induced deaminase by binding to the promoter. J. Immunol. 183, 1238–1244 (2009).
Medina, K. L. & Kincade, P. W. Pregnancy-related steroids are potential negative regulators of B lymphopoiesis. Proc. Natl Acad. Sci. USA 91, 5382–5386 (1994).
Hall, O. J. et al. Progesterone-based contraceptives reduce adaptive immune responses and protection against sequential influenza A virus infections. J. Virol. 91, e02160-16 (2017).
Buyon, J. P., Korchak, H. M., Rutherford, L. E., Ganguly, M. & Weissmann, G. Female hormones reduce neutrophil responsiveness in vitro. Arthritis Rheum. 27, 623–630 (1984).
Roth, J. A., Kaeberle, M. L. & Hsu, W. H. Effect of estradiol and progesterone on lymphocyte and neutrophil functions in steers. Infect. Immun. 35, 997–1002 (1982).
Menzies, F. M., Henriquez, F. L., Alexander, J. & Roberts, C. W. Selective inhibition and augmentation of alternative macrophage activation by progesterone. Immunology 134, 281–291 (2011).
Butts, C. L. et al. Progesterone inhibits mature rat dendritic cells in a receptor-mediated fashion. Int. Immunol. 19, 287–296 (2007).
Jones, L. A. et al. Differential modulation of TLR3- and TLR4-mediated dendritic cell maturation and function by progesterone. J. Immunol. 185, 4525–4534 (2010).
Arruvito, L. et al. NK cells expressing a progesterone receptor are susceptible to progesterone-induced apoptosis. J. Immunol. 180, 5746–5753 (2008).
Oettel, M. & Mukhopadhyay, A. K. Progesterone: the forgotten hormone in men? Aging Male 7, 236–257 (2004).
Boumil, R. M. & Lee, J. T. Forty years of decoding the silence in X-chromosome inactivation. Hum. Mol. Genet. 10, 2225–2232 (2001).
Heard, E., Chaumeil, J., Masui, O. & Okamoto, I. Mammalian X-chromosome inactivation: an epigenetics paradigm. Cold Spring Harb. Symp. Quant. Biol. 69, 89–102 (2004).
Tukiainen, T. et al. Landscape of X chromosome inactivation across human tissues. Nature 550, 244–248 (2017).
Carrel, L. & Willard, H. F. X-inactivation profile reveals extensive variability in X-linked gene expression in females. Nature 434, 400–404 (2005).
Cotton, A. M. et al. Analysis of expressed SNPs identifies variable extents of expression from the human inactive X chromosome. Genome Biol. 14, R122 (2013).
Anderson, C. L. & Brown, C. J. Polymorphic X-chromosome inactivation of the human TIMP1 gene. Am. J. Hum. Genet. 65, 699–708 (1999).
Souyris, M., Mejia, J. E., Chaumeil, J. & Guery, J. C. Female predisposition to TLR7-driven autoimmunity: gene dosage and the escape from X chromosome inactivation. Semin. Immunopathol. 41, 153–164 (2019).
Kaneko, S. & Li, X. X chromosome protects against bladder cancer in females via a KDM6A-dependent epigenetic mechanism. Sci. Adv. 4, eaar5598 (2018).
Mousavi, M. J., Mahmoudi, M. & Ghotloo, S. Escape from X chromosome inactivation and female bias of autoimmune diseases. Mol. Med. 26, 127 (2020).
Dou, D. R. et al. Xist ribonucleoproteins promote female sex-biased autoimmunity. Cell 187, 733–749.e16 (2024).
Jenks, S. A. et al. Distinct effector B cells induced by unregulated Toll-like receptor 7 contribute to pathogenic responses in systemic lupus erythematosus. Immunity 49, 725–739.e6 (2018).
Gao, X. & Cockburn, I. A. The development and function of CD11c+ atypical B cells — insights from single cell analysis. Front. Immunol. 13, 979060 (2022).
Tang, Z., Kang, B., Li, C., Chen, T. & Zhang, Z. GEPIA2: an enhanced web server for large-scale expression profiling and interactive analysis. Nucleic Acids Res. 47, W556–W560 (2019).
Han, W. et al. Pan-cancer analysis of lncRNA XIST and its potential mechanisms in human cancers. Heliyon 8, e10786 (2022).
Swerdlow, A. J. et al. Cancer incidence and mortality in men with Klinefelter syndrome: a cohort study. J. Natl Cancer Inst. 97, 1204–1210 (2005).
Mattei, J. et al. Gastrin-releasing peptide receptor expression in lung cancer. Arch. Pathol. Lab. Med. 138, 98–104 (2014).
Lou, N. et al. Proteomics identifies circulating TIMP-1 as a prognostic biomarker for diffuse large B-cell lymphoma. Mol. Cell. Proteomics 22, 100625 (2023).
Schoemaker, M. J. et al. Cancer incidence in women with Turner syndrome in Great Britain: a national cohort study. Lancet Oncol. 9, 239–246 (2008).
Jacobs, P. A., Brunton, M., Court Brown, W. M., Doll, R. & Goldstein, H. Change of human chromosome count distribution with age: evidence for a sex differences. Nature 197, 1080–1081 (1963).
Jacobs, P. A., Court Brown, W. M. & Doll, R. Distribution of human chromosome counts in relation to age. Nature 191, 1178–1180 (1961).
Forsberg, L. A. et al. Mosaic loss of chromosome Y in leukocytes matters. Nat. Genet. 51, 4–7 (2019).
Thompson, D. J. et al. Genetic predisposition to mosaic Y chromosome loss in blood. Nature 575, 652–657 (2019).
Loftfield, E. et al. Predictors of mosaic chromosome Y loss and associations with mortality in the UK Biobank. Sci. Rep. 8, 12316 (2018).
Forsberg, L. A. et al. Mosaic loss of chromosome Y in peripheral blood is associated with shorter survival and higher risk of cancer. Nat. Genet. 46, 624–628 (2014).
Dumanski, J. P. et al. Mosaic loss of chromosome Y in blood is associated with Alzheimer disease. Am. J. Hum. Genet. 98, 1208–1219 (2016).
Haitjema, S. et al. Loss of Y chromosome in blood is associated with major cardiovascular events during follow-up in men after carotid endarterectomy. Circ. Cardiovasc. Genet. 10, e001544 (2017).
Sano, S. et al. Hematopoietic loss of Y chromosome leads to cardiac fibrosis and heart failure mortality. Science 377, 292–297 (2022).
Chandler, C., Liu, T., Buckanovich, R. & Coffman, L. G. The double edge sword of fibrosis in cancer. Transl. Res. 209, 55–67 (2019).
Li, M. O., Wan, Y. Y., Sanjabi, S., Robertson, A. K. & Flavell, R. A. Transforming growth factor-β regulation of immune responses. Annu. Rev. Immunol. 24, 99–146 (2006).
Dumanski, J. P. et al. Immune cells lacking Y chromosome show dysregulation of autosomal gene expression. Cell. Mol. Life Sci. 78, 4019–4033 (2021).
Brunelli, M., Eble, J. N., Zhang, S., Martignoni, G. & Cheng, L. Gains of chromosomes 7, 17, 12, 16, and 20 and loss of Y occur early in the evolution of papillary renal cell neoplasia: a fluorescent in situ hybridization study. Mod. Pathol. 16, 1053–1059 (2003).
Buscheck, F. et al. Y-chromosome loss is frequent in male renal tumors. Ann. Transl. Med. 9, 209 (2021).
Hunter, S., Gramlich, T., Abbott, K. & Varma, V. Y chromosome loss in esophageal carcinoma: an in situ hybridization study. Genes Chromosomes Cancer 8, 172–177 (1993).
Komura, K. et al. Resistance to docetaxel in prostate cancer is associated with androgen receptor activation and loss of KDM5D expression. Proc. Natl Acad. Sci. USA 113, 6259–6264 (2016).
Komura, K. et al. ATR inhibition controls aggressive prostate tumors deficient in Y-linked histone demethylase KDM5D. J. Clin. Invest. 128, 2979–2995 (2018).
Panani, A. D. & Roussos, C. Sex chromosome abnormalities in bladder cancer: Y polysomies are linked to PT1-grade III transitional cell carcinoma. Anticancer Res. 26, 319–323 (2006).
Sauter, G. et al. Y chromosome loss detected by FISH in bladder cancer. Cancer Genet. Cytogenet. 82, 163–169 (1995).
Powell, I., Tyrkus, M. & Kleer, E. Apparent correlation of sex chromosome loss and disease course in urothelial cancer. Cancer Genet. Cytogenet. 50, 97–101 (1990).
Abdel-Hafiz, H. A. et al. Y chromosome loss in cancer drives growth by evasion of adaptive immunity. Nature 619, 624–631 (2023).
Dohner, H. et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 129, 424–447 (2017).
United Kingdom Cancer Cytogenetics Group (UKCCG). Loss of the Y chromosome from normal and neoplastic bone marrows. Genes Chromosomes Cancer 5, 83–88 (1992).
Ouseph, M. M. et al. Genomic alterations in patients with somatic loss of the Y chromosome as the sole cytogenetic finding in bone marrow cells. Haematologica 106, 555–564 (2021).
Ganster, C. et al. New data shed light on Y-loss-related pathogenesis in myelodysplastic syndromes. Genes Chromosomes Cancer 54, 717–724 (2015).
Wong, A. K. et al. Loss of the Y chromosome: an age-related or clonal phenomenon in acute myelogenous leukemia/myelodysplastic syndrome? Arch. Pathol. Lab. Med. 132, 1329–1332 (2008).
Ljungstrom, V. et al. Loss of Y and clonal hematopoiesis in blood — two sides of the same coin? Leukemia 36, 889–891 (2022).
Holmes, R. I. et al. Loss of the Y chromosome in acute myelogenous leukemia: a report of 13 patients. Cancer Genet. Cytogenet. 17, 269–278 (1985).
Tamaki, M. et al. Deletion of Y chromosome before allogeneic hematopoietic stem cell transplantation in male recipients with female donors. Blood Adv. 6, 1895–1903 (2022).
Caceres, A., Jene, A., Esko, T., Perez-Jurado, L. A. & Gonzalez, J. R. Extreme downregulation of chromosome Y and cancer risk in men. J. Natl Cancer Inst. 112, 913–920 (2020).
Dunford, A. et al. Tumor-suppressor genes that escape from X-inactivation contribute to cancer sex bias. Nat. Genet. 49, 10–16 (2017).
Qi, M., Pang, J., Mitsiades, I., Lane, A. A. & Rheinbay, E. Loss of chromosome Y in primary tumors. Cell https://doi.org/10.1016/j.cell.2023.06.006 (2023).
Arseneault, M. et al. Loss of chromosome Y leads to down regulation of KDM5D and KDM6C epigenetic modifiers in clear cell renal cell carcinoma. Sci. Rep. 7, 44876 (2017).
Zhang, Q. et al. Mosaic loss of chromosome Y promotes leukemogenesis and clonal hematopoiesis. JCI Insight 7, e153768 (2022).
Dawson, M. A. & Kouzarides, T. Cancer epigenetics: from mechanism to therapy. Cell 150, 12–27 (2012).
Forbes, S. A. et al. COSMIC: mining complete cancer genomes in the Catalogue of Somatic Mutations in Cancer. Nucleic Acids Res. 39, D945–D950 (2011).
Stratton, M. R., Campbell, P. J. & Futreal, P. A. The cancer genome. Nature 458, 719–724 (2009).
Zhao, A., Zhou, H., Yang, J., Li, M. & Niu, T. Epigenetic regulation in hematopoiesis and its implications in the targeted therapy of hematologic malignancies. Signal Transduct. Target. Ther. 8, 71 (2023).
Fernandez-Morera, J. L., Calvanese, V., Rodriguez-Rodero, S., Menendez-Torre, E. & Fraga, M. F. Epigenetic regulation of the immune system in health and disease. Tissue Antigens 76, 431–439 (2010).
Li, E. & Zhang, Y. DNA methylation in mammals. Cold Spring Harb. Perspect. Biol. 6, a019133 (2014).
Ji, H. et al. Comprehensive methylome map of lineage commitment from haematopoietic progenitors. Nature 467, 338–342 (2010).
Bergstedt, J. et al. The immune factors driving DNA methylation variation in human blood. Nat. Commun. 13, 5895 (2022).
Correa, L. O., Jordan, M. S. & Carty, S. A. DNA methylation in T-cell development and differentiation. Crit. Rev. Immunol. 40, 135–156 (2020).
Roy, R. et al. DNA methylation signatures reveal that distinct combinations of transcription factors specify human immune cell epigenetic identity. Immunity 54, 2465–2480.e5 (2021).
Lin, S. et al. Sex-related DNA methylation differences in B cell chronic lymphocytic leukemia. Biol. Sex Differ. 10, 2 (2019).
Golden, L. C. et al. Parent-of-origin differences in DNA methylation of X chromosome genes in T lymphocytes. Proc. Natl Acad. Sci. USA 116, 26779–26787 (2019).
Arnold, A. P. & Chen, X. What does the “four core genotypes” mouse model tell us about sex differences in the brain and other tissues? Front. Neuroendocrinol. 30, 1–9 (2009).
Cisternas, C. D., Cortes, L. R., Bruggeman, E. C., Yao, B. & Forger, N. G. Developmental changes and sex differences in DNA methylation and demethylation in hypothalamic regions of the mouse brain. Epigenetics 15, 72–84 (2020).
Cisternas, C. D., Cortes, L. R., Golynker, I., Castillo-Ruiz, A. & Forger, N. G. Neonatal inhibition of DNA methylation disrupts testosterone-dependent masculinization of neurochemical phenotype. Endocrinology 161, bqz022 (2020).
McCartney, D. L. et al. An epigenome-wide association study of sex-specific chronological ageing. Genome Med. 12, 1 (2019).
Aubert, Y., Egolf, S. & Capell, B. C. The unexpected noncatalytic roles of histone modifiers in development and disease. Trends Genet. 35, 645–657 (2019).
Tricarico, R., Nicolas, E., Hall, M. J. & Golemis, E. A. X- and Y-linked chromatin-modifying genes as regulators of sex-specific cancer incidence and prognosis. Clin. Cancer Res. 26, 5567–5578 (2020).
Li, J. et al. Histone demethylase KDM5D upregulation drives sex differences in colon cancer. Nature 619, 632–639 (2023).
Yang, S. et al. KDM1A triggers androgen-induced miRNA transcription via H3K4me2 demethylation and DNA oxidation. Prostate 75, 936–946 (2015).
Metzler, V. M. et al. The KDM5B and KDM1A lysine demethylases cooperate in regulating androgen receptor expression and signalling in prostate cancer. Front. Cell Dev. Biol. 11, 1116424 (2023).
Wade, M. A. et al. The histone demethylase enzyme KDM3A is a key estrogen receptor regulator in breast cancer. Nucleic Acids Res. 43, 196–207 (2015).
Jones, D., Wilson, L., Thomas, H., Gaughan, L. & Wade, M. A. The histone demethylase enzymes KDM3A and KDM4B co-operatively regulate chromatin transactions of the estrogen receptor in breast cancer. Cancers 11, 1122 (2019).
Cheng, M. I. et al. The X-linked epigenetic regulator UTX controls NK cell-intrinsic sex differences. Nat. Immunol. 24, 780–791 (2023).
Itoh, Y. et al. The X-linked histone demethylase Kdm6a in CD4+ T lymphocytes modulates autoimmunity. J. Clin. Invest. 129, 3852–3863 (2019).
Gagnidze, K., Weil, Z. M. & Pfaff, D. W. Histone modifications proposed to regulate sexual differentiation of brain and behavior. Bioessays 32, 932–939 (2010).
Tsai, H. W., Grant, P. A. & Rissman, E. F. Sex differences in histone modifications in the neonatal mouse brain. Epigenetics 4, 47–53 (2009).
Kozomara, A., Birgaoanu, M. & Griffiths-Jones, S. miRBase: from microRNA sequences to function. Nucleic Acids Res. 47, D155–D162 (2019).
Ghorai, A. & Ghosh, U. miRNA gene counts in chromosomes vary widely in a species and biogenesis of miRNA largely depends on transcription or post-transcriptional processing of coding genes. Front. Genet. 5, 100 (2014).
Bhat-Nakshatri, P. et al. Estradiol-regulated microRNAs control estradiol response in breast cancer cells. Nucleic Acids Res. 37, 4850–4861 (2009).
Hah, N. et al. A rapid, extensive, and transient transcriptional response to estrogen signaling in breast cancer cells. Cell 145, 622–634 (2011).
Fletcher, C. E. et al. Androgen-regulated processing of the oncomir miR-27a, which targets prohibitin in prostate cancer. Hum. Mol. Genet. 21, 3112–3127 (2012).
Cui, C. et al. Identification and analysis of human sex-biased microRNAs. Genomics Proteomics Bioinformatics 16, 200–211 (2018).
Baulina, N. et al. Immune-related miRNA expression patterns in peripheral blood mononuclear cells differ in multiple sclerosis relapse and remission. J. Neuroimmunol. 317, 67–76 (2018).
Cavone, L. & Chiarugi, A. Targeting poly(ADP-ribose) polymerase-1 as a promising approach for immunomodulation in multiple sclerosis? Trends Mol. Med. 18, 92–100 (2012).
Malmhall, C., Weidner, J. & Radinger, M. MicroRNA-155 expression suggests a sex disparity in innate lymphoid cells at the single-cell level. Cell. Mol. Immunol. 17, 544–546 (2020).
Johansson, K., Malmhall, C., Ramos-Ramirez, P. & Radinger, M. MicroRNA-155 is a critical regulator of type 2 innate lymphoid cells and IL-33 signaling in experimental models of allergic airway inflammation. J. Allergy Clin. Immunol. 139, 1007–1016.e9 (2017).
Fuseini, H. & Newcomb, D. C. Mechanisms driving gender differences in asthma. Curr. Allergy Asthma Rep. 17, 19 (2017).
Rahmawati, S. F. et al. Pharmacological rationale for targeting IL-17 in asthma. Front. Allergy 2, 694514 (2021).
Ayers, M. et al. IFN-γ-related mRNA profile predicts clinical response to PD-1 blockade. J. Clin. Invest. 127, 2930–2940 (2017).
Rooney, M. S., Shukla, S. A., Wu, C. J., Getz, G. & Hacohen, N. Molecular and genetic properties of tumors associated with local immune cytolytic activity. Cell 160, 48–61 (2015).
Han, J. et al. Pan-cancer analysis reveals sex-specific signatures in the tumor microenvironment. Mol. Oncol. 16, 2153–2173 (2022).
Yoshihara, K. et al. Inferring tumour purity and stromal and immune cell admixture from expression data. Nat. Commun. 4, 2612 (2013).
Ye, Y. et al. Sex-associated molecular differences for cancer immunotherapy. Nat. Commun. 11, 1779 (2020).
Conforti, F. et al. Sex-based dimorphism of anticancer immune response and molecular mechanisms of immune evasion. Clin. Cancer Res. 27, 4311–4324 (2021).
Gubbels Bupp, M. R., Potluri, T., Fink, A. L. & Klein, S. L. The confluence of sex hormones and aging on immunity. Front. Immunol. 9, 1269 (2018).
Petralia, F. et al. Pan-cancer proteogenomics characterization of tumor immunity. Cell https://doi.org/10.1016/j.cell.2024.01.027 (2024).
Cristescu, R. et al. Pan-tumor genomic biomarkers for PD-1 checkpoint blockade-based immunotherapy. Science 362, eaar3593 (2018).
Conforti, F. et al. Sex-based differences of the tumor mutational burden and T-cell inflammation of the tumor microenvironment. Ann. Oncol. 30, 653–655 (2019).
Botticelli, A. et al. The sexist behaviour of immune checkpoint inhibitors in cancer therapy? Oncotarget 8, 99336–99346 (2017).
Conforti, F. et al. Cancer immunotherapy efficacy and patients’ sex: a systematic review and meta-analysis. Lancet Oncol. 19, 737–746 (2018).
Wallis, C. J. D. et al. Association of patient sex with efficacy of immune checkpoint inhibitors and overall survival in advanced cancers: a systematic review and meta-analysis. JAMA Oncol. 5, 529–536 (2019).
Grassadonia, A. et al. Effect of gender on the outcome of patients receiving immune checkpoint inhibitors for advanced cancer: a systematic review and meta-analysis of phase III randomized clinical trials. J. Clin. Med. 7, 542 (2018).
Conforti, F. et al. Sex-based heterogeneity in response to lung cancer immunotherapy: a systematic review and meta-analysis. J. Natl Cancer Inst. 111, 772–781 (2019).
Wang, L. et al. The role of the sex hormone–gut microbiome axis in tumor immunotherapy. Gut Microbes 15, 2185035 (2023).
Viaud, S. et al. The intestinal microbiota modulates the anticancer immune effects of cyclophosphamide. Science 342, 971–976 (2013).
Sivan, A. et al. Commensal Bifidobacterium promotes antitumor immunity and facilitates anti-PD-L1 efficacy. Science 350, 1084–1089 (2015).
Matson, V. et al. The commensal microbiome is associated with anti-PD-1 efficacy in metastatic melanoma patients. Science 359, 104–108 (2018).
Routy, B. et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science 359, 91–97 (2018).
Sinha, T. et al. Analysis of 1135 gut metagenomes identifies sex-specific resistome profiles. Gut Microbes 10, 358–366 (2019).
Miceli, R. et al. Sex differences in burden of adverse events in patients receiving immunotherapy. J. Clin. Oncol. https://doi.org/10.1200/JCO.2023.41.16_suppl.2646 (2023).
Unger, J. M. et al. Sex differences in risk of severe adverse events in patients receiving immunotherapy, targeted therapy, or chemotherapy in cancer clinical trials. J. Clin. Oncol. 40, 1474–1486 (2022).
Duma, N. et al. Sex differences in tolerability to anti-programmed cell death protein 1 therapy in patients with metastatic melanoma and non-small cell lung cancer: are we all equal? Oncologist 24, E1148–E1155 (2019).
Bui, A.-T. N., Bougrine, A., Buchbinder, E. I., Giobbie-Hurder, A. & LeBoeuf, N. R. Female sex is associated with higher rates of dermatologic adverse events among patients with melanoma receiving immune checkpoint inhibitor therapy: a retrospective cohort study. J. Am. Acad. Dermatol. 87, 403–406 (2022).
Kitagataya, T. et al. Prevalence, clinical course, and predictive factors of immune checkpoint inhibitor monotherapy-associated hepatitis in Japan. J. Gastroenterol. Hepatol. 35, 1782–1788 (2020).
Chua, K. J. et al. Comparing the rate of immunotherapy treatment change due to toxicity by sex. Cancer Rep. 7, e1932 (2024).
Cortellini, A. et al. Immune-related adverse events of pembrolizumab in a large real-world cohort of patients with NSCLC with a PD-L1 expression ≥ 50% and their relationship with clinical outcomes. Clin. Lung Cancer 21, 498–508.e2 (2020).
Kartolo, A., Sattar, J., Sahai, V., Baetz, T. & Lakoff, J. M. Predictors of immunotherapy-induced immune-related adverse events. Curr. Oncol. 25, E403–E410 (2018).
Chen, C., Zhang, C., Jin, Z., Wu, B. & Xu, T. Sex differences in immune-related adverse events with immune checkpoint inhibitors: data mining of the FDA adverse event reporting system. Int. J. Clin. Pharm. 44, 689–697 (2022).
Seethapathy, H. et al. Immune-related adverse events and kidney function decline in patients with genitourinary cancers treated with immune checkpoint inhibitors. Eur. J. Cancer 157, 50–58 (2021).
Ozdemir, B. C., Gerard, C. L. & Espinosa da Silva, C. Sex and gender differences in anticancer treatment toxicity: a call for revisiting drug dosing in oncology. Endocrinology 163, bqac058 (2022).
Desnoyer, A. et al. Pharmacokinetic/pharmacodynamic relationship of therapeutic monoclonal antibodies used in oncology: part 2, immune checkpoint inhibitor antibodies. Eur. J. Cancer 128, 119–128 (2020).
Melhem, M. et al. Population pharmacokinetics and exposure-response of anti-programmed cell death protein-1 monoclonal antibody dostarlimab in advanced solid tumours. Br. J. Clin. Pharmacol. 88, 4142–4154 (2022).
De Courcy, L., Bezak, E. & Marcu, L. G. Gender-dependent radiotherapy: the next step in personalised medicine? Crit. Rev. Oncol. Hematol. 147, 102881 (2020).
Luo, H. S. et al. Impact of sex on the prognosis of patients with esophageal squamous cell cancer underwent definitive radiotherapy: a propensity score-matched analysis. Radiat. Oncol. 14, 74 (2019).
Ilnytskyy, Y., Zemp, F. J., Koturbash, I. & Kovalchuk, O. Altered microRNA expression patterns in irradiated hematopoietic tissues suggest a sex-specific protective mechanism. Biochem. Biophys. Res. Commun. 377, 41–45 (2008).
Longcope, C., Kato, T. & Horton, R. Conversion of blood androgens to estrogens in normal adult men and women. J. Clin. Invest. 48, 2191–2201 (1969).
Hilborn, E., Stal, O. & Jansson, A. Estrogen and androgen-converting enzymes 17β-hydroxysteroid dehydrogenase and their involvement in cancer: with a special focus on 17β-hydroxysteroid dehydrogenase type 1, 2, and breast cancer. Oncotarget 8, 30552–30562 (2017).
Miller, W. L. & Auchus, R. J. The “backdoor pathway” of androgen synthesis in human male sexual development. PLoS Biol. 17, e3000198 (2019).
Morozov, V. M., Li, Y., Clowers, M. M. & Ishov, A. M. Inhibitor of H3K27 demethylase JMJD3/UTX GSK-J4 is a potential therapeutic option for castration resistant prostate cancer. Oncotarget 8, 62131–62142 (2017).
Xie, G. et al. UTX promotes hormonally responsive breast carcinogenesis through feed-forward transcription regulation with estrogen receptor. Oncogene 36, 5497–5511 (2017).
DePinho, R. A. The age of cancer. Nature 408, 248–254 (2000).
Giefing-Kroll, C., Berger, P., Lepperdinger, G. & Grubeck-Loebenstein, B. How sex and age affect immune responses, susceptibility to infections, and response to vaccination. Aging Cell 14, 309–321 (2015).
Cook, M. B. et al. Sex disparities in cancer incidence by period and age. Cancer Epidemiol. Biomarkers Prev. 18, 1174–1182 (2009).
Rubin, J. B. The spectrum of sex differences in cancer. Trends Cancer 8, 303–315 (2022).
Valeri, F. & Endres, K. How biological sex of the host shapes its gut microbiota. Front. Neuroendocrinol. 61, 100912 (2021).
Org, E. et al. Sex differences and hormonal effects on gut microbiota composition in mice. Gut Microbes 7, 313–322 (2016).
Fransen, F. et al. The impact of gut microbiota on gender-specific differences in immunity. Front. Immunol. 8, 754 (2017).
Gopalakrishnan, V. et al. Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science 359, 97–103 (2018).
Li, X., Zhang, S., Guo, G., Han, J. & Yu, J. Gut microbiome in modulating immune checkpoint inhibitors. EBioMedicine 82, 104163 (2022).
Zhao, R. et al. A GPR174-CCL21 module imparts sexual dimorphism to humoral immunity. Nature 577, 416–420 (2020).
Schumacher, T. N. & Thommen, D. S. Tertiary lymphoid structures in cancer. Science 375, eabf9419 (2022).
Helmink, B. A. et al. B cells and tertiary lymphoid structures promote immunotherapy response. Nature 577, 549–555 (2020).
Pan, Y. et al. Unique distribution of programmed death ligand 1 (PD-L1) expression in East Asian non-small cell lung cancer. J. Thorac. Dis. 9, 2579–2586 (2017).
Moutafi, M. K. et al. Comparison of programmed death-ligand 1 protein expression between primary and metastatic lesions in patients with lung cancer. J. Immunother. Cancer 9, e002230 (2021).
de Coana, Y. P. et al. Ipilimumab treatment results in an early decrease in the frequency of circulating granulocytic myeloid-derived suppressor cells as well as their arginase1 production. Cancer Immunol. Res. 1, 158–162 (2013).
El-Khoueiry, A. B. et al. Results from a phase 1a/1b study of botensilimab (BOT), a novel innate/adaptive immune activator, plus balstilimab (BAL; anti-PD-1 antibody) in metastatic heavily pretreated microsatellite stable colorectal cancer (MSS CRC). J. Clin. Oncol. 41, LBA8 (2023).
US National Library of Medicine. ClinicalTrials.gov https://www.clinicaltrials.gov/study/NCT03860272 (2023).
Straining, R. & Eighmy, W. Tazemetostat: EZH2 inhibitor. J. Adv. Pract. Oncol. 13, 158–163 (2022).
Goswami, S. et al. Modulation of EZH2 expression in T cells improves efficacy of anti-CTLA-4 therapy. J. Clin. Invest. 128, 3813–3818 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT03480646 (2021).
Aggarwal, R. R. et al. A phase Ib/IIa study of the pan-BET inhibitor ZEN-3694 in combination with enzalutamide in patients with metastatic castration-resistant prostate cancer. Clin. Cancer Res. 26, 5338–5347 (2020).
Besancon, M. et al. Combining antiandrogens with immunotherapy for bladder cancer treatment. Eur. Urol. Open. Sci. 43, 35–44 (2022).
Natale, C. A. et al. Pharmacologic activation of the G protein-coupled estrogen receptor inhibits pancreatic ductal adenocarcinoma. Cell. Mol. Gastroenterol. Hepatol. 10, 868–880.e1 (2020).
Natale, C. A. et al. Activation of G protein-coupled estrogen receptor signaling inhibits melanoma and improves response to immune checkpoint blockade. eLife 7, e31770 (2018).
Hu, W. Y. et al. Estrogen-initiated transformation of prostate epithelium derived from normal human prostate stem-progenitor cells. Endocrinology 152, 2150–2163 (2011).
Mirza, N. et al. All-trans-retinoic acid improves differentiation of myeloid cells and immune response in cancer patients. Cancer Res. 66, 9299–9307 (2006).
Yang, L. et al. Expansion of myeloid immune suppressor Gr+CD11b+ cells in tumor-bearing host directly promotes tumor angiogenesis. Cancer Cell 6, 409–421 (2004).
Vasquez-Dunddel, D. et al. STAT3 regulates arginase-I in myeloid-derived suppressor cells from cancer patients. J. Clin. Invest. 123, 1580–1589 (2013).
Osada, T. et al. The effect of anti-VEGF therapy on immature myeloid cell and dendritic cells in cancer patients. Cancer Immunol. Immunother. 57, 1115–1124 (2008).
Acknowledgements
This work is supported by the Pelotonia Institute for Immuno-Oncology (to Z.L.), the American Brain Tumour Association (to J.L.), the Cleveland Clinic (to J.L. and J.D.L.), the Case Comprehensive Cancer Center (to J.D.L.), the US National Institutes of Health grants P01 CA245705 (to J.D.L.), P01 CA278732 (to Z.L.), R01 CA262069 (to Z.L.), R35 NS127083 (to J.D.L.), R01 AG084250 (to J.D.L.) and T32 2T32CA09223-16A1 (to T.D.G.), and the Pelotonia Graduate Fellowship Program from The Ohio State University Comprehensive Cancer Center-James (to T.X.).
Author information
Authors and Affiliations
Contributions
All authors participated in the conceptualization and writing of the manuscript. J.D.L. and Z.L. also provided overall project management.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Cancer thanks Maureen Su and Sabra Klein, who co-reviewed with Joseph Hoffmann, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- All-cause mortality
-
The death rate from all causes of death for a population within a specific time period.
- Castration
-
A medical procedure that involves the removal or suppression of the testes in males.
- Four-core genotype (FCG) mouse model
-
A mouse strain that has four possible combinations of sex chromosome complement and gonadal sex — XX gonadal males (XXM), XY gonadal males (XYM), XX gonadal females (XXF) and XY gonadal females (XYF) — used to investigate the influence of sex chromosomes and gonadal hormones separately.
- Graft-versus-leukaemia effect
-
The ability of donor immune cells to eliminate host leukaemic cells after allogeneic haematopoietic stem cell transplantation.
- Hypogonadism
-
A condition in both males and females in which the body’s sex glands produce little or no sex hormones.
- Pharmacodynamic
-
The biochemical and physiological effects of the foreign chemicals on the body.
- Pharmacokinetic
-
The dynamic changes of foreign chemicals in the body.
- Progenitor-exhausted CD8+ T cells
-
A subpopulation of CD8+ tumour-infiltrating lymphocytes that retain polyfunctionality, persist long term and differentiate into ‘terminally exhausted’ progenies.
- Regulatory T (Treg) cells
-
A subset of CD4+ T lymphocytes that are defined by FOXP3 expression and suppress the immune system to prevent autoimmune reactions.
- T follicular helper cell
-
A subset of CD4+ T lymphocytes that have a key role in regulating B cell responses and antibody production within lymphoid follicles during the immune response.
- T helper 1 (TH1) cells
-
A subset of CD4+ T lymphocytes that promote cell-mediated immune responses and is required for host defence against intracellular viral and bacterial pathogens.
- T helper 17 (TH17) cells
-
A subset of pro-inflammatory CD4+ T lymphocytes defined by their production of IL-17 and have an important role in maintaining mucosal barriers and contributing to pathogen clearance at mucosal surfaces.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xiao, T., Lee, J., Gauntner, T.D. et al. Hallmarks of sex bias in immuno-oncology: mechanisms and therapeutic implications. Nat Rev Cancer 24, 338–355 (2024). https://doi.org/10.1038/s41568-024-00680-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41568-024-00680-z