Abstract
Human malignancies arise predominantly in tissues of epithelial origin, where the stepwise transformation from healthy epithelium to premalignant dysplasia to invasive neoplasia involves sequential dysregulation of biological networks that govern essential functions of epithelial homeostasis. Cutaneous squamous cell carcinoma (cSCC) is a prototype epithelial malignancy, often with a high tumour mutational burden. A plethora of risk genes, dominated by UV-induced sun damage, drive disease progression in conjunction with stromal interactions and local immunomodulation, enabling continuous tumour growth. Recent studies have identified subpopulations of SCC cells that specifically interact with the tumour microenvironment. These advances, along with increased knowledge of the impact of germline genetics and somatic mutations on cSCC development, have led to a greater appreciation of the complexity of skin cancer pathogenesis and have enabled progress in neoadjuvant immunotherapy, which has improved pathological complete response rates. Although measures for the prevention and therapeutic management of cSCC are associated with clinical benefit, the prognosis remains poor for advanced disease. Elucidating how the genetic mechanisms that drive cSCC interact with the tumour microenvironment is a current focus in efforts to understand, prevent and treat cSCC.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Chang, M. S., Azin, M. & Demehri, S. Cutaneous squamous cell carcinoma: the frontier of cancer immunoprevention. Annu. Rev. Pathol. 17, 101–119 (2022).
Rogers, H. W., Weinstock, M. A., Feldman, S. R. & Coldiron, B. M. Incidence estimate of nonmelanoma skin cancer (keratinocyte carcinomas) in the US population, 2012. JAMA Dermatol. 151, 1081–1086 (2015).
Qureshi, A. A., Laden, F., Colditz, G. A. & Hunter, D. J. Geographic variation and risk of skin cancer in US women. Differences between melanoma, squamous cell carcinoma, and basal cell carcinoma. Arch. Intern. Med. 168, 501–507 (2008).
Dusendang, J. R. et al. Cohort and nested case-control study of cutaneous squamous cell carcinoma in solid organ transplant recipients, by medication. J. Am. Acad. Dermatol. 86, 598–606 (2022).
Nadhan, K. S. et al. Risk factors for keratinocyte carcinoma skin cancer in nonwhite individuals: a retrospective analysis. J. Am. Acad. Dermatol. 81, 373–378 (2019).
Nehal, K. S. & Bichakjian, C. K. Update on keratinocyte carcinomas. N. Engl. J. Med. 379, 363–374 (2018).
Que, S. K. T., Zwald, F. O. & Schmults, C. D. Cutaneous squamous cell carcinoma: Incidence, risk factors, diagnosis, and staging. J. Am. Acad. Dermatol. 78, 237–247 (2018).
Thompson, A. K., Kelley, B. F., Prokop, L. J., Murad, M. H. & Baum, C. L. Risk factors for cutaneous squamous cell carcinoma recurrence, metastasis, and disease-specific death: a systematic review and meta-analysis. JAMA Dermatol. 152, 419–428 (2016).
Haisma, M. S. et al. Multivariate analysis of potential risk factors for lymph node metastasis in patients with cutaneous squamous cell carcinoma of the head and neck. J. Am. Acad. Dermatol. 75, 722–730 (2016).
Eigentler, T. K. et al. Survival of patients with cutaneous squamous cell carcinoma: results of a prospective cohort study. J. Invest. Dermatol. 137, 2309–2315 (2017).
Schmults, C. D., Karia, P. S., Carter, J. B., Han, J. & Qureshi, A. A. Factors predictive of recurrence and death from cutaneous squamous cell carcinoma: a 10-year, single-institution cohort study. JAMA Dermatol. 149, 541–547 (2013).
Eviston, T. J. et al. Gene expression profiling of perineural invasion in head and neck cutaneous squamous cell carcinoma. Sci. Rep. 11, 13192 (2021).
Venables, Z. C. et al. Nationwide incidence of metastatic cutaneous squamous cell carcinoma in england. JAMA Dermatol. 155, 298–306 (2019).
Karia, P. S., Han, J. & Schmults, C. D. Cutaneous squamous cell carcinoma: estimated incidence of disease, nodal metastasis, and deaths from disease in the United States, 2012. J. Am. Acad. Dermatol. 68, 957–966 (2013).
Pickering, C. R. et al. Mutational landscape of aggressive cutaneous squamous cell carcinoma. Clin. Cancer Res. 20, 6582–6592 (2014).
Cammareri, P. et al. Inactivation of TGFβ receptors in stem cells drives cutaneous squamous cell carcinoma. Nat. Commun. 7, 12493 (2016).
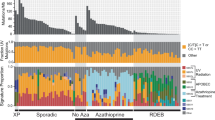
Inman, G. J. et al. The genomic landscape of cutaneous SCC reveals drivers and a novel azathioprine associated mutational signature. Nat. Commun. 9, 3667 (2018).
Rodriguez-Paredes, M. et al. Methylation profiling identifies two subclasses of squamous cell carcinoma related to distinct cells of origin. Nat. Commun. 9, 577 (2018).
Ji, A. L. et al. Multimodal analysis of composition and spatial architecture in human squamous cell carcinoma. Cell 182, 497–514 e422 (2020). Using cSCC as a model, this paper integrates single-cell RNA sequencing with spatial transcriptomics and multiplexed ion beam imaging, revealing a complex interplay of malignant and nonmalignant cells at the tumour edge, and outlines a tumour-specific cell type at the leading edge that may drive stromal and immune changes that facilitate progression.
Oshimori, N., Oristian, D. & Fuchs, E. TGF-β promotes heterogeneity and drug resistance in squamous. Cell Carcinoma Cell 160, 963–976 (2015). This study shows how TGFβ directly interacts with tumour cells to promote tumour heterogeneity and implicates this pathway in drug-resistance mechanisms.
Manyam, B. V. et al. A multi-institutional comparison of outcomes of immunosuppressed and immunocompetent patients treated with surgery and radiation therapy for cutaneous squamous cell carcinoma of the head and neck. Cancer 123, 2054–2060 (2017).
Gross, N. D. et al. Neoadjuvant cemiplimab for stage II to IV cutaneous squamous-cell carcinoma. N. Engl. J. Med. 387, 1557–1568 (2022). Landmark paper demonstrating the efficacy of immunotherapy with cemiplimab for cSCC in a phase II trial.
Agbai, O. N. et al. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public. J. Am. Acad. Dermatol. 70, 748–762 (2014).
Tadokoro, T. et al. UV-induced DNA damage and melanin content in human skin differing in racial/ethnic origin. FASEB J. 17, 1177–1179 (2003).
Thody, A. J. et al. Pheomelanin as well as eumelanin is present in human epidermis. J. Invest. Dermatol. 97, 340–344 (1991).
Hunt, G. et al. Eumelanin and phaeomelanin contents of human epidermis and cultured melanocytes. Pigment. Cell Res. 8, 202–208 (1995).
Ziegler, A. et al. Sunburn and p53 in the onset of skin cancer. Nature 372, 773–776 (1994). This study identifies the role of UVR in both tumour initiation and tumour propagation through p53.
Xu, X. et al. HSD17B7 gene in self-renewal and oncogenicity of keratinocytes from Black versus White populations. EMBO Mol. Med. 13, e14133 (2021).
Martena, M. J. et al. Monitoring of mercury, arsenic, and lead in traditional Asian herbal preparations on the Dutch market and estimation of associated risks. Food Addit. Contam. Part. A Chem. Anal. Control. Expo. Risk Assess. 27, 190–205 (2010).
Oh, C. C., Jin, A. & Koh, W. P. Trends of cutaneous basal cell carcinoma, squamous cell carcinoma, and melanoma among the Chinese, Malays, and Indians in Singapore from 1968-2016. JAAD Int. 4, 39–45 (2021).
Knobeloch, L. M., Zierold, K. M. & Anderson, H. A. Association of arsenic-contaminated drinking-water with prevalence of skin cancer in Wisconsin’s Fox River Valley. J. Health Popul. Nutr. 24, 206–213 (2006).
Karagas, M. R., Gossai, A., Pierce, B. & Ahsan, H. Drinking water arsenic contamination, skin lesions, and malignancies: a systematic review of the global evidence. Curr. Env. Health Rep. 2, 52–68 (2015).
Gronskov, K., Ek, J. & Brondum-Nielsen, K. Oculocutaneous albinism. Orphanet J. Rare Dis. 2, 43 (2007).
Fine, J. D., Johnson, L. B., Weiner, M., Li, K. P. & Suchindran, C. Epidermolysis bullosa and the risk of life-threatening cancers: the National EB Registry experience, 1986-2006. J. Am. Acad. Dermatol. 60, 203–211 (2009).
McGrath, J. A., Schofield, O. M., Mayou, B. J., McKee, P. H. & Eady, R. A. Epidermolysis bullosa complicated by squamous cell carcinoma: report of 10 cases. J. Cutan. Pathol. 19, 116–123 (1992).
Ng, Y. Z. et al. Fibroblast-derived dermal matrix drives development of aggressive cutaneous squamous cell carcinoma in patients with recessive dystrophic epidermolysis bullosa. Cancer Res. 72, 3522–3534 (2012).
Cho, R. J. et al. APOBEC mutation drives early-onset squamous cell carcinomas in recessive dystrophic epidermolysis bullosa. Sci. Transl. Med. 10, eaas9668 (2018).
Youssefian, L., Vahidnezhad, H. & Uitto, J. Kindler syndrome. in GeneReviews (eds Adam, M. P. et al.) (University of Washington, 1993).
Siegel, D. H. et al. Loss of kindlin-1, a human homolog of the Caenorhabditis elegans actin-extracellular-matrix linker protein UNC-112, causes Kindler syndrome. Am. J. Hum. Genet. 73, 174–187 (2003).
Rognoni, E. et al. Kindlin-1 controls Wnt and TGF-β availability to regulate cutaneous stem cell proliferation. Nat. Med. 20, 350–359 (2014).
Chacon-Solano, E. et al. Fibroblast activation and abnormal extracellular matrix remodelling as common hallmarks in three cancer-prone genodermatoses. Br. J. Dermatol. 181, 512–522 (2019).
Sarin, K. Y. et al. Genome-wide meta-analysis identifies eight new susceptibility loci for cutaneous squamous cell carcinoma. Nat. Commun. 11, 820 (2020).
Kim, Y. et al. Genome-wide association study of actinic keratosis identifies new susceptibility loci implicated in pigmentation and immune regulation pathways. Commun. Biol. 5, 386 (2022).
Chahal, H. S. et al. Genome-wide association study identifies novel susceptibility loci for cutaneous squamous cell carcinoma. Nat. Commun. 7, 12048 (2016).
D’Orazio, J., Jarrett, S., Amaro-Ortiz, A. & Scott, T. UV radiation and the skin. Int. J. Mol. Sci. 14, 12222–12248 (2013).
Kim, Y. & He, Y. Y. Ultraviolet radiation-induced non-melanoma skin cancer: regulation of DNA damage repair and inflammation. Genes. Dis. 1, 188–198 (2014).
Vogeley, C., Rolfes, K. M., Krutmann, J. & Haarmann-Stemmann, T. The aryl hydrocarbon receptor in the pathogenesis of environmentally-induced squamous cell carcinomas of the skin. Front. Oncol. 12, 841721 (2022).
Green, A. C. & Olsen, C. M. Cutaneous squamous cell carcinoma: an epidemiological review. Br. J. Dermatol. 177, 373–381 (2017).
Dotto, G. P. & Rustgi, A. K. Squamous cell cancers: a unified perspective on biology and genetics. Cancer Cell 29, 622–637 (2016).
Slaughter, D. P., Southwick, H. W. & Smejkal, W. Field cancerization in oral stratified squamous epithelium; clinical implications of multicentric origin. Cancer 6, 963–968 (1953). Landmark paper from 1953 introducing the concept of field cancerization, based on the observations of frequent arisal of tumours within the same area of tissue.
Martincorena, I. et al. Tumor evolution. High burden and pervasive positive selection of somatic mutations in normal human skin. Science 348, 880–886 (2015). Seminal paper describing how somatic mutations linked to epithelial cancer exist in normal-appearing sun-exposed skin.
Dotto, G. P. Multifocal epithelial tumors and field cancerization: stroma as a primary determinant. J. Clin. Invest. 124, 1446–1453 (2014).
Hu, B. et al. Multifocal epithelial tumors and field cancerization from loss of mesenchymal CSL signaling. Cell 149, 1207–1220 (2012). This study shows how mesenchymal NOTCH–CSL signaling causes tissue alterations, including stromal atrophy and inflammation, which precede and are potent triggers for epithelial tumours, and in human skin inducable by UVR.
Fisher, G. J. et al. Pathophysiology of premature skin aging induced by ultraviolet light. N. Engl. J. Med. 337, 1419–1428 (1997).
Vosseler, S. et al. Distinct progression-associated expression of tumor and stromal MMPs in HaCaT skin SCCs correlates with onset of invasion. Int. J. Cancer 125, 2296–2306 (2009).
Lee, C. S. et al. Mutant collagen COL11A1 enhances cancerous invasion. Oncogene 40, 6299–6307 (2021).
Quan, T., He, T., Voorhees, J. J. & Fisher, G. J. Ultraviolet irradiation induces Smad7 via induction of transcription factor AP-1 in human skin fibroblasts. J. Biol. Chem. 280, 8079–8085 (2005).
Quan, T., He, T., Kang, S., Voorhees, J. J. & Fisher, G. J. Solar ultraviolet irradiation reduces collagen in photoaged human skin by blocking transforming growth factor-β type II receptor/Smad signaling. Am. J. Pathol. 165, 741–751 (2004).
Kripke, M. L. & Fisher, M. S. Immunologic parameters of ultraviolet carcinogenesis. J. Natl Cancer Inst. 57, 211–215 (1976).
Simon, J. C., Tigelaar, R. E., Bergstresser, P. R., Edelbaum, D. & Cruz, P. D. Jr. Ultraviolet B radiation converts Langerhans cells from immunogenic to tolerogenic antigen-presenting cells. Induction of specific clonal anergy in CD4+ T helper 1 cells. J. Immunol. 146, 485–491 (1991).
Loser, K. et al. IL-10 controls ultraviolet-induced carcinogenesis in mice. J. Immunol. 179, 365–371 (2007). This paper demonstrates how the immunosuppressive cytokine IL-10 dictates UVR-induced carcinogenesis in mouse skin.
Bottomley, M. J., Thomson, J., Harwood, C. & Leigh, I. The role of the immune system in cutaneous squamous cell carcinoma. Int. J. Mol. Sci. 20, 2009 (2019).
Garssen, J. et al. UVB exposure-induced systemic modulation of Th1- and Th2-mediated immune responses. Immunology 97, 506–514 (1999).
Jantschitsch, C., Weichenthal, M., Proksch, E., Schwarz, T. & Schwarz, A. IL-12 and IL-23 affect photocarcinogenesis differently. J. Invest. Dermatol. 132, 1479–1486 (2012).
Maeda, A. et al. Enhanced photocarcinogenesis in interleukin-12-deficient mice. Cancer Res. 66, 2962–2969 (2006).
Nasti, T. H. et al. Differential roles of T-cell subsets in regulation of ultraviolet radiation induced cutaneous photocarcinogenesis. Photochem. Photobiol. 87, 387–398 (2011).
Lewis, J. M. et al. Chronic UV radiation-induced RORγt+ IL-22-producing lymphoid cells are associated with mutant KC clonal expansion. Proc. Natl Acad. Sci. USA https://doi.org/10.1073/pnas.2016963118 (2021).
Azzimonti, B. et al. Intense Foxp3+CD25+ regulatory T-cell infiltration is associated with high-grade cutaneous squamous cell carcinoma and counterbalanced by CD8+/Foxp3+CD25+ ratio. Br. J. Dermatol. 172, 64–73 (2015).
Bluth, M. J. et al. Myeloid dendritic cells from human cutaneous squamous cell carcinoma are poor stimulators of T-cell proliferation. J. Invest. Dermatol. 129, 2451–2462 (2009).
Armstrong, B. K. & Kricker, A. The epidemiology of UV induced skin cancer. J. Photochem. Photobiol. B 63, 8–18 (2001).
Schmitt, J., Seidler, A., Diepgen, T. L. & Bauer, A. Occupational ultraviolet light exposure increases the risk for the development of cutaneous squamous cell carcinoma: a systematic review and meta-analysis. Br. J. Dermatol. 164, 291–307 (2011).
Alfonso, J. H. et al. Occupation and relative risk of cutaneous squamous cell carcinoma (cSCC): a 45-year follow-up study in 4 Nordic countries. J. Am. Acad. Dermatol. 75, 548–555 (2016).
Garrett, G. L. et al. Incidence of and risk factors for skin cancer in organ transplant recipients in the United States. JAMA Dermatol. 153, 296–303 (2017).
Krynitz, B. et al. Risk of skin cancer and other malignancies in kidney, liver, heart and lung transplant recipients 1970 to 2008–a Swedish population-based study. Int. J. Cancer 132, 1429–1438 (2013).
Falchi, L. et al. Incidence and prognostic impact of other cancers in a population of long-term survivors of chronic lymphocytic leukemia. Ann. Oncol. 27, 1100–1106 (2016).
Silverberg, M. J. et al. HIV infection status, immunodeficiency, and the incidence of non-melanoma skin cancer. J. Natl Cancer Inst. 105, 350–360 (2013).
Nguyen, P., Vin-Christian, K., Ming, M. E. & Berger, T. Aggressive squamous cell carcinomas in persons infected with the human immunodeficiency virus. Arch. Dermatol. 138, 758–763 (2002).
Azzimonti, B. et al. CD8+ T-cell lymphocytopenia and lack of EVER mutations in a patient with clinically and virologically typical epidermodysplasia verruciformis. Arch. Dermatol. 141, 1323–1325 (2005).
Zavattaro, E. et al. Identification of defective Fas function and variation of the perforin gene in an epidermodysplasia verruciformis patient lacking EVER1 and EVER2 mutations. J. Invest. Dermatol. 128, 732–735 (2008).
Landini, M. M. et al. α- and β-Papillomavirus infection in a young patient with an unclassified primary T-cell immunodeficiency and multiple mucosal and cutaneous lesions. J. Am. Acad. Dermatol. 71, 108–115 e101 (2014).
Wang, J., Aldabagh, B., Yu, J. & Arron, S. T. Role of human papillomavirus in cutaneous squamous cell carcinoma: a meta-analysis. J. Am. Acad. Dermatol. 70, 621–629 (2014).
Bernard, H. U. et al. Classification of papillomaviruses (PVs) based on 189 PV types and proposal of taxonomic amendments. Virology 401, 70–79 (2010).
Arron, S. T., Ruby, J. G., Dybbro, E., Ganem, D. & Derisi, J. L. Transcriptome sequencing demonstrates that human papillomavirus is not active in cutaneous squamous cell carcinoma. J. Invest. Dermatol. 131, 1745–1753 (2011).
Hazard, K. et al. Cutaneous human papillomaviruses persist on healthy skin. J. Invest. Dermatol. 127, 116–119 (2007).
Middleton, K. et al. Organization of human papillomavirus productive cycle during neoplastic progression provides a basis for selection of diagnostic markers. J. Virol. 77, 10186–10201 (2003).
Bosch, F. X. et al. Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. International biological study on cervical cancer (IBSCC) Study Group. J. Natl Cancer Inst. 87, 796–802 (1995).
Riddel, C., Rashid, R. & Thomas, V. Ungual and periungual human papillomavirus-associated squamous cell carcinoma: a review. J. Am. Acad. Dermatol. 64, 1147–1153 (2011).
Munger, K., Phelps, W. C., Bubb, V., Howley, P. M. & Schlegel, R. The E6 and E7 genes of the human papillomavirus type 16 together are necessary and sufficient for transformation of primary human keratinocytes. J. Virol. 63, 4417–4421 (1989).
Hawley-Nelson, P., Vousden, K. H., Hubbert, N. L., Lowy, D. R. & Schiller, J. T. HPV16 E6 and E7 proteins cooperate to immortalize human foreskin keratinocytes. EMBO J. 8, 3905–3910 (1989).
Huibregtse, J. M., Scheffner, M. & Howley, P. M. A cellular protein mediates association of p53 with the E6 oncoprotein of human papillomavirus types 16 or 18. EMBO J. 10, 4129–4135 (1991).
Dyson, N., Howley, P. M., Munger, K. & Harlow, E. The human papilloma virus-16 E7 oncoprotein is able to bind to the retinoblastoma gene product. Science 243, 934–937 (1989). Seminal paper demonstrating how the E7 oncoprotein from HPV16 regulates retinoblastoma signalling.
de Sanjose, S. et al. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol. 11, 1048–1056 (2010).
Mirabello, L. et al. HPV16 E7 genetic conservation is critical to carcinogenesis. Cell 170, 1164–1174 e1166 (2017).
Viarisio, D. et al. Beta HPV38 oncoproteins act with a hit-and-run mechanism in ultraviolet radiation-induced skin carcinogenesis in mice. PLoS Pathog. 14, e1006783 (2018).
Barbosa, M. S., Vass, W. C., Lowy, D. R. & Schiller, J. T. In vitro biological activities of the E6 and E7 genes vary among human papillomaviruses of different oncogenic potential. J. Virol. 65, 292–298 (1991).
Asgari, M. M. et al. Detection of human papillomavirus DNA in cutaneous squamous cell carcinoma among immunocompetent individuals. J. Invest. Dermatol. 128, 1409–1417 (2008).
Strickley, J. D. et al. Immunity to commensal papillomaviruses protects against skin cancer. Nature 575, 519–522 (2019). Thought-provoking paper demonstrating how commensal viruses could prevent development of skin cancer by boosting immunity.
Herman, M. et al. Effect of cyclosporin A on DNA repair and cancer incidence in kidney transplant recipients. J. Lab. Clin. Med. 137, 14–20 (2001).
McCarroll, N. et al. An evaluation of the mode of action framework for mutagenic carcinogens case study: cyclophosphamide. Env. Mol. Mutagen. 49, 117–131 (2008).
Lin, J. Q. et al. A 10-year retrospective cohort study of ruxolitinib and association with nonmelanoma skin cancer in patients with polycythemia vera and myelofibrosis. J. Am. Acad. Dermatol. 86, 339–344 (2022).
De Simone, C. et al. Multiple squamous cell carcinomas of the skin during long-term treatment with hydroxyurea. Eur. J. Dermatol. 8, 114–115 (1998).
Ming, M., Zhao, B., Qiang, L. & He, Y. Y. Effect of immunosuppressants tacrolimus and mycophenolate mofetil on the keratinocyte UVB response. Photochem. Photobiol. 91, 242–247 (2015).
Euvrard, S. et al. Sirolimus and secondary skin-cancer prevention in kidney transplantation. N. Engl. J. Med. 367, 329–339 (2012).
Hojo, M. et al. Cyclosporine induces cancer progression by a cell-autonomous mechanism. Nature 397, 530–534 (1999).
Maluccio, M. et al. Tacrolimus enhances transforming growth factor-beta1 expression and promotes tumor progression. Transplantation 76, 597–602 (2003).
Guba, M., Graeb, C., Jauch, K. W. & Geissler, E. K. Pro- and anti-cancer effects of immunosuppressive agents used in organ transplantation. Transplantation 77, 1777–1782 (2004).
Wu, X. et al. Opposing roles for calcineurin and ATF3 in squamous skin cancer. Nature 465, 368–372 (2010).
Shin, D. et al. Association between the use of thiazide diuretics and the risk of skin cancers: a meta-analysis of observational studies. J. Clin. Med. Res. 11, 247–255 (2019).
Selvaag, E., Petersen, A. B., Gniadecki, R., Thorn, T. & Wulf, H. C. Phototoxicity to diuretics and antidiabetics in the cultured keratinocyte cell line HaCaT: evaluation by clonogenic assay and single cell gel electrophoresis Comet assay. Photodermatol. Photoimmunol. Photomed. 18, 90–95 (2002).
O’Donovan, P. et al. Azathioprine and UVA light generate mutagenic oxidative DNA damage. Science 309, 1871–1874 (2005).
Karran, P. & Brem, R. Protein oxidation, UVA and human DNA repair. DNA Repair 44, 178–185 (2016).
Williams, K., Mansh, M., Chin-Hong, P., Singer, J. & Arron, S. T. Voriconazole-associated cutaneous malignancy: a literature review on photocarcinogenesis in organ transplant recipients. Clin. Infect. Dis. 58, 997–1002 (2014).
McCarthy, K. L., Playford, E. G., Looke, D. F. & Whitby, M. Severe photosensitivity causing multifocal squamous cell carcinomas secondary to prolonged voriconazole therapy. Clin. Infect. Dis. 44, e55–e56 (2007).
Cowen, E. W. et al. Chronic phototoxicity and aggressive squamous cell carcinoma of the skin in children and adults during treatment with voriconazole. J. Am. Acad. Dermatol. 62, 31–37 (2010).
Hamandi, B. et al. Voriconazole and squamous cell carcinoma after lung transplantation: a multicenter study. Am. J. Transplant. 18, 113–124 (2018).
Tang, H., Shi, W., Song, Y. & Han, J. Voriconazole exposure and risk of cutaneous squamous cell carcinoma among lung or hematopoietic cell transplant patients: a systematic review and meta-analysis. J. Am. Acad. Dermatol. 80, 500–507 e510 (2019).
D’Arcy, M. E. et al. Voriconazole and the risk of keratinocyte carcinomas among lung transplant recipients in the United States. JAMA Dermatol. 156, 772–779 (2020).
Ikeya, S., Sakabe, J. I., Yamada, T., Naito, T. & Tokura, Y. Voriconazole-induced photocarcinogenesis is promoted by aryl hydrocarbon receptor-dependent COX-2 upregulation. Sci. Rep. 8, 5050 (2018).
Anforth, R. M. et al. Cutaneous manifestations of dabrafenib (GSK2118436): a selective inhibitor of mutant BRAF in patients with metastatic melanoma. Br. J. Dermatol. 167, 1153–1160 (2012).
Lacouture, M. E. et al. Analysis of dermatologic events in vemurafenib-treated patients with melanoma. Oncologist 18, 314–322 (2013).
Flaherty, K. T. et al. Combined BRAF and MEK inhibition in melanoma with BRAF V600 mutations. N. Engl. J. Med. 367, 1694–1703 (2012).
Robert, C. et al. Improved overall survival in melanoma with combined dabrafenib and trametinib. N. Engl. J. Med. 372, 30–39 (2015).
Pott, P. Chirurgical Observations Relative to the Cataract, the Polypus of the Nose, Cancer of the Scrotum, Different Kinds of Ruptures, and the Mortification of the Toes and Feet (printed by T. J. Carnegy, for L. Hawes, W. Clarke and R. Collins, 1775).
Siddens, L. K. et al. Polycyclic aromatic hydrocarbons as skin carcinogens: comparison of benzo[a]pyrene, dibenzo[def,p]chrysene and three environmental mixtures in the FVB/N mouse. Toxicol. Appl. Pharmacol. 264, 377–386 (2012).
De Hertog, S. A. et al. Relation between smoking and skin cancer. J. Clin. Oncol. 19, 231–238 (2001).
Braithwaite, E., Wu, X. & Wang, Z. Repair of DNA lesions induced by polycyclic aromatic hydrocarbons in human cell-free extracts: involvement of two excision repair mechanisms in vitro. Carcinogenesis 19, 1239–1246 (1998).
Shimizu, Y. et al. Benzo[a]pyrene carcinogenicity is lost in mice lacking the aryl hydrocarbon receptor. Proc. Natl Acad. Sci. USA 97, 779–782 (2000).
Hahn, M. E., Karchner, S. I., Shapiro, M. A. & Perera, S. A. Molecular evolution of two vertebrate aryl hydrocarbon (dioxin) receptors (AHR1 and AHR2) and the PAS family. Proc. Natl Acad. Sci. USA 94, 13743–13748 (1997).
Pollet, M. et al. The AHR represses nucleotide excision repair and apoptosis and contributes to UV-induced skin carcinogenesis. Cell Death Differ. 25, 1823–1836 (2018).
Luch, A. Nature and nurture — lessons from chemical carcinogenesis. Nat. Rev. Cancer 5, 113–125 (2005).
Yu, H. S., Liao, W. T. & Chai, C. Y. Arsenic carcinogenesis in the skin. J. Biomed. Sci. 13, 657–666 (2006).
Czarnecki, D., Meehan, C. J., Bruce, F. & Culjak, G. The majority of cutaneous squamous cell carcinomas arise in actinic keratoses. J. Cutan. Med. Surg. 6, 207–209 (2002).
Marks, R., Rennie, G. & Selwood, T. S. Malignant transformation of solar keratoses to squamous cell carcinoma. Lancet 1, 795–797 (1988).
Reinehr, C. P. H. & Bakos, R. M. Actinic keratoses: review of clinical, dermoscopic, and therapeutic aspects. Bras. Dermatol. 94, 637–657 (2019).
Criscione, V. D. et al. Actinic keratoses: natural history and risk of malignant transformation in the veterans affairs topical tretinoin chemoprevention trial. Cancer 115, 2523–2530 (2009).
Cassarino, D. S., Derienzo, D. P. & Barr, R. J. Cutaneous squamous cell carcinoma: a comprehensive clinicopathologic classification. Part one. J. Cutan. Pathol. 33, 191–206 (2006).
Willenbrink, T. J. et al. Field cancerization: definition, epidemiology, risk factors, and outcomes. J. Am. Acad. Dermatol. 83, 709–717 (2020).
Waldman, A. & Schmults, C. Cutaneous squamous cell carcinoma. Hematol. Oncol. Clin. North Am. 33, 1–12 (2019).
Pandeya, N., Olsen, C. M. & Whiteman, D. C. The incidence and multiplicity rates of keratinocyte cancers in Australia. Med. J. Aust. 207, 339–343 (2017).
Morton, S. & Muir, J. Field cancerization in the skin: past errors repeated. J. Am. Acad. Dermatol. 85, e41 (2021).
Pitha-Rowe, I., Petty, W. J., Kitareewan, S. & Dmitrovsky, E. Retinoid target genes in acute promyelocytic leukemia. Leukemia 17, 1723–1730 (2003).
Lebwohl, M., Tannis, C. & Carrasco, D. Acitretin suppression of squamous cell carcinoma: case report and literature review. J. Dermatol. Treat. 14, 3–6 (2003).
Kraemer, K. H., DiGiovanna, J. J., Moshell, A. N., Tarone, R. E. & Peck, G. L. Prevention of skin cancer in xeroderma pigmentosum with the use of oral isotretinoin. N. Engl. J. Med. 318, 1633–1637 (1988).
Bavinck, J. N. et al. Prevention of skin cancer and reduction of keratotic skin lesions during acitretin therapy in renal transplant recipients: a double-blind, placebo-controlled study. J. Clin. Oncol. 13, 1933–1938 (1995).
Driessens, G., Beck, B., Caauwe, A., Simons, B. D. & Blanpain, C. Defining the mode of tumour growth by clonal analysis. Nature 488, 527–530 (2012). A central study presenting experimental evidence for the existence of cancer stem cells during unperturbed solid tumour growth by clonal analysis of squamous skin tumours using genetic lineage tracing.
Latil, M. et al. Cell-type-specific chromatin states differentially prime squamous cell carcinoma tumor-initiating cells for epithelial to mesenchymal transition. Cell Stem Cell 20, 191–204.e195 (2017).
Sánchez-Danés, A. & Blanpain, C. Deciphering the cells of origin of squamous cell carcinomas. Nat. Rev. Cancer 18, 549–561 (2018).
Di Nardo, L. et al. Molecular genetics of cutaneous squamous cell carcinoma: perspective for treatment strategies. J. Eur. Acad. Dermatol. Venereol. 34, 932–941 (2020).
Wang, N. J. et al. Loss-of-function mutations in Notch receptors in cutaneous and lung squamous cell carcinoma. Proc. Natl Acad. Sci. USA 108, 17761–17766 (2011). Paper identifying NOTCH1 and NOTCH2 mutations in a majority of cSCCs.
Pacella, G. & Capell, B. C. Epigenetic and metabolic interplay in cutaneous squamous cell carcinoma. Exp. Dermatol. 30, 1115–1125 (2021).
Lee, C. S. et al. Recurrent point mutations in the kinetochore gene KNSTRN in cutaneous squamous cell carcinoma. Nat. Genet. 46, 1060–1062 (2014).
South, A. P. et al. NOTCH1 mutations occur early during cutaneous squamous cell carcinogenesis. J. Investig. Dermatol. 134, 2630–2638 (2014).
Li, Y. Y. et al. Genomic analysis of metastatic cutaneous squamous cell carcinoma. Clin. Cancer Res. 21, 1447–1456 (2015).
Ratushny, V., Gober, M. D., Hick, R., Ridky, T. W. & Seykora, J. T. From keratinocyte to cancer: the pathogenesis and modeling of cutaneous squamous cell carcinoma. J. Clin. Invest. 122, 464–472 (2012).
Tufaro, A. P. et al. Molecular markers in cutaneous squamous cell carcinoma. Int. J. Surg. Oncol. 2011, 231475 (2011).
Nassar, D., Latil, M., Boeckx, B., Lambrechts, D. & Blanpain, C. Genomic landscape of carcinogen-induced and genetically induced mouse skin squamous cell carcinoma. Nat. Med. 21, 946–954 (2015). A comprehensive analysis of DMBA-induced skin cancer.
Huang, P. Y. & Balmain, A. Modeling cutaneous squamous carcinoma development in the mouse. Cold Spring Harb. Perspect. Med. 4, a013623 (2014).
Balmain, A. & Pragnell, I. B. Mouse skin carcinomas induced in vivo by chemical carcinogens have a transforming Harvey-ras oncogene. Nature 303, 72–74 (1983). Seminal paper showing that mouse cSCCs induced by chemical carcinogens contain a Hras oncogene.
Morris, R. J., Fischer, S. M. & Slaga, T. J. Evidence that a slowly cycling subpopulation of adult murine epidermal cells retains carcinogen. Cancer Res. 46, 3061–3066 (1986).
Furstenberger, G. et al. Stimulatory role of transforming growth factors in multistage skin carcinogenesis: possible explanation for the tumor-inducing effect of wounding in initiated NMRI mouse skin. Int. J. Cancer 43, 915–921 (1989).
Guasch, G. et al. Loss of TGFβ signaling destabilizes homeostasis and promotes squamous cell carcinomas in stratified epithelia. Cancer Cell 12, 313–327 (2007). Paper showing how TGFβ signalling promotes cSCC and perturbs tissue homeostasis.
Owens, D. M. & Watt, F. M. Influence of β1 integrins on epidermal squamous cell carcinoma formation in a transgenic mouse model: α3β1, but not α2β1, suppresses malignant conversion1. Cancer Res. 61, 5248–5254 (2001). This paper shows how integrin signalling in cSCC can suppress malignant conversion.
Owens, D. M. & Watt, F. M. Contribution of stem cells and differentiated cells to epidermal tumours. Nat. Rev. Cancer 3, 444–451 (2003).
Owens, D. M., Romero, M. R., Gardner, C. & Watt, F. M. Suprabasal α6β4 integrin expression in epidermis results in enhanced tumourigenesis and disruption of TGFβ signalling. J. Cell Sci. 116, 3783–3791 (2003).
Quintanilla, M., Brown, K., Ramsden, M. & Balmain, A. Carcinogen-specific mutation and amplification of Ha-ras during mouse skin carcinogenesis. Nature 322, 78–80 (1986).
Wong, C. E. et al. Inflammation and Hras signaling control epithelial-mesenchymal transition during skin tumor progression. Genes Dev. 27, 670–682 (2013).
Pastushenko, I. et al. Fat1 deletion promotes hybrid EMT state, tumour stemness and metastasis. Nature 589, 448–455 (2021).
Dajee, M. et al. NF-κB blockade and oncogenic Ras trigger invasive human epidermal neoplasia. Nature 421, 639–643 (2003).
Ortiz-Urda, S. et al. Type VII collagen is required for Ras-driven human epidermal tumorigenesis. Science 307, 1773–1776 (2005). These findings show how type VII collagen is required for tumour–stroma interactions in cSCC.
Khavari, P. A. Modelling cancer in human skin tissue. Nat. Rev. Cancer 6, 270–280 (2006).
Lazarov, M. et al. CDK4 coexpression with Ras generates malignant human epidermal tumorigenesis. Nat. Med. 8, 1105–1114 (2002). This paper reveals the mechanism by which oncogenic Ras controls CDK4 to drive invasive human neoplasia resembling cSCC.
Ridky, T. W., Chow, J. M., Wong, D. J. & Khavari, P. A. Invasive three-dimensional organotypic neoplasia from multiple normal human epithelia. Nat. Med. 16, 1450–1455 (2010). This paper establishes an invasive in vitro 3D model of organotypic neoplasia, recapitulating major features of cSCC.
Reuter, J. A. et al. Modeling inducible human tissue neoplasia identifies an extracellular matrix interaction network involved in cancer progression. Cancer Cell 15, 477–488 (2009).
Jameson, K. L. et al. IQGAP1 scaffold-kinase interaction blockade selectively targets RAS-MAP kinase-driven tumors. Nat. Med. 19, 626–630 (2013).
Goldie, S. J., Chincarini, G. & Darido, C. Targeted therapy against the cell of origin in cutaneous squamous cell carcinoma. Int. J. Mol. Sci. 20, 2201 (2019).
Coulombe, P. A., Bernot, K. M. & Lee, C. H. in Encyclopedia of Biological Chemistry 2nd edn (eds Lennarz, W. J. & Lane, M. D.) 665–671 (Academic Press, 2013).
Brown, K., Strathdee, D., Bryson, S., Lambie, W. & Balmain, A. The malignant capacity of skin tumours induced by expression of a mutant H-ras transgene depends on the cell type targeted. Curr. Biol. 8, 516–524 (1998).
Bailleul, B. et al. Skin hyperkeratosis and papilloma formation in transgenic mice expressing a ras oncogene from a suprabasal keratin promoter. Cell 62, 697–708 (1990).
Greenhalgh, D. A. et al. Induction of epidermal hyperplasia, hyperkeratosis, and papillomas in transgenic mice by a targeted v-Ha-ras oncogene. Mol. Carcinog. 7, 99–110 (1993).
White, A. C. et al. Defining the origins of Ras/p53-mediated squamous cell carcinoma. Proc. Natl Acad. Sci. USA 108, 7425–7430 (2011).
Lapouge, G. et al. Identifying the cellular origin of squamous skin tumors. Proc. Natl Acad. Sci. USA 108, 7431–7436 (2011).
Lynch, M. D. & Watt, F. M. Fibroblast heterogeneity: implications for human disease. J. Clin. Invest. 128, 26–35 (2018).
Wong, V. W., Sorkin, M., Glotzbach, J. P., Longaker, M. T. & Gurtner, G. C. Surgical approaches to create murine models of human wound healing. J. Biomed. Biotechnol. 2011, 969618 (2011).
Jonason, A. S. et al. Frequent clones of p53-mutated keratinocytes in normal human skin. Proc. Natl Acad. Sci. 93, 14025–14029 (1996). This study discovers how, in addition to being a tumorigenic mutagen, sunlight acts as a tumour promoter by favouring the clonal expansion of p53-mutant cells in skin.
Albibas, A. A. et al. Subclonal evolution of cancer-related gene mutations in p53 immunopositive patches in human skin. J. Investig. Dermatol. 138, 189–198 (2018).
Reeves, M. Q., Kandyba, E., Harris, S., Del Rosario, R. & Balmain, A. Multicolour lineage tracing reveals clonal dynamics of squamous carcinoma evolution from initiation to metastasis. Nat. Cell Biol. 20, 699–709 (2018).
Ezhkova, E. et al. Ezh2 orchestrates gene expression for the stepwise differentiation of tissue-specific stem cells. Cell 136, 1122–1135 (2009).
Hernández-Ruiz, E. et al. The Polycomb proteins RING1B and EZH2 repress the tumoral pro-inflammatory function in metastasizing primary cutaneous squamous cell carcinoma. Carcinogenesis 39, 503–513 (2018).
Teknos, T. N. et al. A phase 1 trial of vorinostat in combination with concurrent chemoradiation therapy in the treatment of advanced staged head and neck squamous cell carcinoma. Invest. N. Drugs 37, 702–710 (2019).
Kurundkar, D. et al. Vorinostat, an HDAC inhibitor attenuates epidermoid squamous cell carcinoma growth by dampening mTOR signaling pathway in a human xenograft murine model. Toxicol. Appl. Pharmacol. 266, 233–244 (2013).
Kilgour, J. M. et al. Treatment of cutaneous squamous cell carcinoma with the topical histone deacetylase inhibitor remetinostat. JAMA Dermatol. 158, 105–107 (2022).
Brown, V. L. et al. p16INK4a and p14ARF tumor suppressor genes are commonly inactivated in cutaneous squamous cell carcinoma. J. Invest. Dermatol. 122, 1284–1292 (2004).
Hervás-Marín, D. et al. Genome wide DNA methylation profiling identifies specific epigenetic features in high-risk cutaneous squamous cell carcinoma. PLoS ONE 14, e0223341 (2019).
Bao, X. et al. CSNK1a1 regulates PRMT1 to maintain the progenitor state in self-renewing somatic tissue. Dev. Cell 43, 227–239 e225 (2017).
Sen, G. L., Reuter, J. A., Webster, D. E., Zhu, L. & Khavari, P. A. DNMT1 maintains progenitor function in self-renewing somatic tissue. Nature 463, 563–567 (2010).
Darr, O. A. et al. Epigenetic alterations in metastatic cutaneous carcinoma. Head Neck 37, 994–1001 (2015).
Sahai, E. et al. A framework for advancing our understanding of cancer-associated fibroblasts. Nat. Rev. Cancer 20, 174–186 (2020).
Hanahan, D. & Coussens, L. M. Accessories to the crime: functions of cells recruited to the tumor microenvironment. Cancer Cell 21, 309–322 (2012).
Guo, X. et al. Global characterization of T cells in non-small-cell lung cancer by single-cell sequencing. Nat. Med. 24, 978–985 (2018).
Puram, S. V. et al. Single-cell transcriptomic analysis of primary and metastatic tumor ecosystems in head and neck cancer. Cell 171, 1611–1624 e1624 (2017).
Savas, P. et al. Single-cell profiling of breast cancer T cells reveals a tissue-resident memory subset associated with improved prognosis. Nat. Med. 24, 986–993 (2018).
Yost, K. E. et al. Clonal replacement of tumor-specific T cells following PD-1 blockade. Nat. Med. 25, 1251–1259 (2019).
Zheng, C. et al. Landscape of infiltrating T cells in liver cancer revealed by single-cell sequencing. Cell 169, 1342–1356 e1316 (2017).
Zhang, L. et al. Lineage tracking reveals dynamic relationships of T cells in colorectal cancer. Nature 564, 268–272 (2018).
Miao, Y. et al. Adaptive immune resistance emerges from tumor-initiating stem cells. Cell 177, 1172–1186 e1114 (2019).
Bissell, M. J. & Hines, W. C. Why don’t we get more cancer? A proposed role of the microenvironment in restraining cancer progression. Nat. Med. 17, 320–329 (2011).
Flaberg, E. et al. High-throughput live-cell imaging reveals differential inhibition of tumor cell proliferation by human fibroblasts. Int. J. Cancer 128, 2793–2802 (2011).
Kalluri, R. The biology and function of fibroblasts in cancer. Nat. Rev. Cancer 16, 582–598 (2016).
Katarkar, A. et al. NOTCH1 gene amplification promotes expansion of cancer associated fibroblast populations in human skin. Nat. Commun. 11, 5126 (2020).
Beebe, E. et al. Defining the molecular landscape of cancer-associated stroma in cutaneous squamous cell carcinoma. J. Invest. Dermatol. 142, 3304–3312 (2022).
Liu, T. et al. Cancer-associated fibroblasts: an emerging target of anti-cancer immunotherapy. J. Hematol. Oncol. 12, 86 (2019).
Khalili, J. S. et al. Oncogenic BRAF(V600E) promotes stromal cell-mediated immunosuppression via induction of interleukin-1 in melanoma. Clin. Cancer Res. 18, 5329–5340 (2012).
Nazareth, M. R. et al. Characterization of human lung tumor-associated fibroblasts and their ability to modulate the activation of tumor-associated T cells. J. Immunol. 178, 5552–5562 (2007).
Lim, Y. Z. & South, A. P. Tumour-stroma crosstalk in the development of squamous cell carcinoma. Int. J. Biochem. Cell Biol. 53, 450–458 (2014).
Berx, G. & van Roy, F. Involvement of members of the cadherin superfamily in cancer. Cold Spring Harb. Perspect. Biol. 1, a003129 (2009).
Rodriguez, F. J., Lewis-Tuffin, L. J. & Anastasiadis, P. Z. E-cadherin’s dark side: possible role in tumor progression. Biochim. Biophys. Acta 1826, 23–31 (2012).
Zhang, Y., Lu, H., Dazin, P. & Kapila, Y. Squamous cell carcinoma cell aggregates escape suspension-induced, p53-mediated anoikis: fibronectin and integrin αv mediate survival signals through focal adhesion kinase. J. Biol. Chem. 279, 48342–48349 (2004).
Schafer, M. & Werner, S. Cancer as an overhealing wound: an old hypothesis revisited. Nat. Rev. Mol. Cell Biol. 9, 628–638 (2008).
Strieth, S., Hartschuh, W., Pilz, L. & Fusenig, N. E. Angiogenic switch occurs late in squamous cell carcinomas of human skin. Br. J. Cancer 82, 591–600 (2000).
Azimi, A. et al. Differential proteomic analysis of actinic keratosis, Bowen’s disease and cutaneous squamous cell carcinoma by label-free LC-MS/MS. J. Dermatol. Sci. 91, 69–78 (2018).
Lichtenberger, B. M. et al. Autocrine VEGF signaling synergizes with EGFR in tumor cells to promote epithelial cancer development. Cell 140, 268–279 (2010).
Beck, B. et al. A vascular niche and a VEGF-Nrp1 loop regulate the initiation and stemness of skin tumours. Nature 478, 399–403 (2011).
Argiris, A. et al. Phase III randomized trial of chemotherapy with or without bevacizumab in patients with recurrent or metastatic head and neck cancer. J. Clin. Oncol. 37, 3266–3274 (2019).
Mantovani, A., Garlanda, C. & Allavena, P. Molecular pathways and targets in cancer-related inflammation. Ann. Med. 42, 161–170 (2010).
Arwert, E. N. et al. Tumor formation initiated by nondividing epidermal cells via an inflammatory infiltrate. Proc. Natl Acad. Sci. USA 107, 19903–19908 (2010).
Dvorak, H. F. Tumors: wounds that do not heal. Similarities between tumor stroma generation and wound healing. N. Engl. J. Med. 315, 1650–1659 (1986).
Naik, S. et al. Inflammatory memory sensitizes skin epithelial stem cells to tissue damage. Nature 550, 475–480 (2017). This paper demonstrates how epidermal stem cells develop a prolonged memory to acute inflammation through altered chromatin accessibility at key response genes, and suggests that this enhanced sensitivity increases susceptibility to cancer.
Linde, N. et al. Vascular endothelial growth factor-induced skin carcinogenesis depends on recruitment and alternative activation of macrophages. J. Pathol. 227, 17–28 (2012).
Qin, H. et al. Gene therapy for head and neck cancer using vaccinia virus expressing IL-2 in a murine model, with evidence of immune suppression. Mol. Ther. 4, 551–558 (2001).
Rohrer, J. W. & Coggin, J. H. Jr CD8 T cell clones inhibit antitumor T cell function by secreting IL-10. J. Immunol. 155, 5719–5727 (1995).
Goudie, D. R. et al. Multiple self-healing squamous epithelioma is caused by a disease-specific spectrum of mutations in TGFBR1. Nat. Genet. 43, 365–369 (2011).
Chen, J. et al. Interferon-γ-induced PD-L1 surface expression on human oral squamous carcinoma via PKD2 signal pathway. Immunobiology 217, 385–393 (2012).
Strome, S. E. et al. B7-H1 blockade augments adoptive T-cell immunotherapy for squamous cell carcinoma. Cancer Res. 63, 6501–6505 (2003).
Slater, N. A. & Googe, P. B. PD-L1 expression in cutaneous squamous cell carcinoma correlates with risk of metastasis. J. Cutan. Pathol. 43, 663–670 (2016).
Okiyama, N. & Katz, S. I. Programmed cell death 1 (PD-1) regulates the effector function of CD8 T cells via PD-L1 expressed on target keratinocytes. J. Autoimmun. 53, 1–9 (2014).
Arwert, E. N. et al. STING and IRF3 in stromal fibroblasts enable sensing of genomic stress in cancer cells to undermine oncolytic viral therapy. Nat. Cell Biol. 22, 758–766 (2020).
Guy, G. P. Jr, Machlin, S. R., Ekwueme, D. U. & Yabroff, K. R. Prevalence and costs of skin cancer treatment in the US, 2002–2006 and 2007–2011. Am. J. Prev. Med. 48, 183–187 (2015).
Singer, D. S. A new phase of the Cancer Moonshot to end cancer as we know it. Nat. Med. 28, 1345–1347 (2022).
Ernst, A., Grimm, A. & Lim, H. W. Tanning lamps: health effects and reclassification by the Food and Drug Administration. J. Am. Acad. Dermatol. 72, 175–180 (2015).
U.S. Department of Health and Human Services. The Surgeon General’s Call to Action to Prevent Skin Cancer (Office of the Surgeon General, 2014).
Force, U. S. P. S. T. et al. Behavioral counseling to prevent skin cancer: US preventive services task force recommendation statement. J. Am. Med. Assoc. 319, 1134–1142 (2018).
Jones, O. T. et al. Artificial intelligence and machine learning algorithms for early detection of skin cancer in community and primary care settings: a systematic review. Lancet Digit. Health 4, e466–e476 (2022).
Force, U. S. P. S. T. et al. Screening for skin cancer: US preventive services task force recommendation statement. J. Am. Med. Assoc. 316, 429–435 (2016).
Riemenschneider, K., Liu, J. & Powers, J. G. Skin cancer in the military: a systematic review of melanoma and nonmelanoma skin cancer incidence, prevention, and screening among active duty and veteran personnel. J. Am. Acad. Dermatol. 78, 1185–1192 (2018).
Weinstock, M. A. et al. Chemoprevention of basal and squamous cell carcinoma with a single course of fluorouracil, 5%, cream: a randomized clinical trial. JAMA Dermatol. 154, 167–174 (2018).
Chen, A. C. et al. A phase 3 randomized trial of nicotinamide for skin-cancer chemoprevention. N. Engl. J. Med. 373, 1618–1626 (2015).
Surjana, D., Halliday, G. M. & Damian, D. L. Nicotinamide enhances repair of ultraviolet radiation-induced DNA damage in human keratinocytes and ex vivo skin. Carcinogenesis 34, 1144–1149 (2013).
Carneiro, R. V., Sotto, M. N., Azevedo, L. S., Ianhez, L. E. & Rivitti, E. A. Acitretin and skin cancer in kidney transplanted patients. Clinical and histological evaluation and immunohistochemical analysis of lymphocytes, natural killer cells and Langerhans’ cells in sun exposed and sun protected skin. Clin. Transpl. 19, 115–121 (2005).
Solomon-Cohen, E., Reiss-Huss, S., Hodak, E. & Davidovici, B. Low-dose acitretin for secondary prevention of keratinocyte carcinomas in solid-organ transplant recipients. Dermatology 238, 161–166 (2022).
Patel, G. K. et al. Imiquimod 5% cream monotherapy for cutaneous squamous cell carcinoma in situ (Bowen’s disease): a randomized, double-blind, placebo-controlled trial. J. Am. Acad. Dermatol. 54, 1025–1032 (2006).
Salido-Vallejo, R. et al. Neoadjuvant intralesional methotrexate in cutaneous squamous cell carcinoma: a comparative cohort study. J. Eur. Acad. Dermatol. Venereol. 30, 1120–1124 (2016).
Metterle, L., Nelson, C. & Patel, N. Intralesional 5-fluorouracil (FU) as a treatment for nonmelanoma skin cancer (NMSC): a review. J. Am. Acad. Dermatol. 74, 552–557 (2016).
Hanlon, A., Kim, J. & Leffell, D. J. Intralesional interferon alfa-2b for refractory, recurrent squamous cell carcinoma of the face. J. Am. Acad. Dermatol. 69, 1070–1072 (2013).
Work, G. et al. Guidelines of care for the management of cutaneous squamous cell carcinoma. J. Am. Acad. Dermatol. 78, 560–578 (2018).
Navarrete-Dechent, C., Veness, M. J., Droppelmann, N. & Uribe, P. High-risk cutaneous squamous cell carcinoma and the emerging role of sentinel lymph node biopsy: a literature review. J. Am. Acad. Dermatol. 73, 127–137 (2015).
Durham, A. B. et al. Sentinel lymph node biopsy for cutaneous squamous cell carcinoma on the head and neck. JAMA Otolaryngol. Head. Neck Surg. 142, 1171–1176 (2016).
Maubec, E. et al. Phase II study of cetuximab as first-line single-drug therapy in patients with unresectable squamous cell carcinoma of the skin. J. Clin. Oncol. 29, 3419–3426 (2011).
Foote, M. C. et al. Phase II study of single-agent panitumumab in patients with incurable cutaneous squamous cell carcinoma. Ann. Oncol. 25, 2047–2052 (2014).
Migden, M. R. et al. Cemiplimab in locally advanced cutaneous squamous cell carcinoma: results from an open-label, phase 2, single-arm trial. Lancet Oncol. 21, 294–305 (2020). Phase II trial showing great promise of PDL1 inhibition in cSCC, changing the field of therapy for advanced cSCC.
Migden, M. R. et al. PD-1 blockade with cemiplimab in advanced cutaneous squamous-cell carcinoma. N. Engl. J. Med. 379, 341–351 (2018).
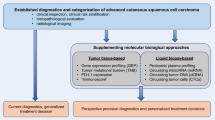
Harwood, C. A., Proby, C. M., Inman, G. J. & Leigh, I. M. The promise of genomics and the development of targeted therapies for cutaneous squamous cell carcinoma. Acta Derm. Venereol. 96, 3–16 (2016).
Chang, A. L., Kim, J., Luciano, R., Sullivan-Chang, L. & Colevas, A. D. A case report of unresectable cutaneous squamous cell carcinoma responsive to pembrolizumab, a programmed cell death protein 1 inhibitor. JAMA Dermatol. 152, 106–108 (2016). Seminal paper showing responsiveness to pembrolizumab in unresectable cSCC.
Chalmers, Z. R. et al. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med. 9, 34 (2017).
Curiel, C. N. et al. A single arm phase 2 study of talimogene laherparepvec in patients with low-risk invasive cutaneous squamous cell cancer. interim analysis. J. Clin. Oncol. 40, e21583–e21583 (2022).
Nguyen, T. A., Offner, M., Hamid, O., Zumsteg, Z. S. & Gharavi, N. M. Complete and sustained remission of metastatic cutaneous squamous cell carcinoma in a liver transplant patient treated with talimogene laherparepvec. Dermatol. Surg. 47, 820–822 (2021).
US National Library of Medicine. ClinicalTrials.gov https://ClinicalTrials.gov/show/NCT03714828 (2023).
Rajadhyaksha, M., Marghoob, A., Rossi, A., Halpern, A. C. & Nehal, K. S. Reflectance confocal microscopy of skin in vivo: From bench to bedside. Lasers Surg. Med. 49, 7–19 (2017).
Esteva, A. et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature 542, 115–118 (2017).
Nikolaou, V., Stratigos, A. J. & Tsao, H. Hereditary nonmelanoma skin cancer. Semin. Cutan. Med. Surg. 31, 204–210 (2012).
Smith, P. J. & Paterson, M. C. Enhanced radiosensitivity and defective DNA repair in cultured fibroblasts derived from Rothmund Thomson syndrome patients. Mutat. Res. 94, 213–228 (1982).
Ghosh, A. K. et al. RECQL4, the protein mutated in Rothmund-Thomson syndrome, functions in telomere maintenance. J. Biol. Chem. 287, 196–209 (2012).
Franchitto, A. & Pichierri, P. Protecting genomic integrity during DNA replication: correlation between Werner’s and Bloom’s syndrome gene products and the MRE11 complex. Hum. Mol. Genet. 11, 2447–2453 (2002).
Bolognia, J. L., Schaffer, J. V. & Cerroni, L. Dermatology 4th edn (Elsevier Saunders, 2018).
Emmert, H., Patel, H. & Brunton, V. G. Kindlin-1 protects cells from oxidative damage through activation of ERK signalling. Free Radic. Biol. Med. 108, 896–903 (2017).
Vulliamy, T. J. et al. Mutations in dyskeratosis congenita: their impact on telomere length and the diversity of clinical presentation. Blood 107, 2680–2685 (2006).
Alter, B. P., Giri, N., Savage, S. A. & Rosenberg, P. S. Cancer in dyskeratosis congenita. Blood 113, 6549–6557 (2009).
Waterman, E. A. et al. A laminin-collagen complex drives human epidermal carcinogenesis through phosphoinositol-3-kinase activation. Cancer Res. 67, 4264–4270 (2007).
Tasanen, K., Tunggal, L., Chometon, G., Bruckner-Tuderman, L. & Aumailley, M. Keratinocytes from patients lacking collagen XVII display a migratory phenotype. Am. J. Pathol. 164, 2027–2038 (2004).
de Jong, S. J. et al. The human CIB1-EVER1-EVER2 complex governs keratinocyte-intrinsic immunity to beta-papillomaviruses. J. Exp. Med. 215, 2289–2310 (2018).
Youssefian, L. et al. Epidermodysplasia verruciformis: genetic heterogeneity and EVER1 and EVER2 mutations revealed by genome-wide analysis. J. Invest. Dermatol. 139, 241–244 (2019).
Rosenberg, P. S., Greene, M. H. & Alter, B. P. Cancer incidence in persons with Fanconi anemia. Blood 101, 822–826 (2003).
Brash, D. E. et al. A role for sunlight in skin cancer: UV-induced p53 mutations in squamous cell carcinoma. Proc. Natl Acad. Sci. USA 88, 10124–10128 (1991).
Purdie, K. J. et al. Single nucleotide polymorphism array analysis defines a specific genetic fingerprint for well-differentiated cutaneous SCCs. J. Invest. Dermatol. 129, 1562–1568 (2009).
Chang, D. & Shain, A. H. The landscape of driver mutations in cutaneous squamous cell carcinoma. NPJ Genom. Med. 6, 61 (2021).
Pierceall, W. E., Goldberg, L. H., Tainsky, M. A., Mukhopadhyay, T. & Ananthaswamy, H. N. Ras gene mutation and amplification in human nonmelanoma skin cancers. Mol. Carcinog. 4, 196–202 (1991).
Sherr, C. J. & McCormick, F. The RB and p53 pathways in cancer. Cancer Cell 2, 103–112 (2002).
Almquist, L. M. et al. The role of TP53 and MDM2 polymorphisms in TP53 mutagenesis and risk of non-melanoma skin cancer. Carcinogenesis 32, 327–330 (2011).
William, W. N. Jr et al. Gefitinib for patients with incurable cutaneous squamous cell carcinoma: A single-arm phase II clinical trial. J. Am. Acad. Dermatol. 77, 1110–1113 e1112 (2017).
Jenni, D. et al. A prospective clinical trial to assess lapatinib effects on cutaneous squamous cell carcinoma and actinic keratosis. ESMO Open 1, e000003 (2016).
Grob, J. J. et al. Pembrolizumab monotherapy for recurrent or metastatic cutaneous squamous cell carcinoma: a single-arm phase II trial (KEYNOTE-629). J. Clin. 38, 2916–2925 (2020).
Boutros, A. et al. Immunotherapy for the treatment of cutaneous squamous cell carcinoma. Front. Oncol. 11, 733917 (2021).
Maxfield, L., Shah, M., Schwartz, C., Tanner, L. S. & Appel, J. Intralesional 5-fluorouracil for the treatment of squamous cell carcinomas. J. Am. Acad. Dermatol. 84, 1696–1697 (2021).
Gualdi, G. et al. Intralesional methotrexate for the treatment of advanced keratinocytic tumors: a multi-center retrospective study. Dermatol. Ther. 10, 769–777 (2020).
Lydiatt, W. M. et al. Head and neck cancers-major changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA Cancer J. Clin. 67, 122–137 (2017).
Jambusaria-Pahlajani, A. et al. Evaluation of AJCC tumor staging for cutaneous squamous cell carcinoma and a proposed alternative tumor staging system. JAMA Dermatol. 149, 402–410 (2013).
Ruiz, E. S., Karia, P. S., Besaw, R. & Schmults, C. D. Performance of the American Joint Committee on Cancer Staging Manual, 8th Edition vs the Brigham and Women’s Hospital Tumor Classification System for Cutaneous Squamous Cell Carcinoma. JAMA Dermatol. 155, 819–825 (2019).
Wysong, A. et al. Validation of a 40-gene expression profile test to predict metastatic risk in localized high-risk cutaneous squamous cell carcinoma. J. Am. Acad. Dermatol. 84, 361–369 (2021).
Ibrahim, S. F. et al. Enhanced metastatic risk assessment in cutaneous squamous cell carcinoma with the 40-gene expression profile test. Future Oncol. 18, 833–847 (2022).
Kwiek, B. & Schwartz, R. A. Keratoacanthoma (KA): an update and review. J. Am. Acad. Dermatol. 74, 1220–1233 (2016).
Goldberg, L. H. et al. Keratoacanthoma as a postoperative complication of skin cancer excision. J. Am. Acad. Dermatol. 50, 753–758 (2004).
Schwartz, R. A. Keratoacanthoma: a clinico-pathologic enigma. Dermatol. Surg. 30, 326–333 (2004). discussion 333.
Ramselaar, C. G., Ruitenberg, E. J. & Kruizinga, W. Regression of induced keratoacanthomas in anagen (hair growth phase) skin grafts in mice. Cancer Res. 40, 1668–1673 (1980).
Acknowledgements
The authors thank members of the Khavari laboratory for helpful discussions. This work was supported by the US Veterans Affairs Office of Research and Development I01BX00140908, NIH, National Cancer Institute (NIH/NCI) CA142635, and by NIH, National Institute for Arthritis and Musculoskeletal and Skin Diseases (NIH/NIAMS) AR43799 and AR49737 (P.A.K.).
Author information
Authors and Affiliations
Contributions
M.C.G.W. wrote the article and designed and executed the primary literature search. L.N.K. wrote a section of the manuscript, and L.N.K., K.G., K.Y.S., S.Z.A., J.Y.T. and S.M.S. contributed substantially to discussions of the content, assisted with the literature search, and edited the manuscript. A.L.S.C. co-wrote a section of the manuscript, assisted with the literature search, edited, critically reviewed and revised the manuscript. P.A.K. conceptualized the article and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
A.L.S.C. has been a clinical investigator and advisory board member for Regeneron and Merck, an advisory board member for Castle Biosciences and a consultant for Feldan Therapeutics. M.C.G.W. is a cofounder of PSOMRI Holding AB. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Cancer thanks Gian-Paolo Dotto, who co-reviewed with Sandro Gorupp; Cedric Blanpain; and Shawn Demehri for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Acantholytic SCC
-
A type of cutaneous squamous cell carcinoma that involves the breakdown of connections between skin cells.
- Actinic keratosis
-
(AK). A premalignant lesion and common cutaneous squamous cell carcinoma precursor characterized by in situ epidermal dysplasia. It forms on skin damaged by chronic exposure to UV radiation from the sun and/or indoor tanning.
- Bulge
-
A region of the hair follicle in which hair stem cells are located.
- Cauterization
-
The process of heating tissue with an instrument or chemical to stop bleeding or to remove tissue.
- cSCC in situ
-
Cutaneous squamous cell carcinoma in situ, also known as Bowen’s disease, is an intra-epidermal malignancy of the skin with a 3–5% risk of progression to invasive carcinoma when left untreated.
- Cutaneous graft versus host disease
-
An immune-mediated condition after transplantation, in which grafted immune cells recognize host skin antigens as foreign, resulting in a complex interaction between donor and recipient adaptive immunity.
- Ferguson–Smith syndrome
-
A rare genetic disorder characterized by the development of multiple skin tumours, including keratoacanthomas and trichoepitheliomas.
- Field cancerization
-
The concept of how large areas of skin are affected by tumorigenic changes. This arises from prolonged DNA-damaging exposure over time, such as chronic UV exposure.
- Foramen
-
An anatomical opening or passage in a bone that allows nerves and blood vessels to pass through.
- Hair follicle stem cells
-
A type of epidermal stem cell found in hair follicles that can differentiate into various cell types, including hair cells.
- Interfollicular epidermis
-
The stratified squamous epithelium located between hair follicles that regenerates from the pool of stem cell progenitors in the basal layer.
- Intralesional therapies
-
Delivery of a therapeutic directly into the tumour or lesion, commonly by injection.
- Jadassohn variant
-
In the context of cutaneous squamous cell carcinoma a rare variant, often classified as of intermediate risk, morphologically characterized by the presence of well-defined islands of monomorphic epithelial cells, typical or atypical, within a thickened epidermis.
- Lamina-associated domains
-
(LADs). Genomic regions that are in close contact with the nuclear lamina, a fibrous layer that lines the inner nuclear membrane. LADs help to establish interphase chromosome topology and may have a role in gene repression.
- Langerhans cells
-
A type of immune cell found in the skin that has a key role in antigen detection and responses.
- Lymphoepithelioma-like subtype
-
A rare variant of squamous cell carcinoma that involves lymphoid tissue.
- Mohs micrographic surgery
-
A surgery technique named after Frederick Mohs that is a tissue-sparing method of skin cancer removal that involves microscopic, intra-operative examination of all tissue margins.
- Muir–Torre syndrome
-
A rare genetic condition caused by germline mutations in DNA mismatch repair genes, characterized by the development of sebaceous tumours and certain types of cancer, particularly in the gastrointestinal tract.
- Non-Mendelian polygenic inheritance pattern
-
An inheritance pattern with a complex genetic basis involving more genomic loci than single loci patterns normally observed in classical autosomal dominant and recessive inheritance.
- Oncolytic virus
-
A genetically engineered or naturally existing virus that can selectively replicate in cancer cells and kill them without damaging healthy cells.
- Perineural invasion
-
The spread of cancer cells along nerves.
- Pigmentation
-
The process of deposition of the pigment melanin in pigment granules of keratinocytes.
- Pilar tumours
-
A type of cutaneous tumour that arises from hair follicles.
- Recessive dystrophic epidermolysis bullosa
-
(RDEB). An incurable, often fatal, condition characterized by severe skin blistering, chronic wounding and inflammation that is caused by lack of functional type VII collagen protein in the skin.
- Spatial transcriptomics
-
Technology that enables spatial mapping of particular mRNA transcripts to specific locations in a tissue.
- Transit-amplifying cells
-
Progenitor cells that, after stem cell division, undergo several rounds of cell division to produce a large number of specialized cells.
- Ungual cSCC
-
Cutaneous squamous cell carcinoma of the nail unit that often invades more quickly and has higher association with human papillomavirus (HPV), especially HPV16.
- UV signature
-
The pattern of specific UV-induced DNA mutations produced by sunlight, commonly leading to a C>T transversion.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Winge, M.C.G., Kellman, L.N., Guo, K. et al. Advances in cutaneous squamous cell carcinoma. Nat Rev Cancer 23, 430–449 (2023). https://doi.org/10.1038/s41568-023-00583-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41568-023-00583-5
This article is cited by
-
Understanding the charismatic potential of nanotechnology to treat skin carcinoma
Medical Oncology (2023)