Abstract
Although it is known that household infections drive the transmission of dengue virus (DENV), it is unclear how household composition and the immune status of inhabitants affect the individual risk of infection. Most population-based studies to date have focused on paediatric cohorts because more severe forms of dengue mainly occur in children, and the role of adults in dengue transmission is understudied. Here we analysed data from a multigenerational cohort study of 470 households, comprising 2,860 individuals, in Kamphaeng Phet, Thailand, to evaluate risk factors for DENV infection. Using a gradient-boosted regression model trained on annual haemagglutination inhibition antibody titre inputs, we identified 1,049 infections, 90% of which were subclinical. By analysing imputed infections, we found that individual antibody titres, household composition and antibody titres of other members in the same household affect an individual’s risk of DENV infection. Those individuals living in households with high average antibody titres, or households with more adults, had a reduced risk of infection. We propose that herd immunity to dengue acts at the household level and may provide insight into the drivers of the recent change in the shifting age distribution of dengue cases in Thailand.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The dataset analysed in this study is available at https://github.com/marcohamins/role-of-HH-immunity.
Code availability
All code associated with the work is available at https://github.com/marcohamins/role-of-HH-immunity.
References
Cattarino, L., Rodriguez-Barraquer, I., Imai, N., Cummings, D. A. T. & Ferguson, N. M. Mapping global variation in dengue transmission intensity. Sci. Transl. Med. 12, eaax4144 (2020).
Wilder-Smith, A., Ooi, E.-E., Horstick, O. & Wills, B. Dengue. Lancet 393, 350–363 (2019).
Bhatt, S. et al. The global distribution and burden of dengue. Nature 496, 504–507 (2013).
Dos Santos, G. R. et al. Individual, household, and community drivers of dengue virus infection risk in Kamphaeng Phet Province, Thailand. J. Infect. Dis. 226, 1348–1356 (2022).
Salje, H. et al. Dengue diversity across spatial and temporal scales: local structure and the effect of host population size. Science 355, 1302–1306 (2017).
Yoon, I.-K. et al. Fine scale spatiotemporal clustering of dengue virus transmission in children and Aedes aegypti in rural Thai villages. PLoS Negl. Trop. Dis. 6, e1730 (2012).
Anders, K. L. et al. Households as foci for dengue transmission in highly urban Vietnam. PLoS Negl. Trop. Dis. 9, e0003528 (2015).
Cuong, H. Q. et al. Spatiotemporal dynamics of dengue epidemics, southern Vietnam. Emerg. Infect. Dis. 19, 945–953 (2013).
Salje, H. et al. Revealing the microscale spatial signature of dengue transmission and immunity in an urban population. Proc. Natl Acad. Sci. USA 109, 9535–9538 (2012).
Ratanawong, P. et al. Spatial variations in dengue transmission in schools in Thailand. PLoS ONE 11, e0161895 (2016).
Chen, Y. et al. Measuring the effects of COVID-19-related disruption on dengue transmission in Southeast Asia and Latin America: a statistical modelling study. Lancet Infect. Dis. 22, 657–667 (2022).
Undurraga, E. A., Halasa, Y. A. & Shepard, D. S. Use of expansion factors to estimate the burden of dengue in Southeast Asia: a systematic analysis. PLoS Negl. Trop. Dis. 7, e2056 (2013).
Clapham, H. E., Cummings, D. A. T. & Johansson, M. A. Immune status alters the probability of apparent illness due to dengue virus infection: evidence from a pooled analysis across multiple cohort and cluster studies. PLoS Negl. Trop. Dis. 11, e0005926 (2017).
Stanaway, J. D. et al. The global burden of dengue: an analysis from the Global Burden of Disease Study 2013. Lancet Infect. Dis. 16, 712–723 (2016).
Huang, A. T. et al. Assessing the role of multiple mechanisms increasing the age of dengue cases in Thailand. Proc. Natl Acad. Sci. USA 119, e2115790119 (2022).
Limkittikul, K., Brett, J. & L’Azou, M. Epidemiological trends of dengue disease in Thailand (2000–2011): a systematic literature review. PLoS Negl. Trop. Dis. 8, e3241 (2014).
Chareonsook, O., Foy, H. M., Teeraratkul, A. & Silarug, N. Changing epidemiology of dengue hemorrhagic fever in Thailand. Epidemiol. Infect. 122, 161–166 (1999).
Rodríguez-Barraquer, I. et al. Revisiting Rayong: shifting seroprofiles of dengue in Thailand and their implications for transmission and control. Am. J. Epidemiol. 179, 353–360 (2014).
Yang, X., Quam, M. B. M., Zhang, T. & Sang, S. Global burden for dengue and the evolving pattern in the past 30 years. J. Travel Med. 28, taab146 (2021).
Endy, T. P. et al. Epidemiology of inapparent and symptomatic acute dengue virus infection: a prospective study of primary school children in Kamphaeng Phet, Thailand. Am. J. Epidemiol. 156, 40–51 (2002).
Kuan, G. et al. The Nicaraguan pediatric dengue cohort study: study design, methods, use of information technology, and extension to other infectious diseases. Am. J. Epidemiol. 170, 120–129 (2009).
Endy, T. P. et al. Determinants of inapparent and symptomatic dengue infection in a prospective study of primary school children in Kamphaeng Phet, Thailand. PLoS Negl. Trop. Dis. 5, e975 (2011).
Gordon, A. et al. The Nicaraguan pediatric dengue cohort study: incidence of inapparent and symptomatic dengue virus infections, 2004–2010. PLoS Negl. Trop. Dis. 7, e2462 (2013).
Ly, S. et al. Asymptomatic dengue virus infections, Cambodia, 2012–2013. Emerg. Infect. Dis. 25, 1354–1362 (2019).
Reyes, M. et al. Index cluster study of dengue virus infection in Nicaragua. Am. J. Trop. Med. Hyg. 83, 683–689 (2010).
Beckett, C. G. et al. Early detection of dengue infections using cluster sampling around index cases. Am. J. Trop. Med. Hyg. 72, 777–782 (2005).
Mammen, M. P. et al. Spatial and temporal clustering of dengue virus transmission in Thai villages. PLoS Med. 5, e205 (2008).
Yoon, I.-K. et al. Underrecognized mildly symptomatic viremic dengue virus infections in rural Thai schools and villages. J. Infect. Dis. 206, 389–398 (2012).
Asish, P. R., Dasgupta, S., Rachel, G., Bagepally, B. S. & Girish Kumar, C. P. Global prevalence of asymptomatic dengue infections—a systematic review and meta-analysis. Int. J. Infect. Dis. 134, 292–298 (2023).
Endy, T. P. et al. Spatial and temporal circulation of dengue virus serotypes: a prospective study of primary school children in Kamphaeng Phet, Thailand. Am. J. Epidemiol. 156, 52–59 (2002).
Sabin, A. B. Research on dengue during World War II. Am. J. Trop. Med. Hyg. 1, 30–50 (1952).
Salje, H. et al. Reconstruction of antibody dynamics and infection histories to evaluate dengue risk. Nature 557, 719–723 (2018).
Anderson, K. B. et al. An innovative, prospective, hybrid cohort–cluster study design to characterize dengue virus transmission in multigenerational households in Kamphaeng Phet, Thailand. Am. J. Epidemiol. 189, 648–659 (2020).
Moodie, Z. et al. Neutralizing antibody correlates analysis of tetravalent dengue vaccine efficacy trials in Asia and Latin America. J. Infect. Dis. 217, 742–753 (2018).
Katzelnick, L. C., Montoya, M., Gresh, L., Balmaseda, A. & Harris, E. Neutralizing antibody titers against dengue virus correlate with protection from symptomatic infection in a longitudinal cohort. Proc. Natl Acad. Sci. USA 113, 728–733 (2016).
Cummings, D. A. T. et al. The impact of the demographic transition on dengue in Thailand: insights from a statistical analysis and mathematical modeling. PLoS Med. https://doi.org/10.1371/journal.pmed.1000139 (2009).
Ribeiro Dos Santos, G. et al. Estimating the effect of the wMel release programme on the incidence of dengue and chikungunya in Rio de Janeiro, Brazil: a spatiotemporal modelling study. Lancet Infect. Dis. 22, 1587–1595 (2022).
Salje, H. et al. Evaluation of the extended efficacy of the Dengvaxia vaccine against symptomatic and subclinical dengue infection. Nat. Med. 27, 1395–1400 (2021).
Clarke, D. H. & Casals, J. Techniques for hemagglutination and hemagglutination–inhibition with arthropod-borne viruses. Am. J. Trop. Med. Hyg. 7, 561–573 (1958).
Innis, B. L. et al. An enzyme-linked immunosorbent assay to characterize dengue infections where dengue and Japanese encephalitis co-circulate. Am. J. Trop. Med. Hyg. 40, 418–427 (1989).
Lanciotti, R. S., Calisher, C. H., Gubler, D. J., Chang, G. J. & Vorndam, A. V. Rapid detection and typing of dengue viruses from clinical samples by using reverse transcriptase-polymerase chain reaction. J. Clin. Microbiol. https://doi.org/10.1128/jcm.30.3.545-551.1992 (1992).
Nisalak, A. Laboratory diagnosis of dengue virus infections. Southeast Asian J. Trop. Med. Public Health 46, 55–76 (2015).
Sirikajornpan, K. et al. Comparison of anti-DENV/JEV Ig-A enzyme-linked immunosorbent assay and hemagglutination inhibition assay. Southeast Asian J. Trop. Med. Public Health 49, 629–638 (2018).
Sirikajornpan, K. et al. Standardization and evaluation of an anti-ZIKV IgM ELISA assay for the serological diagnosis of zika virus infection. Am. J. Trop. Med. Hyg. 105, 936–941 (2021).
Chen, T. et al. xgboost: extreme gradient boosting (2022); https://CRAN.R-project.org/package=xgboost
Chen, T. & Guestrin, C. XGBoost. In Proc. 22nd ACM SIGKDD Int. Conf. on Knowledge Discovery and Data Mining (ed Krishnapuram, B.) 785–794 (ACM, 2016); https://doi.org/10.1145/2939672.2939785
R: a language and environment for statistical computing. R Core Team https://www.R-project.org/ (2022).
Brooks, M. et al. glmmTMB balances speed and flexibility among packages for zero-inflated generalized linear mixed modeling. R J. 9, 378–400 (2017).
O’Driscoll, M. et al. Maternally derived antibody titer dynamics and risk of hospitalized infant dengue disease. Proc. Natl Acad. Sci. USA 120, e2308221120 (2023).
Acknowledgements
We thank the data collection team as well as the children and adults involved in the study for all their efforts. We were supported in this work by the following: the National Institutes of Health (NIH) Grant 5P01AI034533-22: entire team; Military Infectious Disease Research Program (MIDRP): D.B., S.F., A.F. and K.B.A.; NIH 1R01AI175941-01: entire team; European Research Council 804744: H.S.; and NIH 1R35GM138361-01: M.H.-P. and I.R.-B. The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the paper.
Author information
Authors and Affiliations
Contributions
The study was conceived and designed by D.B., H.S., D.A.T.C., S.F., A.F., A.L.R., T.E., I.R.-B. and K.B.A. The data were collected by D.B., S.F., S.K., D.K., S.I. and A.S. The analysis and interpretation of results was performed by M.H.-P., H.S., D.A.T.C., A.F., S.J.T., A.W., A.L.R., T.E., I.R.-B. and K.B.A. The draft manuscript was prepared by M.H.-P., I.R.-B. and K.B.A. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Microbiology thanks Ashley St. John and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
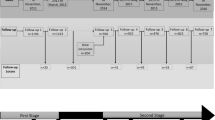
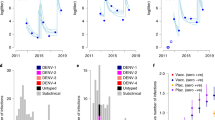
Extended Data Fig. 1 Cohort age distribution and various characteristics broken apart by sex.
(a) Age pyramid of enrolled subjects in five-year bins separated by sex (n = 3539). (b) Seroprevalence curve for subjects enrolled before 2017 in solid line, the analysis was conducted separately by sex. Points are mean seroprevalence in each fifth percentile for non-newborns under 30 years old (n = 6197). Confidence bounds are found using a basic nonparametric bootstrap. (c) Pre-interval DENV titers averaged across all four serotypes and their impact on probability of infection. (d) Relationship between pre-interval DENV titers averaged across all four serotypes and age. Both analyses included n = 11131 intervals with points and intervals representing the mean and 95% confidence interval. Shaded regions represent the 95% confidence intervals of fits.
Extended Data Fig. 2 Model training information and resulting probability of infection distribution.
(a) Confusion matrix for XGBoost model on training data. Reference values are found as outlined in the Methods section titled Training data while prediction values are found using the approach outlined in the Model fit section of the methods section. (b) Histogram of model predictions for probability of infection between sequential blood draws conducted on the full dataset.
Extended Data Fig. 3 Pre and post interval HAI titers by DENV serotype and JEV.
Pre and post interval HAI titers for all DENV serotypes and JEV grouped by age at post interval age and colored by whether the model predicted a DENV infection. Yellow and blue dots represent points that were or were not identified as infections respectively by the model while black and red points represent a similar dichotomy but in laboratory confirmed seroconversions. A four-fold increase in titers between samples is represented by the black diagonal line.
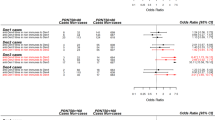
Extended Data Fig. 4 Sensitivity analysis on household related factors when utilizing the four-fold increase in DENV antibodies.
Sensitivity analysis on how household composition (a, b), infection history (c) and immunity (d) impact risk of infection when infections are defined to occur if there is a four-fold increase in antibody levels between paired serological samples (n = 11131). (a) Odds ratio for the number of total individuals in various age bins (newborn [NB], from 1–5 years old, from 5 to 18, and those 18 years or older [GE18]) defined at the time of the post-interval sample. (b) Odds ratio for the number of males and females of various age bins (newborn [NB], from 1–5 years old, from 5 to 18, and those 18 years or older [GE18]) defined at the time of the post-interval sample. (c) Previous interval’s attack rate (AR) and subsequent odds ratio of infection risk relative to having no infections in the previous interval. (d) Geometric mean of DENV HAI titers for the rest of the household and subsequent odds ratio of infection risk relative to having an average household HAI titer under 40. All models are adjusted for household random effects, individual pre-interval titers, as well as the year and month of post-interval sample. The vertical dashed line represents an aOR of 1 (no significant impact on risk).
Extended Data Fig. 5 Sensitivity analysis on household related factors in households with high sampling rates.
Sensitivity analysis on how household composition (a, b), infection history (c) and immunity (d) impact risk of infection in households where more than 80% of samples are recorded (n = 6435). (a) Odds ratio for the number of total individuals in various age bins (newborn [NB], from 1–5 years old, from 5 to 18, and those 18 years or older [GE18]) defined at the time of the post-interval sample. (b) Odds ratio for the number of males and females of various age bins (newborn [NB], from 1–5 years old, from 5 to 18, and those 18 years or older [GE18]) defined at the time of the post-interval sample. (c) Previous interval’s attack rate (AR) and subsequent odds ratio of infection risk relative to having no infections in the previous interval. (d) Geometric mean of DENV HAI titers for the rest of the household and subsequent odds ratio of infection risk relative to having an average household HAI titer under 40. All models are adjusted for household random effects, individual pre-interval titers, as well as the year and month of post-interval sample. The vertical dashed line represents an aOR of 1 (no significant impact on risk).
Extended Data Fig. 6 Sensitivity analysis on household related factors in seronaive individuals.
Sensitivity analysis on how household composition (a, b), infection history (c) and immunity (d) impact risk of infection in individuals who were seronaive at the start of an interval (n = 2066). (a) Odds ratio for the number of total individuals in various age bins (newborn [NB], from 1–5 years old, from 5 to 18, and those 18 years or older [GE18]) defined at the time of the post-interval sample. (b) Odds ratio for the number of males and females of various age bins (newborn [NB], from 1–5 years old, from 5 to 18, and those 18 years or older [GE18]) defined at the time of the post-interval sample. (c) Previous interval’s attack rate (AR) and subsequent odds ratio of infection risk relative to having no infections in the previous interval. (d) Geometric mean of DENV HAI titers for the rest of the household and subsequent odds ratio of infection risk relative to having an average household HAI titer under 40. All models are adjusted for household random effects, individual pre-interval titers, as well as the year and month of post-interval sample. The vertical dashed line represents an aOR of 1 (no significant impact on risk).
Supplementary information
Supplementary Information
Supplementary Figs. 1–6, Discussion and Tables 1–3.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hamins-Puértolas, M., Buddhari, D., Salje, H. et al. Household immunity and individual risk of infection with dengue virus in a prospective, longitudinal cohort study. Nat Microbiol 9, 274–283 (2024). https://doi.org/10.1038/s41564-023-01543-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41564-023-01543-3