Abstract
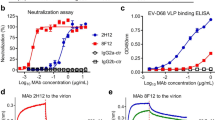
Japanese encephalitis virus (JEV), closely related to dengue, Zika, yellow fever and West Nile viruses, remains neglected and not well characterized1. JEV is the leading causative agent of encephalitis, and is responsible for thousands of deaths each year in Asia. Humoral immunity is essential for protecting against flavivirus infections and passive immunization has been demonstrated to be effective in curing disease2,3. Here, we demonstrate that JEV-specific monoclonal antibodies, 2F2 and 2H4, block attachment of the virus to its receptor and also prevent fusion of the virus. Neutralization of JEV by these antibodies is exceptionally potent and confers clear therapeutic benefit in mouse models. A single 20 μg dose of these antibodies resulted in 100% survival and complete clearance of JEV from the brains of mice. The 4.7 Å and 4.6 Å resolution cryo-electron microscopy structures of JEV–2F2-Fab and JEV–2H4-Fab complexes, together with the crystal structure of 2H4 Fab and our recent near-atomic structure of JEV4, unveil the nature and location of epitopes targeted by the antibodies. Both 2F2 and 2H4 Fabs bind quaternary epitopes that span across three adjacent envelope proteins. Our results provide a structural and molecular basis for the application of 2F2 and 2H4 to treat JEV infection.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Campbell, G. L. et al. Estimated global incidence of Japanese encephalitis: a systematic review. B. World Health Organ. 89, 766–774 (2011).
Diamond, M. S., Shrestha, B., Mehlhop, E., Sitati, E. & Engle, M. Innate and adaptive immune responses determine protection against disseminated infection by West Nile encephalitis virus. Viral Immunol. 16, 259–278 (2003).
Roehrig, J. T., Staudinger, L. A., Hunt, A. R., Mathews, J. H. & Blair, C. D. Antibody prophylaxis and therapy for flavivirus encephalitis infections. Ann. NY Acad. Sci. 951, 286–297 (2001).
Wang, X. et al. Near-atomic structure of Japanese encephalitis virus reveals critical determinants of virulence and stability. Nat. Commun. 8, 14 (2017).
Zhang, M. J., Wang, M. J., Jiang, S. Z. & Ma, W. Y. Passive protection of mice, goats, and monkeys against Japanese encephalitis with monoclonal antibodies. J. Med. Virol. 29, 133–138 (1989).
Zhang, X. et al. Dengue structure differs at the temperatures of its human and mosquito hosts. Proc. Natl Acad. Sci. USA 110, 6795–6799 (2013).
Scheres, S. H. & Chen, S. Prevention of overfitting in cryo-EM structure determination. Nat. Methods 9, 853–854 (2012).
Simhaev, L., McCarty, N. A., Ford, R. C. & Senderowitz, H. Molecular dynamics flexible fitting simulations identify new models of the closed state of the cystic fibrosis transmembrane conductance regulator protein. J. Chen. Inf. Model. 57, 1932–1946 (2017).
Afonine, P. V. et al. Towards automated crystallographic structure refinement with phenix. refine. Acta Crystallogr. D 68, 352–367 (2012).
Pierson, T. C. & Kielian, M. Flaviviruses: braking the entering. Curr. Opin. Virol. 3, 3–12 (2013).
Kuhn, R. J. et al. Structure of dengue virus: implications for flavivirus organization, maturation, and fusion. Cell 108, 717–725 (2002).
Modis, Y., Ogata, S., Clements, D. & Harrison, S. C. Structure of the dengue virus envelope protein after membrane fusion. Nature 427, 313–319 (2004).
Fibriansah, G. et al. A highly potent human antibody neutralizes dengue virus serotype 3 by binding across three surface proteins. Nat. Commun. 6, 6341 (2015).
Fibriansah, G. et al. Cryo-EM structure of an antibody that neutralizes dengue virus type 2 by locking E protein dimers. Science 349, 88–91 (2015).
Rouvinski, A. et al. Recognition determinants of broadly neutralizing human antibodies against dengue viruses. Nature 520, 109–113 (2015).
Teoh, E. P. et al. The structural basis for serotype-specific neutralization of dengue virus by a human antibody. Sci. Transl. Med. 4, 139ra183 (2012).
Smith, S. A. et al. The potent and broadly neutralizing human dengue virus-specific monoclonal antibody 1C19 reveals a unique cross-reactive epitope on the bc loop of domain II of the envelope protein. mBio 00873–00813 (2013).
Dai, L. et al. Structures of the Zika virus envelope protein and its complex with a flavivirus broadly protective antibody. Cell Host Microbe 19, 696–704 (2016).
Nybakken, G. E. et al. Structural basis of West Nile virus neutralization by a therapeutic antibody. Nature 437, 764–769 (2005).
Oliphant, T. et al. Development of a humanized monoclonal antibody with therapeutic potential against West Nile virus. Nat. Med. 11, 522–530 (2005).
Zhao, H. Y. et al. Structural basis of Zika virus-specific antibody protection. Cell 166, 1016–1027 (2016).
Barba-Spaeth, G. et al. Structural basis of potent Zika-dengue virus antibody cross-neutralization. Nature 536, 48–53 (2016).
Kaufmann, B. et al. Neutralization of West Nile virus by cross-linking of its surface proteins with Fab fragments of the human monoclonal antibody CR4354. Proc. Natl Acad. Sci. USA 107, 18950–18955 (2010).
Dang, M. et al. Molecular mechanism of SCARB2-mediated attachment and uncoating of EV71. Protein Cell 5, 692–703 (2014).
Orso, G. et al. Homotypic fusion of ER membranes requires the dynamin-like GTPase atlastin. Nature 460, 978–983 (2009).
Minor, W. & Otwinowski, Z. in Methods in Enzymology, Macromolecular Crystallography (ed. Carter, C. W. Jr) 307–326 (Academic Press, New York, 1997); https://doi.org/10.1016/S0076-6879(97)76066-X.
Wang, X. et al. Potent neutralization of hepatitis A virus reveals a receptor mimic mechanism and the receptor recognition site. Proc. Natl Acad. Sci. USA 114, 770–775 (2017).
McCoy, A. J. et al. Phaser crystallographic software. J. Appl. Crystallogr. 40, 658–674 (2007).
Emsley, P. & Cowtan, K. Coot: model-building tools for molecular graphics. Acta Crystallogr. D 60, 2126–2132 (2004).
Mastronarde, D. N. Automated electron microscope tomography using robust prediction of specimen movements. J. Struct. Biol. 152, 36–51 (2005).
Li, X. et al. Electron counting and beam-induced motion correction enable near-atomic-resolution single-particle cryo-EM. Nat. Methods 10, 584–590 (2013).
Ludtke, S. J., Baldwin, P. R. & Chiu, W. EMAN: semiautomated software for high-resolution single-particle reconstructions. J. Struct. Biol. 128, 82–97 (1999).
Zhang, K. Gctf: real-time CTF determination and correction. J. Struct. Biol. 193, 1–12 (2016).
Scheres, S. H. RELION: implementation of a Bayesian approach to cryo-EM structure determination. J. Struct. Biol. 180, 519–530 (2012).
Tang, G. et al. EMAN2: an extensible image processing suite for electron microscopy. J. Struct. Biol. 157, 38–46 (2007).
Pettersen, E. F. et al. UCSF Chimera—A visualization system for exploratory research and analysis. J. Comput. Chem. 25, 1605–1612 (2004).
Chen, V. B. et al. MolProbity: all-atom structure validation for macromolecular crystallography. Acta Crystallogr. D 66, 12–21 (2009).
Barad, B. A. et al. EMRinger: side chain-directed model and map validation for 3D cryo-electron microscopy. Nat. Methods 12, 943–946 (2015).
Livak, K. J. & Schmittgen, T. D. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT method. Methods 25, 402–408 (2001).
Xiao, C. & Rossmann, M. G. Interpretation of electron density with stereographic roadmap projections. J. Struct. Biol. 158, 182–187 (2007).
Acknowledgements
We thank Y. Chen, Z. Yang and B. Zhou for SPR technical support; X. Huang, B. Zhu and Z. Guo for cryo-EM technical support; and M.S. Diamond, S. Lok and D. Stuart for providing comments on the paper. The cryo-EM datasets were collected at the Center for Biological Imaging, Institute of Biophysics; the X-ray diffraction datasets were collected at beam line BL18U of the Shanghai Synchrotron Facility. Work was supported by the Ministry of Science and Technology 973 Project (grant no. 2014CB542800); the National Key Research and Development Program of China (no. 2016YFC1200400); the National Science Foundation, grant no. 81330036, no. 31570717, no. 81171557 and no.81520108019; the Strategic Priority Research Program of the Chinese Academy of Sciences, grant no. XDB08020200; and US NIH grants R01 AI1 12381 and R21 AI09464. X.W. is supported by the Young Elite Scientist sponsorship of CAST and program C of “One Hundred Talented People” of the Chinese Academy of Sciences.
Author information
Authors and Affiliations
Contributions
X.Q., Y.L., P.Y., N.W., Q.G. and X.Wa. performed the experiments; W.M., X.W., T.D. and F.Z. provided the reagents; X.Wa., Y.L., Z.X. and Z.R. designed the study; all authors analysed the data; and X.Wa., Y.L., Z.X., S.-L.L. and Z.R. wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figures 1–15, Supplementary Tables 1–5 and Supplementary References.
Rights and permissions
About this article
Cite this article
Qiu, X., Lei, Y., Yang, P. et al. Structural basis for neutralization of Japanese encephalitis virus by two potent therapeutic antibodies. Nat Microbiol 3, 287–294 (2018). https://doi.org/10.1038/s41564-017-0099-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41564-017-0099-x
This article is cited by
-
Antiviral drug research for Japanese encephalitis: an updated review
Pharmacological Reports (2022)
-
Structural and molecular basis for foot-and-mouth disease virus neutralization by two potent protective antibodies
Protein & Cell (2022)
-
A unified route for flavivirus structures uncovers essential pocket factors conserved across pathogenic viruses
Nature Communications (2021)
-
Rational development of a human antibody cocktail that deploys multiple functions to confer Pan-SARS-CoVs protection
Cell Research (2021)
-
Structures of Echovirus 30 in complex with its receptors inform a rational prediction for enterovirus receptor usage
Nature Communications (2020)