Abstract
Formal thought disorder (FTD) is a multidimensional syndrome mainly occurring along the psychosis continuum. Cannabis use is known to increase symptoms of psychosis, particularly positive symptoms. However, the impact of cannabis use on FTD in individuals presenting symptoms along the psychosis continuum remains unclear. To address this knowledge gap, we conducted a meta-analysis examining the association between cannabis use and FTD in those individuals. We hypothesized that cannabis would worsen FTD. We conducted a systematic search of the PubMed, ScienceDirect, PsycINFO, Web of Science, Embase and Google Scholar databases up to July 2022. The results were collated through a random-effects model using the statistical software R. Reference lists of included studies were searched for additional relevant publications. Nineteen studies were included, totalling 1840 cannabis users and 3351 non-cannabis users. The severity of FTD was found to be higher in cannabis users (SMD = 0.21, 95%CI [0.12–0.29], p = 0.00009). Subgroup analyses revealed that FTD severity was increased among cannabis users, regardless of the disorder severity: healthy individuals (SMD = 0.19, 95%CI [0.05–0.33], p = 0.02); patients with first-episode psychosis (SMD = 0.21, 95%CI [0.01–0.41], p = 0.04); patients with schizophrenia (SMD = 0.25, 95%CI [0.11–0.38], p = 0.005). Between-group differences were not significant. In line with its already known effect on positive symptoms in psychosis, cannabis use appears to be associated with increased FTD severity all along the psychosis continuum. Future research should consider potential confounding variables such as other substance use disorders and explore how FTD dimensions are impacted by cannabis use.
Similar content being viewed by others
Introduction
Formal thought disorder (FTD) refers to the disruption of the process of thoughts and language production, clinically resulting in an alteration of effective communication1,2 and is regarded as a multidimensional syndrome3. FTD prevalence and severity are proportionally higher in patients with psychotic disorders than in healthy populations2. 6% of people in the general population and up to 80% of patients with psychotic disorders exhibit more or less pronounced symptoms of FTD, suggesting that FTD is best conceptualized as a continuous dimension2. FTD is particularly frequent in schizophrenia, as it is found in 27–80% of patients1, but it may also occur in other types of disorders such as depression and mania1,4. FTD encompasses particularly disabling symptoms that increase social isolation5, reduce quality of life6 and are associated with poorer clinical outcomes7. This disorder is predictive of conversion to psychosis in high-risk populations8, and is the strongest predictor of conversion from first-episode psychosis to schizophrenia9.
Cannabis use is one of the most prominent risk factors associated with the occurrence and severity of many psychotic disorders, including schizophrenia. In patients with schizophrenia, lifetime cannabis use is estimated at 42.110 and 26.2% of patients with schizophrenia suffer from cannabis use disorder11. Cannabis use doubles the risk of developing a psychotic disorder in vulnerable individuals12, and triggers the onset of first-episode psychosis13 and psychotic disorders two to three years earlier than in non-users14. Among patients with schizophrenia, cannabis users present more severe positive symptoms, such as hallucinations and delusions15, whereas negative symptoms such as avolition and anhedonia seem less impacted by cannabis use16. FTD has a special place in the semiology of schizophrenia spectrum disorders, as it has been suggested to constitute a core (psychopathological) dimension of the disorder17. FTD dimensional structure is currently debated in the literature, leading to a high heterogeneity of assessment scales and conceptual definitions of this syndrome. At least two dimensions emerge as a consensus: negative FTD, referring to a deficit in speech and thought production; and positive FTD, referring to an increased amount of produced speech. Positive FTD is consistently associated with the disorganization dimension in several models of schizophrenia symptoms1,7,18. Previous research in individuals with schizotypal traits reported that the severity of disorganization was higher in cannabis users than in non-users19, suggesting that cannabis worsens positive FTD in a non-clinical sample.
The current review and meta-analysis firstly aimed to determine whether FTD and cannabis use are associated at different stages of the psychosis continuum, i.e. no or attenuated symptoms (stages 0, 1a, 1b), first-episode psychosis (stage 2), and recurrence and treatment resistance of the disorder (stages 3, 4)20. Subsequently, it aimed to investigate whether cannabis use would have a distinct impact on FTD depending on the stage of the psychotic disorder. We expected to find a positive association between cannabis use and FTD severity, all along the psychosis continuum.
Methods
The reporting of this meta-analysis was guided by the standards of the updated Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA)21. No pre-registration was performed for this meta-analysis.
Search strategy
PubMed, ScienceDirect, Web of Science, PsycINFO, Embase and Google Scholar were used as sources to retrieve publications. The search syntax was as follows: [“thought disorder” OR “thought disturbance” OR “cognitive disorganization” OR “formal thought disorder” OR “disorganized speech” AND “cannabis” OR “marijuana” OR “THC” OR “pot” OR “hashish” OR “bhang” OR “ganja”] (see supplementary materials “SearchSyntax” for details). A filter was applied on ScienceDirect to only retrieve “research articles”. In addition, only the first 200 relevant sources were retrieved from Google Scholar, as recommended22. Each database supports spelling variations, such as the terms “disorganization” and “disorganized” were automatically searched with British and American spelling. Each source was last searched in July 2022. Reference lists of the selected publications were reviewed to identify additional relevant studies.
Duplicates were removed by manual screening. After duplicate removal, each record was first screened on title and abstract by two independent researchers (MA and GS). In case of disagreement, the inclusion of the study was decided by a third researcher (BR). A second selection round was based on full text reading and followed the same procedure. The flow-chart detailing the selection process is provided in Fig. 1.
Eligibility criteria
To be included, each study had to meet the following criteria: (1) report FTD scores of two distinct groups: one of cannabis users and a control one of non-users; (2) include individuals presenting symptoms pertaining to the psychosis continuum; (3) use validated tools for assessing FTD; and (4) be written in English. Studies were excluded if: (1) FTD was not specifically distinguished from other psychotic symptoms, (2) cannabis use was not assessed, or not distinguished from the use of other substances, (3) the link between FTD and cannabis use was not reported in the analyses.
Data extraction
Data used for statistical analyses were extracted from the Results section or the supplementary material part of selected studies. To allow for a comparison between groups, data had to be extracted into two groups: one group of participants using cannabis and one of participants not using cannabis. In addition, both extracted groups of participants had to present symptoms pertaining to the same stage of the psychosis continuum (i.e. patients with schizophrenia and not using cannabis compared to patients with schizophrenia using cannabis). In cases where study designs included participants pertaining to multiple groups in terms of their drug use (i.e. polysubstance users, cannabis mainly users, alcohol mainly users, non-users), only the relevant groups were extracted (i.e. cannabis mainly users and non-users). Similarly, in the event that multiple groups of participants were formed in terms of the disorder severity (i.e. first-episode psychosis compared to healthy controls), only data of the relevant group was extracted (i.e. first-episode psychosis using and not using cannabis).
In cases where insufficient data was present for the calculation of our primary effect size, the principal investigators were contacted via email13,23,24,25. Two of the contacted authors provided the requested data13,23.
Quality assessment
The risk of bias was assessed by two independent researchers (MA and MR) using the Quality Assessment Tool for Observational Cohort and Cross-sectional studies26, a recommended tool for analytical cross-sectional studies27. This process ensures that the quality of included studies is good enough to provide reliable results. Based on a series of questions, the goal is to identify potential flaws in the publication that may impact the outcome measure we want to study. Quality of studies can be rated as “poor”, “fair”, or “good”. Question 9 “Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants?” and question 11 “Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants?” were judged crucial as the focus for the current meta-analysis is the relationship between FTD (outcome) and cannabis use (exposure). Question 14 “Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)?” was considered important as the presence of confounding variables can distort the relationship between FTD and cannabis use. In cases where studies collected a “no” to questions 9 and 11, the quality was not rated as “good”.
Meta-analysis methods
Analyses were conducted using the statistical software R version 4.1.1 (R Core Team 2021)28. Mean scores, standard deviations and binary outcomes (FTD present or absent) of each study were extracted for cannabis users and for non-users; they were subsequently converted into between-groups Standardized Mean Differences (SMD) using the {esc} package, so that the results obtained from different scales could be pooled together. In cases where studies reported the result of a two-sample t-test29, the t-statistic was converted into a SMD. Hedge’s g correction was applied to all SMDs to correct for small-sample size. In cases where studies categorized groups into types of cannabis used (i.e. skunk, herbal, mixed)30, or level of use (i.e. use, harmful use, Substance Use Disorder)13, we regrouped these cannabis users into a single group for each study by calculating their mean scores and standard deviations. SMDs were calculated comparing the statistics of the cannabis-using groups with those of the non-using groups. In cases where SMD values are positive, cannabis-using groups present higher FTD mean scores than non-using groups. When SMD values are negative, cannabis-using groups present lower FTD mean scores than non-using groups. The overall calculated effect size was then transformed back into natural units of two widely used scales (Positive and Negative Symptoms Scale and Scale for the Assessment of Positive Symptoms) to facilitate interpretation of the results. This transformation is based on a recognized statistical method31,32,33; it was obtained by multiplying the calculated SMD by the pooled standard deviation of selected scales31,34. The interpretation values for effect size (SMD) according to Cohen’s classification are: 0.1–0.3 (small effect), 0.3–0.5 (moderate effect) and superior to 0.5 (large effect).
The meta-analysis was performed using the {meta} package. Group combination, plot generation and outlier identification were performed using the {dmetar} package. Between-study heterogeneity was computed via a random effect model with I², where I² = 25%, I² = 50%, and I² = 75% are considered as low, moderate, and high heterogeneity, respectively35. Tau² was estimated using the Restricted Maximum Likelihood. In addition, Hartung-Knapp adjustment36 was applied to the 95% confidence interval of the pooled effect size to reduce the chances of false positives. The prediction interval was calculated to estimate the reliability of the results in the context of future studies. The search for outliers was performed to address between-study heterogeneity, using the “find.outliers” function included in the {dmetar} package. A sensitivity analysis was conducted to exclude cases that would influence too greatly the results, due to a large sample size. This method allows to visualize if the calculated SMD was distorted by one large study influencing the true effect size. This supplementary analysis ensures that the synthetized results were not distorted and thus robust. In cases where the influence analysis detected studies affecting too greatly the results, the statistical leave-one-out method was applied to confirm those cases. This method estimates the overall effect size omitting one study at a time. In addition, we performed post hoc subgroup analyses to investigate the effect of cannabis use on the different populations included across publications (i.e. no or attenuated symptoms, first-episode psychosis, schizophrenia). Publication bias was visually inspected with a funnel plot and quantified with an Egger’s test measuring the asymmetry of the funnel plot.
Results
The flow diagram of the study selection process is provided in Fig. 1. Searches yielded 1822 results, which were then refined by the screening of titles and abstracts. After the screening process, 201 publications were assessed for eligibility based on a full-text reading, leading to the selection of 21 relevant studies. Details regarding the reasons for study exclusion are provided in Fig. 1. We finally included 19 publications in the meta-analysis because data extraction could not be performed for two studies24,25.
Across the 19 studies, a total of 5191 participants were included: 1840 in the cannabis-users group and 3351 in the non-users group.
Effect measures
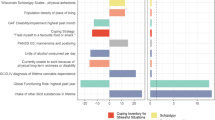
In the various studies, FTD was referred to as “cognitive disorganization”30,37,38,39, “disorganization“23,40,41,42,43,44,45, “thought disturbance”29, “FTD”46,47 or “positive FTD”13,48,49,50,51. This is linked to the scale used (see supplementary material “Scales” for details). Each of these terms refers to a similar concept of FTD, encompassing speech abnormalities, poor attention, conceptual disorganization, and difficulties in thought process. For clarity, the umbrella term “FTD” will be used to refer to all these terms throughout this meta-analysis. Eight studies23,30,37,38,39,42,44,45 assessed FTD globally using two questionnaires, the Oxford-Liverpool Inventory of Feelings and Experiences52 and the Schizotypal Personality Questionnaire53, as well as three scales: the Positive and Negative Syndrome Scale54, the Psychotomimetic States Inventory52, and the Structured Interview for Prodromal Symptoms45. Nine studies13,29,40,41,46,48,49,50,51 evaluated subcomponents of FTD using the Scale for the Assessment of Positive Symptoms55, the Brief Psychiatric Rating Scale56, the Young Mania Rating Scale57, the Operational Criteria for Psychotic Illness58 and the Symptom Onset in Schizophrenia59. The main subcomponent assessed via these scales was positive FTD, characterized by disorganized speech. One study reported results for both negative and positive FTD48. Since the other studies focused on either the global concept of FTD13,29,30,37,47, which includes positive FTD, or only positive FTD23,46,50,51, this dimension was the only one considered in order to maintain homogeneity between compared outcomes. Some studies also reported results as a proportion of participants in whom FTD was either present or absent40,47,48,51.
Study characteristics
The eligible studies included different types of population: (1) individuals with no history of diagnosed mental illness23,30,38,39,42,43,44,45; (2) individuals with a history of first-episode psychosis13,37,40,46; (3) individuals with schizophrenia29,41,48,49,50,51, according to validated diagnosis tools; and (4) individuals with cannabis-induced psychosis47, as determined by an expert. For the purpose of this meta-analysis, it was decided to form four distinct groups of individuals, according to the staging model of psychotic disorders20: (1) individuals without symptoms, or attenuated syndrome (stages 0, 1a, 1b); (2) individuals with first-episode psychosis (stage 2); (3) individuals with schizophrenia (stages 3–4); and (4) individuals with cannabis-induced psychosis (Table 1).
Risk of bias
The overall risk of bias was considered as low: the quality of four studies was rated as “good”29,37,44,51, that of fourteen studies as “fair”13,23,30,38,40,41,42,43,45,46,48,49,50,52 and that of one as “poor”47. Poor quality was firstly determined by the imprecise criteria for pertaining to the cannabis using group, i.e. “regular cannabis use for at least 1 month prior to onset of psychosis”, and by the imprecise measure of FTD in participants, i.e. “no psychopathology scale could be used”47. Most studies were rated as “fair” quality as either question 9 or question 11 of the Quality Assessment Tool for Observational Cohort and Cross-sectional studies rated as “yes” for these publications. Good quality was decided when the questions 9, 11, and 14 rated as “yes”, as well as the other questions of the tool. The detailed ratings can be found in the supplementary material.
Cannabis Use and FTD
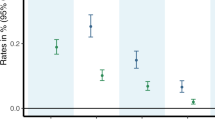
The overall effect size of the 19 pooled studies indicated that FTD severity was significantly increased in cannabis-users groups, compared to non-using groups (SMD = 0.21, p = 0.00009, 95% CI [0.12; 0.29]). Between-group heterogeneity was moderate (I² = 34%, p = 0.08). The estimated range of the prediction interval indicates that the effect size may lie between 0.07 and 0.34 in the context of future studies on the same issue. Original results are presented in Fig. 2.
Sensitivity analyses
The study rated as being of “poor” quality was reported as an outlier47. While its inclusion in the original analysis had a negligible impact on the overall results, it greatly affected heterogeneity (Table 2. “Main” analysis for statistical details). Considering its outlier status and its large impact on heterogeneity, it was excluded from the other analyses performed. Thus, the overall effect size of the 18 remaining studies was kept throughout the current meta-analysis (SMD = 0.22, p = 0.000006, 95% CI [0.14; 0.53]), with a low between-study heterogeneity (I² = 4.8%, p = 0.4). Prediction interval based on the 18 remaining studies confirmed that the effect size may lie within a range of positive values (PI [0.10; 0.33]). A second sensitivity analysis was performed, excluding two studies considered as having a large influence on the results by the statistical leave-one-out method30,42 (see supplementary material “InfluenceAnalysis”). The removal of these two studies did not significantly impact the overall effect size, which means that their influence did not distort the calculated effect size in the first analysis (SMD = 0.22, p < 0.0001, 95% CI [0.15; 0.29], I² < 1%, p = 0.59). Table 2 provides a detailed explanation of the statistical results of the two distinct sensitivity analyses performed.
When the SMD was back transformed using the pooled standard deviation of the PANSS, the mean difference in Cognitive Disorganization score between cannabis-using and non-using groups equals to 0.57 points; Cognitive Disorganization scores ranged from 3 to 21 points. Applied to the SAPS, the mean difference in positive FTD score between cannabis-using and non-using groups equals to 0.93 points; positive FTD ranged from 0 to 45 points.
Subgroup analyses
Subgroup analyses were performed to examine the effect of cannabis use on the groups formed in line with the staging model of psychotic disorders previously mentioned: (1) individuals with no or attenuated symptoms, (2) patients with first-episode psychosis, and (3) patients diagnosed with schizophrenia. The cannabis-induced psychosis group was not represented as the only study focusing on this population was the outlier and thus excluded. Individuals with no or attenuated symptoms were extracted from the general population and are thus considered a prodromal population. First-episode psychosis patients were described in the publications as having experienced psychotic symptoms accompanied by a decrease in functioning over the month before inclusion37, being diagnosed with a primary non-affective psychotic disorder46, having a history of psychotic symptoms that lasted for more than 7 days13, experiencing the first episode of schizophrenia, excluding brief psychotic episodes due to intoxication48, or experiencing a first occurrence of positive and negative, cognitive and affective symptoms40. Individuals using cannabis in the first group (no or attenuated symptoms) demonstrated significantly higher FTD scores compared to non-users (SMD = 0.19, 95% CI [0.05;0.33], p = 0.02). Cannabis users in the second group (first-episode psychosis) also had a higher FTD severity than non-users, the 2 groups showed a comparable effect size (SMD = 0.21, 95% CI [0.01;0.41], p = 0.04). Although tests revealed that the differences in effect size were not significant between groups (p = 0.75), cannabis users with a diagnosis of schizophrenia displayed higher FTD severity compared with non-users, with the highest effect size (SMD = 0.25, 95% CI [0.11;0.38], p = 0.005).
Publication bias
Studies reporting low effect sizes may remain unpublished because of non-significant results. Only studies reporting significant results tend to be published, creating a publication bias. This bias can be visually and statistically assessed via the inspection of a funnel plot and the statistical Egger’s test. The visual inspection of the funnel plot indicates a relatively low asymmetry. However, one study appears far away from the ideal delineated area (see Fig. 3). It is the same study that was found to be an outlier and excluded from the analysis47. Egger’s test was performed on the nineteen studies to statistically assess the publication bias (supplementary material “EggerTest”). The Egger’s test did not reveal significant presence of asymmetry, indicating no evidence for a publication bias.
Discussion
This meta-analysis aimed to review the relationship between cannabis use and FTD along a continuum ranging from individuals with no history of characterized mental disorders to patients meeting the criteria for schizophrenia, what had never been performed to our knowledge. The main results of the global analysis showed that individuals using cannabis presented a significantly higher severity of FTD than non-users. Although the effect was significant, the size of the effect (SMD = 0.20) should be considered as small60. Subgroup analyses were then performed to investigate whether the relationship between cannabis use and FTD varied between individuals of the included populations: no or attenuated symptoms, first-episode psychosis, and schizophrenia. Cannabis users from all three subgroups exhibited a similar FTD severity, suggesting a stable association independent of the underlying stage of the psychotic disorder. Thus, the association between FTD and cannabis use should not be seen as an intermediate vulnerability marker for schizophrenia. However, since both cannabis use and FTD severity were associated with increased risk for psychosis, we cannot rule out a role of the relationship between FTD and cannabis use in the psychotic transition. Indeed, triggering factors of psychotic symptoms are complex and combine both biological features such as genetic traits, and environmental factors such as socio-economic or migration status61. The results support the hypothesis that cannabis use could be seen as one of the key factors explaining the severity of FTD.
The results are in line with previous findings where disorganization symptoms were exacerbated by cannabis use in individuals with schizotypal traits19. In addition, some studies described an aggravation of disorganization when individuals at a prodromal stage of psychosis present an acute cannabis intoxication62,63. Findings from a ten-year longitudinal experiment, which investigated the impact of cannabis use on the course of illness in schizophrenia, reported that compared to non-users, cannabis users presented higher scores of disorganized symptoms at the 6-month, 4-year and 10-year follow-ups64, implying an aggravation of FTD by cannabis use, in line with the findings presented in the current review. In the same study, however, a decrease in disorganized symptoms for some individuals was associated with a higher likelihood of cannabis use64. This could mean that some individuals use cannabis to alleviate their disorganized symptoms64, demonstrating the need to distinguish between subjective and objective FTD3,65.
This meta-analysis has some strengths. Publication bias, as well as the risk of bias in each individual study, and small-sample study biases, were taken into account in our meta-analysis. Between-study heterogeneity is considered as very low, due to the use of a random model and the outlier identification. All the relevant methods that avoid bias were employed to provide the most reliable results. However, there are several factors that could not be controlled for as this meta-analysis used aggregated data. Because the included studies were epidemiological investigations, it is impossible to ascertain a causal effect of cannabis use on the severity of FTD; intermediary factors such as sociodemographic features, the use of cannabis for self-medication, the effect of antipsychotic treatment, or the presence of Substance Use Disorder (SUD) cannot be ruled out. SUDs involving cocaine, alcohol, stimulants, hallucinogens, or tobacco are associated with FTD severity13,66,67. Another identified limitation is that, even if the search syntax used in the current meta-analysis intended to include all publications on FTD and its subcomponents, FTD is actually a heterogeneous construct which can be expressed using many terms, and whose exact conceptual structure is still being explored using factor analyses of clinical scales7. Furthermore, there is a paucity of publications exploring the association between cannabis use and specific FTD subcomponents. Hence, FTD subcomponents other than the positive dimension could not be adequately represented in the current study. Previous works found a significant positive association between cannabis use and negative FTD48. This finding should be replicated, as it could broaden knowledge on this issue. In addition, subcomponents of FTD need to be more systematically explored in future research via the use of scales specifically designed to measure FTD severity such as the Thought And Language Disorder (TALD), the Thought Language and Communication Disorders (TLC), the Thought and Language Index (TLI), and the Thought Disorder Index (TDI)1. Finally, a last limitation of the current meta-analysis is to not have been preregistered in a public registry.
Conclusion
Previous studies found that cannabis use was associated with more severe positive symptoms of psychosis, within an epidemiological continuum ranging from the general population to schizophrenia spectrum disorders. Moreover, accumulating pieces of evidence suggest a causal role of cannabis in triggering and aggravating positive symptoms, particularly in schizophrenia spectrum disorders. Since FTD has been suggested to constitute a core symptom of schizophrenia, it was theoretically expected that cannabis use would be associated with exacerbated FTD. The results presented in this meta-analysis tend to support this association, and the effect of cannabis use on FTD seems consistent along the psychosis continuum, regardless of the severity of the psychotic disorder. Intermediary factors need to be controlled for in future research on this issue. These findings encourage future research to assess FTD using specific scales and support the clinical relevance of assessing FTD in early stages of the psychosis continuum, specifically among individuals using cannabis.
Data availability
The data supporting the findings of this study are available within the paper and its supplementary information files.
Code availability
The code written for the analyses will be available upon request.
References
Kircher, T., Bröhl, H., Meier, F. & Engelen, J. Formal thought disorders: From phenomenology to neurobiology. Lancet Psychiatry 5, 515–526 (2018).
Roche, E., Creed, L., MacMahon, D., Brennan, D. & Clarke, M. The epidemiology and associated phenomenology of formal thought disorder: A systematic review: Fig. 1. SCHBUL 41, 951–962 (2015).
Mutlu, E. et al. The cognitive aspect of formal thought disorder and its relationship with global social functioning and the quality of life in schizophrenia. Soc. Psychiatry Psychiatr. Epidemiol. 56, 1399–1410 (2021).
Cavelti, M., Kircher, T., Nagels, A., Strik, W. & Homan, P. Is formal thought disorder in schizophrenia related to structural and functional aberrations in the language network? A systematic review of neuroimaging findings. Schizophr. Res. 199, 2–16 (2018).
de Sousa, P., Spray, A., Sellwood, W. & Bentall, R. P. ‘No man is an island’. Testing the specific role of social isolation in formal thought disorder. Psychiatry Res. 230, 304–313 (2015).
Tan, E. J. & Rossell, S. L. Building a neurocognitive profile of thought disorder in schizophrenia using a standardized test battery. Schizophr. Res. 152, 242–245 (2014).
Ucok, A., Karakaş, B. & Şahin, O. Ş. Formal thought disorder in patients with first-episode schizophrenia: Results of a one-year follow-up study. Psychiatry Res. 301, 113972 (2021).
Demjaha, A. et al. Combining dimensional and categorical representation of psychosis: The way forward for DSM-V and ICD-11? Psychol. Med. 39, 1943–1955 (2009).
Ayer, A. et al. Formal thought disorder in first-episode psychosis. Comprehensive Psychiatry 70, 209–215 (2016).
Green, B., Young, R. & Kavanagh, D. Cannabis use and misuse prevalence among people with psychosis. Br. J. Psychiatry 187, 306–313 (2005).
Hunt, G. E., Large, M. M., Cleary, M., Lai, H. M. X. & Saunders, J. B. Prevalence of comorbid substance use in schizophrenia spectrum disorders in community and clinical settings, 1990–2017: Systematic review and meta-analysis. Drug Alcohol Dependence 191, 234–258 (2018).
Ortiz-Medina, M. B. et al. Cannabis consumption and psychosis or schizophrenia development. Int. J. Soc. Psychiatry 64, 690–704 (2018).
Stone, J. M. et al. Cannabis use and first-episode psychosis: Relationship with manic and psychotic symptoms, and with age at presentation. Psychol. Med. 44, 499–506 (2014).
Hasan, A. et al. Cannabis use and psychosis: A review of reviews. Eur. Arch. Psychiatry Clin. Neurosci. 270, 403–412 (2020).
Schoeler, T. et al. Continued versus discontinued cannabis use in patients with psychosis: A systematic review and meta-analysis. Lancet Psychiatry 3, 215–225 (2016).
Sabe, M., Zhao, N. & Kaiser, S. Cannabis, nicotine and the negative symptoms of schizophrenia: Systematic review and meta-analysis of observational studies. Neurosci. Biobehav. Rev. 116, 415–425 (2020).
Bleuler, M. [Origin and significance of Eugen Bleuler’s work: “Dementia praecox or the schizophrenia group”. A contribution to the history of Manfred Bleuler’s Zuricher psychiatry]. Schweiz Rundsch Med. Prax 77, 1322–1326 (1988).
Minor, K. S., Marggraf, M. P., Davis, B. J., Mehdiyoun, N. F. & Breier, A. Affective systems induce formal thought disorder in early-stage psychosis. J. Abnormal Psychol. 125, 537–542 (2016).
Szoke, A. et al. Association between cannabis use and schizotypal dimensions-a meta-analysis of cross-sectional studies. Psychiatry Res. 219, 58–66 (2014).
McGorry, P. D., Hartmann, J. A., Spooner, R. & Nelson, B. Beyond the “at risk mental state” concept: transitioning to transdiagnostic psychiatry. World Psychiatry 17, 133–142 (2018).
Page, M. J. et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 372, n71 (2021).
Bramer, W. M., Rethlefsen, M. L., Kleijnen, J. & Franco, O. H. Optimal database combinations for literature searches in systematic reviews: A prospective exploratory study. Syst. Rev. 6, 245 (2017).
Cohen, A. S., Buckner, J. D., Najolia, G. M. & Stewart, D. W. Cannabis and psychometrically-defined schizotypy: Use, problems and treatment considerations. J. Psychiatric Res. 45, 548–554 (2011).
Kiang, M. et al. Association of abnormal semantic processing with delusion-like ideation in frequent cannabis users: An electrophysiological study. Psychopharmacology 225, 95–104 (2013).
Shakoor, S. et al. Psychotic experiences are linked to cannabis use in adolescents in the community because of common underlying environmental risk factors. Psychiatry Res. 227, 144–151 (2015).
National Institution of Health: U.S Department of Health and Human Services. Quality assessment tool for observational cohort and cross-sectional studies. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (2015).
Ma, L. L. et al. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: What are they and which is better? Military Med. Res. 7, 7 (2020).
R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing. https://www.R-project.org/ (2021).
Caspari, D. Cannabis and schizophrenia: Results of a follow-up study. European Archives Psychiatry Clin. Neurosci. 249, 45–49 (1999).
Mackie, C. J. et al. A latent class analysis of cannabis use products in a general population sample of adolescents and their association with paranoia, hallucinations, cognitive disorganisation and grandiosity. Addictive Behav. 117, 106837 (2021).
Schünemann, H. J. et al. Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (eds. Higgins, J., Thomas, J. & Chandler, J. et al.) (Wiley, 2021).
Devji, T. et al. Presentation approaches for enhancing interpretability of patient-reported outcomes (PROs) in meta-analysis: A protocol for a systematic survey of Cochrane reviews. BMJ Open 7, e017138 (2017).
Murad, M. H., Wang, Z., Chu, H. & Lin, L. When continuous outcomes are measured using different scales: Guide for meta-analysis and interpretation. BMJ 364, k4817 (2019).
Thorlund, K., Walter, S. D., Johnston, B. C., Furukawa, T. A. & Guyatt, G. H. Pooling health-related quality of life outcomes in meta-analysis-a tutorial and review of methods for enhancing interpretability: Enhancing interpretability in continuous meta-analysis. Res. Syn. Meth. 2, 188–203 (2011).
Higgins, J. P. T. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558 (2002).
Jackson, D., Law, M., Rücker, G. & Schwarzer, G. The Hartung–Knapp modification for random‐effects meta‐analysis: A useful refinement but are there any residual concerns. Stat. Med. 36, 3923–3934 (2017).
Herzig, D. A. et al. Hemispheric language asymmetry in first episode psychosis and schizotypy: The role of cannabis consumption and cognitive disorganization. Schizophr. Bull. 41, S455–S464 (2015).
Nunn, J. A., Rizza, F. & Peters, E. R. The incidence of schizotypy among cannabis and alcohol users. J. Nervous Mental Dis. 189, 741–748 (2001).
Mason, O. J., Morgan, C. J. M., Stefanovic, A. & Curran, H. V. The Psychotomimetic States Inventory (PSI): Measuring psychotic-type experiences from ketamine and cannabis. Schizophr. Res. 103, 138–142 (2008).
González-Blanco, L. et al. Impact of previous tobacco use with or without cannabis on first psychotic experiences in patients with first-episode psychosis. Schizophr. Res. 236, 19–28 (2021).
Ho, B. C., Wassink, T. H., Ziebell, S. & Andreasen, N. C. Cannabinoid receptor 1 gene polymorphisms and marijuana misuse interactions on white matter and cognitive deficits in schizophrenia. Schizophr. Res. 128, 66–75 (2011).
O’Tuathaigh, C. M. P. et al. Does cannabis use predict psychometric schizotypy via aberrant salience? Schizophr. Res. 220, 194–200 (2020).
Schiffman, J., Nakamura, B., Earleywine, M. & LaBrie, J. Symptoms of schizotypy precede cannabis use. Psychiatry Res. 134, 37–42 (2005).
Soler, J. et al. The interaction between the ZNF804A gene and cannabis use on the risk of psychosis in a non-clinical sample. Prog. Neuropsychopharmacol. Biol. Psychiatry 89, 174–180 (2019).
Korver, N. et al. Symptomatology and neuropsychological functioning in cannabis using subjects at ultra-high risk for developing psychosis and healthy controls. Aust. N. Z. J. Psychiatry 44, 230–236 (2010).
Pope, L. G., Manseau, M. W., Kelley, M. E. & Compton, M. T. Symptomatology and neurocognition among first-episode psychosis patients with and without cannabis use in the three months prior to first hospitalization. Schizophr. Res. 228, 83–88 (2021).
Basu, D., Malhotra, A., Bhagat, A. & Varma, V. K. Cannabis psychosis and acute schizophrenia—A case-control study from India. Eur. Addict. Res. 5, 71–73 (1999).
Boydell, J. et al. A comparison of symptoms and family history in schizophrenia with and without prior cannabis use: Implications for the concept of cannabis psychosis. Schizophr. Res. 93, 203–210 (2007).
Koen, L., Jonathan, R. & Niehaus, D. J. Cannabis use and abuse correlates in a homogenous South African schizophrenia population. S. Afr. J. Psych. 15, 5 (2009).
Peralta, V. & Cuesta, M. J. Influence of cannabis abuse on schizophrenic psychopathology. Acta Psychiatr. Scand. 85, 127–130 (1992).
Dubertret, C., Bidard, I., Adès, J. & Gorwood, P. Lifetime positive symptoms in patients with schizophrenia and cannabis abuse are partially explained by co-morbid addiction. Schizophr. Res. 86, 284–290 (2006).
Mason, O., Claridge, G. & Jackson, M. New scales for the assessment of schizotypy. Personality Individual Differences 18, 7–13 (1995).
Raine, A. & Benishay, D. The SPQ-B: A brief screening instrument for schizotypal personality disorder. J. Personality Dis. 9, 346–355 (1995).
Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 13, 261–276 (1987).
Andreasen, N. C. Scale for the assessment of positive symptoms. https://doi.org/10.1037/t48377-000 (2018).
Mueser, K. T., Curran, P. J. & McHugo, G. J. Factor structure of the Brief Psychiatric Rating Scale in schizophrenia. Psychol. Assess. 9, 196–204 (1997).
Young, R. C., Biggs, J. T., Ziegler, V. E. & Meyer, D. A. A rating scale for mania: Reliability, validity, and sensitivity. Br. J. Psychiatry 133, 429–435 (1978).
Bergman, H. et al. Operational Criteria Checklist for Psychotic Illness and Affective Illness (OPCRIT+) for diagnosing schizophrenia in people with psychotic symptoms. Cochrane Schizophrenia Group, ed. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD011104 (2014).
Perkins, D. O. et al. Characterizing and dating the onset of symptoms in psychotic illness: The Symptom Onset in Schizophrenia (SOS) inventory. Schizophr. Res. 44, 1–10 (2000).
Cohen J. Statistical Power Analysis for the Behavioral Sciences. Rev. ed. New York: Academic Press; 1977.
Owen, M. J., Sawa, A. & Mortensen, P. B. Schizophrenia. Lancet 388, 86–97 (2016).
Mason, O. et al. Acute cannabis use causes increased psychotomimetic experiences in individuals prone to psychosis. Psychol. Med. 39, 951–956 (2009).
Mokrysz, C., Freeman, T. P., Korkki, S., Griffiths, K. & Curran, H. V. Are adolescents more vulnerable to the harmful effects of cannabis than adults? A placebo-controlled study in human males. Translational Psychiatry 6, e961–e961 (2016).
Foti, D. J., Kotov, R., Guey, L. T. & Bromet, E. J. Cannabis use and the course of schizophrenia: 10-year follow-up after first hospitalization. AJP 167, 987–993 (2010).
Sumner, P. J., Rossell, S. L. & Tan, E. J. On the assessment of subjective formal thought disorder. Schizophr. Res. 228, 58–59 (2021).
Mauri, M. et al. Substance abuse in first-episode schizophrenic patients: A retrospective study. Clin. Pract. Epidemiol. Ment. Health 2, 4 (2006).
Nagels, A. et al. Distinct neuropsychological correlates in positive and negative formal thought disorder syndromes: The thought and language disorder scale in endogenous psychoses. Neuropsychobiology 73, 139–147 (2016).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Argote, M., Sescousse, G., Brunelin, J. et al. Association between formal thought disorder and cannabis use: a systematic review and meta-analysis. Schizophr 8, 78 (2022). https://doi.org/10.1038/s41537-022-00286-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41537-022-00286-0
This article is cited by
-
Psychotic features, particularly mood incongruence, as a hallmark of severity of bipolar I disorder
International Journal of Bipolar Disorders (2022)