Abstract
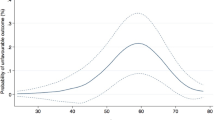
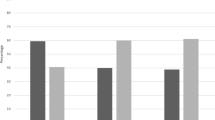
Penile prosthesis implantation (PP surgery) is a well-established solution for severe, medication-refractory erectile dysfunction (ED). Despite its effectiveness, limited data exists on patient characteristics influencing the timing of PP surgery after ED onset. We aimed to investigate predictors for early PP surgery and compare preoperative factors in men who had early (<12 months) vs. late PP surgery (≥12 months). We analyzed data from 210 men undergoing inflatable PP surgery for medication-refractory ED to investigate predictors for early PP surgery. Men with early PP surgery were older (64 vs. 61 years), had more comorbidities, (97.2% vs. 63.3% CCI ≥ 1). Linear regression analysis showed that more comorbidities were associated with an earlier time to PP surgery (Coeff: −1.82, 95% CI: −3.08 to −0.56, p = 0.004). At multivariate Cox regression analysis, CCI ≥ 1 emerged as the sole predictor of early PP surgery (OR: 1.29, 95% CI: 1.07–1.56, p = 0.007) after adjusting for age, ED etiology, and ethnicity. Our study sheds light on factors influencing decisions for early vs. late PP surgery post-medication-refractory ED. Men with more comorbidities were more likely to receive early PP surgery, emphasizing the importance of preoperative counseling and personalized treatment plans.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
NIH Consensus Conference. Impotence. NIH Consensus Development Panel on Impotence. JAMA. 1993;270:83–90.
Bajic P, Mahon J, Faraday M, Sadeghi-Nejad H, Hakim L, McVary KT. Etiology of erectile dysfunction and duration of symptoms in patients undergoing penile prosthesis: a systematic review. Sex Med Rev. 2020;8:333–7.
Muneer A, Fowler S, Ralph DJ, Summerton DJ, Rees RW, BAUS Section of Andrology, Genitourethral Surgery. UK practice for penile prosthesis surgery: baseline analysis of the British Association of Urological Surgeons (BAUS) Penile Prosthesis Audit. BJU Int. 2020. https://doi.org/10.1111/bju.15219.
Burnett AL, Nehra A, Breau RH, Culkin DJ, Faraday MM, Hakim LS, et al. Erectile dysfunction: AUA guideline. J Urol. 2018;200:633–41.
Salonia A, Bettocchi C, Capogrosso P, Carvalho J, Corona G, Hatzichristodoulou G, et al. EAU guidelines on sexual and reproductive health. Arnhem, The Netherlands: EAU Guidelines Office; 2023.
Van Huele A, Mennes J, Chung E, Van Renterghem K. Majority of erectile dysfunction patients would have preferred earlier implantation of their penile prosthesis: validation of the recently changed EAU guidelines. Int J Impot Res. 2023;35:731–5.
Chierigo F, Capogrosso P, Dehò F, Pozzi E, Schifano N, Belladelli F, et al. Long-term follow-up after penile prosthesis implantation-survival and quality of life outcomes. J Sex Med. 2019;16:1827–33.
Corona G, Petrone L, Mannucci E, Magini A, Lotti F, Ricca V, et al. Assessment of the relational factor in male patients consulting for sexual dysfunction: the concept of couple sexual dysfunction. J Androl. 2006;27:795–801.
Salonia A, Castagna G, Saccà A, Ferrari M, Capitanio U, Castiglione F, et al. Is erectile dysfunction a reliable proxy of general male health status? The case for the International Index of Erectile Function-Erectile Function domain. J Sex Med. 2012;9:2708–15.
Suarez Arbelaez MC, Nackeeran S, Shah K, Blachman-Braun R, Bronson I, Towe M, et al. Association between body mass index, metabolic syndrome and common urologic conditions: a cross-sectional study using a large multi-institutional database from the United States. Ann Med. 2023;55:2197293.
Wagenknecht LE, Lawrence JM, Isom S, Jensen ET, Dabelea D, Liese AD, et al. Trends in incidence of youth-onset type 1 and type 2 diabetes in the USA, 2002-18: results from the population-based SEARCH for Diabetes in Youth study. Lancet Diabetes Endocrinol. 2023;11:242–50.
Zhou B, Carrillo-Larco RM, Danaei G, Riley LM, Paciorek CJ, Stevens GA, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80.
Kivimäki M, Strandberg T, Pentti J, Nyberg ST, Frank P, Jokela M, et al. Body-mass index and risk of obesity-related complex multimorbidity: an observational multicohort study. Lancet Diabetes Endocrinol. 2022;10:253–63.
Kontis V, Bennett JE, Mathers CD, Li G, Foreman K, Ezzati M. Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet. 2017;389:1323–35.
Falcone M, Rolle L, Ceruti C, Timpano M, Sedigh O, Preto M, et al. Prospective analysis of the surgical outcomes and patients’ satisfaction rate after the AMS Spectra penile prosthesis implantation. Urology. 2013;82:373–6.
Akakpo W, Pineda MA, Burnett AL. Critical analysis of satisfaction assessment after penile prosthesis surgery. Sex Med Rev. 2017;5:244–51.
Atri E, Wong V, Barengo NC, Nieder AM, Polackwich AS. A comparison between AMS 700 and coloplast titan: a systematic literature review. Cureus. 2020;12. https://doi.org/10.7759/cureus.11350.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. 2007;18:800–4.
Tal R, Alphs HH, Krebs P, Nelson CJ, Mulhall JP. Erectile function recovery rate after radical prostatectomy: a meta-analysis. J Sex Med. 2009;6:2538–46.
Mulhall JP, Kattan MW, Bennett NE, Stasi J, Nascimento B, Eastham J, et al. Development of nomograms to predict the recovery of erectile function following radical prostatectomy. J Sex Med. 2019;16:1796–802.
Capogrosso P, Vertosick EA, Benfante NE, Eastham JA, Scardino PJ, Vickers AJ, et al. Are we improving erectile function recovery after radical prostatectomy? Analysis of patients treated over the last decade. Eur Urol. 2019;75:221–8.
Preto M, Falcone M, Plamadeala N, Schifano N, Bettocchi C, Colombo F, et al. Risk of unfavorable outcomes after penile prosthesis implantation - results from a national registry (INSIST-ED). Int J Impot Res. 2023. https://doi.org/10.1038/s41443-023-00784-4.
Chung E. Penile prosthesis implant in the special populations: diabetics, neurogenic conditions, fibrotic cases, concurrent urinary continence surgery, and salvage implants. Asian J Androl. 2019;22:39–44.
Acknowledgements
This work was supported by NIH grants UE5 DK137308, R01 DK130991 to RR. Additionally, we acknowledge resources from the Miami Clinical and Translational Science Institute, which is supported by the National Center for Advancing Translational Sciences, National Institutes of Health, Award Number UL1TR002736.
Author information
Authors and Affiliations
Contributions
EP: writing, conceptualization, data curation; MS: data curation; AS: data curation; JY: data curation; RR: conceptualization, supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pozzi, E., Sandler, M.D., Swayze, A. et al. Early versus late penile prosthesis surgery: a cross-sectional real-life study unveiling predictive factors. Int J Impot Res (2024). https://doi.org/10.1038/s41443-024-00880-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41443-024-00880-z