Abstract
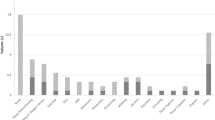
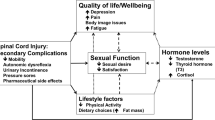
Hard flaccid syndrome (HFS) is a poorly understood condition with no formal consensus on its definition. We aimed to advance the understanding of HFS by evaluating symptom prevalence, cause of symptom onset, comorbidities, and self-reported efficacy and satisfaction with current treatments. An online, open, 42-question survey on Qualtrics with purposive and convenience sampling methods was conducted between May 9 and June 9, 2023 on participants self-identifying as having HFS. Participants were recruited through social media platforms. Only 58.0% of participants reported their HFS symptoms began following a specific incident/injury. Changes in penis shape/size (92.3%) and rigid penis when not erect (90.9%) were the most common complaints. Activities such as laying down and stretching improved symptoms in 73.0% and 44.1% of the participants, respectively, while masturbation and standing worsened symptoms in 75.9%, and 64.5% of the participants, respectively. Pudendal neuralgia (16.9%) was the most prevalent comorbid condition. Of those who participated in therapies, phosphodiesterase-5 (PDE5) inhibitor treatment had the highest patient global impression of change (PGIC) score (2.6 ± 1.1), indicating little to moderate improvement in symptoms. All other therapies scored between 1 and 2, indicating no change to little improvement in symptoms: pelvic floor physical therapy (PFPT) (1.8 ± 0.9), shockwave therapy (1.6 ± 1.1), diet/nutrition changes (1.6 ± 0.8), nerve blocks (1.6 ± 0.8), muscle relaxants (1.5 ± 0.6), anti-inflammatory medications (1.5 ± 0.7), cognitive therapy (1.4 ± 0.7), and nerve pain medications (1.4 ± 0.5). Overall, a direct injury to the penis may not necessarily be the only cause of HFS for some patients, and current therapies generally do not benefit most patients. A better understanding of the root causes of HFS and innovative treatment strategies are greatly needed for HFS patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The data that support these findings are available upon reasonable request from the corresponding author.
References
Abdessater M, Kanbar A, Akakpo W, Beley S. Hard flaccid syndrome: state of current knowledge. Basic Clin Androl. 2020;30:7.
Gul M, Huynh LM, El-Khatib FM, Yafi FA, Serefoglu EC. A qualitative analysis of Internet forum discussions on hard flaccid syndrome. Int J Impot Res. 2020;32:503–9.
Hughes K, Parnham A, Lucky M. Hard flaccid syndrome. Urol News. 2018;23:1.
Goldstein I, Yee A, Komisaruk B. Hard flaccid syndrome proposed to be secondary to pathological activation of a pelvic/pudendal-hypogastric reflex; AUA News. May 2023; 1.
Gul M, Towe M, Yafi FA, Serefoglu EC. Hard flaccid syndrome: initial report of four cases. Int J Impot Res. 2020;32:176–9.
Wang X, Cheng Z. Cross-sectional studies: strengths, weaknesses, and recommendations. Chest. 2020;158:S65–S71.
Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES). J Med Internet Res. 2004;6:e34.
Elfil M, Negida A. Sampling methods in clinical research; an educational review. Emergency. 2017;5:e52.
Campbell S, Greenwood M, Prior S, Shearer T, Walkem K, Young S, et al. Purposive sampling: complex or simple? Research case examples. J Res Nurs. 2020;25:652–61.
Rhoden EL, Riedner CE, Fuchs SC, Ribeiro EP, Halmenschlager G. A cross-sectional study for the analysis of clinical, sexual and laboratory conditions associated to Peyronie’s disease. J Sex Med. 2010;7:1529–37.
Gruenwald I, Gutzeit O, Petruseva A, Gartman I, Lowenstein L. Low-intensity shockwave for treatment of vestibulodynia: a randomized controlled therapy trial. J Sex Med. 2021;18:347–52.
Pukall CF, Bergeron S, Brown C, Bachmann G, Wesselmann U, Vulvodynia Collaborative Research G. Recommendations for self-report outcome measures in vulvodynia clinical trials. Clin J Pain. 2017;33:756–65.
Bergeron S, Khalife S, Dupuis MJ, McDuff P. A randomized clinical trial comparing group cognitive-behavioral therapy and a topical steroid for women with dyspareunia. J Consult Clin Psychol. 2016;84:259–68.
Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, Farrar JT, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9:105–21.
Yachia D. Comment on “A qualitative analysis of Internet forum discussions on hard flaccid syndrome”. Int J Impot Res. 2020;32:551–3.
Spinosa JP, de Bisschop E, Laurençon J, Kuhn G, Dubuisson JB, Riederer BM. [Sacral staged reflexes to localize the pudendal compression: an anatomical validation of the concept]. Rev Med Suisse. 2006;2:2416–8.
Carter OD, Haynes SG. Prevalence rates for scoliosis in US adults: results from the first National Health and Nutrition Examination Survey. Int J Epidemiol. 1987;16:537–44.
Nico E, Rubin R, Trosch L. Successful treatment of hard flaccid syndrome: a case report. J Sex Med. 2022;19:S103.
Acknowledgements
We thank all participants for their willingness to participate in our study. We thank all social media groups for allowing us to advertise the study on their groups.
Funding
No financial assistance was received in support of this study.
Author information
Authors and Affiliations
Contributions
JN: conception, organization, and execution of research project; advertised study on social media; acquired IRB exempt status; designed survey on Qualtrics; collected, managed, and analyzed data; wrote manuscript. DMS: assisted with execution of research project, data interpretation, and manuscript writing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study qualified for exempt status from University of Florida Institutional Review Board since it was an online survey that had no substantial risks to participants, the participants were not identifiable, and the data was confidential.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Niedenfuehr, J., Stevens, D.M. Hard flaccid syndrome symptoms, comorbidities, and self-reported efficacy and satisfaction of treatments: a cross-sectional survey. Int J Impot Res (2024). https://doi.org/10.1038/s41443-024-00853-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41443-024-00853-2