Abstract
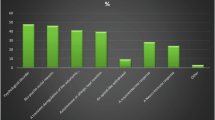
We sought to characterize the prevalence of sexual dysfunction and barriers to treatment among male physicians. Between June and December 2022, male physicians were invited to complete a questionnaire regarding sexual function. Surveys were disseminated electronically via social media and professional medical societies using Qualtrics (Provo, UT). In totla, 235 responses were included in the final analysis. The mean age of respondents was 36.3 ± 7.4 years (range 23–72). 27 (11.5%) reported having seen a doctor for sexual health. Of these 27, 40.7% saw a physician for erectile dysfunction, 29.6% for low libido, 22.2% for premature ejaculation, 7.4% for delayed ejaculation, and 33.3% for other concerns. An additional 29 (12.3%) considered establishing care for sexual issues but didn’t, mostly due to being too busy. 46 (19.6%) respondents reported having taken medication to improve erectile function. Therefore, in a cohort of young male physicians, 23.8% had seen or considered seeing a doctor for sexual health concerns, and nearly 1 in 5 had taken medication for erectile dysfunction. Male physicians appear to be at higher risk for sexual dysfunction than the general population and face significant and unique barriers in access to care for sexual dysfunction.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, JAH, upon reasonable request.
References
Latini DM, Penson DF, Wallace KL, Lubeck DP, Lue TF. Longitudinal differences in psychological outcomes for men with erectile dysfunction: results from ExCEED. J Sex Med. 2006;3:1068–76.
Johannes CB, Araujo AB, Feldman HA, Derby CA, Kleinman KP, McKinlay JB. Incidence of erectile dysfunction in men 40 to 69 years old: longitudinal results from the Massachusetts male aging study. J Urol. 2000;163:460–3.
Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol. 1994;151:54–61.
Rosen R, Altwein J, Boyle P, Kirby RS, Lukacs B, Meuleman E, et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7). Eur Urol. 2003;44:637–49.
Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999;281:537–44.
Batty GD, Li Q, Czernichow S, Neal B, Zoungas S, Huxley R, et al. Erectile dysfunction and later cardiovascular disease in men with type 2 diabetes: prospective cohort study based on the ADVANCE (Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified-Release Controlled Evaluation) trial. J Am Coll Cardiol. 2010;56:1908–13.
Araujo AB, Hall SA, Ganz P, Chiu GR, Rosen RC, Kupelian V, et al. Does erectile dysfunction contribute to cardiovascular disease risk prediction beyond the Framingham risk score? J Am Coll Cardiol. 2010;55:350–6.
Bohm M, Baumhakel M, Teo K, Sleight P, Probstfield J, Gao P, et al. Erectile dysfunction predicts cardiovascular events in high-risk patients receiving telmisartan, ramipril, or both: The ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial/Telmisartan Randomized AssessmeNt Study in ACE iNtolerant subjects with cardiovascular Disease (ONTARGET/TRANSCEND) Trials. Circulation. 2010;121:1439–46.
Schouten BW, Bohnen AM, Bosch JL, Bernsen RM, Deckers JW, Dohle GR, et al. Erectile dysfunction prospectively associated with cardiovascular disease in the Dutch general population: results from the Krimpen Study. Int J Impot Res. 2008;20:92–9.
Hawton K, Catalan J, Fagg J. Sex therapy for erectile dysfunction: characteristics of couples, treatment outcome, and prognostic factors. Arch Sex Behav. 1992;21:161–75.
Suija K, Kerkela M, Rajala U, Jokelainen J, Laakso M, Harkonen P, et al. The association between erectile dysfunction, depressive symptoms and testosterone levels among middle-aged men. Scand J Public Health. 2014;42:677–82.
Aghighi A, Grigoryan VH, Delavar A. Psychological determinants of erectile dysfunction among middle-aged men. Int J Impot Res. 2015;27:63–8.
Huang SS, Lin CH, Chan CH, Loh el W, Lan TH. Newly diagnosed major depressive disorder and the risk of erectile dysfunction: a population-based cohort study in Taiwan. Psychiatry Res. 2013;210:601–6.
Jeon YJ, Yoon DW, Han DH, Won TB, Kim DY, Shin HW. Low quality of life and depressive symptoms as an independent risk factor for erectile dysfunction in patients with obstructive sleep apnea. J Sex Med. 2015;12:2168–77.
Furukawa S, Sakai T, Niiya T, Miyaoka H, Miyake T, Yamamoto S, et al. Depressive symptoms and prevalence of erectile dysfunction in Japanese patients with type 2 diabetes mellitus: the Dogo Study. Int J Impot Res. 2017;29:57–60.
Dyrbye LN, Awad KM, Fiscus LC, Sinsky CA, Shanafelt TD. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;171:600–1.
Oreskovich MR, Kaups KL, Balch CM, Hanks JB, Satele D, Sloan J, et al. Prevalence of alcohol use disorders among American surgeons. Arch Surg. 2012;147:168–74.
Shanafelt TD, Balch CM, Bechamps GJ, Russell T, Dyrbye L, Satele D, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250:463–71.
Ahola K, Pulkki-Raback L, Kouvonen A, Rossi H, Aromaa A, Lonnqvist J. Burnout and behavior-related health risk factors: results from the population-based Finnish Health 2000 study. J Occup Environ Med. 2012;54:17–22.
Goldney R. Suicide by health professionals: a retrospective mortality study in Australia, 2001-2012. Med J Aust. 2017;206:506.
Torre DM, Wang NY, Meoni LA, Young JH, Klag MJ, Ford DE. Suicide compared to other causes of mortality in physicians. Suicide Life Threat Behav. 2005;35:146–53.
Menon NK, Shanafelt TD, Sinsky CA, Linzer M, Carlasare L, Brady KJS, et al. Association of physician burnout with suicidal ideation and medical errors. JAMA Netw Open. 2020;3:e2028780.
Cappelleri JC, Rosen RC, Smith MD, Mishra A, Osterloh IH. Diagnostic evaluation of the erectile function domain of the International Index of Erectile Function. Urology. 1999;54:346–351.
Rosen RC, Catania JA, Althof SE, Pollack LM, O’Leary M, Seftel AD, et al. Development and validation of four-item version of Male Sexual Health Questionnaire to assess ejaculatory dysfunction. Urology. 2007;69:805–9.
Lin CY, Alimoradi Z, Griffiths MD, Pakpour AH. Psychometric properties of the Maslach Burnout Inventory for Medical Personnel (MBI-HSS-MP) Heliyon. 2022;8:e08868.
Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual, 3rd edn. Consulting Psychologists Press: Palo Alto, Calif. (577 College Ave., Palo Alto 94306), 1996.
Laumann EO, Paik A, Rosen RC. The epidemiology of erectile dysfunction: results from the National Health and Social Life Survey. Int J Impot Res. 1999;11:S60–64.
Rosen RC, Fisher WA, Eardley I, Niederberger C, Nadel A, Sand M, et al. The multinational Men’s Attitudes to Life Events and Sexuality (MALES) study: I. Prevalence of erectile dysfunction and related health concerns in the general population. Curr Med Res Opin. 2004;20:607–17.
Bulut EC, Ertas K, Bulut D, Koparal MY, Cetin S. The effect of COVID-19 epidemic on the sexual function of healthcare professionals. Andrologia. 2021;53:e13971.
Viera AJ, Thorpe JM, Garrett JM. Effects of sex, age, and visits on receipt of preventive healthcare services: a secondary analysis of national data. BMC Health Serv Res. 2006;6:15.
Vaidya V, Partha G, Karmakar M. Gender differences in utilization of preventive care services in the United States. J Women’s Health (Larchmt). 2012;21:140–5.
Schlichthorst M, Sanci LA, Pirkis J, Spittal MJ, Hocking JS. Why do men go to the doctor? Socio-demographic and lifestyle factors associated with healthcare utilisation among a cohort of Australian men. BMC Public Health. 2016;16:1028.
Hammond WP, Matthews D, Mohottige D, Agyemang A, Corbie-Smith G. Masculinity, medical mistrust, and preventive health services delays among community-dwelling African-American men. J Gen Intern Med. 2010;25:1300–8.
Cheong AT, Tong SF, Chinna K, Khoo EM, Liew SM. Gender differences in factors influencing intention to undergo cardiovascular disease health checks: A cross-sectional survey. PLoS One. 2020;15:e0239679.
Rice SM, Oliffe JL, Kealy D, Seidler ZE, Ogrodniczuk JS. Men’s help-seeking for depression: attitudinal and structural barriers in symptomatic men. J Prim Care Community Health. 2020;11:2150132720921686.
Duran MB, Yildirim O, Kizilkan Y, Tosun C, Cirakoglu A, Gultekin MH, et al. Variations in the number of patients presenting with andrological problems During the Coronavirus Disease 2019 Pandemic and the Possible Reasons for These Variations: A Multicenter Study. Sex Med. 2021;9:100292.
Fang D, Peng J, Liao S, Tang Y, Cui W, Yuan Y, et al. An online questionnaire survey on the sexual life and sexual function of chinese adult men during the Coronavirus Disease 2019 Epidemic. Sex Med. 2021;9:100293.
Author information
Authors and Affiliations
Contributions
JL, JD, and JH conceived of the presented idea and study design. JL, JD, JA, DR, and JH contributed to the design of the survey and the collection and analysis of survey results. All authors contributed to the dissemination of the survey to respondents. All authors discussed the results of the survey and provided input on the drafted and final manuscripts.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, J.S., Dubin, J.M., Aguiar, J. et al. Prevalence of sexual dysfunction and pursuit of sexual medicine evaluation among male physicians—a survey. Int J Impot Res (2024). https://doi.org/10.1038/s41443-024-00827-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41443-024-00827-4