Abstract
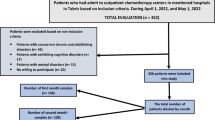
In recent years, numerous epidemiological studies have investigated the prevalence of female sexual dysfunction (FSD) in females with inflammatory bowel disease (IBD). However, a comprehensive systematic review with meta-analysis pooling their findings is lacking. This study aimed to determine the pooled prevalence estimates of FSD and its risk factors among females with IBD based on extensive research in electronic databases (PubMed, Embase, and Web of Science) from inception until April 1, 2023. The overall prevalence of FSD among females with IBD, along with its 95% confidence interval (CI), and subgroup-specific prevalence rates, were summarized. Sources of heterogeneity were identified through subgroup analyses and meta-regression. A total of 13 studies were included in this systematic review and meta-analysis. The pooled global prevalence of FSD among females with IBD was 61.4% (95% CI: 52.8–70.1%). Sensitivity analysis, which involved excluding individual studies, indicated no significant variation in the pooled prevalence, confirming the robustness of our results. Additionally, a significant risk factor for FSD among females with IBD was the quality of life (OR = 0.39, 95% CI: 0.19–0.79). In conclusion, our systematic review and meta-analysis revealed a high prevalence of FSD among females with IBD, which warrants attention from health organizations and clinical practitioners. Importantly, the quality of life was identified as a potential risk factor for FSD in this population. Nonetheless, future prospective cohort studies with a large sample size are warranted to confirm these findings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The original contributions presented in the study are included in the article. Further inquiries can be directed to the corresponding author.
References
Abraham C, Cho JH. Inflammatory bowel disease. N. Engl J Med. 2009;361:2066–78.
Dahlhamer JM, Zammitti EP, Ward BW, Wheaton AG, Croft JB. Prevalence of inflammatory bowel disease among adults aged >/=18 years—United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:1166–9.
Perler BK, Ungaro R, Baird G, Mallette M, Bright R, Shah S, et al. Presenting symptoms in inflammatory bowel disease: descriptive analysis of a community-based inception cohort. BMC Gastroenterol. 2019;19:47.
Abu-Freha N, Cohen B, Gordon M, Weissmann S, Kestenbaum EH, Vosko S, et al. Colorectal cancer among inflammatory bowel disease patients: risk factors and prevalence compared to the general population. Front Med (Lausanne). 2023;10:1225616.
Park KT, Ehrlich OG, Allen JI, Meadows P, Szigethy EM, Henrichsen K, et al. The cost of inflammatory bowel disease: an initiative from the Crohn’s & Colitis foundation. Inflamm Bowel Dis. 2020;26:1–10.
Umar N, King D, Chandan JS, Bhala N, Nirantharakumar K, Adderley N, et al. The association between inflammatory bowel disease and mental ill health: a retrospective cohort study using data from UK primary care. Aliment Pharm Ther. 2022;56:814–22.
Navabi S, Gorrepati VS, Yadav S, Chintanaboina J, Maher S, Demuth P, et al. Influences and impact of anxiety and depression in the setting of inflammatory bowel disease. Inflamm Bowel Dis. 2018;24:2303–8.
Loftus EV Jr., Sandborn WJ. Epidemiology of inflammatory bowel disease. Gastroenterol Clin North Am. 2002;31:1–20.
Clayton AH, Valladares Juarez EM. Female sexual dysfunction. Med Clin North Am. 2019;103:681–98.
Truta B. The impact of inflammatory bowel disease on women’s lives. Curr Opin Gastroenterol. 2021;37:306–12.
Boyd T, de Silva PS, Friedman S. Sexual dysfunction in female patients with inflammatory bowel disease: an overview. Clin Exp Gastroenterol. 2022;15:213–24.
Ona S, James K, Ananthakrishnan AN, Long MD, Martin C, Chen W, et al. Association between vulvovaginal discomfort and activity of inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2020;18:604–11.e601.
Zhao S, Wang J, Liu Y, Luo L, Zhu Z, Li E, et al. Inflammatory bowel diseases were associated with risk of sexual dysfunction in both sexes: a meta-analysis. Inflamm Bowel Dis. 2019;25:699–707.
Zhang J, Wei S, Zeng Q, Wu X, Gan H. Prevalence and risk factors of sexual dysfunction in patients with inflammatory bowel disease: systematic review and meta-analysis. Int J Colorectal Dis. 2021;36:2027–38.
Nohr EA, Nielsen J, Norgard BM, Friedman S. Sexual health in women with inflammatory bowel disease in the danish national birth cohort. J Crohn’s colitis. 2020;14:1082–9.
Knowles SR, Gass C, Macrae F. Illness perceptions in IBD influence psychological status, sexual health and satisfaction, body image and relational functioning: A preliminary exploration using Structural Equation Modeling. J Crohn’s colitis. 2013;7:e344–50.
Yoshida K, Araki T, Uchida K, Okita Y, Fujikawa H, Inoue M, et al. Sexual activity after ileal pouch-anal anastomosis in Japanese patients with ulcerative colitis. Surg Today. 2014;44:73–9.
Muller KR, Prosser R, Bampton P, Mountifield R, Andrews JM. Female gender and surgery impair relationships, body image, and sexuality in inflammatory bowel disease: patient perceptions. Inflamm Bowel Dis. 2010;16:657–63.
Moody GA, Mayberry JF. Perceived sexual dysfunction amongst patients with inflammatory bowel disease. Digestion. 1993;54:256–60.
Boudiaf R, Bouchard D, Riviere P, Brochard C, Laharie D, Abramowitz L, et al. Assessment of sexual dysfunction in patients with perianal Crohn’s disease. Colorectal Dis. 2021;23:114–22.
Domislovic V, Brinar M, Cukovic-Cavka S, Turk N, Mikolasevic I, Krznaric Z. Prevalence, predictors and age-related sexual and erectile dysfunction in patients with inflammatory bowel disease: a tertiary centre experience. Int J Clin Pract. 2021;75:e14486.
Mules TC, Swaminathan A, Hirschfeld E, Borichevsky GM, Frampton CM, Day AS et al. The impact of disease activity on SD and ED in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2022;29:1244–54.
Pires F, Martins D, Ministro P. A survey on the impact of IBD in sexual health: Into intimacy. Medicine. 2022;101:e32279.
Shmidt E, Suarez-Farinas M, Mallette M, Moniz H, Bright R, Shah SA, et al. A longitudinal study of sexual function in women with newly diagnosed inflammatory bowel disease. Inflamm Bowel Dis. 2019;25:1262–70.
Zhang J, Nie J, Zou M, Zeng Q, Feng Y, Luo Z, et al. Prevalence and associated factors of sexual dysfunction in patients with inflammatory bowel disease. Front Endocrinol. 2022;13:881485.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:ED000142.
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208.
McGahuey CA, Gelenberg AJ, Laukes CA, Moreno FA, Delgado PL, McKnight KM, et al. The Arizona Sexual Experience Scale (ASEX): reliability and validity. J sex marital Ther. 2000;26:25–40.
Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health. 2013;67:974–8.
van Houwelingen HC, Arends LR, Stijnen T. Advanced methods in meta-analysis: multivariate approach and meta-regression. Stat Med. 2002;21:589–624.
Shah SC, Khalili H, Chen CY, Ahn HS, Ng SC, Burisch J, et al. Sex-based differences in the incidence of inflammatory bowel diseases-pooled analysis of population-based studies from the Asia-Pacific region. Aliment Pharm Ther. 2019;49:904–11.
Shah SC, Khalili H, Gower-Rousseau C, Olen O, Benchimol EI, Lynge E, et al. Sex-based differences in incidence of inflammatory bowel diseases-pooled analysis of population-based studies from western countries. Gastroenterology. 2018;155:1079–89.e1073.
Gklavas A, Kyprianou C, Exarchos G, Metaxa L, Dellis A, Papaconstantinou I. Sexual function after proctectomy in patients with inflammatory bowel disease: A prospective study. Turkish J Gastroenterol. 2019;30:943–50.
Eluri S, Cross RK, Martin C, Weinfurt KP, Flynn KE, Long MD, et al. Inflammatory bowel diseases can adversely impact domains of sexual function such as satisfaction with sex life. Digest Dis Sci. 2018;63:1572–82.
Xu L, Huang G, Cong Y, Yu Y, Li Y. Sex-related differences in inflammatory bowel diseases: the potential role of sex hormones. Inflamm Bowel Dis. 2022;28:1766–75.
Ates Bulut E, Toruner M. The influence of disease type and activity to sexual life and health quality in inflammatory bowel disease. Turk J Gastroenterol. 2019;30:33–9.
Bel LG, Vollebregt AM, Van der Meulen-de Jong AE, Fidder HH, Ten Hove WR, Vliet-Vlieland CW, et al. Sexual dysfunctions in men and women with inflammatory bowel disease: the influence of IBD-related clinical factors and depression on sexual function. J Sex Med. 2015;12:1557–67.
Harnoy Y, Desfourneaux V, Bouguen G, Rayar M, Meunier B, Siproudhis L, et al. Sexuality and fertility outcomes after hand sewn versus stapled ileal pouch anal anastomosis for ulcerative colitis. J Surg Res. 2016;200:66–72.
Mahmood S, Nusrat S, Crosby A, Zhao YD, Ali T. Assessment of sexual function among inflammatory bowel disease patients. Am J Gastroenterol. 2015;110:601–3.
Marin L, Manosa M, Garcia-Planella E, Gordillo J, Zabana Y, Cabre E, et al. Sexual function and patients’ perceptions in inflammatory bowel disease: a case-control survey. J Gastroenterol. 2013;48:713–20.
Ogilvie JW Jr., Goetz L, Baxter NN, Park J, Minami S, Madoff RD. Female sexual dysfunction after ileal pouch-anal anastomosis. Br J Surg. 2008;95:887–92.
Riviere P, Zallot C, Desobry P, Sabate JM, Vergniol J, Zerbib F, et al. Frequency of and factors associated with sexual dysfunction in patients with inflammatory bowel disease. J Crohn’s colitis. 2017;11:1347–52.
Guyatt G, Mitchell A, Irvine EJ, Singer J, Williams N, Goodacre R, et al. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology. 1989;96:804–10.
Choy CL, Sidi H, Koon CS, Ming OS, Mohamed IN, Guan NC, et al. Systematic review and meta-analysis for sexual dysfunction in women with hypertension. J Sex Med. 2019;16:1029–48.
Loh HH, Yee A, Loh HS, Kanagasundram S, Francis B, Lim LL. Sexual dysfunction in polycystic ovary syndrome: a systematic review and meta-analysis. Hormones. 2020;19:413–23.
Pope R, Lee MH, Myers A, Song J, Abou Ghayda R, Kim JY, et al. Lichen sclerosus and sexual dysfunction: a systematic review and meta-analysis. J Sex Med. 2022;19:1616–24.
Wu X, Zhang Y, Zhang W, Liu G, Huang H, Jiang H, et al. The prevalence and associated risk factors of erectile dysfunction in patients with inflammatory bowel disease: a systematic review and meta-analysis. J Sex Med. 2022;19:950–60.
Wiegel M, Meston C, Rosen R. The female sexual function index (FSFI): cross-validation and development of clinical cutoff scores. J Sex Marital Ther. 2005;31:1–20.
Barberio B, Zamani M, Black CJ, Savarino EV, Ford AC. Prevalence of symptoms of anxiety and depression in patients with inflammatory bowel disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021;6:359–70.
D’Silva A, Fox DE, Nasser Y, Vallance JK, Quinn RR, Ronksley PE, et al. Prevalence and risk factors for fatigue in adults with inflammatory bowel disease: a systematic review with meta-analysis. Clin Gastroenterol Hepatol. 2022;20:995–1009.e1007.
Author information
Authors and Affiliations
Contributions
XLZ provided the presented idea. XLZ, ZRZ, and GLT performed the data analysis. XLZ wrote the manuscript. HLX did critical reading and editing the manuscript. All authors discussed the results and contributed to the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, X., Zhu, Z., Tang, G. et al. The prevalence and risk factors of sexual dysfunction among females with inflammatory bowel disease: a systematic review and meta-analysis. Int J Impot Res (2023). https://doi.org/10.1038/s41443-023-00767-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41443-023-00767-5
This article is cited by
-
Commentary on: The prevalence and risk factors of sexual dysfunction among females with inflammatory bowel disease: a systematic review and meta-analysis
International Journal of Impotence Research (2024)