Abstract
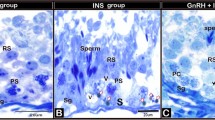
The effects of hormone levels on ejaculation are known. In addition to thyroid hormone levels, testosterone levels are also associated with ejaculation, but no consensus has been reached on this issue. Thus, we investigated the effect of decreased testosterone levels due to bilateral orchiectomy on the chemical stimulation-induced ejaculation phases in rats. Twenty-one male Wistar rats were randomized into the orchiectomy, sham, and control groups, with seven rats in each group. Bilateral orchiectomy was performed. The ejaculation parameters were evaluated 5 days after the sham and bilateral orchiectomy operations and the waiting period in the control group. The seminal vesicle (SV) phasic contraction number and increase in basal pressure amplitude were significantly lower in the orchiectomy group (6.9 ± 3.3 and 0.6 ± 0.3 mmHg) than in the sham and control groups (11.2 ± 1.7 and 1.0 ± 0.4 mmHg, and 14.5 ± 6.6 and 1.1 ± 0.2 mmHg, respectively; p = 0.016 and p = 0.03, respectively). The interval between the SV contractions was significantly longer in the orchiectomy group (166.2 ± 104.3 s) than in the sham and control groups (76.0 ± 15.5 s and 63.1 ± 31.1 s, respectively; p = 0.014 (between groups), orchiectomy vs sham p = 0.040 and orchiectomy vs control p = 0.018). The SV weights of the rats were significantly lower in the orchiectomy group (0.14 ± 0.01 g) than in the sham and control groups (0.37 ± 0.05 g and 0.48 ± 0.03 g respectively; p < 0.0001 (between groups), orchiectomy vs sham p < 0.0001 and orchiectomy vs control p < 0.0001). The groups showed no significant differences in ejaculation time, SV basal pressure, SV maximum amplitude, and bulbospongiosus muscle contraction electromyographic activity. Our results partially clarified the relationship between decreased testosterone levels and ejaculation. Decreased testosterone levels caused statistically significant changes in SV functions and affected the ejaculation emission phase.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
References
Serefoglu EC, Yaman O, Cayan S, Asci R, Orhan I, Usta MF, et al. Prevalence of the complaint of ejaculating prematurely and the four premature ejaculation syndromes: results from the Turkish Society of Andrology Sexual Health Survey. J Sex Med. 2011;8:540–8.
Waldinger MD, Schweitzer DH. The use of old and recent DSM definitions of premature ejaculation in observational studies: a contribution to the present debate for a new classification of PE in the DSM-V. J Sex Med. 2008;5:1079–87.
Giuliano F, Clément P. Serotonin and premature ejaculation: from physiology to patient management. Eur Urol. 2006;50:454–66.
Alizadeh F, Rangzan N, Mohseni M, Rangzan N. Serum testosterone and gonadotropins levels in patients with premature ejaculation: a comparison with normal men. Adv Biomed Res. 2014;3:6.
Corona G, Jannini EA, Mannucci E, Fisher AD, Lotti F, Petrone L, et al. Different testosterone levels are associated with ejaculatory dysfunction. J Sex Med. 2008;5:1991–8.
Deng B, Bondarenko T, Pakhomov O. Changes in sexual behavior of orchidectomized rats under influence of allotransplantation of testicular interstitial cell suspension. Cell Transplant. 2017;26:795–803.
Lin BJT, Chen K-K, Chen M-T, Chang LS. The time for serum testosterone to reach castrate level after bilateral orchiectomy or oral estrogen in the management of metastatic prostatic cancer. Urology. 1994;43:834–7.
Ongün Ş, Acar S, Koca P, Uzut M, Esen AA, Durmus N, et al. Can botulinum-A toxin be used to delay ejaculation: results of an ejaculation model in male rats. J Sex Med. 2019;16:1338–43.
Clément P, Kia HK, Droupy S, Bernabe J, Alexandre L, Denys P, et al. Role of peripheral innervation in p-chloroamphetamine-induced ejaculation in anesthetized rats. J Androl. 2006;27:381–9.
Cihan A, Demir O, Demir T, Aslan G, Comlekci A, Esen A. The relationship between premature ejaculation and hyperthyroidism. J Urol. 2009;181:1273–80.
Cohen PG. The association of premature ejaculation and hypogonadotropic hypogonadism. J Sex Marital Ther. 1997;23:208–11.
Corona G, Jannini EA, Lotti F, Boddi V, Vita GD, Forti G, et al. Premature and delayed ejaculation: two ends of a single continuum influenced by hormonal milieu. Int J Androl. 2011;34:41–8.
Tahtalı IN. Is testosterone replacement an effective treatment of secondary premature ejaculation? Andrologia. 2020;52:e13452.
Culha MG, Tuken M, Gonultas S, Cakir OO, Serefoglu EC. Frequency of etiological factors among patients with acquired premature ejaculation: prospective, observational, single-center study. Int J Impot Res. 2020;32:352–7.
Corona G, Mannucci E, Petrone L, Fisher AD, Balercia G, Scisciolo G, et al. Psychobiological correlates of delayed ejaculation in male patients with sexual dysfunctions. J Androl. 2006;27:453–8.
Wu F, Chen T, Mao S, Jiang H, Ding Q, Xu G. Levels of estradiol and testosterone are altered in Chinese men with sexual dysfunction. Andrology. 2016;4:932–8.
Morgentaler A, Polzer P, Althof S, Bolyakov A, Donatucci C, Ni X, et al. Delayed ejaculation and associated complaints: relationship to ejaculation times and serum testosterone levels. J Sex Med. 2017;14:1116–24.
Abu El-Hamd M, Farah A. Possible role of serum testosterone, gonadotropins and prolactin in patients with premature ejaculation. Andrologia. 2017;50:e12808.
Paduch DA, Polzer PK, Ni X, Basaria S. Testosterone replacement in androgen-deficient men with ejaculatory dysfunction: a randomized controlled trial. J Clin Endocrinol Metab. 2015;100:2956–62.
Keleta YB, Lumia AR, Anderson GM, McGinnis MY. Behavioral effects of pubertal anabolic androgenic steroid exposure in male rats with low serotonin. Brain Res. 2007;9:129–38.
Kim JK, Han WH, Lee MY, Myung CS, Kim SC, Kim MK. Testosterone relaxes rabbit seminal vesicle by calcium channel inhibition. Korean J Physiol Pharmacol. 2008;12:73–7.
Giuliano F, Clement P. Neuroanatomy and physiology of ejaculation. Annu Rev Sex Res. 2005;16:190–216.
Hamill RW, Schroeder B. Hormonal regulation of adult sympathetic neurons: the effects of castration on neuropeptide Y, norepinephrine, and tyrosine hydroxylase activity. J Neurobiol. 1990;21:731–42.
Maggi M, Heiselman D, Knorr J, Iyengar S, Paduch DA, Donatucci CF. Impact of testosterone solution 2% on ejaculatory dysfunction in hypogonadal men. J Sex Med. 2016;13:1220–6.
de Paiva Gonçalves V, Cabrera-Ortega AA, Carvalho JS, Ramadan D, Spolidorio LC. Physiological testosterone replacement effects on male aged rats with orchiectomy-induced osteoporosis in advanced stage: a tomographic and biomechanical pilot study. Aging Male. 2021;24:139–47.
Funding
This study was funded by Dokuz Eylul University under Project No. 2018.KB.SAG.065.
Author information
Authors and Affiliations
Contributions
Conceptualization: SO, E Sarikaya, AS. Experiment execution: SO, E Sarikaya, E Sel, AS. Formal analysis: SO, AS, ND, OG. Methodology: SO, OD, AAE. Funding acquisition: ND, E Sel, OG. Writing–original draft: SO, ND, AS. Writing–review & editing: SO, OD, AAE.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ongun, S., Sarikaya, E., Sarac, A. et al. Bilateral orchiectomy deteriorates the structure and function of seminal vesicles in a rat model. Int J Impot Res (2023). https://doi.org/10.1038/s41443-023-00662-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41443-023-00662-z
This article is cited by
-
Low frequency neuromuscular electrical stimulation applied to the bulbospongiosus muscle prolongs the ejaculation latency in a rat model
International Journal of Impotence Research (2023)