Abstract
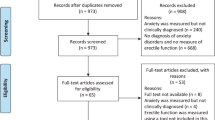
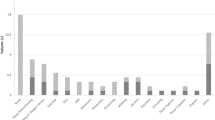
The prevalence of personality disorders (PDs) and sexual dysfunction in chronic pain patients is higher than in general population. Our main objective was to analyse the influence of PD in patients with erectile dysfunction and chronic non-cancer pain and their response to andrological treatment. One-hundred one patients were included along 30 months. Pain intensity, quality of life, sexual life quality, anxiety and depression were analysed together with opioid dose. Erectile functioning was measured with the International Index of Erectile Function (IIEF) and PDs with Millon Clinical Multiaxial Inventory (MCMI-III). The mean age was 57 ± 12 years old, with moderate to severe pain, 70% were sexually active and presented moderate to severe ED. PDs were very frequent (31%, cut-off 85 and 84% cut-off 75 scores) mostly anxiety, compulsive, though disorder, somatoform and narcissistic. Self-defeating feature presence was significantly correlated (r = −0.4, 95% CI = −0.605 to −0.145, p = 0.002) with a more severe baseline ED and narcissistic, and a better response to andrological treatment (p = 0.010, d = 1.082). Patients with dysthymia features required significantly higher opioid doses vs. control (238 vs. 102 mg/day, respectively). These findings underline the importance of diagnosing PDs to rigorously treat patients with chronic pain and ED.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
NIH Consensus Conference. Impotence. NIH Consensus Development Panel on Impotence. JAMA. 1993;270:83–90.
Özkorumak E, Karkucak M, Civil F, Tiryaki A, Özden G. Sexual function in male patients with ankylosing spondylitis. Int J Impot Res. 2011;23:262–7.
Bal S, Bal K, Turan Y, Deniz G, Gurgan A, Berkit IK, et al. Sexual functions in ankylosing spondylitis. Rheumatol Int. 2011;31:889–94.
Pirildar T, Muezzinoglu T, Pirildar S. Sexual function in ankylosing spondylitis: a study of 65 men. J Urol. 2004;171:1598–600.
Shen B, Zhang A, Liu J, Da Z, Xu X, Gu Z. A primary analysis of sexual problems in Chinese patients with ankylosing spondylitis. Rheumatol Int. 2013;33:1429–35.
SED Sociedad Española del Dolor. Manual de Medicina del Dolor Fundamentos, evaluación y tratamiento. Madrid: Editorial Médica Panamericana; 2016. p. 542.
Samolsky Dekel BG, Ghedini S, Gori A, Vasarri A, Di Nino G, Melotti RM. Lasting prolonged-release tapentadol for moderate/severe non-cancer musculoskeletal chronic pain. Pain Ther. 2015;4:107–17.
Varrassi G, Muller-Schwefe G, Pergolizzi J, Oronska A, Morlion B, Mavrocordatos P, et al. Pharmacological treatment of chronic pain—the need for CHANGE. Curr Med Res Opin. 2010;26:1231–45.
Pergolizzi J, Ahlbeck K, Aldington D, Alon E, Coluzzi F, Dahan A, et al. The development of chronic pain: physiological CHANGE necessitates a multidisciplinary approach to treatment. Curr Med Res Opin. 2013;29:1127–35.
Ajo R, Segura A, Inda MD, Planelles B, Martinez L, Ferrandez G, et al. Opioids increase sexual dysfunction in patients with non-cancer pain. J Sex Med. 2016;13:1377–86.
Ajo R, Segura A, Inda MD, Margarit C, Ballester P, Martinez E, et al. Erectile dysfunction in patients with chronic pain treated with opioids. Disfunción eréctil en pacientes con dolor crónico tratados con opioides. Med Clin (Barc). 2017;149:49–54. https://doi.org/10.1016/j.medcli.2016.12.038.
Kimball AB, Jacobson C, Weiss S, Vreeland MG, Wu Y. The psychosocial burden of psoriasis. Am J Clin Dermatol. 2005;6:383–92.
Palijan TZ, Kovacevic D, Koic E, Ruzic K, Dervinja F. The impact of psoriasis on the quality of life and psychological characteristics of persons suffering from psoriasis. Coll Antropol. 2011;35:81–5.
Ajo R, Segura A, Mira L, Inda MD, Alfayate R, Sanchez-Barbie A, et al. The relationship of salivary testosterone and male sexual dysfunction in opioid-associated androgen deficiency (OPIAD). Aging Male. 2017;20:1–8.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). Washington, DC: American Psychiatric Publishing; 2013.
Millon T. Classifying personality disorders: an evolution-based alternative to an evidence-based approach. J Personal Disord. 2011;25:279–304.
Millon T, Grossman SD, Lenzenweger M, Clarkin J. Personology: a theory based on evolutionary concepts. In: Clarkin J, Lenzenweger M (eds). Major theories of personality disorder (2nd ed.). New York: Guilford; 2005. pp. 282–331.
Pergolizzi J, Boger RH, Budd K, Dahan A, Erdine S, Hans G, et al. Opioids and the management of chronic severe pain in the elderly: consensus statement of an International Expert Panel with focus on the six clinically most often used World Health Organization Step III opioids (buprenorphine, fentanyl, hydromorphone, methadone, morphine, oxycodone). Pain Pract. 2008;8:287–313.
Cardenal V, Sánchez M, Ortiz-Tallo M. Adaptación y baremación al español del Inventario Clínico Multiaxial de Millon-III (MCMI-III). Madrid: TEA Ediciones. 2007.
Rossi G, Derksen J. International adaptations of the Millon Clinical Multiaxial Inventory: construct validity and clinical applications. J Personal Assess. 2015;97:572–90.
Exner J, Exner J, Levy A, Exner J, Groth-Marnat G, Wood J, et al. The Rorschach: a comprehensive system. Basic foundations and principles of interpretation (4th ed., Vol. 1). Hoboken, NJ: John Wiley & Sons, New York; 2008.
Herdman M, Badía X, Berra S. El EuroQol-5D: una alternativa sencilla para la medición de la calidad de vida relacionada con la salud en atención primaria. Aten Prim. 2001;28:425–9.
Snaith RP. The hospital anxiety and depression scale. Health Qual Life Outcomes. 2003;1:29.
Rosen RC, Cappelleri J, Gendrano N. The International Index of Erectile Function (IIEF): a state-of-the-science review. Int J Impot Res. 2002;14:226.
Woodward JM, Hass SL, Woodward PJ. Reliability and validity of the sexual life quality questionnaire (SLQQ). Qual Life Res. 2002;11:365–77.
Conrad R, Schilling G, Bausch C, Nadstawek J, Wartenberg HC, Wegener I, et al. Temperament and character personality profiles and personality disorders in chronic pain patients. Pain. 2007;133:197–209.
Fischer-Kern M, Kapusta ND, Doering S, Horz S, Mikutta C, Aigner M. The relationship between personality organization and psychiatric classification in chronic pain patients. Psychopathology. 2011;44:21–6.
Goldstein RB, Dawson DA, Chou SP, Grant BF. Sex differences in prevalence and comorbidity of alcohol and drug use disorders: results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Stud Alcohol Drugs. 2012;73:938–50.
Trull TJ, Jahng S, Tomko RL, Wood PK, Sher KJ. Revised NESARC personality disorder diagnoses: gender, prevalence, and comorbidity with substance dependence disorders. J Personal Disord. 2010;24:412–26.
Litwin MS, Nied RJ, Dhanani N. Health‐related quality of life in men with erectile dysfunction. J Gen Intern Med. 1998;13:159–66.
Burri A, Spector T. Recent and lifelong sexual dysfunction in a female UK population sample: prevalence and risk factors. J Sex Med. 2011;8:2420–30.
McMahon CG, Jannini E, Waldinger M, Rowland D. Standard operating procedures in the disorders of orgasm and ejaculation. J Sex Med. 2013;10:204–29.
Angstman KB, Seshadri A, Marcelin A, Gonzalez CA, Garrison GM, Allen JS. Personality disorders in primary care: impact on depression outcomes within collaborative care. J Prim Care Community Health. 2017;8:233–8.
French L, Turner K, Dawson S, Moran P. Psychological treatment of depression and anxiety in patients with co‐morbid personality disorder: a scoping study of trial evidence. Personal Ment Health. 2017;11:101–17.
Dixon-Gordon KL, Berghoff CR, McDermott MJ. Borderline personality disorder symptoms and pain in college students: the role of emotional suppression. J Personal Disord. 2018;32:277–88. https://doi.org/10.1521/pedi_2017_31_300.
Sternbach RA, Wolf S, Murphy R, Akeson W. Traits of pain patients: the low-back “loser”. Psychosomatics. 1973;14:226–9.
Kalmbach DA, Ciesla JA, Janata JW, Kingsberg SA. Specificity of anhedonic depression and anxious arousal with sexual problems among sexually healthy young adults. J Sex Med. 2012;9:505–13.
Kurd SK, Troxel AB, Crits-Christoph P, Gelfand JM. The risk of depression, anxiety, and suicidality in patients with psoriasis: a population-based cohort study. Arch Dermatol. 2010;146:891–5.
Chang M-C, Chen P-F, Lung F-W. Personality disparity in chronic regional and widespread pain. Psychiatry Res. 2017;254:284–9.
Lavan H, Johnson JG. The association between axis I and II psychiatric symptoms and high-risk sexual behavior during adolescence. J Personal Disord. 2002;16:73–94.
Langas AM, Malt UF, Opjordsmoen S. In-depth study of personality disorders in first-admission patients with substance use disorders. BMC Psychiatry. 2012;12:180.
Zikos E, Gill KJ, Charney DA. Personality disorders among alcoholic outpatients: prevalence and course in treatment. Can J Psychiatry. 2010;55:65–73.
Payer DE, Park MTM, Kish SJ, Kolla NJ, Lerch JP, Boileau I, et al. Personality disorder symptomatology is associated with anomalies in striatal and prefrontal morphology. Front Hum Neurosci. 2015;9:472. Published 2015 Aug 31. https://doi.org/10.3389/fnhum.2015.00472.
Acknowledgements
We acknowledge the help received from Dr Olga Alda (pain clinical coordinator), Ms Raquel Martín (pain health care assistant), Ms Emi Martínez (biology fellow) and Mr Carlos García-Navas (pharmacy fellow).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ajo, R., Inda, MdM., Mateu, M. et al. Personality and psychiatric disorders in chronic pain male affected by erectile dysfunction: prospective and observational study. Int J Impot Res 33, 339–347 (2021). https://doi.org/10.1038/s41443-020-0294-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-020-0294-9
This article is cited by
-
Sexual Dysfunctions and Problematic Sexuality in Personality Disorders and Pathological Personality Traits: A Systematic Review
Current Psychiatry Reports (2023)