Abstract
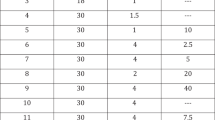
Successful treatment of erectile dysfunction (ED) is associated with improvements in quality of life; however, treatment utilisation is sub-optimal. The aim of this systematic review was to identify the rates of ED treatment utilisation and the barriers and enablers men experience when using treatment. We searched: MEDLINE®, Embase, the Cochrane library; AMED; HMIC; HTA; CINAHL; PsychARTICLES; PsychINFO up to August 2018. Data on rates of treatment utilisation and barriers and enablers of utilisation were extracted and summarised. Fifty studies were included. Discontinuation rates ranged from 4.4 to 76% for phosphodiesterase type 5 inhibitors, 18.6 to 79.9% for intracavernosal injections, and 32 to 69.2% for urethral suppositories. In relation to those with a penile prosthesis, 30% discontinued having sex due to, e.g. device complications, lack of partner or a loss of sexual interest. Most research included in the current review examined barriers to treatment utilisation and therefore focussed on reasons for discontinuing treatment. However, a small number explored factors that men found helpful with regards to treatment utilisation. The most prevalent barriers to utilisation were treatment ineffectiveness, side effects, the quality of men’s intimate relationships and treatment costs. With regards to treatment enablers, the most salient finding was that men who reported side effects to a healthcare professionals (HCPs) were significantly less likely to discontinue treatment. There were limitations in methodology in that the studies did not use validated measures of treatment utilisation or barriers and enablers and no study used psychological theory to inform the examination of factors that influenced treatment utilisation. This review identifies a number of influential factors relating to ED treatment utilisation and highlights the importance of men’s beliefs with regards to ED and its treatment. Beliefs are potentially modifiable and therefore the findings of this review highlight important considerations for HCPs with regards to supporting men to make better use of treatment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Nehra A, Jackson G, Miner M, Billups KL, Burnett AL, Buvat J, et al. The Princeton III Consensus recommendations for the management of erectile dysfunction and cardiovascular disease. Mayo Clinic Proc. 2012;87:766–78.
Lewis RW, Fugl‐Meyer KS, Corona G, Hayes RD, Laumann EO, Moreira ED Jr, et al. Definitions/epidemiology/risk factors for sexual dysfunction. J Sex Med. 2010;7:1598–607.
Fugl-Meyer A, Lodnert G, Bränholm I, Fugl-Meyer K. On life satisfaction in male erectile dysfunction. Int J Impot Res. 1997;9:141.
Jonler M, Moon T, Brannan W, Stone NN, Heisey D, Bruskewitz RC. The effect of age, ethnicity and geographical location on impotence and quality of life. Br J Urol. 1995;75:651–5.
Guest JF, Gupta RD. Health-related quality of life in a UK-based population of men with erectile dysfunction. Pharmacoeconomics. 2002;20:109–17.
Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol. 1994;151:54–61.
Shabsigh R, Klein LT, Seidman S, Kaplan SA, Lehrhoff BJ, Ritter JS. Increased incidence of depressive symptoms in men with erectile dysfunction. Urology. 1998;52:848–52.
Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. J Am Med Assoc. 1999;281:537–44.
Moreira ED Jr, Abdo CHN, Torres EB, Lôbo CFL, Fittipaldi JAS. Prevalence and correlates of erectile dysfunction: results of the Brazilian study of sexual behavior. Urology. 2001;58:583–8.
Turner LA, Althof SE, Levine SB, Bodner DR, Kursh ED, Resnick MI. Twelve-month comparison of two treatments for erectile dysfunction: self-injection versus external vacuum devices. Urology. 1992;39:139–44.
Costa P, Grandmottet G, Mai HD, Droupy S. Impact of a first treatment with phosphodiesterase inhibitors on men and partners’ quality of sexual life: results of a prospective study in primary care. J Sex Med. 2013;10:1850–60.
McCabe MP, O’Connor EJ, Conaglen JV, Conaglen HM. The impact of oral ED medication on female partners’ relationship satisfaction. J Sex Med. 2011;8:479–83.
Rosen RC, Fisher WA, Eardley I, Niederberger C, Nadel A, Sand M. The multinational Men’s Attitudes to Life Events and Sexuality (MALES) study: I. Prevalence of erectile dysfunction and related health concerns in the general population. Curr Med Res Opin. 2004;20:607–17.
Shabsigh R, Zakaria L, Anastasiadis AG, Seidman SN. Sexual dysfunction and depression: etiology, prevalence, and treatment. Curr Urol Rep. 2001;2:463–7.
Williams G, Abbou C, Amar E, Desvaux P, Flam T, Lynch S, et al. The effect of transurethral alprostadil on the quality of life of men with erectile dysfunction, and their partners. MUSE Study Group. Br J Urol. 1998;82:847–54.
McKernan S. Erectile dysfunction guidance 2015. http://www.lancsmmg.nhs.uk/wp-content/uploads/sites/3/2013/04/Erectile-Dysfunction-Guideline-Version-1.0.pdf.
Hatzimouratidis K, Giuliano F, Moncada I, Muneer A, Salonia A, Verze P. EAU guidelines on erectile dysfunction, premature ejaculation, penile curvature and priapism. Eur Assoc Urol. 2016;46. https://uroweb.org/wp-content/uploads/EAU-Guidelines-Male-Sexual-Dysfunction-2016.pdf. Accessed 7 July 2018.
Morales AM, Casillas M, Turbi C. Patients’ preference in the treatment of erectile dysfunction: a critical review of the literature. Int J Impot Res. 2011;23:1.
Hackett GI. Patient preferences in treatment of erectile dysfunction: the continuing importance of patient education. Clin Cornerstone. 2005;7:57–64.
Althof S. When an erection alone is not enough: biopsychosocial obstacles to lovemaking. Int J Impot Res. 2002;14(S1):S99.
Nunes V, Neilson J, O’flynn N, Calvert N, Kuntze S, Smithson H, et al. Medicines adherence: Involving patients in decisions about prescribed medicines and supporting adherence. NICE Clinical Guidance. 2009;1–30.
Collaboration TC Effective Practice and Organisation of Care (EPOC). Data collection form. EPOC resources for review authors. Oslo: Norwegian Knowledge Centre for the Health Services; 2013;7-3-2014.
Kmet LM, Cook LS, Lee RC. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Edmonton: Alberta Heritage Foundation for Medical Research (AHFMR). HTA Initiative #13. 2004.
Johnson S, Butow P, Kerridge I, Tattersall M. Advance care planning for cancer patients: a systematic review of perceptions and experiences of patients, families, and healthcare providers. Psycho‐Oncol. 2016;25:362–86.
Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J health Serv Res Policy. 2005;10 suppl 1:6–20.
Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11:44–7.
Carvalheira A, Forjaz V, Pereira NM. Adherence to phosphodiesterase type 5 inhibitors in the treatment of erectile dysfunction in long-term users: how do men use the inhibitors? Sex Med. 2014;2:96–102.
Conaglen HM, Conaglen JV. Couples’ reasons for adherence to, or discontinuation of, PDE type 5 inhibitors for men with erectile dysfunction at 12 to 24‐month follow‐up after a 6‐month free trial. J Sex Med. 2012;9:857–65.
Buvat J, Hatzichristou D, Boess F, Büttner H, Gehchan N, Henneges C, et al. Continuation and effectiveness of tadalafil once daily during a 6‐month observational study in erectile dysfunction: the EDATE study. Int J Clin Pract. 2014;68:1087–99.
McMurray JG, Feldman RA, Auerbach SM, DeRiesthal H, Wilson N, Group MS. Long-term safety and effectiveness of sildenafil citrate in men with erectile dysfunction. Ther Clin Risk Manag. 2007;3:975.
Buvat J, Büttner H, Hatzimouratidis K, Vendeira PA, Moncada I, Boehmer M, et al. Adherence to initial PDE5 inhibitor treatment: randomized OpenLabel study comparing tadalafil once a day, tadalafil on demand, and sildenafil on demand in patients with erectile dysfunction. J Sex Med. 2013;10:1592–602.
Kim E, Seftel A, Goldfischer E, Baygani S, Burns P. Comparative efficacy of tadalafil once daily in men with erectile dysfunction who demonstrated previous partial responses to as-needed sildenafil, tadalafil, or vardenafil. Curr Med Res Opin. 2015;31:379–89.
Mazzola CR, Deveci S, Teloken P, Mulhall JP. Exploring the association between erectile rigidity and treatment adherence with sildenafil. J Sex Med. 2013;10:1861–6.
Kim S, Lee Y, Seo K, Jung G, Kim T. Reasons and predictive factors for discontinuation of PDE-5 inhibitors despite successful intercourse in erectile dysfunction patients. Int J Impot Res. 2014;26:87.
Carvalheira AA, Pereira NM, Maroco J, Forjaz V. Dropout in the treatment of erectile dysfunction with PDE5: a study on predictors and a qualitative analysis of reasons for discontinuation. J Sex Med. 2012;9:2361–9.
Roumeguère T, Verheyden B, Arver S, Bitton A, Belger M, Schmitt H, et al. Therapeutic response after first month of tadalafil treatment predicts 12 months treatment continuation in patients with erectile dysfunction: results from the DETECT study. J Sex Med. 2008;5:1708–19.
Salonia A, Abdollah F, Gallina A, Pellucchi F, Molina RAC, Maccagnano C, et al. Does educational status affect a patient’s behavior toward erectile dysfunction? J Sex Med. 2008;5:1941–8.
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–30.
Rosen RC, Cappelleri J, Smith M, Lipsky J, Pena B. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319.
Sexton WJ, Benedict JF, Jarow JP. Comparison of long-term outcomes of penile prostheses and intracavernosal injection therapy. J Urol. 1998;159:811–5.
Cairoli C, Reyes LA, Henneges C, Sorsaburu S. PDE5 inhibitor treatment persistence and adherence in Brazilian men: post-hoc analyses from a 6-month, prospective, observational study. Int Braz J Urol. 2014;40:390–9.
El-Meliegy A, Rabah D, Al-Mitwalli K, Mostafa T, Hussein T, Istarabadi M, et al. A 6-month, prospective, observational study of PDE5 inhibitor treatment persistence and adherence in Middle Eastern and North African men with erectile dysfunction. Curr Med Res Opin. 2013;29:707–17.
Rubio-Aurioles E, Reyes LA, Borregales L, Cairoli C, Sorsaburu S. A 6 month, prospective, observational study of PDE5 inhibitor treatment persistence and adherence in Latin American men with erectile dysfunction. Curr Med Res Opin. 2013;29:695–706.
Souverein P, Egberts A, Meuleman E, Urquhart J, Leufkens H. Incidence and determinants of sildenafil (dis) continuation: the Dutch cohort of sildenafil users. Int J Impot Res. 2002;14:259.
Jiann B, Yu C, Su C, Tsai J. Compliance of sildenafil treatment for erectile dysfunction and factors affecting it. Int J Impot Res. 2006;18:146.
Lee DJ, Cheetham P, Badani KK. Penile rehabilitation protocol after robot‐assisted radical prostatectomy: assessment of compliance with phosphodiesterase type 5 inhibitor therapy and effect on early potency. BJU Int 2010;105:382–8.
Sato Y, Tanda H, Kato S, Onishi S, Nitta T, Koroku M. How long do patients with erectile dysfunction continue to use sildenafil citrate? Dropout rate from treatment course as outcome in real life. Int J Urol. 2007;14:339–42.
Lehmann K, Casella R, Blöchlinger A, Gasser T. Reasons for discontinuing intracavernous injection therapy with prostaglandin E1 (alprostadil). Urology. 1999;53:397–400.
Rowland D, Boedhoe H, Dohle G, Slob A. Intracavernosal self-injection therapy in men with erectile dysfunction: satisfaction and attrition in 119 patients. Int J Impot Res. 1999;11:145.
Purvis K, Egdetveit I, Christiansen E. Intracavernosal therapy for erectile failure—impact of treatment and reasons for drop-out and dissatisfaction. Int J Impot Res. 1999;11:287.
El-Galley R, Rutland H, Talic R, Keane T, Clark H. Long-term efficacy of sildenafil and tachyphylaxis effect. J Urol. 2001;166:927–31.
Fagelman E, Fagelman A, Shabsigh R. Efficacy, safety, and use of sildenafil in urologic practice. Urology. 2001;57:1141–4.
Green BG, Martin S. Clinical assessment of sildenafil in the treatment of neurogenic male sexual dysfunction: after the hype. NeuroRehabilitation. 2000;15:101–5.
Incrocci L, Hop WC, Slob AK. Efficacy of sildenafil in an open-label study as a continuation of a double-blind study in the treatment of erectile dysfunction after radiotherapy for prostate cancer. Urology. 2003;62:116–20.
Ljunggren C, Hedelin H, Salomonsson K, Stroberg P. Giving patients with erectile dysfunction the opportunity to try all three available phosphodiesterase type 5 inhibitors. J Sex Med. 2008;5:469–75.
Montorsi F, Verheyden B, Meuleman E, Jünemann K-P, Moncada I, Valiquette L, et al. Long-term safety and tolerability of tadalafil in the treatment of erectile dysfunction. Eur Urol. 2004;45:339–45.
Raina R, Lakin MM, Agarwal A, Sharma R, Goyal KK, Montague DK, et al. Long-term effect of sildenafil citrate on erectile dysfunction after radical prostatectomy: 3-year follow-up. Urology. 2003;62:110–5.
Salonia A, Gallina A, Zanni G, Briganti A, Deho F, Sacca A, et al. Acceptance of and discontinuation rate from erectile dysfunction oral treatment in patients following bilateral nerve-sparing radical prostatectomy. Eur Urol. 2008;53:564–70.
Bai W-J, Li H-J, Dai Y-T, He X-Y, Huang Y-R, Liu J-H, et al. An open-label, multicenter, randomized, crossover study comparing sildenafil citrate and tadalafil for treating erectile dysfunction in Chinese men naïve to phosphodiesterase 5 inhibitor therapy. Asian J Androl. 2015;17:61.
Choi H, Kim J, Shim J, Park JY, Kang SH, Moon DG, et al. Comparison of the efficacy and safety of 5-mg once-daily versus 5-mg alternate-day tadalafil in men with erectile dysfunction and lower urinary tract symptoms. Int J Impot Res. 2015;27:33.
Panach-Navarrete J, Morales-Giraldo A, Ferrandis-Cortés C, García-Morata F, Pastor-Lence J, Martínez-Jabaloyas J. Satisfaction and treatment adherence in erectile dysfunction in the medium and long term. Actas Urológicas Españolas. 2017;41:258–66.
Sung H, Ahn J, Kim J-J, Choo S, Han D, Lee S. The role of intracavernosal injection therapy and the reasons of withdrawal from therapy in patients with erectile dysfunction in the era of PDE 5 inhibitors. Andrology. 2014;2:45–50.
GROUP EAS. The long‐term safety of alprostadil (prostaglandin‐E1) in patients with erectile dysfunction. Br J Urol. 1998;82:538–43.
Armstrong D, Convery A, Dinsmore W. Reasons for patient drop‐out from an intracavernous autoinjection programme for erectile dysfunction. Br J Urol. 1994;74:99–101.
Gerber GS, Levine LA. Pharmacological erection program using prostaglandin E1. J Urol. 1991;146:786–9.
Kunelius P, Lukkarinen O. Intracavernous self-injection of prostaglandin E1 in the treatment of erectile dysfunction. Int J Impot Res. 1999;11:21.
Perimenis P, Gyftopoulos K, Athanasopoulos A, Barbalias G. Diabetic impotence treated by intracavernosal injections: high treatment compliance and increasing dosage of vaso–active drugs. Eur Urol. 2001;40:398–403.
Polito M, d’Anzeo G, Conti A, Muzzonigro G. Erectile rehabilitation with intracavernous alprostadil after radical prostatectomy: refusal and dropout rates. BJU Int. 2012;110:E954–7.
Raina R, Lakin M, Thukral M, Agarwal A, Ausmundson S, Montague D, et al. Long-term efficacy and compliance of intracorporeal (IC) injection for erectile dysfunction following radical prostatectomy: SHIM (IIEF-5) analysis. Int J Impot Res. 2003;15:318.
Mulhall JP, Jahoda AE, Ahmed A, Parker M. Analysis of the consistency of intraurethral prostaglandin E1 (MUSE) during at-home use. Urology. 2001;58:262–6.
Raina R, Agarwal A, Ausmundson S, Mansour D, Zippe C. Long-term efficacy and compliance of MUSE for erectile dysfunction following radical prostatectomy: SHIM (IIEF-5) analysis. Int J Impot Res. 2005;17:86.
Raina R, Pahlajani G, Agarwal A, Zippe CD. The early use of transurethral alprostadil after radical prostatectomy potentially facilitates an earlier return of erectile function and successful sexual activity. BJU Int. 2007;100:1317–21.
Cimen S, Demir O, Aslan G, Esen AA. Factors associated with phosphodiesterase type 5 inhibitor treatment satisfactions: results of patient interrogation. Aging Male. 2009;12:58–61.
Klotz T, Mathers M, Klotz R, Sommer F. Why do patients with erectile dysfunction abandon effective therapy with sildenafil (Viagra®)? Int J Impot Res. 2005;17:2.
Ricardi U, Gontero P, Ciammella P, Badellino S, Valentino F, Munoz F, et al. Efficacy and safety of tadalafil 20 mg on demand vs. tadalafil 5 mg once‐a‐day in the treatment of post‐radiotherapy erectile dysfunction in prostate cancer men: a randomized phase II trial. J Sex Med. 2010;7:2851–9.
Li G, Lan H, Liang J, Zhang C, Huang C. Efficacy of tadalafil de-escalation in the treatment of psychogenic erectile dysfunction. Urol Int. 2017;98:205–9.
Irwin MB, Kata EJ. High attrition rate with intracavernousinjection of prostaglandin E1 for impotency. Urology. 1994;43:84–7.
Son H, Park K, Kim S-W, Paick J-S. Reasons for discontinuation of sildenafil citrate after successful restoration of erectile function. Diabetes. 2004;23:16.70.
DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004:42;200–9.
Ian Peate O. Men’s health: the practice nurse’s handbook. United States: John Wiley & Sons; 2007.
Horne R, Clatworthy J, Polmear A, Weinman J. Do hypertensive patients’ beliefs about their illness and treatment influence medication adherence and quality of life? J Hum Hypertens. 2001;15:S65.
Horne R, Clatworthy J, Hankins M, Investigators A. High adherence and concordance within a clinical trial of antihypertensives. Chronic Illn. 2010;6:243–51.
Horne R, Chapman SC, Parham R, Freemantle N, Forbes A, Cooper V. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the Necessity-Concerns Framework. PLoS ONE. 2013;8:e80633.
Petrie KJ, Weinman J. Perceptions of health and illness: current research and applications. London: Taylor & Francis; 1997.
Horne R, Weinman J, Barber N. Concordance, adherence and compliance in medicine taking: a conceptual map and research priorities. London: National Coordinating Centre for NHS Service Delivery and Organisation (NCCSDO); 2006.
Department of Health. NHS executive health service circular. England: Department of Health; 1999.
Partnership M. Can I get medication for erectile dysfunction (ED) on the NHS? 2019. https://modalitypartnership.nhs.uk/self-help/chq/articles/882-can-i-get-medication-for-erectile-dysfunction-(ed)-on-the-nhs. Accessed 6 June 2019.
Group CPJP. Prescribing policy: drugs and devices used in the treatment of erectile dysfunction. 2018. https://www.cambridgeshireandpeterboroughccg.nhs.uk/easysiteweb/getresource.axd?assetid=15703&type=0&servicetype=1. Accessed 6 June 2019.
Committe PMAP. Phosphodiesterase type-5 inhibitors for the treatment of erectile dysfunction. 2018. https://www.panmerseyapc.nhs.uk/media/2039/phosphodiesterase5inhibitors_201807_v0601.pdf. Accessed 6 June 2019.
Wu FC, Tajar A, Beynon JM, Pye SR, Silman AJ, Finn JD, et al. Identification of late-onset hypogonadism in middle-aged and elderly men. N. Engl J Med. 2010;363:123–35.
Garfield S, Clifford S, Eliasson L, Barber N, Willson A. Suitability of measures of self-reported medication adherence for routine clinical use: a systematic review. BMC Med Res Methodol. 2011;11:149.
Wagner J, Justice A, Chesney M, Sinclair G, Weissman S, Rodriguez-Barradas M. Patient-and provider-reported adherence: toward a clinically useful approach to measuring antiretroviral adherence. J Clin Epidemiol. 2001;54:S91–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Williams, P., McBain, H., Amirova, A. et al. Men’s beliefs about treatment for erectile dysfunction—what influences treatment use? A systematic review. Int J Impot Res 33, 16–42 (2021). https://doi.org/10.1038/s41443-020-0249-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-020-0249-1
This article is cited by
-
News and future perspectives of non-surgical treatments for erectile dysfunction
International Journal of Impotence Research (2023)
-
Erektile Dysfunktion: Diagnostik und Therapie
Urologie in der Praxis (2023)