Abstract
Penile prosthesis implantation is a safe and effective treatment option in the management of erectile dysfunction, associated with high satisfaction and low complication rates. Infection is a rare complication (0.5–3%), but devastating for the patient and surgeon when it occurs. Adapting from other surgical disciplines, we have utilized vancomycin paste to provide prolonged focal antibiotic exposure around the penile prosthesis pump, a site prone to infection. The aim of this study is to determine the safety and efficacy of intraoperative vancomycin paste with regards to infection prevention during penile prosthesis placement. This is a multi-institutional nonrandomized retrospective IRB-approved study comparing patients who underwent placement of a primary inflatable penile prosthesis with intraoperative vancomycin paste to those without. Primary outcomes included pump fibrosis, infection, erosion, hematoma, and complete device malfunction. From April 2019 to October 2019, two surgeons utilized vancomycin paste intraoperatively during virginal penile prosthesis surgery on 90 patients, whose mean age was 60 years. These patients were compared to an historical control group that included 166 patients, also with a mean age of 60 years, who underwent the same penile prosthesis surgery between 2014 and 2017 without the paste. Among the intervention group, the overall complication rate was 1.1%, due to a scrotal hematoma. Ultimately, there was no statistically significant difference in infection rate (0% in both groups) or overall complication rate (1.1% in the intervention group compared to 1.2% in the control group). The use of vancomycin paste appears to be safe, however future prospective studies are needed to determine its efficacy in infection prevention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Montague DK, Jarow JP, Broderick GA, Dmochowski RR, Heaton JPW, Lue TF, et al. Chapter 1: the management of erectile dysfunction: an AUA update. J Urol. 2005;174:230–9.
Mulhall JP, Ahmed A, Branch J, Parker M. Serial assessment of efficacy and satisfaction profiles following penile prosthesis surgery. J Urol. 2003;169:1429–33.
Mulcahy JJ, Carson CC. Long-term infection rates in diabetic patients implanted with antibiotic-impregnated versus nonimpregnated inflatable penile prostheses: 7-year outcomes. Eur Urol. 2011;60:167–72.
Eid JF Penile Implant: Review of a “No-Touch” Technique. Sexual Medicine Reviews. 2016;4:294–300.
Montague DK. Periprosthetic infections. J Urol. 1987;138:68–9.
Carson CC, Robertson CN. Late hematogenous infection of penile prostheses. J Urol. 1988;139:50–2.
Krzastek SC, Smith R An update on the best approaches to prevent complications in penile prosthesis recipients. Ther Adv Urol. 2019;11:1–9.
Carvajal A, Benavides J, García-Perdomo HA, Henry GD Risk factors associated with penile prosthesis infection: systematic review and meta-analysis. Int J Impotence Res. 2020;32:587–97.
Mulcahy JJ. Current approach to the treatment of penile implant infections. Ther Adv Urol. 2010;2:69–75.
Gross MS, Phillips EA, Balen A, Eid JF, Yang C, Simon R, et al. The malleable implant salvage technique: infection outcomes after mulcahy salvage procedure and replacement of infected inflatable penile prosthesis with malleable prosthesis. J Urol. 2016;195:694–8.
Huiras P, Logan JK, Papadopoulos S, Whitney D. Local antimicrobial administration for prophylaxis of surgical site infections. Pharmacotherapy. 2012;32:1006–19.
Mandava SH, Serefoglu EC, Freier MT, Wilson SK, Hellstrom WJG. Infection retardant coated inflatable penile prostheses decrease the incidence of infection: a systematic review and meta-analysis. J Urol. 2012;188:1855–60.
Kowalewski M, Raffa GM, Szwed KA, Anisimowicz L. Meta-analysis to assess the effectiveness of topically used vancomycin in reducing sternal wound infections after cardiac surgery. J Thorac Cardiovasc Surg [Internet]. 2017;154:1320. https://doi.org/10.1016/j.jtcvs.2017.06.004.
Hamman BL, Stout LY, Theologes TT, Sass DM, Da Graca B, Filardo G. Relation between topical application of platelet-rich plasma and vancomycin and severe deep sternal wound infections after a first median sternotomy. Am J Cardiol. 2014;113:1415–9.
Lazar HL, Ketchedjian A, Haime M, Karlson K, Cabral H. Topical vancomycin in combination with perioperative antibiotics and tight glycemic control helps to eliminate sternal wound infections. J Thorac Cardiovasc Surg. 2014;148:1038–40.
Vander Salm TJ, Okike ON, Pasque MK, Pezzella AT, Lew R, Traina V, et al. Reduction of sternal infection by application of topical vancomycin. J Thorac Cardiovasc Surg. 1989;98:618–22.
Swanton A, Munarriz R, Gross MS. Updates in penile prosthesis infections. Asian J Androl. 2020;22:28–33.
Gross MS, Reinstatler L, Henry GD, Honig SC, Stahl PJ, Burnett AL, et al. Multicenter investigation of fungal infections of inflatable penile prostheses. J Sex Med. 2019;16:100–1105.
Tanner J, Norrie P, Melen K. Preoperative hair removal to reduce surgical site infection. Cochrane Database Syst Rev. 2011;11:CD004122.
Darouiche RO, Wall MJ, Itani KMF, Otterson MF, Webb AL, Carrick MM, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N. Engl J Med. 2010;362:18–26.
Pan S, Rodriguez D, Thirumavalavan N, Gross MS, Eid JF, Mulcahy J, et al. The Use of Antiseptic Solutions in the Prevention and Management of Penile Prosthesis Infections: A Review of the Cytotoxic and Microbiological Effects of Common Irrigation Solutions. J Sexual Med. 2019;16:781–90.
Sadeghi-Nejad H, Ilbeigi P, Wilson SK, Delk JR, Siegel A, Seftel AD, et al. Multi-institutional outcome study on the efficacy of closed-suction drainage of the scrotum in three-piece inflatable penile prosthesis surgery. Int J Impot Res. 2005;17:535–8.
Apoj M, Rodriguez D, Barbosa P, Pan S, Rajender A, Biebel M, et al. Closed suction drain outputs at 12 and 24 h after primary three-piece inflatable penile prosthesis surgery. Int J Impot Res. 2020;32:117–21.
Henry GD. The Henry mummy wrap and the Henry finger sweep surgical techniques. J Sex Med. 2009;6:619–22.
Wosnitzer MS, Greenfield JM. Antibiotic patterns with inflatable penile prosthesis insertion. J Sex Med. 2011;8:1521–8.
Lightner DJ, Wymer K, Sanchez J, Kavoussi L. Best practice statement on urologic procedures and antimicrobial prophylaxis. J Urol. 2020;203:351–6.
Sweet FA, Roh M, Sliva C. Intrawound application of vancomycin for prophylaxis in instrumented thoracolumbar fusions: efficacy, drug levels, and patient outcomes. Spine (Philos Pa 1976). 2011;36:2084–8.
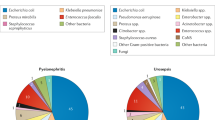
Gross MS, Phillips EA, Carrasquillo RJ, Thornton A, Greenfield JM, Levine LA, et al. Multicenter investigation of the micro-organisms involved in penile prosthesis infection: an analysis of the efficacy of the AUA and EAU Guidelines for Penile Prosthesis Prophylaxis. J Sex Med. 2017;14:455–63.
Lexicomp online, Pediatric and neonatal lexi-drugs online, Hudson, OH: Wolters Kluwer UpToDate, Inc.; 2020; 2020.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
RM, PM, and MG are consultants for Coloplast.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bearelly, P., D’Amico, M., Pan, S. et al. Intraoperative use of vancomycin paste during penile prosthesis placement: initial outcomes. Int J Impot Res 34, 81–85 (2022). https://doi.org/10.1038/s41443-020-00368-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-020-00368-6