Abstract
Molecular genetic testing of the FMR1 gene is commonly performed in clinical laboratories. Pathogenic variants in the FMR1 gene are associated with fragile X syndrome, fragile X–associated tremor ataxia syndrome (FXTAS), and fragile X–associated primary ovarian insufficiency (FXPOI). This document provides updated information regarding FMR1 pathogenic variants, including prevalence, genotype–phenotype correlations, and variant nomenclature. Methodological considerations are provided for Southern blot analysis and polymerase chain reaction (PCR) amplification of FMR1, including triplet repeat–primed and methylation-specific PCR.
The American College of Medical Genetics and Genomics (ACMG) Laboratory Quality Assurance Committee has the mission of maintaining high technical standards for the performance and interpretation of genetic tests. In part, this is accomplished by the publication of the document ACMG Technical Standards for Clinical Genetics Laboratories, which is now maintained online (http://www.acmg.net). This subcommittee also reviews the outcome of national proficiency testing in the genetics area and may choose to focus on specific diseases or methodologies in response to those results. Accordingly, the subcommittee selected fragile X syndrome to be the first topic in a series of supplemental sections, recognizing that it is one of the most frequently ordered genetic tests and that it has many alternative methods with different strengths and weaknesses. This document is the fourth update to the original standards and guidelines for fragile X testing that were published in 2001, with revisions in 2005 and 2013, respectively.
This version
Clarifies the clinical features associated with different FMRI variants (Section 2.3)
Discusses important reporting considerations (Section 3.3.1.3)
Provides updates on technology (Section 4.1)
Similar content being viewed by others
FX 1: INTRODUCTION
Disease-specific statements are intended to augment the current general American College of Medical Genetics and Genomics (ACMG) Technical Standards for Clinical Genetics Laboratories. Individual laboratories are responsible for meeting the CLIA/College of American Pathologists (CAP) quality assurance standards with respect to appropriate sample documentation, assay validation, general proficiency, and quality control measures.
FX 2: BACKGROUND ON FRAGILE X SYNDROME
FX 2.1: Gene symbol/chromosome locus
FMR1 is the gene symbol recognized by the Human Genome Organisation (HUGO) gene nomenclature committee.4 Historically, the locus was referred to as FXA. The chromosome locus is Xq27.3.
FX 2.2: OMIM number
The OMIM numbers are as follows: 309550 for the FMR1 gene, 300624 for fragile X syndrome (FXS), 311360 for fragile X–associated primary ovarian insufficiency (FXPOI), and 300623 for fragile X–associated tremor ataxia syndrome (FXTAS).5,6
FX 2.3: Brief clinical description
Pathogenic variants in the FMR1 gene cause a spectrum of disorders, each with a different pathophysiological mechanism leading to a corresponding phenotype ranging from neurodevelopmental problems in childhood to neurodegenerative issues with aging (Table 1). The features of FXS include varying degrees of cognitive deficits, seizures, and certain characteristic physical features such as macro-orchidism and large ears. While not all individuals with the premutation (alleles ranging from ≥55 to ≤200 CGG repeats) demonstrate FXS-related features, some with larger repeat sizes (>100–200 CGG repeats) have been identified with learning difficulties, prominent ears, neuropsychiatric disorders, or intellectual disabilities.6 Farzin et al. demonstrated a high rate of attention-deficit/hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) in boys with FXS.7 Females with premutations (usually in the range of >80–200 CGG repeats) have approximately a 20% risk for fragile X–associated primary ovarian insufficiency (FXPOI).8,9,10,11,12,13 There is no evidence to support an association between high normal and intermediate range (45–54 repeats) FMR1 alleles with a risk of FXPOI.14,15 Older males and females with premutations are at risk for fragile X–associated tremor/ataxia syndrome (FXTAS).16,17,18,19,20,21,22 FXTAS is a late-onset, progressive development of intention tremor and ataxia often accompanied by progressive cognitive and behavioral deterioration including memory loss, anxiety, reclusive behavior, deficits of executive function, and dementia. The phenotype of FXTAS gets more defined and prevalent with age and with premutation repeat length.23,24 Guidelines are available to identify individuals with FXTAS.25 Adults with heterozygote premutation alleles (both male and female) can express a spectrum of neuropsychiatric problems referred to as fragile X–associated neuropsychiatric disorders (FXAND).26 The symptoms include anxiety, depression, adult ADHD, addictive behaviors, chronic pain, and fibromyalgia. The risk for phenotypic findings is higher in males than in females with a premutation allele. For more information on these disorders, see the online GeneReviews profile for FMR1-related disorders (https://www.ncbi.nlm.nih.gov/books/NBK1384/) and the National Fragile X Foundation website (http://www.fragilex.org).
FX 2.4: Mode of inheritance
Inheritance of the FMR1 variant is X-linked, although the pattern of FXS is complicated due to the characteristics of the unstable repeat sequence. In typical fragile X families, the variant is a multistep expansion occurring over one or more generations in a region of CGG repeats in the 5’-untranslated region (UTR) of the gene. Small expansions are not generally associated with cognitive deficits in males and females. Large expansions (i.e., large premutations or full mutations) are fully penetrant in all males and many females (depending on X chromosome inactivation). With extremely rare exceptions,27 the parent of origin of the expansion to the full mutation is female.27,28
FX 2.5: Gene product and mutational mechanism
The gene product of the FMR1 gene is the fragile X mental retardation protein (FMRP), a widely expressed RNA-binding protein. FXS is caused by the deficiency or absence of FMRP. Theoretically, this can occur through any type of deletion or a single base pair change resulting in an inactivating variant, but in more than 99% of cases, there is an expansion of a segment of CGG repeats in the 5’ UTR of exon 1 of FMR1. Large CGG expansions in this region are associated with hypermethylation and inhibition of transcription resulting in the absence of FMRP.29 In individuals with a heterozygous premutation, FMR1 messenger RNA (mRNA) levels are increased, with higher CGG repeat numbers correlating with higher mRNA levels.30
FMRP is a selective RNA-binding protein that can form a messenger ribonucleoprotein complex and associate with polysomes.31 At the neuroanatomic level, the fragile X brain differs from a unaffected brain by the presence of unusually long and thin dendritic spines in the cortical regions.32,33 Excitatory synaptic transmission occurs at the dendritic spines and FMRP appears to associate with polyribosomes within dendritic spines of “wildtype” neurons.34 From these data, FMRP, which is shown to behave in vitro as an inhibitor of protein translation,35 is hypothesized to suppress translation of dendritic proteins in response to synaptic stimulation signals.36 There are no known forms of FMRP deficiency that do not map to the FMR1 gene. In the fragile X brain, therefore, translation of certain messages may be exaggerated because the normal inhibition provided by FMRP is absent.37
Studies of FMR1 mRNA expression provide evidence that expansion in the premutation range perturbs gene expression and may have pathophysiological consequences, particularly those related to FXTAS and FXPOI (see Section 2.3). Reductions in the amount of FMRP have been found in both lymphocytes and transformed lymphocytes of premutation heterozygotes.38 Using a highly sensitive fluorescent assay, Kenneson et al. demonstrated a decrement of FMRP in individuals with expansions only slightly larger than the upper edge of the normal range.30 The reduction in FMRP is associated with an increase in FMR1 mRNA in individuals with premutations.6,30,38,39 The understanding of the mechanisms involved in expansion of the CGG repeats into the premutation range and the effects of FMR1 transcription dysregulation continues to evolve.39,40,41,42
FX 2.6: Non-CGG repeat expansion variants in the FMR1 gene
Pathogenic variants other than the typical CGG repeat expansion have been described in the FMR1 gene, including single-nucleotide variants (missense and nonsense), splicing and regulatory substitutions, small deletions resulting in frameshift and premature truncation, several gross deletions, and one complex rearrangement, which could be detected by Sanger, exome, and genome sequencing; a growing list of these variants is available in ClinVar. Evidence suggests that intragenic FMR1 variants, although much less frequent than CGG repeat expansions, are also a mutational mechanism leading to FXS. Guidelines for detecting these relatively rare variants are beyond the scope of this document.
FX 2.7: Prevalence and ethnic association of common variants
FX 2.7.1: Full mutations
The genetics and clinical heterogeneity of FXS have made the diagnosis, and therefore the assessment of prevalence, challenging. All major ethnic groups and races appear to be susceptible to expansion of the FMR1 CGG region.38,40 Hunter and colleagues carried out a systematic literature review of 5,562 papers of which 54 were identified for inclusion, and a meta-analysis of the prevalence of expanded FMR1 alleles performed.43 Studies assessing three types of populations were considered: (1) total population studies that assessed the whole population without selection bias (these studies were typically screening studies of pregnant women and random newborns); (2) normal population studies that assessed healthy individuals without any intellectual disability (studies in the normal populations were used only to assess the carrier frequency of FMR1 variants in females, because these individuals are usually considered to be healthy); and (3) populations with intellectual disability being defined individually in each study. The 54 epidemiologic studies analyzed used only polymerase chain reaction (PCR) and Southern blot analysis for variant detection. The analysis included over 90,000 females and 50,000 males. The prevalence of the full mutation was 1.4 per 10,000 males and 0.9 per 10,000 females or 1:7,000 males and 1:11,111 females. Due to the 95% confidence intervals' overlap between males and females, it cannot be determined that individuals with the full mutation are more prevalent in males than females. The prevalence of premutation alleles among the general population was 1:300 females and 1:850 males. The frequency of individuals with the premutation allele in the healthy female population was the same as that in the total female population (34.4 per 10,000 or 1:291). Prevalence estimates for the full mutation from this meta-analysis are lower than those in previous reviews of FXS epidemiological data. Approximately 2.4% of individuals with intellectual disability identified in this study had the full mutation.43
FX 2.7.2: Premutations
Different studies have proposed a range of carrier frequencies across varied populations. While a study of 2,300 US women identified 1 in 382 as heterozygotes,44 a study of 119,000 individuals tested identified the premutation carrier frequency among US females to be 1 in 59.45 A larger study evaluating approximately 135,000 individuals across a self-reported ethnically diverse population identified a pan‐ethnic premutation carrier frequency of 1 in 201.46 A different study of 21,411 anonymous Canadian females (mothers of newborns) identified 1 in 549 as heterozygotes.47 Previous screens for the prevalence of premutations (with 55–101 repeats) in French-Canadian women estimated the carrier frequency to be 1 in 259.48 A subsequent study demonstrated a 1 in 1,760 prevalence of premutation alleles among Canadian males.49 A study from Israel of 36,483 women who requested screening identified 1 in 157 as heterozygotes.50 This result is consistent with an earlier study of 9,459 women in Israel that found 1 in 152 with alleles having >54 repeats.51 In the individuals with no family history of FXS, 1 in 113–152 women were determined to have premutations with a CGG repeat range of 55–101.52 This estimate of the premutation carrier frequency is approximately twofold higher than that reported in the studies performed in Canada. Toledano-Alhadef et al. obtained similar values when studying 14,334 preconceptual or pregnant women in Israel, namely, 1 in 113 women with >54 CGG repeats.53 This study excluded women with a family history of developmental delays. In addition, they found that the premutation heterozygotes were well distributed among all the Jewish ethnic groups, in contrast to a previous study.54 A fragile X screen of 10,000 newborn males in Taiwan showed a premutation prevalence of 1 in 1,674.55 Therefore the carrier frequencies vary widely among populations and may be higher than those determined in the French-Canadian population. Among females with FXPOI and simplex cases of adult males with cerebellar ataxia, the FMR1 premutation is identified in 4–6% and 2%, respectively.9,56,57,58
FX 2.8: Special testing considerations
FX 2.8.1: Sensitivity and specificity
CGG repeat expansion to full mutations account for >99% of cases of FXS. Therefore, PCR tests that effectively detect and measure the CGG repeat region (up to 200 repeats) of the FMR1 gene are >99% sensitive. As one report demonstrates there also appears to be an association between schizophrenia and mood disorders with low FMRP.59 FXS should not be confused with the unrelated syndrome associated with the FRAXE locus (MIM 309548/locus MIM 30086).
FX 2.8.2: Indications for testing
The ACMG and the American College of Obstetricians and Gynecologists (ACOG) as well as the National Society for Genetic Counselors (NSGC) have published practice guidelines with recommendations regarding fragile X testing for diagnostic testing and heterozygote detection.60,61,62,63,64 These include screening with the appropriate family history of intellectual disability suggestive of FXS or ovarian insufficiency or failure prior to age 40 years.60 Studies have demonstrated that the diagnostic yield of FX testing in males with intellectual disability and learning delay is about 2.5% and in individuals with autism is ~1.2% suggesting that FX testing may not be indicated as a first-tier test.65,66 The identification of a full mutation in a male is considered diagnostic rather than predictive, inasmuch as penetrance of FXS is virtually 100% in males and the age of onset is not variable. The identification of a full mutation in a female may be diagnostic, although <50% of females with full mutations have intellectual disability. They may have some other manifestations of the disease such as avoidance personality, mood, or stereotypic disorders.67,68 Nonrandom X-inactivation may explain the milder phenotype in females, although the extent of symptoms cannot be determined by X-inactivation patterns from diagnostic tests since they evaluate the expansion and methylation in blood and not the brain. The identification of a premutation in an asymptomatic male or female undergoing carrier testing (e.g., preconception carrier screening or due to a family history of intellectual disability) is predictive because FXPOI and FXTAS are not fully penetrant and are dependent on both age and allele size. Population carrier screening and newborn screening for FXS are somewhat controversial and not recommended at this time. It is important that clinicians and laboratorians alike refer to the ACMG/ACOG/NSGC guidelines referred above60,61,62,63,64 to make clinically relevant decisions.
FX 2.8.3: Prenatal testing
This test can be used for prenatal diagnosis in cells obtained from amniocentesis and chorionic villus sampling (CVS). Because methylation is not fully established at the time of CVS, the appearance of full mutations examined by a methylation-specific method may vary in CVS as compared with blood and amniocytes. Laboratories offering testing of chorionic villi must be aware of this tissue’s unique properties:
-
Methylation associated with lyonization is usually not present, and methylation associated with full mutations may or may not be present.69 In the past, the hypomethylated status of this locus in this tissue had been thought of as a limitation or possible source of confusion. However, because it is unwarranted to use methylation status or X-inactivation for phenotypic prediction of a full mutation, the possible hypomethylation of this tissue is no disadvantage, provided that the tissue-specific basis of the hypomethylation is understood.70,71 It is acceptable to omit methylation analysis entirely when testing CVS specimens. In the minor fraction of CVS cases with a result that is ambiguous between a large premutation and a small full mutation by size criteria alone, a follow-up amniocentesis may be required.
-
The degree of somatic variation in a full-mutation “smear” has a wider range of possibilities than is typically seen in blood specimens, from very limited to extraordinarily diffuse.
-
Mosaicism between trophoblasts and somatic cells is theoretically possible. For this reason, when CVS results indicate a premutation, a follow-up amniocentesis has been suggested to rule out mosaicism for a full mutation. However, there are currently no known occurrences of this type of mosaicism.
Genetic counseling regarding the potential limitations of CVS is recommended. Close contact with the laboratory accepting the specimen should be maintained before testing begins and throughout the testing process.
FX 2.9: Nomenclature
The use of standard nomenclature is important for the accurate communication of results to health-care providers and is recommended by the ACMG and CAP in accordance with Human Genome Variation Society (HGVS) recommendations. According to HGVS, regarding the nomenclature for short sequence repeats, the designation for the FMR1 triplet repeats varies based on whether the AGG interruptions are being evaluated or not. If the AGG interruptions are not being evaluated, then the designation for the FMR1 triplet repeats starting at position c.-129 based on the coding DNA reference sequence, NM_002024.5 is c.-129CGG[X] for a male, and c.-129CGG[X_X] for a female. The start of the variable repeat is specified by -129, and CGG indicates the sequence of the repeat unit. The number of triplet repeats present is specified by “X.” If the exact size of the repeat cannot be determined (e.g., full mutations sized by Southern blot analysis), then the square brackets are replaced by parenthesis, (X), to signify uncertainties.72 Current HGVS recommendations do not address nomenclature for nucleotide repeat variants with size mosaicism. Standard nomenclature is recommended, although laboratorians and clinicians may continue to use common variant nomenclature. To avoid confusion, it is acceptable to describe a variant using standard nomenclature followed by the common name in parentheses throughout the report or to use the standard and common name in the beginning of the report (e.g., results) and either the standard or common name subsequently.
FX 3: GUIDELINES
FX 3.1: Definition of normal and variant categories
There are four allelic forms of the gene: normal, intermediate, premutation, and full mutation (Table 2). The associated number of CGGs for each can be defined based on our current information to date. It must be recognized that the borders of each definition may change with increased empirical data and research as well as the variation observed in laboratories.73
FX 3.1.1: Normal alleles
Normal alleles have a range of ~5 to ≤44 repeats. The most common repeat length is 29 or 30 CGG repeats. Normal alleles rarely have meiotic or mitotic instability.74
FX 3.1.2: Intermediate (gray zone, inconclusive, borderline)
The range of repeats from ≥45 to ≤54 is considered intermediate (also referred to as gray zone, inconclusive, or borderline). Studies have shown that 7.7% of parents with FMR1 alleles in the 40–49 range and 25% of parents with FMR1 alleles in the 50–60 CGG repeat range are likely to pass a changed FMR1 allele to their children. Both expansion and contraction of the CGG repeat size were observed in the next generation.75 Alleles in this range can be considered normal in the sense that such alleles are not associated with FXS and have not been observed to expand to a full mutation in one generation. Although earlier studies suggested an association between alleles in this size range and FXPOI, larger subsequent studies did not support these initial findings.14,15 A small number of patients meeting the criteria for FXTAS with FMR1 intermediate alleles have been described, although larger studies are needed to determine the significance of this finding.76,77
Minor increases and decreases in repeat number can occur when alleles in the intermediate range are passed on, but there is no measurable risk of a child with FXS in the next generation. Alleles of this size may be associated with FXS in future generations or in distant relatives. Intermediate range alleles can be referred to as premutations if they are confirmed by family studies to be traceable to a known full mutation or unambiguous premutation. A gray zone allele of 52 repeats was reported to expand to a premutation allele of 56 repeats in one generation, which subsequently expanded to a full-mutation allele in the next generation.78 Testing at-risk relatives of individuals with an intermediate allele may determine the stability of the allele in the family. However, the rate of expansion of intermediate alleles is not well understood.74,79
FX 3.1.3: Premutation
Premutation alleles range from ≥55 to ≤200 repeats. These alleles are long repeat tracks that are unstably transmitted from parent to child. Expansions from the premutation size range to the full mutation typically occur during maternal transmission. Due to the possibility of somatic mosaicism, careful examination for mosaicism into the full-mutation range is recommended when a premutation is detected. FMR1 alleles in the premutation size range are not hypermethylated or associated with FXS. Although males and females with premutations and manifestations of some symptoms of FXS have been reported, further studies are needed.80 Women with premutation alleles are considered to be at risk for having affected children.75,81,82 The smallest FMR1 premutation allele reported to expand to a full mutation in a single generation is 56 repeats.78 Females who carry an FMR1 premutation should be offered prenatal diagnosis for all pregnancies. All at-risk family members of known heterozygotes should be offered testing to determine their status (Table 3).
FX 3.1.4: Full mutations
Full mutations have more than 200 repeats, typically several hundred to several thousand. There is usually broad somatic variation within each patient. Partial or complete promoter hypermethylation is typically seen in full mutations in most or all cases,83 except in the case of DNA extracted from CVS (see Section 2.8.3).
FX 3.1.5: Mosaicism
Size mosaics due to aneuploidy84 and methylation mosaics have been observed85,86,87,88,89 at the FMR1 CGG repeat region. When mosaicism is present, tissue-specific differences can be seen. Individuals with size or methylation mosaicism may be higher functioning than individuals with completely methylated full mutations.
FX 3.1.5.1: Size mosaics
This term refers to an individual with subpopulations of full mutations, which are methylated, and premutations, which are unmethylated. Occasionally, there also may be minor subpopulations with near-normal or normal length. For this reason, care must be taken in examining larger alleles when a normal or gray zone allele is detected using standard PCR methods.
FX 3.1.5.2: Methylation mosaics
This term refers to individuals with an FMR1 allele in the full-mutation size range, with subpopulations of cells containing an unmethylated full mutation and other populations of cells containing a methylated full mutation.
FX 3.1.6: AGG interruptions
In stable, normal alleles, the CGG region is interrupted by an AGG triplet after every 9 or 10 CGG repeats. The AGG triplets are thought to anchor the region during replication and prevent strand slippage. Premutation alleles, in contrast, are less likely to contain AGGs and have long stretches of uninterrupted CGGs at their 3’ end. The number of AGG interruptions helps predict the risk of expansion from premutations of <100 repeats to full mutations.90 Recent studies have demonstrated that premutation alleles with no AGGs are at risk for expansion to full mutations in the next generation while alleles that include AGG interruptions are associated with greater intergenerational stability of the repeat.74,82,90,91,92 More than 5,000 cases of normal, intermediate, and premutation alleles were surveyed to examine the relationship of the sex of the transmitting parent, repeat size, and pattern of AGG interruptions with allele instability.74 The instability was strongly influenced by the sex of the transmitting parent and by the number of repeats and location of the AGG interruptions in the parental allele.
Given the emerging role of AGG interruptions, determining the size of the repeat and the AGG interruption structure is relevant when performing family/prenatal counseling for women with premutations. Smaller repeat lengths and the presence of at least two AGGs decrease the risk of expansion in the next generation.92,93 Although not routinely performed, direct testing for the AGG triplets can be interrogated via triplet repeat–primed PCR (TP-PCR) or long-read single-molecule sequencing,79,92,94 and is available clinically in a limited number of laboratories.
FX 3.2: Methodological considerations
All general guidelines for Southern blot analysis and PCR in the ACMG Technical Standards for Clinical Laboratories apply. The following additional details are specific for fragile X testing. For this test, there are many valid methods with different strengths and weaknesses. Laboratories will likely need to use more than one method because no single method can characterize all aspects of the FMR1 full mutation, and precision in determining allele size varies between PCR and Southern blot analysis. For mosaic samples spanning the premutation and full-mutation ranges, traditional PCR may amplify the premutation population but not the subpopulation with the full mutation. The expected phenotype for an individual with a premutation versus mosaicism for a premutation and full mutation is very different. Therefore, not detecting the full mutation would result in a different risk assessment for fragile X, FXTAS, and FXPOI,60 resulting in the previous recommendation to always perform Southern blot analysis along with traditional PCR.3 Newer repeat-primed PCR methods or methylation PCR reduce the need to perform Southern blot analysis (see Section 3.2.2.7) on every sample. Additionally, because the fragile X assay is technically challenging due to high GC content, varying size repeats, and size limitations of conventional PCR and Southern blot (especially in the case of small premutations, or unmethylated normal alleles), it is important to ensure that appropriate controls are used while processing clinical samples. Characterized reference material possessing specific FMR1 premutation and full-mutation CGG repeat sizes that can be used across different methodologies95 may be obtained from the CDC Genetic Testing Reference Materials (GeT-RM) Program (https://www.cdc.gov/labquality/get-rm/index.html) through the Coriell Institute for Medical Research (https://www.coriell.org/).
FX 3.2.1: Southern blot analysis
FX 3.2.1.1: Probe and restriction site combinations
Supplemental Table 1 describes several single- and double-enzyme options that are commonly used as well as several probes that are available for this analysis.96,97,98,99 In general, when using the StB12.3 probe, small premutations are more easily detected when the normal fragment is small and/or electrophoretic migration is long, whereas large/diffuse full mutations are more easily detected when the normal fragment is large and/or electrophoretic migration is short. Other restriction enzymes and probes can be used, if equivalence is demonstrated. Probes can be embedded in plasmid DNA and isolated using a plasmid preparation procedure. They can be generated using PCR amplification, or they can be purchased commercially.
FX 3.2.1.2
Controls should be included to confirm the proper choice and activity of restriction enzymes and probe. They should ideally represent the more difficult to recognize genotypes. To verify digestion and hybridization parameters, a normal control will suffice. However, in fragile X blot analyses, the abnormal controls are extremely important because they provide quality control on the resolution of small premutations and the detectability of diffuse smears. Refer to Section 3.2 for a discussion of reference materials. Laboratories should use verified reference materials95 to confirm their results.
FX 3.2.1.3
For female patients, it should be noted that the degree of separation between two differently sized normal alleles could appear identical to that between a normal and a premutation allele (e.g., 20 and 44 repeats vs. 35 and 59 repeats). A Southern blot analysis with superior resolution and appropriate size standards or controls is required to distinguish between these possibilities (Fig. 1). Alternatively, most PCR-based methods can provide the required resolution. Similar considerations apply to detection of premutation alleles in normal transmitting males.
1: Normal female. 2: Full-mutation male; note the combination of a predominant band with a diffuse smear. 3: Female with 28 and 52 repeats, with the smaller allele predominantly active. 4: Female with 26 and 52 repeats, with the larger allele predominantly active. 5: Female with 18 and ~80 repeats, with equal X-inactivation. 6: Normal male. 7: Normal male, underloaded due to DNA degradation (the apparent line between lanes 6 and 7 is a photographic artifact). 8: Normal female. 9: Normal male. 10: Normal male. 11: Affected male, underloaded and very diffuse. 12: Premutation male. 13: Female with 20 and 70 repeats, with the smaller allele virtually exclusively active (the only evidence of abnormality is the slow migration of the “5.2 kb” band). 14: Female with 27 and 42 repeats, with the larger allele somewhat more active. 15–17: Unremarkable normal females and male. Figure provided by Genetics & IVF Institute. Reprinted from Maddalena et al.2
FX 3.2.1.4
Because full mutations can be extremely diffuse and faint, signal to noise ratios must be very good. Laboratories are advised to be aware of the many different appearances of full mutations. Full mutations are not likely to be overlooked in males, inasmuch as the normal signal will be absent (or light, in size mosaics), but full mutations can be easily missed in females if the background is poor. Skewed X-inactivation may also present problems in the use of Southern blot analyses performed with methylation-sensitive restriction enzymes in the detection of females with premutations or full mutations.
FX 3.2.1.5
Migration distances should be interpreted using a standard ladder such as lambda Hind III fragments or a set of carefully chosen, independently tested human references.
FX 3.2.1.6
The following guidelines refer to methylation analysis using two different restriction enzymes, one of which is methylation-sensitive.
FX 3.2.1.6.1: In DNA extracted from tissues other than chorionic villi, methylation analysis reveals the degree of hypermethylation in full mutations and shows the distribution of X-inactivation in any female with two distinguishable alleles. Southern blot analysis with the addition of methylation-sensitive enzyme digestion can
-
Help discriminate between premutations and full mutations for the rare alleles that fall near the boundary (i.e., around 200 repeats).
-
Detect rare individuals who are methylation mosaics.
FX 3.2.1.6.2: In DNA extracted from tissues other than chorionic villi, the results of routine methylation analysis and PCR are sometimes confounded by an abnormal karyotype such as 45,X or 47,XXY. Individuals with testicular feminization (XY females) will have a male methylation pattern. In these cases, sex chromosome constitution should be confirmed. Interpretation of results should take the individual’s karyotype into account, when it is available to the molecular laboratory.
FX 3.2.1.6.3: In DNA extracted from tissues other than chorionic villi, methylation analysis increases the difficulty of detecting females with small premutations who have highly skewed X-inactivation. Double digestion with a methylation-sensitive restriction enzyme causes the signal from each allele in a female to be split into active and inactive bands, forming four bands in a heterozygous female. When X-inactivation is balanced in a heterozygote, the two active bands are readily seen, although the two inactive bands may co-migrate. However, if X-inactivation is heavily skewed, there may be only two visible bands of the predominant X population. This result is challenging to interpret particularly when the premutation is predominantly inactive because then it appears only in the upper region of the gel, where resolution is considerably poorer. For an example of a heterozygote with extremely skewed X-inactivation, see lane 13 of Fig. 1. Lanes 3 and 4 show two females with oppositely skewed X-inactivation. The above data are true for the use of the StB12.1 probe. Use of other probes such as pE5.1 will yield an additional small control band.
FX 3.2.1.6.4: FMR1 methylation status should not be used to predict severity in fetal or newborn cases, regardless of whether the DNA was extracted from amniocytes, chorionic villi, or blood.
FX 3.2.1.6.5: In DNA extracted from chorionic villi, the FMR1 region usually does not have methylation associated with X-inactivation, and it may or may not have hypermethylation associated with full mutations if the CVS procedure was performed before 12.5 weeks’ gestation.69 When testing DNA extracted from chorionic villi, methylation analysis is optional. Incidentally, methylation analysis before 12.5 weeks of gestation can serendipitously alert a laboratory to maternal cell contamination in chorionic villus specimens. Inasmuch as methylation associated with X-inactivation is usually not present at this locus in tissue obtained via CVS, a strong normal inactive band can be a sign of possible maternal cell contamination. Other explanations for such a band include X-inactivation in some fetal cells or incomplete digestion. Further investigation is merited in such cases.
FX 3.2.2: PCR methods
FX 3.2.2.1
Several sets of primers, PCR conditions, and methods of separation and detection have been published.100,101,102,103 Other primers and methods can be used if equivalence is demonstrated, keeping in mind regions such as deletion hotspots, particularly in primer design. PCR can be performed by incorporating a fluorescently labeled primer followed by capillary electrophoresis (CE). Regardless of the locus, any PCR can theoretically fail to detect an allele if there is a polymorphism at the primer binding site. There are no known polymorphisms that would affect any of the commonly used primers. Patient amplicon sizes should be determined using a size standard. For CE, a standard fluorescently labeled size marker can be used.
FX 3.2.2.2
Controls representing the genotypes to be distinguished should be used for each run. Refer to Section 3.2 for information on reference materials. The upper limit of allele size that can be successfully detected should be known, and a control corresponding to that size should be included in each run. Laboratories should confirm the size of their control DNA by sequencing (if possible) or by using verified reference materials.95
FX 3.2.2.3
Amplification of GC-rich regions is difficult, and special conditions are required. The difficulty increases with increasing numbers of CGG repeats; therefore, many PCR strategies do not attempt to detect large alleles. In such a system, it is not possible to tell the difference between a female who is homozygous for a normal allele and one who has a large nonamplifiable second allele. Similarly, patients who are mosaics for premutations and full mutations may appear to have only premutations.
FX 3.2.2.4
When a PCR strategy can detect large alleles, amplification nevertheless may favor the smaller allele in any specimen with multiple alleles, i.e., females and mosaics. Such methods should be validated with heterozygous females and mosaics, in addition to males. Because of disproportionate amplification, PCR is not reliable for determining the ratio of different species in a mosaic individual. In PCR amplification of samples from females and mosaics, heteroduplexes can form due to technical artifacts, particularly if denaturing gels are used and should be duly considered.
FX 3.2.2.5
Basic PCR amplification is not affected by methylation. Although PCR tests specifically modified to detect methylation status have been described,104,105 the original PCR strategies that have been in use for many years are completely independent of methylation.
FX 3.2.2.6
When a PCR strategy is used to detect full mutations, the presence of a deletion hotspot in the CGG repeat region should be noted.106 Primers located within the deletion hotspot may result in failure to detect the expanded allele. Primers located upstream of the deletion hotspot may result in apparent size mosaicism.
FX 3.2.2.7: Triplet repeat–primed PCR
FX 3.2.2.7.1: TP-PCR allows rapid detection of PCR products formed by a chimeric primer binding inside a triplet repeat region. In TP-PCR for fragile X, one primer is anchored completely outside of the CGG repeat region, whereas the other overlaps the CGG repeat and the adjacent nonrepeated sequence. A third primer can be anchored outside of the CGG region that, when paired with the opposite anchored primer, will amplify “over” the CGG repeat. This will increase the amount of full-length product from the largest CGG repeat allele and in some assays enables accurate sizing of alleles up to 200 CGG repeats. From the chimeric primer annealing at each CGG repeat, multiple amplicons are made, forming products each with a length differing by three bases. The application of TP-PCR for fragile X testing has been described in multiple studies.107,108,109,110,111,112,113
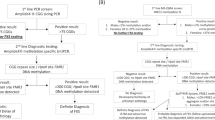
FX 3.2.2.7.2: Although products can be separated by ethidium bromide–stained agarose gels to detect “smears,” combining TP-PCR with single base resolution fragment analysis, the “smear” on a lower resolution agarose gel becomes characteristic “stutters” or “ladders” that are easily visualized. The stuttering will end at the allele with the greatest number of CGG repeats. An increase of this product can be seen, particularly if the third primer is used. For alleles with >200 repeats, a “compression” product can be seen, which can be used as a marker for an allele with >200 repeats, although the fragment cannot be sized (Fig. 2a). If a third primer is used, full mutations appear as a compression (or compacted) product. These are seen by CE as a compacted product of ~200 CGG repeats, thereby indicating a full mutation (Fig. 2b).
Triplet repeat–primed polymerase chain reaction (TP-PCR) using a two-primer system (a) and a three-primer system (b). (a) Top panel: female with 20 and 31 CGG repeats. Middle panel: male with 103 CGG repeats. Bottom panel: male with size mosaicism from ~140 to 800 CGG repeats (inset: reduced y-axis to better visualize baseline). (b) Left panel: male with 32 CCG repeats. Middle panel: female with 20 and 64 CGG repeats. Right panel: female with 29 and >200 CGG repeats.
FX 3.2.2.7.3: PCR followed by CE at a single base resolution has a high analytical sensitivity and specificity for detecting expanded alleles. A threshold can be set to distinguish premutation and full-mutation (and intermediate, if desired) alleles from normal alleles. If no expansion is detected, no further testing is necessary. Alleles with a stuttering pattern past a threshold (>150 repeats) and consistent with an expansion can be tested further to determine methylation status (by Southern blot analysis or methylation-sensitive PCR) or to determine size (traditional PCR and/or Southern blot analysis). Therefore, the simple yes/no answer for the presence of expansions can eliminate the need for Southern blot analysis in samples with normal sized and intermediate sized FMR1 allele(s).
FX 3.2.2.7.4: TP-PCR resolves the challenges associated with apparent homozygous females, because the normal allele will not outcompete the expanded allele. The increased sensitivity of the TP-PCR assay also resolves the difficulty of detecting mosaic males because mosaicism can be detected up to ~10%.109,110 Laboratories using TP-PCR are encouraged to define the sensitivity of their assay using DNA with a normal FMR1 allele titrated with serial dilutions of full-mutation FMR1 DNA.
FX 3.2.2.7.5: Controls for various stages of processing need to be included as part of the testing workflow, including a no DNA control, a sensitivity control (particularly for the detection of mosaics and full expansions), and a rotating group of patient controls of different genotypes or by using verified reference materials.95 Refer to Section 3.2 for information on reference materials.
FX 3.2.3: Non–Southern blot methods for methylation detection
FX 3.2.3.1: Methylation-specific PCR
Several methods besides Southern blot analysis have been described to determine methylation. Methylation-specific PCR involves the differential treatment of DNA with methylation-specific restriction enzymes followed by allele-specific PCR and resolution of the PCR products with CE.108,113 This method not only determines methylation status but also FMR1 allele size up to 250 repeats; however, to size alleles with >250 repeats accurately, Southern blot analysis is needed.
FX 3.2.3.2: Multiplexed ligation probe amplification (MLPA)
MLPA has been described to identify males with methylated fragile X alleles.114 In this method, sequence-specific probes are hybridized to methylated and unmethylated alleles. Probes are simultaneously ligated and digested with a methylation-sensitive restriction endonuclease. A universal PCR primer set will amplify only probes that are ligated and undigested, indicating methylated alleles.
FX 3.2.3.3: Real-time PCR
Real-time PCR has also been described with TaqMan chemistry and by melt curve analysis, using methylation-specific PCR. TaqMan chemistry amplification separates methylated and unmethylated specific alleles and provides a ratio based on amplification cycle thresholds. Using melt analysis, however, methylated and unmethylated alleles are amplified simultaneously due to differences of GC content, but this can be resolved by differences in melting temperature between methylated and unmethylated alleles.115 These methods have high analytical sensitivity and specificity for detecting methylation in males but are less sensitive and specific in females.
FX 3.3: Interpretations
FX 3.3.1
In addition to the items described in the general ACMG Technical Standards for Clinical Genetics Laboratories (https://www.nature.com/gim/articles?type=acmg-standards-and-guidelines), the following elements should be included in the report.
FX 3.3.1.1
State whether the method used was PCR, Southern blot analysis, or both. If Southern blot analysis is the method of evaluation, state the restriction enzymes and probes that were used. If PCR, describe the PCR method used (e.g., TP-PCR) and method used for separation and detection (e.g., CE).
FX 3.3.1.2
State the ranges (per literature and guidelines) and analytical precision (as determined by the testing laboratory during validation) for the different categories of normal, intermediate (gray zone, borderline, inconclusive), premutation, and full mutation.
FX 3.3.1.2.1: Note that it is not necessarily obvious that the borderline category (intermediate/gray) refers to the border between normal and premutation and not to the border between premutation and full mutation. Similarly note that the term instability, which is often used regarding borderline allele calls to describe minor intergenerational or mitotic changes, may unintentionally suggest a risk of having an affected child or personal late-onset symptoms.
FX 3.3.1.3
Classify the patient’s result using the defined categories and HGVS nomenclature (refer to Section 2.9). Common nomenclature can be included for clarity. The term size mosaic should be used for alleles that have significant subpopulations in both the premutation and full-mutation range. Caution is needed not to suggest that a sample with size mosaicism has multiple alleles. The term subpopulation of an allele is recommended. See Table 3 for example interpretation paragraphs for use in reporting.
FX 3.3.1.4
All positive results should state that genetic counseling is recommended, and testing is available for at-risk family members.
FX 3.3.2: The following descriptive elements may appear, with caution:
FX 3.3.2.1
The size of the alleles may be reported and could be of clinical use for individuals who are heterozygous for the premutation. The premutation allele size may be used for risk assessment in determining the chance of expansion in the offspring of these individuals and in determining the chance of FXTAS or FXPOI. If so, the precision used in quoting the size must be supportable by the precision of the size marker used, the sharpness of the bands or peaks, degree of stutter, and so on. It may be appropriate to state a range or use qualifying terms such as “approximately.” Descriptions such as “positive for an allele with 55–200 repeats” are ambiguous and should not be included on the laboratory report.
The CAP/ACMG Biochemical and Molecular Genetics Resource Committee published results of laboratory performance on the CAP proficiency surveys for molecular genetic testing for fragile X conducted between 2001 and 200973 and the acceptable range for sizing CGG repeats for fragile X is based on these results. Acknowledging the technical limitations of size analysis, the ACMG supports the following grading criteria for the CAP/ACMG proficiency testing survey: consensus size ±5 repeats for alleles with <55 repeats, consensus size ±10 repeats for alleles with 56–100 repeats, and consensus size ±2 SDs for alleles with >100 repeats.
FX 3.3.2.2
Description of methylation may be provided. The two kinds of methylation must be clearly distinguished: methylation due to X-inactivation and hypermethylation of full mutations. The term methylation mosaic or incomplete methylation may be used if not all molecules in a full mutation are hypermethylated.
FX 3.3.2.3: Occasionally unexpected patterns are seen that may not fit within the descriptions provided here. In those cases, a detailed description may be helpful. For example, methylation PCR may exhibit a pattern of size and methylation mosaicism with subpopulations of premutations (<200 CGG repeats), which are methylated, and full mutations (>200 CGG repeats), which are unmethylated.
FX 3.3.3: Helpful points on alternative diagnoses may be included
FX 3.3.3.1
There are rare forms of FMRP deficiency not caused by CGG expansion, which may not be detected by this test.
FX 3.3.3.2
Intellectual disability associated with other fragile X sites, FRAXE, or other gene variants will not be detected with this test.
FX 3.3.3.3
DNA analysis for FXS should be performed as part of a comprehensive genetic evaluation that includes chromosomal microarray and a five-cell screen for chromosome rearrangement analysis as recommended by ACMG.116,117
FX 3.3.4
Comments on phenotype, if included, should be abstract rather than case specific. The following concepts apply:
FX 3.3.4.1
All males with full mutations have FXS to some degree. The severity cannot be predicted from the size of the full mutation, but if premutations are also present or if the majority of the full-mutation molecules are unmethylated, the phenotype may be less severe.
FX 3.3.4.2
Females with full mutations exhibit a wide spectrum of phenotypes. They may be as severely affected as a male with an expanded fragile X allele (which is itself a range of phenotypes). Females with full mutations may also exhibit very mild learning disabilities or have no detectable deficits. The severity cannot be predicted from the size of the full mutation, nor can it be predicted from the pattern of X-inactivation in blood.
FX 3.3.4.3
Individuals with heterozygous premutations should not be interpreted as unaffected. Females who carry a premutation are at risk for FXPOI and FXTAS. Males with the premutation are at risk for FXTAS. Both sexes are at risk for FXAND. If an individual referred for diagnostic testing due to intellectual disability, autism, or learning disability is found to carry a premutation, the upper end of the premutation is often associated with these problems, because FMRP levels are lower than normal above 120 repeats. FMRP deficiency or mosaicism for a full mutation can be detected.
FX 3.3.4.4
Individuals with intermediate alleles should be interpreted as unaffected. Even more so than a premutation, an intermediate allele is considered a coincidence when found in an individual referred for diagnostic testing due to intellectual disability, learning disability, or autism. FMRP deficiency or mosaicism for a full mutation can be investigated by methylation-sensitive Southern blot analysis but with less likelihood of success because intermediate alleles are common in the general population.
FX 3.3.5
Comments on reproductive risk, if included, should be abstract rather than case specific. The following concepts apply:
FX 3.3.5.1
All affected males and most affected females inherit their variant from their mothers. Mothers carry either a premutation or full-mutation allele. Females with heterozygous premutations may have inherited their FMR1 allele from either their mother or father.
FX 3.3.5.2
Women with full mutations have a theoretical 50% chance of passing on the full mutation with each pregnancy.
FX 3.3.5.3
Women with premutations have a 50% chance of passing on the fragile X variant with each pregnancy. If it is passed on, the chance the allele will increase to a full mutation depends on its size in the mother and the number of AGG interruptions. Probabilities range from 3% for maternal alleles with CGG repeats from 55 to 59 (1/23 transmissions) to ~100% for maternal alleles with 90 CGGs and above.75 The smallest allele known to expand to the full mutation is 56 repeats.64 Laboratories should be familiar with publications on this topic,75,81,82,102,118 including any current publications.
FX 3.3.5.4
Men with premutations will almost always pass premutation alleles to all their daughters. An extremely rare phenomenon involves males with premutations who have had daughters with full mutations, apparently due to gonadal mosaicism for full mutations.119,120,121 The sons of men with the premutation are not at risk for developing the FXS or FXTAS since they inherit their father’s Y chromosome.
FX 3.3.5.5
To date, there have been no reports of males or females with heterozygous intermediate alleles having offspring with an FMR1 allele in the full-mutation range. Instability may be identified if the allele can be traced through the family to a known full mutation or unambiguous premutation. In the absence of such a connection, it may be possible to show meiotic instability or a specific repeat sequence pattern (absence of AGG interruptions) that is at higher risk for instability. Testing for AGG status is available in a limited number of laboratories.
FX 4: ALTERNATIVE TESTING METHODS
FX 4.1: Next-generation sequencing (NGS)
Testing for FMR1 repeats is included in expanded carrier testing using NGS for multiple genes. Inherent limitations of short read NGS technology include difficulties sequencing across GC-rich regions, ineffective mapping of repetitive elements, and in the case of capture-based technology, PCR amplification bias of smaller alleles compared to larger full-mutation FMR1 alleles. To combat these constraints, multiple algorithms have been designed to identify clinically relevant repeat expansions from short read sequence data. However, these attempts demonstrated poor sensitivity and specificity performance in detection of FMR1 expanded alleles.122,123 Currently, short read NGS technology cannot reliably detect expanded FMR1 alleles and should not be used to rule out or confirm any FMR1-related disorders. Advances in genome testing, using PCR-free methods, reduces some of the difficulties in sequencing through repetitive regions. Combined with new analysis software, repeat disorders may be identified from PCR-free genomes,124,125,126 although genome sequencing for fragile X is cost prohibitive for expanded carrier testing. In those applications, FMR1 testing is often performed separately.
Single-molecule, real-time (SMRT) long-read sequencing is able to sequence through a full-mutation allele of 750 CGG repeats (~2 kb) and may be used to distinguish the number and location of AGG interruptions.94,127 Long-read technology is not yet widely available for clinical use, though this may change as error rate and costs decrease, and more bioinformatics tools become available for clinical application. Currently, TP-PCR and Southern blot methods remain the gold standards for identification of expanded FMR1 alleles and CGG repeat quantification.
FX 4.2: Cytogenetic evaluation
Testing for the fragile site FRAXA at Xq27 is no longer an acceptable diagnostic method. Clinical and analytical specificity and sensitivity are both insufficient.
FX 4.3: Protein analysis
Immunohistochemical staining for FMRP is a valid diagnostic method in lymphocytes.71 Willemsen et al. demonstrated that staining for the FMRP protein in chorionic villus samples could be used as an alternative prenatal diagnostic method for detection of full mutations in male fetuses.69 The situation is more complicated in female fetuses for which some chorionic villi may be completely positive and others from the same sample may be completely negative for FMRP staining. The authors’ data shed light on the timing of X-inactivation in chorionic villus cells of the female fetus. The diagnostic application of this method is not recommended at this time for the prenatal diagnosis of females carrying FMR1 full mutations.
FX 5: Policy statements
FX 5.1
The American College of Medical Genetics and Genomics issued a policy statement titled Fragile X Syndrome: Diagnosis and Carrier Testing in 1994,128 which was updated in October 2005.63 This document is also available online (http://www.acmg.net). These Standards are in general agreement with that statement.
FX 5.2
The NSGC also published practice guidelines to assist genetic counselors in providing accurate risk assessment and appropriate educational and supportive counseling for individuals with positive test results and families affected by FMR1-associated disorders.64 Additionally, in 2017, ACOG issued a Committee Opinion, No. 691, on carrier screening for genetic conditions, including fragile X syndrome.60 The Standards presented here are in general agreement with those opinions.
References
Maddalena, A. et al. Technical standards and guidelines for fragile X: the first of a series of disease-specific supplements to the Standards and Guidelines for Clinical Genetics Laboratories of the American College of Medical Genetics. Genet. Med. 3, 200–205 (2001).
Spector, E. & Kronquist, K. Technical standards and guidelines for fragile X testing: a revision to the disease-specific supplements to the Standards and Guidelines for Clinical Genetics Laboratories of the American College of Medical Genetics. 2005 (online publication) (retired).
Monaghan, K. G. et al. ACMG Standards and Guidelines for fragile X testing: a revision to the disease-specific supplements to the Standards and Guidelines for Clinical Genetics Laboratories of the American College of Medical Genetics and Genomics. Genet. Med. 15, 575–586 (2013).
Yates, B. et al. Genenames.org: the HGNC and VGNC resources in 2017. Nucleic Acids Res. 45, D619–D625 (2017).
Online Mendelian Inheritance in Man. https://omim.org (2020).
Tassone, F. et al. Clinical involvement and protein expression in individuals with the FMR1 premutation. Am. J. Med. Genet. 91, 144–152 (2000).
Farzin, F. et al. Autism spectrum disorders and attention-deficit/hyperactivity disorder in boys with the fragile X premutation. J. Dev. Behav. Pediatr. 27, S137–144 (2006).
Hundscheid, R. D. L., Smits, A. P. T., Thomas, C. M. G., Kiemeney, L. A. L. M. & Braat, D. D. M. Female carriers of fragile X premutations have no increased risk for additional diseases other than premature ovarian failure. Am. J. Med. Genet. A. 117A, 6–9 (2003).
Sherman, S. L. Premature ovarian failure in the fragile X syndrome. Am. J. Med. Genet. 97, 189–194 (2000).
Murray, A., Ennis, S. & Morton, N. No evidence for parent of origin influencing premature ovarian failure in fragile X premutation carriers. Am. J. Hum. Genet. 67, 253–254 (2000). author reply 256-258.
Murray, A. Premature ovarian failure and the FMR1 gene. Semin. Reprod. Med. 18, 59–66 (2000).
Marozzi, A. et al. Association between idiopathic premature ovarian failure and fragile X premutation. Hum. Reprod. 15, 197–202 (2000).
Wittenberger, M. D. et al. The FMR1 premutation and reproduction. Fertil. Steril. 87, 456–465 (2007).
Spath, M. A. et al. Predictors and risk model development for menopausal age in fragile X premutation carriers. Genet. Med. 13, 643–650 (2011).
Bennett, C. E., Conway, G. S., Macpherson, J. N., Jacobs, P. A. & Murray, A. Intermediate sized CGG repeats are not a common cause of idiopathic premature ovarian failure. Hum. Reprod. 25, 1335–1338 (2010).
Tassone, F. et al. Intranuclear inclusions in neural cells with premutation alleles in fragile X associated tremor/ataxia syndrome. J. Med. Genet. 41, e43 (2004).
Rogers, C., Partington, M. W. & Turner, G. M. Tremor, ataxia and dementia in older men may indicate a carrier of the fragile X syndrome. Clin. Genet. 64, 54–56 (2003).
Rodriguez-Revenga, L. et al. Penetrance of FMR1 premutation associated pathologies in fragile X syndrome families. Eur. J. Hum. Genet. 17, 1359–1362 (2009).
Jacquemont, S. et al. Penetrance of the fragile X–associated tremor/ataxia syndrome in a premutation carrier population. JAMA. 291, 460–469 (2004).
Jacquemont, S. et al. Fragile X premutation tremor/ataxia syndrome: molecular, clinical, and neuroimaging correlates. Am. J. Hum. Genet. 72, 869–878 (2003).
Hagerman, R. J. et al. Fragile-X-associated tremor/ataxia syndrome (FXTAS) in females with the FMR1 premutation. Am. J. Hum. Genet. 74, 1051–1056 (2004).
Hagerman, P. J., Greco, C. M. & Hagerman, R. J. A cerebellar tremor/ataxia syndrome among fragile X premutation carriers. Cytogenet. Genome Res. 100, 206–212 (2003).
Tassone, F. et al. CGG repeat length correlates with age of onset of motor signs of the fragile X–associated tremor/ataxia syndrome (FXTAS). Am. J. Med. Genet. B Neuropsychiatr. Genet. 144B, 566–569 (2007).
Leehey, M. A. et al. FMR1 CGG repeat length predicts motor dysfunction in premutation carriers. Neurology. 70, 1397–1402 (2008).
Berry-Kravis, E. et al. Fragile X–associated tremor/ataxia syndrome: clinical features, genetics, and testing guidelines. Mov. Disord. 22, 2018–2030 (2007). quiz 2140.
Hagerman, R. J. et al. Fragile X–associated neuropsychiatric disorders (FXAND). Front. Psychiatry. 9, 564 (2018).
Alvarez-Mora, M. I. et al. Paternal transmission of a FMR1 full mutation allele. Am. J. Med. Genet. A. 173, 2795–2797 (2017).
Fisch, G. S. et al. The fragile X premutation in carriers and its effect on mutation size in offspring. Am. J. Hum. Genet. 56, 1147–1155 (1995).
Sutcliffe, J. S. et al. DNA methylation represses FMR-1 transcription in fragile X syndrome. Hum. Mol. Genet. 1, 397–400 (1992).
Kenneson, A., Zhang, F., Hagedorn, C. H. & Warren, S. T. Reduced FMRP and increased FMR1 transcription is proportionally associated with CGG repeat number in intermediate-length and premutation carriers. Hum. Mol. Genet. 10, 1449–1454 (2001).
O’Donnell, W. T. & Warren, S. T. A decade of molecular studies of fragile X syndrome. Annu. Rev. Neurosci. 25, 315–338 (2002).
Irwin, S. A., Galvez, R. & Greenough, W. T. Dendritic spine structural anomalies in fragile-X mental retardation syndrome. Cereb. Cortex. 10, 1038–1044 (2000).
Hinton, V. J., Brown, W. T., Wisniewski, K. & Rudelli, R. D. Analysis of neocortex in three males with the fragile X syndrome. Am. J. Med. Genet. 41, 289–294 (1991).
Feng, Y. et al. Fragile X mental retardation protein: nucleocytoplasmic shuttling and association with somatodendritic ribosomes. J. Neurosci. 17, 1539–1547 (1997).
Li, Z. et al. The fragile X mental retardation protein inhibits translation via interacting with mRNA. Nucleic Acids Res. 29, 2276–2283 (2001).
Bardoni, B. & Mandel, J. L. Advances in understanding of fragile X pathogenesis and FMRP function, and in identification of X linked mental retardation genes. Curr. Opin. Genet. Dev. 12, 284–293 (2002).
Aschrafi, A., Cunningham, B. A., Edelman, G. M. & Vanderklish, P. W. The fragile X mental retardation protein and group I metabotropic glutamate receptors regulate levels of mRNA granules in brain. Proc. Natl. Acad. Sci. U. S. A. 102, 2180–2185 (2005).
Tassone, F. et al. Elevated levels of FMR1 mRNA in carrier males: a new mechanism of involvement in the fragile-X syndrome. Am. J. Hum. Genet. 66, 6–15 (2000).
Tassone, F., Hagerman, R. J., Chamberlain, W. D. & Hagerman, P. J. Transcription of the FMR1 gene in individuals with fragile X syndrome. Am. J. Med. Genet. 97, 195–203 (2000).
Beilina, A., Tassone, F., Schwartz, P. H., Sahota, P. & Hagerman, P. J. Redistribution of transcription start sites within the FMR1 promoter region with expansion of the downstream CGG-repeat element. Hum. Mol. Genet. 13, 543–549 (2004).
Galloway, J. N. & Nelson, D. L. Evidence for RNA-mediated toxicity in the fragile X–associated tremor/ataxia syndrome. Future Neurol. 4, 785 (2009).
Sellier, C. et al. Translation of expanded CGG repeats into FMRpolyG is pathogenic and may contribute to fragile X tremor ataxia syndrome. Neuron. 93, 331–347 (2017).
Hunter, J. et al. Epidemiology of fragile X syndrome: a systematic review and meta-analysis. Am. J. Med. Genet. A. 164A, 1648–1658 (2014).
Cronister, A., DiMaio, M., Mahoney, M. J., Donnenfeld, A. E. & Hallam, S. Fragile X syndrome carrier screening in the prenatal genetic counseling setting. Genet. Med. 7, 246–250 (2005).
Strom, C. M. et al. Molecular testing for fragile X syndrome: lessons learned from 119,232 tests performed in a clinical laboratory. Genet. Med. 9, 46–51 (2007).
Owens, K. M. et al. FMR1 premutation frequency in a large, ethnically diverse population referred for carrier testing. Am. J. Med. Genet. A. 176, 1304–1308 (2018).
Levesque, S. et al. Screening and instability of FMR1 alleles in a prospective sample of 24,449 mother-newborn pairs from the general population. Clin. Genet. 76, 511–523 (2009).
Rousseau, F., Rouillard, P., Morel, M. L., Khandjian, E. W. & Morgan, K. Prevalence of carriers of premutation-size alleles of the FMRI gene–and implications for the population genetics of the fragile X syndrome. Am. J. Hum. Genet. 57, 1006–1018 (1995).
Dombrowski, C. et al. Premutation and intermediate-size FMR1 alleles in 10,572 males from the general population: loss of an AGG interruption is a late event in the generation of fragile X syndrome alleles. Hum. Mol. Genet. 11, 371–378 (2002).
Berkenstadt, M., Ries-Levavi, L., Cuckle, H., Peleg, L. & Barkai, G. Preconceptional and prenatal screening for fragile X syndrome: experience with 40,000 tests. Prenat. Diagn. 27, 991–994 (2007).
Pesso, R. et al. Screening for fragile X syndrome in women of reproductive age. Prenat. Diagn. 20, 611–614 (2000).
Hagerman, P. J. The fragile X prevalence paradox. J. Med. Genet. 45, 498–499 (2008).
Toledano-Alhadef, H. et al. Fragile-X carrier screening and the prevalence of premutation and full-mutation carriers in Israel. Am. J. Hum. Genet. 69, 351–360 (2001).
Falik-Zaccai, T. C. et al. Predisposition to the fragile X syndrome in Jews of Tunisian descent is due to the absence of AGG interruptions on a rare Mediterranean haplotype. Am. J. Hum. Genet. 60, 103–112 (1997).
Tzeng, C. C. et al. Prevalence of the FMR1 mutation in Taiwan assessed by large-scale screening of newborn boys and analysis of DXS548-FRAXAC1 haplotype. Am. J. Med. Genet. A. 133A, 37–43 (2005).
Cellini, E. et al. Fragile X premutation with atypical symptoms at onset. Arch. Neurol. 63, 1135–1138 (2006).
Sullivan, S. D., Welt, C. & Sherman, S. FMR1 and the continuum of primary ovarian insufficiency. Semin. Reprod. Med. 29, 299–307 (2011).
De Caro, J. J., Dominguez, C. & Sherman, S. L. Reproductive health of adolescent girls who carry the FMR1 premutation: expected phenotype based on current knowledge of fragile X-associated primary ovarian insufficiency. Ann. N. Y. Acad. Sci. 1135, 99–111 (2008).
Folsom, T. D., Thuras, P. D. & Fatemi, S. H. Protein expression of targets of the FMRP regulon is altered in brains of subjects with schizophrenia and mood disorders. Schizophr. Res. 165, 201–211 (2015).
American College of Obstetricians and Gynecologists Committee on Genetics. ACOG Committee Opinion No. 469: carrier screening for fragile X syndrome. Obstet. Gynecol. 116, 1008–1010 (2010).
Committee on Genetics. Committee Opinion No. 691: carrier screening for genetic conditions. Obstet. Gynecol. 129, e41–e55 (2017).
Kronquist, K. E., Sherman, S. L. & Spector, E. B. Clinical significance of tri-nucleotide repeats in fragile X testing: a clarification of American College of Medical Genetics guidelines. Genet. Med. 10, 845–847 (2008).
Sherman, S., Pletcher, B. A. & Driscoll, D. A. Fragile X syndrome: diagnostic and carrier testing. Genet. Med. 7, 584–587 (2005).
Finucane, B. et al. Genetic counseling and testing for FMR1 gene mutations: practice guidelines of the National Society of Genetic Counselors. J. Genet. Couns. 21, 752–760 (2012).
Weinstein, V., Tanpaiboon, P., Chapman, K. A., Ah Mew, N. & Hofherr, S. Do the data really support ordering fragile X testing as a first-tier test without clinical features? Genet. Med. 19, 1317–1322 (2017).
Borch, L. A., Parboosingh, J., Thomas, M. A. & Veale, P. Re-evaluating the first-tier status of fragile X testing in neurodevelopmental disorders. Genet. Med. 22, 1036–1039 (2020).
de Vries, B. B. et al. Mental status of females with an FMR1 gene full mutation. Am. J. Hum. Genet. 58, 1025–1032 (1996).
Hagerman, R. J. et al. Girls with fragile X syndrome: physical and neurocognitive status and outcome. Pediatrics. 89, 395–400 (1992).
Willemsen, R., Bontekoe, C. J., Severijnen, L. A. & Oostra, B. A. Timing of the absence of FMR1 expression in full mutation chorionic villi. Hum. Genet. 110, 601–605 (2002).
Maddalena, A., Hicks, B. D., Spence, W. C., Levinson, G. & Howard-Peebles, P. N. Prenatal diagnosis in known fragile X carriers. Am. J. Med. Genet. 51, 490–496 (1994).
Oostra, B. A. & Willemsen, R. Diagnostic tests for fragile X syndrome. Expert. Rev. Mol. Diagn. 1, 226–232 (2001).
den Dunnen, J. T. et al. HGVS recommendations for the description of sequence variants: 2016 update. Hum. Mutat. 37, 564–569 (2016).
Weck, K. E., Zehnbauer, B., Datto, M. & Schrijver, I. Molecular genetic testing for fragile X syndrome: laboratory performance on the College of American Pathologists proficiency surveys (2001-2009). Genet. Med. 14, 306–312 (2012).
Nolin, S. L. et al. Expansions and contractions of the FMR1 CGG repeat in 5,508 transmissions of normal, intermediate, and premutation alleles. Am. J. Med. Genet. A. 179, 1148–1156 (2019).
Nolin, S. L. et al. Familial transmission of the FMR1 CGG repeat. Am. J. Hum. Genet. 59, 1252–1261 (1996).
Hagerman, P. J. & Hagerman, R. J. Fragile X–associated tremor/ataxia syndrome. Ann. N. Y. Acad. Sci. 1338, 58–70 (2015).
Hall, D., Tassone, F., Klepitskaya, O. & Leehey, M. Fragile X–associated tremor ataxia syndrome in FMR1 gray zone allele carriers. Mov. Disord. 27, 296–300 (2012).
Fernandez-Carvajal, I. et al. Expansion of an FMR1 grey-zone allele to a full mutation in two generations. J. Mol. Diagn. 11, 306–310 (2009).
Manor, E. et al. The role of AGG interruptions in the FMR1 gene stability: a survey in ethnic groups with low and high rate of consanguinity. Mol. Genet. Genomic Med. 7, e00946 (2019).
Hunter, J. E., Abramowitz, A., Rusin, M. & Sherman, S. L. Is there evidence for neuropsychological and neurobehavioral phenotypes among adults without FXTAS who carry the FMR1 premutation? A review of current literature. Genet. Med. 11, 79–89 (2009).
Kallinen, J., Heinonen, S., Mannermaa, A. & Ryynanen, M. Prenatal diagnosis of fragile X syndrome and the risk of expansion of a premutation. Clin. Genet. 58, 111–115 (2000).
Nolin, S. L. et al. Expansion of the fragile X CGG repeat in females with premutation or intermediate alleles. Am. J. Hum. Genet. 72, 454–464 (2003).
Godler, D. E. et al. Methylation of novel markers of fragile X alleles is inversely correlated with FMRP expression and FMR1 activation ratio. Hum. Mol. Genet. 19, 1618–1632 (2010).
Wakeling, E. N., Nahhas, F. A. & Feldman, G. L. Extra alleles in FMR1 triple-primed PCR: artifact, aneuploidy, or somatic mosaicism? J. Mol. Diagn. 16, 689–696 (2014).
Hagerman, R. J. et al. High functioning fragile X males: demonstration of an unmethylated fully expanded FMR-1 mutation associated with protein expression. Am. J. Med. Genet. 51, 298–308 (1994).
Rousseau, F., Robb, L. J., Rouillard, P. & Der Kaloustian, V. M. No mental retardation in a man with 40% abnormal methylation at the FMR-1 locus and transmission of sperm cell mutations as premutations. Hum. Mol. Genet. 3, 927–930 (1994).
Schmucker, B. & Seidel, J. Mosaicism for a full mutation and a normal size allele in two fragile X males. Am. J. Med. Genet. 84, 221–225 (1999).
Smeets, H. J. et al. Normal phenotype in two brothers with a full FMR1 mutation. Hum. Mol. Genet. 4, 2103–2108 (1995).
Hensel, C. H. et al. Abnormally methylated FMR1 in absence of a detectable full mutation in a U.S.A patient cohort referred for fragile X testing. Sci. Rep. 9, 15315 (2019).
Yrigollen, C. M. et al. AGG interruptions within the maternal FMR1 gene reduce the risk of offspring with fragile X syndrome. Genet. Med. 14, 729–736 (2012).
Nolin, S. L. et al. Fragile X full mutation expansions are inhibited by one or more AGG interruptions in premutation carriers. Genet. Med. 17, 358–364 (2015).
Yrigollen, C. M. et al. AGG interruptions and maternal age affect FMR1 CGG repeat allele stability during transmission. J. Neurodev. Disord. 6, 24 (2014).
Latham, G. J., Coppinger, J., Hadd, A. G. & Nolin, S. L. The role of AGG interruptions in fragile X repeat expansions: a twenty-year perspective. Front. Genet. 5, 244 (2014).
Ardui, S. et al. Detecting AGG interruptions in females with a FMR1 premutation by long-read single-molecule sequencing: a 1 year clinical experience. Front. Genet. 9, 150 (2018).
Amos Wilson, J. et al. Consensus characterization of 16 FMR1 reference materials: a consortium study. J. Mol. Diagn. 10, 2–12 (2008).
Nakahori, Y. et al. Molecular heterogeneity of the fragile X syndrome. Nucleic Acids Res. 19, 4355–4359 (1991).
Rousseau, F. et al. Direct diagnosis by DNA analysis of the fragile X syndrome of mental retardation. N. Engl. J. Med. 325, 1673–1681 (1991).
Verkerk, A. J. et al. Identification of a gene (FMR-1) containing a CGG repeat coincident with a breakpoint cluster region exhibiting length variation in fragile X syndrome. Cell. 65, 905–914 (1991).
Yu, S. et al. Fragile X genotype characterized by an unstable region of DNA. Science. 252, 1179–1181 (1991).
Brown, W. T. et al. Rapid fragile X carrier screening and prenatal diagnosis using a nonradioactive PCR test. JAMA. 270, 1569–1575 (1993).
Erster, S. H. et al. Polymerase chain reaction analysis of fragile X mutations. Hum. Genet. 90, 55–61 (1992).
Fu, Y. H. et al. Variation of the CGG repeat at the fragile X site results in genetic instability: resolution of the Sherman paradox. Cell. 67, 1047–1058 (1991).
Yu, S. et al. Fragile-X syndrome: unique genetics of the heritable unstable element. Am. J. Hum. Genet. 50, 968–980 (1992).
Das, S. et al. Methylation analysis of the fragile X syndrome by PCR. Genet. Test. 1, 151–155 (1997–1998).
Panagopoulos, I., Lassen, C., Kristoffersson, U. & Aman, P. A methylation PCR approach for detection of fragile X syndrome. Hum. Mutat. 14, 71–79 (1999).
de Graaff, E. et al. Hotspot for deletions in the CGG repeat region of FMR1 in fragile X patients. Hum. Mol. Genet. 4, 45–49 (1995).
Chen, L. et al. An information-rich CGG repeat primed PCR that detects the full range of fragile X expanded alleles and minimizes the need for southern blot analysis. J. Mol. Diagn. 12, 589–600 (2010).
Chen, L. et al. High-resolution methylation polymerase chain reaction for fragile X analysis: evidence for novel FMR1 methylation patterns undetected in southern blot analyses. Genet. Med. 13, 528–538 (2011).
Hantash, F. M. et al. Qualitative assessment of FMR1 (CGG)n triplet repeat status in normal, intermediate, premutation, full mutation, and mosaic carriers in both sexes: implications for fragile X syndrome carrier and newborn screening. Genet. Med. 12, 162–173 (2010).
Lyon, E. et al. A simple, high-throughput assay for fragile X expanded alleles using triple repeat primed PCR and capillary electrophoresis. J. Mol. Diagn. 12, 505–511 (2010).
Nahhas, F. A. et al. Evaluation of the human fragile X mental retardation 1 polymerase chain reaction reagents to amplify the FMR1 gene: testing in a clinical diagnostic laboratory. Genet. Test. Mol. Biomarkers. 16, 187–192 (2012).
Tassone, F., Pan, R., Amiri, K., Taylor, A. K. & Hagerman, P. J. A rapid polymerase chain reaction-based screening method for identification of all expanded alleles of the fragile X (FMR1) gene in newborn and high-risk populations. J. Mol. Diagn. 10, 43–49 (2008).
Zhou, Y. et al. Robust fragile X (CGG)n genotype classification using a methylation specific triple PCR assay. J. Med. Genet. 41, e45 (2004).
Nygren, A. O. H., Lens, S. I. & Carvalho, R. Methylation-specific multiplex ligation-dependent probe amplification enables a rapid and reliable distinction between male FMR1 premutation and full-mutation alleles. J. Mol. Diagn. 10, 496–501 (2008).
Elias, M. H. et al. A new method for FMR1 gene methylation screening by multiplex methylation-specific real-time polymerase chain reaction. Genet. Test. Mol. Biomarkers. 15, 387–393 (2011).
Schaefer, G. B. & Mendelsohn, N. J. Clinical genetics evaluation in identifying the etiology of autism spectrum disorders: 2013 guideline revisions. Genet. Med. 15, 399–407 (2013).
Shaffer, L. G. American College of Medical Genetics guideline on the cytogenetic evaluation of the individual with developmental delay or mental retardation. Genet. Med. 7, 650–654 (2005).
Heitz, D., Devys, D., Imbert, G., Kretz, C. & Mandel, J. L. Inheritance of the fragile X syndrome: size of the fragile X premutation is a major determinant of the transition to full mutation. J. Med. Genet. 29, 794–801 (1992).
Patsalis, P. C. et al. Genetic variation and intergenerational FMR1 CGG-repeat stability in 100 unrelated three-generation families from the normal population. Am. J. Med. Genet. 84, 217–220 (1999).
Rife, M. et al. Analysis of CGG variation through 642 meioses in fragile X families. Mol. Hum. Reprod. 10, 773–776 (2004).
Zeesman, S. et al. Paternal transmission of fragile X syndrome. Am. J. Med. Genet. A. 129A, 184–189 (2004).
Bahlo, M. et al. Recent advances in the detection of repeat expansions with short-read next-generation sequencing. F1000Res. 7, F1000 (2018).
Tankard, R. M. et al. Detecting expansions of tandem repeats in cohorts sequenced with short-read sequencing data. Am. J. Hum. Genet. 103, 858–873 (2018).
Dolzhenko, E. et al. Detection of long repeat expansions from PCR-free whole-genome sequence data. Genome Res. 27, 1895–1903 (2017).
Dashnow, H. et al. STRetch: detecting and discovering pathogenic short tandem repeat expansions. Genome Biol. 19, 121 (2018).
Mousavi, N., Shleizer-Burko, S., Yanicky, R. & Gymrek, M. Profiling the genome-wide landscape of tandem repeat expansions. Nucleic Acids Res. 47, e90 (2019).
Loomis, E. W. et al. Sequencing the unsequenceable: expanded CGG-repeat alleles of the fragile X gene. Genome Res. 23, 121–128 (2013).
Fragile X syndrome: diagnostic and carrier testing. Am. J. Med. Genet. 53, 380–381 (1994).
Author information
Authors and Affiliations
Consortia
Ethics declarations
Competing interests
E.S., A.B., K.K., and H.V.R. direct or work in laboratories that offer clinical molecular genetic testing for fragile X syndrome. N.C.R. and E.L. declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Disclaimer
This technical standard is designed primarily as an educational resource for clinical laboratory geneticists to help them provide quality clinical laboratory genetic services. Adherence to this technical standard is voluntary and does not necessarily assure a successful medical outcome. This technical standard should not be considered inclusive of all proper procedures and tests or exclusive of other procedures and tests that are reasonably directed to obtaining the same results. In determining the propriety of any specific procedure or test, the clinical laboratory geneticist should apply his or her own professional judgment to the specific circumstances presented by the individual patient or specimen.
Clinical laboratory geneticists are encouraged to document in the patient’s record the rationale for the use of a particular procedure or test, whether or not it is in conformance with this technical standard. They also are advised to take notice of the date any particular technical standard was adopted, and to consider other relevant medical and scientific information that becomes available after that date. It also would be prudent to consider whether intellectual property interests may restrict the performance of certain tests and other procedures.
Note
This document supersedes the Technical Standards and Guidelines for Fragile X Testing: The First of a Series of Disease-Specific Supplements to the Standards and Guidelines for Clinical Genetics Laboratories of the American College of Medical Genetics and Genomics (2001),1 the Technical Standards and Guidelines for Fragile X Testing: A Revision to the Disease-Specific Supplements to the Standards and Guidelines for Clinical Genetics Laboratories of the American College of Medical Genetics and Genomics (2005)2 and the ACMG Standards and Guidelines for Fragile X testing: a revision to the disease-specific supplements to the Standards and Guidelines for Clinical Genetics Laboratories of the American College of Medical Genetics and Genomics (2013).3 It is designed for genetic testing professionals who are already familiar with the disease and the methods of analysis.
The Board of Directors of the American College of Medical Genetics and Genomics approved this technical standard on 14 December 2020.
Supplementary information
Rights and permissions
About this article
Cite this article
Spector, E., Behlmann, A., Kronquist, K. et al. Laboratory testing for fragile X, 2021 revision: a technical standard of the American College of Medical Genetics and Genomics (ACMG). Genet Med 23, 799–812 (2021). https://doi.org/10.1038/s41436-021-01115-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-021-01115-y
This article is cited by
-
Sequence composition changes in short tandem repeats: heterogeneity, detection, mechanisms and clinical implications
Nature Reviews Genetics (2024)
-
Attitudes of medical professionals toward fragile X carrier screening and genetic counseling in China
Journal of Community Genetics (2024)
-
A sensitive and reproducible qRT-PCR assay detects physiological relevant trace levels of FMR1 mRNA in individuals with Fragile X syndrome
Scientific Reports (2023)
-
Atypical vocal quality in women with the FMR1 premutation: an indicator of impaired sensorimotor control
Experimental Brain Research (2023)