Abstract
Purpose
To measure the prevalence of medically actionable pathogenic variants (PVs) among a population of healthy elderly individuals.
Methods
We used targeted sequencing to detect pathogenic or likely pathogenic variants in 55 genes associated with autosomal dominant medically actionable conditions, among a population of 13,131 individuals aged 70 or older (mean age 75 years) enrolled in the ASPirin in Reducing Events in the Elderly (ASPREE) trial. Participants had no previous diagnosis or current symptoms of cardiovascular disease, physical disability or dementia, and no current diagnosis of life-threatening cancer. Variant curation followed American College of Medical Genetics and Genomics/Association for Molecular Pathology (ACMG/AMP) standards.
Results
One in 75 (1.3%) healthy elderly individuals carried a PV. This was lower than rates reported from population-based studies, which have ranged from 1.8% to 3.4%. We detected 20 PV carriers for Lynch syndrome (MSH6/MLH1/MSH2/PMS2) and 13 for familial hypercholesterolemia (LDLR/APOB/PCSK9). Among 7056 female participants, we detected 15 BRCA1/BRCA2 PV carriers (1 in 470 females). We detected 86 carriers of PVs in lower-penetrance genes associated with inherited cardiac disorders.
Conclusion
Medically actionable PVs are carried in a healthy elderly population. Our findings raise questions about the actionability of lower-penetrance genes, especially when PVs are detected in the absence of symptoms and/or family history of disease.
Similar content being viewed by others
INTRODUCTION
The American College of Medical Genetics and Genomics (ACMG) has published a list of 59 genes relating to medically actionable conditions, intended to promote the standardized reporting of information from clinical sequencing.1 The ACMG’s recommendations do not extend to standardized reporting of research findings.2 However, recently some research groups have used the gene list as a guide for identifying medically actionable findings, including from research and in population-based DNA screening of asymptomatic adults.3,4,5 Of these 59 genes, 55 are associated with autosomal dominant conditions, where single variants confer disease predisposition.
The prevalence of pathogenic variant (PV) carriers for genes associated with autosomal dominant medically actionable conditions, using the ACMG59™ list as a guide, has recently been estimated from population-based studies at between 1 in 53 (1.8%) to 1 in 29 (3.4%).4,6,7 However, the prevalence of these PVs among healthy older individuals is unknown. Measuring PV frequencies in healthy older populations, as well as population-based studies, may improve understanding of gene penetrance, help overcome historic clinical ascertainment bias, and help determine the relative survival risk conferred by PVs during middle years of life. Healthy elderly populations may also provide new insights into the role of protective alleles in modifying gene penetrance.
Here, we measured PV frequencies in a population of 13,131 healthy elderly individuals from Australia enrolled in the ASPREE clinical trial,8 aged 70 years and older, without cardiovascular disease, dementia, physical disability, or life-threatening cancer diagnoses. We report the frequency of PVs in medically actionable genes among this uniquely ascertained population.
MATERIALS AND METHODS
Study population
All participants were enrolled in the ASPirin in Reducing Events in the Elderly (ASPREE) study, a randomized, placebo-controlled trial for daily low-dose aspirin. Study design,9 recruitment,10 baseline characteristics,11 and outcomes8 have been published previously. Genetic analysis was conducted on 13,131 samples from Australian participants aged 70 years or older who met ASPREE trial entry criteria at enrollment.11 Participants had no previous diagnosis or current symptoms of atherothrombotic cardiovascular disease, physical disability, or dementia, and no current diagnosis of life-threatening cancer at enrollment (ASPREE eligibility criteria in Supplementary Appendix).
DNA sequencing and variant analysis
A custom sequencing panel of 762 genes was designed, which included 59 genes on the ACMG59™ Secondary Findings list.1 Following standard protocols, DNA was extracted and sequenced using the Thermo Fisher Scientific S5TM XL system, to average 200× depth (see Supplementary Appendix). Variants with pathogenic or likely pathogenic annotation12 and/or high-confidence predicted loss-of-function in coding regions13 were curated following ACMG/Association for Molecular Pathology (AMP) Standards and Guidelines for the Interpretation of Sequence Variants,14 including review by two or more laboratory scientists and a clinical geneticist. Analysis was restricted to single-nucleotide variants and small insertions/deletions. Variants of uncertain significance or conflicting interpretations of pathogenicity were excluded.
Ethics statement
This work was approved by the Alfred Hospital Human Research Ethics Committee (project 390/15) in accordance with the National Statement on Ethical Conduct in Human Research (2007). Informed consent was obtained from all study participants.
RESULTS
Characteristics of the 13,131 sequenced participants are shown in Table 1 and include low rates of obesity and smoking, and no personal history of cardiovascular events or dementia at enrollment.11 Most participants were white/Caucasian and 54% were female. Age at enrollment ranged between 70–74 years (60%), 75–79 (26%), and >80 years (14%).
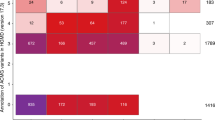
Among 13,131 participants, DNA sequencing and variant analysis identified 172 different pathogenic or likely pathogenic sequence variants meeting ACMG/AMP guidelines14 in 59 genes associated with medically actionable conditions. Of the PVs detected, 129 were in genes associated with autosomal dominant conditions, detected in 176 participants. This corresponded to a PV carrier rate of 1 in 75 healthy elderly participants (N = 176/13,131 or 1.3%). We validated a representative sample of 10% of these 129 variants by Sanger sequencing (N = 14), with 100% concordance. The highest number of PVs found in any one dominant gene was N = 22 (BRCA2 and KCNQ1) (Table 2 and Table S1).
We found that overall, the carrier rate for PVs in genes associated with autosomal dominant medically actionable conditions was lower in the healthy elderly (1 in 75 or 13 per 1000) than the UK Biobank (1 in 50 or 20 per 1000, unpublished data) and other population-based studies, which have reported carrier rates between 1 in 53 (1.8%) and 1 in 29 (3.4%).4,6,7
We detected 15 female BRCA1 or BRCA2 PV carriers among 7056 female ASPREE participants (0.2% or 2 per 1000). We detected 13 PV carriers for familial hypercholesterolemia genes (LDLR, APOB, PCSK9) and 20 carriers for Lynch syndrome genes (MSH6, MLH1, MSH2, PMS2). Additionally, we detected 86 PV carriers for genes associated with inherited cardiac disorders, including Romano–Ward, Brugada, and long QT syndrome (N = 39); hypertrophic and dilated cardiomyopathy (N = 25); and arrhythmogenic right-ventricular cardiomyopathy (N = 22).
We found no individuals carrying two or more variants in genes associated with autosomal recessive conditions (homozygotes or compound heterozygotes). However, we found two individuals carrying multiple PVs in genes associated with different autosomal dominant conditions (PMS2 + KCNQ1 and MYBPC3 + LDLR respectively).
DISCUSSION
In this study, we report the prevalence of PVs in genes associated with autosomal dominant medically actionable conditions, among a population of 13,131 healthy elderly individuals. The observed PV carrier rate was 1 in 75 participants, in a population of individuals aged 70 years and older without prior history or current symptoms of atherothrombotic cardiovascular disease, physical disability or dementia, or current diagnosis of life-threatening cancer.11 Compared with published population-based studies,4,6,7 lower PV frequencies were observed in mismatch-repair genes associated with Lynch syndrome and lipid metabolism genes associated with familial hypercholesterolemia. However, PVs in other genes with lower penetrance on the ACMG list were found at equivalent frequencies to population-based studies.4,6,7 Our findings raise questions about the medical actionability of these lower-penetrance genes, especially when PVs are detected in the absence of symptoms and/or family history of disease.
Strengths of the study include the unique ascertainment, enabling a rare opportunity for a population study of clinically significant genetic variation in >10,000 healthy older individuals. Other strengths include the depth of sequencing and stringency of variant curation, ensuring high-confidence PV calls. Limitations include ASPREE PV carriers potentially having a personal history of indicated disease prior to enrollment, including personal history of cancer (not an exclusion criterion of the study, unlike prior cardiovascular events). Other limitations include a sequencing assay not capable of detecting large structural variants, including those in MSH2 and other mismatch-repair genes. The strict variant curation criteria may also have resulted in an underestimation of PV carriers in ASPREE. Differences in variant curation likely account for some variability in rare PV frequencies reported between different studies.
We detected 176 carriers of PVs in genes associated with autosomal dominant medically actionable conditions in the healthy elderly ASPREE population (13 per 1000 participants). This relatively high rate of PV detection raises a clinically relevant question of whether there is an indicative age at which some PV carriers for dominant conditions outlive their genetic risk; that is, whether there is an age at which population risk and genetic risk for carriers of PVs converge and become equal. Previous studies suggest the majority of clinical risk attributed to PVs in genes associated with autosomal dominant conditions diminishes by age 70, especially for cancer.15,16 The diminishing risk conferred by PVs beyond age 70 could also have implications for predictive clinical testing of older individuals, and decisions around the return of genetic results to elderly research participants.17 However, that would not necessarily preclude older individuals from gaining benefits from genetic testing as it becomes more widespread, especially those with a family history of a disease.
In conclusion, PVs in genes associated with medically actionable conditions are carried by individuals in a healthy elderly population, often in the absence of indicated disease phenotypes. Further study of healthy elderly populations may provide an opportunity to identify protective alleles that may decrease the disease-causing effect of otherwise highly penetrant pathogenic variants.
Data and code availability
Data and code can be provided upon reasonable request from the corresponding author.
References
Kalia SS, Adelman K, Bale SJ, Chung WK, Eng C, Evans JP, et al. Recommendations for reporting of secondary findings in clinical exome and genome sequencing, 2016 update (ACMG SF v2.0): a policy statement of the American College of Medical Genetics and Genomics. Genet Med. 2017;19:249–255.
Directors ABO. The use of ACMG secondary findings recommendations for general population screening: a policy statement of the American College of Medical Genetics and Genomics (ACMG). Genet Med. 2019;21:1467–1468.
Linderman MD, Nielsen DE, Green RC. Personal genome sequencing in ostensibly healthy individuals and the PeopleSeq Consortium. J Pers Med. 2016;6:14.
Schwartz MLB, McCormick CZ, Lazzeri AL, Lindbuchler DM, Hallquist MLG, Manickam K, et al. A model for genome-first care: returning secondary genomic findings to participants and their healthcare providers in a large research cohort. Am J Hum Genet. 2018;103:328–337.
Carey DJ, Fetterolf SN, Davis FD, Faucett WA, Kirchner HL, Mirshahi U, et al. The Geisinger MyCode community health initiative: an electronic health record-linked biobank for precision medicine research. Genet Med. 2016;18:906–913.
Dewey FE, Murray MF, Overton JD, Habegger L, Leader JB, Fetterolf SN, et al. Distribution and clinical impact of functional variants in 50,726 whole-exome sequences from the DiscovEHR study. Science. 2016;354:aaf6814.
Haer-Wigman L, van der Schoot V, Feenstra I, Vulto-van Silfhout AT, Gilissen C, Brunner HG, et al. 1 in 38 individuals at risk of a dominant medically actionable disease. Eur J Hum Genet. 2019;27:325–330.
McNeil JJ, Woods RL, Nelson MR, Reid CM, Kirpach B, Wolfe R, et al. Effect of aspirin on disability-free survival in the healthy elderly. N Engl J Med. 2018;379:1499–1508.
Group AI. Study design of ASPirin in Reducing Events in the Elderly (ASPREE): a randomized, controlled trial. Contemp Clin Trials. 2013;36:555–564.
Lockery JE, Collyer TA, Abhayaratna WP, Fitzgerald SM, McNeil JJ, Nelson MR, et al. Recruiting general practice patients for large clinical trials: lessons from the Aspirin in Reducing Events in the Elderly (ASPREE) study. Med J Aust. 2019;210:168–173.
McNeil JJ, Woods RL, Nelson MR, Murray AM, Reid CM, Kirpach B, et al. Baseline characteristics of participants in the ASPREE (ASPirin in Reducing Events in the Elderly) study. J Gerontol A Biol Sci Med Sci. 2017;72:1586–1593.
Landrum MJ, Lee JM, Riley GR, Jang W, Rubinstein WS, Church DM, et al. ClinVar: public archive of relationships among sequence variation and human phenotype. Nucleic Acids Res. 2014;42(Database issue):D980–D985.
Lek M, Karczewski KJ, Minikel EV, Samocha KE, Banks E, Fennell T, et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature. 2016;536:285–291.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–424.
Kuchenbaecker KB, Hopper JL, Barnes DR, Phillips KA, Mooij TM, Roos-Blom MJ, et al. Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA. 2017;317:2402–2416.
Moller P, Seppala TT, Bernstein I, Holinski-Feder E, Sala P, Gareth Evans D, et al. Cancer risk and survival in path_MMR carriers by gene and gender up to 75 years of age: a report from the Prospective Lynch Syndrome Database. Gut. 2018;67:1306–1316.
Lacaze P, Ryan J, Woods R, Winship I, McNeil J. Pathogenic variants in the healthy elderly: unique ethical and practical challenges. J Med Ethics. 2017;43:714–722.
Acknowledgements
Supported by a Flagship cluster grant (including the Commonwealth Scientific and Industrial Research Organisation, Monash University, Menzies Research Institute, Australian National University, University of Melbourne), grants U01AG029824 from the National Institute on Aging and the National Cancer Institute at the National Institutes of Health, by grants 334047 and 1127060 from the National Health and Medical Research Council of Australia, and by Monash University and the Victorian Cancer Agency. We thank the trial staff in Australia and the United States, the participants who volunteered for this trial, and the general practitioners and staff of the medical clinics who cared for the participants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare no conflicts of interest.
Ethics committee approval
This work was approved by the Alfred Hospital Human Research Ethics Committee (project 390/15) in accordance with the National Statement on Ethical Conduct in Human Research (2007).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Joint first authors: Paul Lacaze, Robert Sebra
Joint senior authors: Ingrid Winship, John J McNeil, Eric Schadt
Supplementary information
Rights and permissions
About this article
Cite this article
Lacaze, P., Sebra, R., Riaz, M. et al. Medically actionable pathogenic variants in a population of 13,131 healthy elderly individuals. Genet Med 22, 1883–1886 (2020). https://doi.org/10.1038/s41436-020-0881-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-020-0881-7
Keywords
This article is cited by
-
A polygenic risk score predicts mosaic loss of chromosome Y in circulating blood cells
Cell & Bioscience (2021)
-
Genetic variants associated with inherited cardiovascular disorders among 13,131 asymptomatic older adults of European descent
npj Genomic Medicine (2021)
-
Population-based estimates of breast cancer risk for carriers of pathogenic variants identified by gene-panel testing
npj Breast Cancer (2021)