Abstract
Objectives
To determine the locations on the 24-2 visual field (VF) testing grid that are most likely to progress in patients with ocular hypertension (OHTN). Based on a structural model of superior and inferior areas of relative vulnerability at the optic disc, we hypothesized that the nasal and paracentral regions are more prone to show a reduction in sensitivity.
Methods
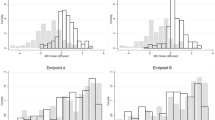
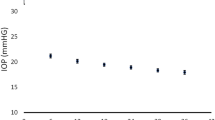
Posthoc analysis of data collected in phases 1 and 2 of the Ocular Hypertension Treatment Study (OHTS). A pointwise analysis was applied to determine the progression patterns in the early and delayed treatment groups. Each group’s progression rate and frequency were calculated for each of the 52 locations corresponding to the 24-2 VF strategy, using trend- and event-based analyses, respectively.
Results
For the event-based analysis, the events were most commonly found in the nasal and paracentral regions. The same regions, with some modest variation, were found to have the fastest rates of progression (ROP) measured with trend analysis. A similar pattern of progression was observed in both the early and delayed treatment groups. The difference in event rates and ROP between the early and delayed treatment groups was also greatest in the nasal and paracentral regions.
Conclusions
Development of VF loss in ocular hypertensive eyes appears to be consistent with the vulnerability zones previously described in glaucomatous eyes with established VF loss. Ocular hypotensive treatment likely helps to slow the rate of progression in these regions. This suggests that careful monitoring of these locations may be useful.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Data is available and will be provided upon reasonable request.
References
Hood DC, Wang DL, Raza AS, de Moraes CG, Liebmann JM, Ritch R. The locations of circumpapillary glaucomatous defects seen on frequency-domain OCT scans. Invest Ophthalmol Vis Sci. 2013;54:7338. https://doi.org/10.1167/iovs.13-12680.
Nouri-Mahdavi K, Hoffman D, Tannenbaum DP, Law SK, Caprioli J. Identifying early glaucoma with optical coherence tomography. Am J Ophthalmol. 2004;137:228–35. https://doi.org/10.1016/j.ajo.2003.09.004.
Medeiros FA, Zangwill LM, Bowd C, Vessani RM, Susanna R, Weinreb RN. Evaluation of retinal nerve fiber layer, optic nerve head, and macular thickness measurements for glaucoma detection using optical coherence tomography. Am J Ophthalmol. 2005;139:44–55. https://doi.org/10.1016/j.ajo.2004.08.069.
Kanamori A, Nakamura M, Escano MFT, Seya R, Maeda H, Negi A. Evaluation of the glaucomatous damage on retinal nerve fiber layer thickness measured by optical coherence tomography. Am J Ophthalmol. 2003;135:513–20. https://doi.org/10.1016/s0002-9394(02)02003-2.
Budenz DL, Michael A, Chang RT, McSoley J, Katz J. Sensitivity and specificity of the StratusOCT for perimetric glaucoma. Ophthalmology. 2005;112:3–9. https://doi.org/10.1016/j.ophtha.2004.06.039.
Quigley HA, Green WR. The histology of human glaucoma cupping and optic nerve damage: clinicopathologic correlation in 21 eyes. Ophthalmology. 1979;86:1803–30. https://doi.org/10.1016/s0161-6420(79)35338-6.
Hood DC. Improving our understanding, and detection, of glaucomatous damage: An approach based upon optical coherence tomography (OCT). Prog Retin Eye Res. 2017;57:46–75. https://doi.org/10.1016/j.preteyeres.2016.12.002.
Gordon MO. The ocular hypertension treatment study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:714. https://doi.org/10.1001/archopht.120.6.714.
Asman P, Heijl A. Glaucoma Hemifield Test. Automated visual field evaluation. Arch Ophthalmol. 1992;110:812–9. https://doi.org/10.1001/archopht.1992.01080180084033.
Gordon MO. The ocular hypertension treatment study: design and baseline description of the participants. Arch Ophthalmol. 1999;117:573. https://doi.org/10.1001/archopht.117.5.573.
Johnson CA, Keltner JL, Cello KE, Edwards M, Kass MA, Gordon MO, et al. Baseline visual field characteristics in the ocular hypertension treatment study. Ophthalmology. 2002;109:432–7. https://doi.org/10.1016/s0161-6420(01)00948-4.
Keltner JL, Johnson CA, Cello KE, Edwards MA, Bandermann SE, Kass MA, et al. Classification of visual field abnormalities in the ocular hypertension treatment study. Arch Ophthalmol. 2003;121:643–50. https://doi.org/10.1001/archopht.121.5.643.
De Moraes CG, Demirel S, Gardiner SK, Liebmann JM, Cioffi GA, Ritch R, et al. Effect of treatment on the rate of visual field change in the ocular hypertension treatment study observation group. Invest Ophthalmol Vis Sci. 2012;53:1704. https://doi.org/10.1167/iovs.11-8186.
Wild JM, Pacey IE, Hancock SA, Cunliffe IABetween-algorithm. between-individual differences in normal perimetric sensitivity: full threshold, FASTPAC, and SITA. Swedish Interactive Threshold algorithm. Invest Ophthalmol Vis Sci. 1999;40:1152–61.
Budenz DL, Rhee P, Feuer WJ, McSoley J, Johnson CA, Anderson DR. Comparison of glaucomatous visual field defects using standard full threshold and Swedish interactive threshold algorithms. Arch Ophthalmol. 2002;120:1136–41. https://doi.org/10.1001/archopht.120.9.1136.
Jansonius NM, Schiefer J, Nevalainen J, Paetzold J, Schiefer U. A mathematical model for describing the retinal nerve fiber bundle trajectories in the human eye: average course, variability, and influence of refraction, optic disc size and optic disc position. Exp Eye Res. 2012;105:70–8. https://doi.org/10.1016/j.exer.2012.10.008.
R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2019. Available at: https://www.R-project.org/.
Wickham H, François R, Henry L, Müller K. Dplyr: A grammar of data manipulation.; 2019. Available at: https://CRAN.R-project.org/package=dplyr.
Wickham H, Henry L. Tidyr: Easily tidy data with ’spread()’ and ’gather()’ functions.; 2019. Available at: https://CRAN.R-project.org/package=tidyr.
Wickham H, Chang W, Henry L, Pedersen TL Takahashi K, Wilke C, et al. Ggplot2: Create elegant data visualizations using the grammar of graphics.; 2019. Available at: https://CRAN.R-project.org/package=ggplot2.
Wilke CO. Cowplot: Streamlined plot theme and plot annotations for ’ggplot2’.; 2019. Available at: https://CRAN.R-project.org/package=cowplot.
Xie Y. Knitr: A general-purpose package for dynamic report generation in r.; 2019. Available at: https://CRAN.R-project.org/package=knitr.
Xie Y. Bookdown: Authoring books and technical documents with r markdown.; 2018. Available at: https://CRAN.R-project.org/package=bookdown.
Germano RAS, Germano CS, Susanna FN, Susanna R. Patterns of visual field loss in early, moderate, and severe stages of open angle glaucoma. J Glaucoma. 2022;31:609–13. https://doi.org/10.1097/IJG.0000000000001986.
Werner EB, Beraskow J. Peripheral nasal field defects in glaucoma. Ophthalmology. 1979;86:1875–8. https://doi.org/10.1016/s0161-6420(79)35335-0.
Lau LI, Liu CJling, Chou JCK, Hsu WM, Liu JH. Patterns of visual field defects in chronic angle-closure glaucoma with different disease severity. Ophthalmology. 2003;110:1890–4. https://doi.org/10.1016/S0161-6420(03)00666-3.
Bonomi L, Marraffa M, Marchini G, Canali N. Perimetric defects after a single acute angle-closure glaucoma attack. Graefes Arch Clin Exp Ophthalmol. 1999;237:908–14. https://doi.org/10.1007/s004170050385.
Park SC, De Moraes CG, Teng CCW, Tello C, Liebmann JM, Ritch R. Initial Parafoveal versus peripheral scotomas in glaucoma: risk factors and visual field characteristics. Ophthalmology. 2011;118:1782–9. https://doi.org/10.1016/j.ophtha.2011.02.013.
Park SC, Kung Y, Su D, Simonson JL, Furlanetto RL, Liebmann JM, et al. Parafoveal scotoma progression in glaucoma. Ophthalmology. 2013;120:1546–50. https://doi.org/10.1016/j.ophtha.2013.01.045.
De Moraes CG, Sun A, Jarukasetphon R, Rajshekhar R, Shi L, Blumberg DM, et al. Association of macular visual field measurements with glaucoma staging systems. JAMA Ophthalmol. 2019;137:139–45. https://doi.org/10.1001/jamaophthalmol.2018.5398.
Schiefer U, Papageorgiou E, Sample PA, Pascual JP, Selig B, Krapp E, et al. Spatial pattern of glaucomatous visual field loss obtained with regionally condensed stimulus arrangements. Invest Ophthalmol Vis Sci. 2010;51:5685–9. https://doi.org/10.1167/iovs.09-5067.
Heijl A, Lundqvist L. The frequency distribution of earliest glaucomatous visual field defects documented by automatic perimetry. Acta Ophthalmol. 1984;62:658–64. https://doi.org/10.1111/j.1755-3768.1984.tb03979.x.
Hood DC, La Bruna S, Tsamis E, Leshno A, Melchior B, Grossman J, et al. The 24-2 visual field guided progression analysis can miss the progression of glaucomatous damage of the macula seen using OCT. Ophthalmol Glaucoma. 2022;5:614–27. https://doi.org/10.1016/j.ogla.2022.03.007.
Pathak M, Demirel S, Gardiner SK. Nonlinear trend analysis of longitudinal pointwise visual field sensitivity in suspected and early glaucoma. Trans Vis Sci Tech. 2015;4:8 https://doi.org/10.1167/tvst.4.1.8.
Leske MC, Heijl A, Hyman L, Bengtsson B, Dong L, Yang Z, et al. Predictors of long-term progression in the early manifest glaucoma trial. Ophthalmology. 2007;114:1965–72. https://doi.org/10.1016/j.ophtha.2007.03.016.
The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration.The AGIS Investigators. Am J Ophthalmol. 2000;130:429-40. https://doi.org/10.1016/s0002-9394(00)00538-9.
Musch DC, Gillespie BW, Lichter PR, Niziol LM, Janz NK. CIGTS Study Investigators. Visual field progression in the Collaborative Initial Glaucoma Treatment Study the impact of treatment and other baseline factors. Ophthalmology. 2009;116:200–7. https://doi.org/10.1016/j.ophtha.2008.08.051.
Miglior S, Zeyen T, Pfeiffer N, Cunha-Vaz J, Torri V, Adamsons I, et al. The European glaucoma prevention study design and baseline description of the participants. Ophthalmology. 2002;109:1612–21. https://doi.org/10.1016/s0161-6420(02)01167-3.
Medeiros FA, Weinreb RN, Zangwill LM, Alencar LM, Sample PA, Vasile C, et al. Long-term intraocular pressure fluctuations and risk of conversion from ocular hypertension to glaucoma. Ophthalmology. 2008;115:934–40. https://doi.org/10.1016/j.ophtha.2007.08.012.
Folgar FA, de Moraes CGV, Prata TS, Teng CC, Tello C, Ritch R, et al. Glaucoma surgery decreases the rates of localized and global visual field progression. Am J Ophthalmol. 2010;149:258–264.e2. https://doi.org/10.1016/j.ajo.2009.09.010.
Kass MA, Gordon MO, Gao F, Heuer DK, Higginbotham EJ, Johnson CA, et al. Delaying treatment of ocular hypertension: the ocular hypertension treatment study. Arch Ophthalmol. 2010;128:276–87. https://doi.org/10.1001/archophthalmol.2010.20.
Funding
Supported in part by the Jane and David Walentas Glaucoma Research Fund, Columbia University Department of Ophthalmology; an unrestricted grant to the Department of Ophthalmology, Columbia University Department of Ophthalmology from Research to Prevent Blindness, Inc., New York, NY USA; and Schur Family Glaucoma Fellowship (AL), Columbia University Department of Ophthalmology.
Author information
Authors and Affiliations
Contributions
Conceptualization: NB, CGDM, JML; Data curation: NB, CGDM, JML, MOG, MAK; Formal analysis: AL, CGDM, NB; Investigation: AL, CGDM, JML, NB; Methodology: AL, JML, CGDM, MOG, MAK, GAC; Project administration: AL, JML, CGDM; Resources: GAC, CGDM and JML; Supervision: JML, GAC and CGDM; Validation: CGDM, MOG, MAK, GAC, JML; Writing – original draft: AL, JML, NB, CGDM; Writing - review & editing: AL, JML, NB, MOG, MAK, GAC, JML.
Corresponding author
Ethics declarations
Competing interests
Carlos G. De Moraes: Carl Zeiss Meditec, Inc. (C); Novartis (C); Heidelberg Engineering (R); Topcon (F); Galimedix (C); Perfuse Therapeutics (C); Ora Clinical, Inc. (E) Jeffrey M. Liebmann: Novartis (R), Alcon (C), Allergan (C), Genentech (C), Thea (C).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Leshno, A., Bommakanti, N., De Moraes, C.G. et al. Visual field progression patterns in the ocular hypertension treatment study correspond to vulnerability regions of the disc. Eye 38, 1549–1555 (2024). https://doi.org/10.1038/s41433-024-02949-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-024-02949-x